Abstract
In this study, the optimal combination of three commercial glycoprotein G-2 (gG-2)-based herpes simplex virus type 2 (HSV-2) type-specific enzyme-linked immunosorbent assays (Euroimmun anti-HSV-2 immunoglobulin G [IgG] ELISA [Eu2], Gull HSV-2-specific IgG ELISA [Gu2], and Radim HSV-2 IgG ELISA [Ra2]) and one gG-2-based HSV-2-specific immunoblot (Euroimmun anti-HSV-1/HSV-2 gG Western blot [EuW]) was determined with regard to diagnostic performance and cost efficiency. Two hundred fifty serum samples were included in this study, 194 of which were from female prostitutes. When a formal primary “gold standard” was defined based on majority agreement of the commercial tests, with EuW being decisive in stand-off situations, the sensitivity and specificity of the assays in the samples from prostitutes were as follows: Eu2, 100 and 89.22%; Gu2, 94.44 and 96.08%; Ra2, 61.18 and 95.10%; and EuW, 98.90 and 100%. The most cost-effective confirmatory strategy in the samples from prostitutes was screening with Eu2, retesting positive and equivocal samples with Gu2, and resolving the remaining discordant results with EuW (estimated additional costs per sample, 79.02%; sensitivity, 100%; positive predictive value, 96.81%). Applying a self-developed gG-2-independent assay to the discordant and concordant negative samples in the samples from prostitutes suggested that the primary gold standard may have missed six HSV-2-positive samples. In conclusion, confirmatory strategies based on commercial gG-2-dependent seroassays result in an increase in the specificity of HSV-2-specific serology. However, further improvement of the sensitivity of current HSV-2-specific serology may require the additional exploitation of the gG-2-independent type-specific antibody response.
Genital herpes represents a global problem for public health, as it is one of the most prevalent sexually transmitted diseases (9). The number of people experiencing painful, chronic remittent illness due to genital herpes is estimated to be approximately 90 million worldwide. Serious medical consequences of genital herpes are neonatal infections and an increased risk of acquisition of other sexually transmitted infectious agents, such as human immunodeficiency virus (14, 33). In addition, genital herpes causes considerable psychological and psychosexual morbidity (27). Thus, measures to control its spread and guidelines for the management of infected individuals are urgently needed. Although herpes simplex virus type 1 (HSV-1) may be the causative agent of a significant proportion of first episodes of genital herpes, especially in young white females, the principal agent of chronic remittent herpes genitalis is HSV-2 (7). The abilities of the viruses to cause recurrent infections in the anogenital region differ significantly (20), with median recurrence rates of 5 for HSV-2 and 1 for HSV-1 in the first year after primary infection (4). A number of serological surveys indicate that in developed countries there is an ongoing HSV-2 epidemic, with a significant rise in HSV-2 seroprevalence over the last 2 decades (8, 11, 12, 18, 28). Risk factors for the acquisition of HSV-2 are female gender, high number of lifetime sexual partners, black race and/or African country of origin, and low socioeconomic status (17).
Roughly two-thirds of HSV-2 infections remain subclinical or completely asymptomatic. Therefore, most infections with HSV-2 remain undiagnosed, and the number of HSV-2 carriers is frequently underestimated. The high proportion of unrecognized carriers facilitates spread of HSV-2, since virus is shed intermittently from anogenital sites of most HSV-2-seropositive individuals. The majority of new infections with HSV-2 is thus believed to result from sexual contacts during periods of asymptomatic viral shedding by source partners (26).
Since virus isolation and PCR yield positive results only during phases of active infection and virus shedding, serological screening is needed for the reliable identification of individuals with a past HSV-2 infection (13). Detection of type-specific antibodies against HSV-2, however, is hampered by the extensive serological cross-reactivity between HSV-1 and HSV-2. At present, commercial immunoassays allowing a reliable detection of HSV-2-specific antibodies are mainly based on glycoprotein G-2 (gG-2) as the diagnostic antigen (2, 16). Glycoproteins G of HSV-1 and HSV-2 are highly divergent (25) and typically elicit no or only limited humoral cross-reactivity (21, 22).
Despite substantial progress in the development of simple, cost-effective commercial assays, such as gG-2-based enzyme-linked immunosorbent assays (ELISAs), however, determination of the individual serostatus may require confirmation of results in a second assay, such as immunoblotting. To address this problem, we first analyzed the diagnostic performance of three commercial type-specific ELISAs and a commercial immunoblot in a high-HSV-2-risk collective. Additionally, a gG-2-independent in-house immunoblot assay was applied. The principle of this test (which has been successfully employed for the identification of cross-reactive antibodies between HSV and varicella-zoster virus [19]) was to perform an immunoblot assay on blot strips carrying HSV-2 full antigen with serum samples that had each been preabsorbed with HSV-1 lysates, HSV-2 lysates, or both or mock absorbed. Changes in the reactivity pattern after preabsorption allowed a differentiation between type-common and HSV-2-specific reactivity of a given serum sample, taking into account the complete pattern of HSV-2-specific humoral immune response directed against epitopes other than gG-2. Based on the results of the commercial seroassays, we then evaluated potential confirmatory strategies.
Our results show that of all confirmatory strategies based exclusively on commercial assays, the sequential use of two screening ELISAs and retesting of sera with equivocal results by immunoblotting was the most cost-effective approach with reasonable sensitivity and specificity. The results obtained with the gG-2-independent assay suggested that the commercial assays may have missed some HSV-2-positive samples and that additional gG-2-independent approaches are needed to maximize the sensitivity of HSV-2-specific seroassays.
MATERIALS AND METHODS
Patients and sera.
A total of 250 serum samples were included in this study, 194 from routine examinations of human immunodeficiency virus-negative female prostitutes from North Rhine-Westphalia and 56 from nonselected hospitalized patients without type-common antibodies in Enzygnost HSV-IgG ELISA (Dade Behring, Marburg, Germany) as negative controls.
Viruses and cells.
The HSV strains in this study were the strains used by Euroimmun (Gross-Groenau, Germany) for production of the anti-HSV-1/HSV-2 gG Western blot assay (EuW) and the immunoblot strips employed in the in-house HSV-2-specific immunoblot assay (IhW; see below), i.e., HSV-1 strain F (ATCC 733) and HSV-2 strain G (ATCC 734). Viral stocks were obtained by serial passages at a multiplicity of infection of 0.01 PFU/cell. Low-passage titers were approximately 5 × 105 PFU/ml for HSV-1 F and 5 × 104 PFU/ml for HSV-2 G. For propagation of virus stocks, Vero cells (Vircell, Grenada, Spain) were used for HSV-1 and MRC-5 cells (Vircell) were used for HSV-2. Cells were maintained in 100% humidity, 5% CO2, and Eagle's minimal essential medium supplemented with antibiotics (penicillin, 100 U/ml; streptomycin, 100 μg/ml) and 5% fetal calf serum.
Type-common HSV ELISA.
All serum samples were tested for the presence of type-common HSV immunoglobulin G (IgG) and IgM antibodies with the Enzygnost HSV/IgG and IgM ELISA (Dade Behring; BeG and BeM, respectively) according to the manufacturer's instructions.
HSV-2-specific commercial assays.
The three HSV-2-specific ELISAs are based on gG-2: the Euroimmun anti-HSV-2 IgG ELISA (Eu2), the Gull Laboratories (Bad Homburg, Germany) HSV-2-specific IgG ELISA (Gu2), and the Radim (Sulzbach, Germany) HSV-2 IgG ELISA (Ra2). EuW consisted of HSV-1-loaded Western blot strips with an additional gG-2 band blotted onto the bottom of the strip. All tests were carried out according to the manufacturers' instructions.
Production of viral antigens and preabsorption of sera.
Production of viral antigens for preabsorption of sera was always done with Vero cells. Tissue culture flasks (175 cm2) were infected at a multiplicity of infection of 1 to 5 PFU/cell and incubated at least for 2 days or until 100% cytopathic effect was reached. Subsequently, cells were scraped into the medium and pelleted in conical 50-ml tubes by centrifugation at 2,000 × g and 4°C for 15 min. The supernatant was discarded, and the pellet was stored at −80°C until further use. To obtain cell lysates for preabsorption of sera, pellets were thawed, sonicated at 80 W for 5 min, and resuspended in 880 μl of sample dilution buffer provided with the Euroimmun Western blot kit. Preabsorption was performed by mixing 20 μl of serum with 440 μl of cell lysate and 40 μl of proteinase inhibitor (Complete; Roche, Mannheim, Germany) stock solution prepared according to the instructions of the manufacturer and adjusting to a final volume of 1 ml with sample dilution buffer. For mock absorption, the cell lysate was replaced with the appropriate volume of sample dilution buffer, and for preabsorption with both HSV types, 440 μl of HSV-1 lysate and 440 μl of HSV-2 lysate were used. Preabsorption mixtures were incubated at 4°C for 20 h under vigorous shaking and subsequently cleared by centrifugation at 50,000 × g and 4°C for 30 min. The supernatants were recovered, adjusted to 3 ml with sample dilution buffer to give a final serum dilution of 1:150, and stored at −20°C until further use.
IhW.
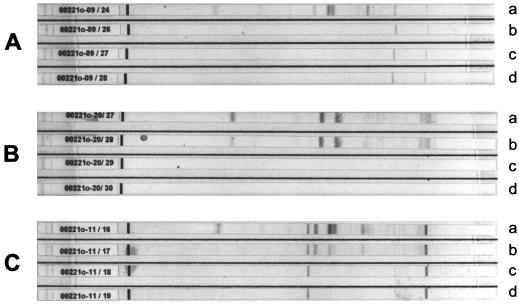
The immunoblot strips loaded with HSV-2 full antigen were manufactured by Euroimmun and are commercially available from Euroimmun upon request. Four strips per serum were preincubated with 1.5 ml of sample dilution buffer (see above) at room temperature for 15 min. Subsequently, one strip was incubated with 2 ml of mock-preabsorbed serum, a second strip was incubated with 2 ml of the same serum preabsorbed with HSV-1 lysate, a third strip was incubated with 2 ml of the serum preabsorbed with HSV-2 lysate, and a fourth strip was incubated with 2 ml of the same serum preabsorbed with both HSV strains. After overnight incubation at room temperature, strips were washed and further processed as described previously (19). The typical patterns for sera positive for HSV-2 antibodies, HSV-1 antibodies, or both are shown in Fig. 1. The criteria for the interpretation of the IhW are given in Table 1.
FIG. 1.
Prototype reactivity patterns of HSV-positive human sera in the HSV-2-specific in-house confirmatory assay. (A) HSV-2-negative serum; (B) exclusively HSV-2-positive serum; (C) HSV-1- and HSV-2-positive serum. Strips were loaded with lysates of HSV-2-infected cells. Shown are the serum reactivity patterns observed after mock absorption (a) or preabsorption with HSV-1 (b), HSV-2 (c), or HSV-1 and HSV-2 (d).
TABLE 1.
Evaluation criteria for the in-house confirmatory assay
| Observation | Result for:
|
||||
|---|---|---|---|---|---|
| Strip a | Strip b | Strip c | Strip d | HSV-2 | HSV-1 |
| No bands | No bands | No bands | No bands | Negative | Negative |
| Clear band(s) | No bands | No bands | No bands | Negative | Positive |
| Clear band(s) | Bands at the same position as on strip a, same intensity of the signal | No bands | No bands | Positive | Negative |
| Clear band(s) | Bands at the same position as on strip a, removal of antibody reactivity with single bands and/or lower intensity of the signal | No bands | No bands | Positive | Positive |
Test flow and definition of the HSV-2 serostatus.
All assays were performed by individual technical staff who were not informed about the outcome of the other tests. Sera were considered true HSV negatives if they were negative by BeG and showed no reactivity with HSV antigens by EuW. Sera positive by BeG were considered HSV positive. All sera were tested in parallel with Eu2, Gu2, Ra2, and EuW for HSV-2-specific antibodies; for the definition of a primary “gold standard” (PGS), sera with three or more positive results in the commercial tests were considered true HSV-2 positives, and in stand-off situations, the result of the EuW was used to determine the HSV-2 serostatus.
Estimation of cost of confirmatory strategies.
The estimation of additional costs raised by the individual confirmatory strategies was done in a relative manner. Based on the official tariffs of the German health insurance (Gebührenordnung für Ärzte), we defined the relative cost of an ELISA as 1 and the cost of a Western blot assay as 3.352. Cost estimations for a hypothetical low-risk collective were done by disregarding borderline results and assuming that the diagnostic performance of confirmatory tests was the same as in the high-risk collective studied here. The costs of a given confirmatory strategy were expressed as (i) the additional costs per sample in relation to the costs of the respective screening assay and (ii) the cost per additionally correctly diagnosed sample in relation to screening only.
RESULTS
HSV seroprevalence in female prostitutes.
Three of 194 serum samples did not react with the entire panel of commercial HSV type-common and HSV-2-specific seroassays employed in this study and were classified as HSV IgG and IgM seronegative. The remaining sera were positive by BeG (type-common HSV IgG), corresponding to a proportion of HSV-seropositive individuals of 98.5% (191 of 194). HSV IgM was detected in two HSV IgG-positive sera (BeM), and 20 sera gave equivocal results by BeM.
Specificity of the commercial gG-2-based ELISAs in an HSV-seronegative control group.
Fifty-six serum samples from HSV IgG- and IgM-seronegative individuals were assayed (for source and definition of HSV-negative control sera, see Materials and Methods). All samples were HSV-2 negative by Eu2 and EuW. In Gu2, four samples (7.1%) were repeatedly reactive and two samples (3.6%) yielded equivocal results. Thirteen samples (23.2%) were found to be reactive by Ra2, and four (7.1%) gave equivocal results. A single serum sample was positive by Gu2 and Ra2. No serum sample gave equivocal results in both assays.
Detection of HSV-2-specific antibodies in female prostitutes by commercial seroassays.
The results obtained with the gG-2-based HSV-2-specific seroassays are summarized in Table 2. In Eu2, 102 serum samples (52.57%) were reactive, 91 (46.91%) were negative, and 1 (0.52%) gave an equivocal result. In Gu2, 89 samples (45.88%) were reactive, 103 (53.09%) showed no reactivity, and 2 (1.03%) gave equivocal results. In Ra2, 57 samples (29.38%) were positive, 130 (67%) were negative, and 7 (3.61%) gave equivocal results.
TABLE 2.
Comparison of HSV-2 type-specific seroassays in sera from female prostitutes (n = 194)
| gG-2-based EIA(s) | gG-2-based commercial immunoblot
|
No. of sera positive by IhW/no. retested | ||||
|---|---|---|---|---|---|---|
| Yielding positive result | Yielding equivocal result | Yielding negative result | No. of sera | Resulta | No. of sera | |
| Eu2, Gu2, Ra2 | 52 | Pos | 51 | 14/14b | ||
| Neg | 1 | 1/1 | ||||
| Eu2, Gu2 | Ra2 | 6 | Pos | 6 | 6/6 | |
| Eu2, Gu2 | Ra2 | 30 | Pos | 27 | 26/27 | |
| Neg | 3 | 1/3 | ||||
| Eu2 | Gu2 | Ra2 | 1 | Pos | 1 | 1/1 |
| Eu2 | Gu2, Ra2 | 13 | Pos | 5 | 5/5 | |
| Neg | 8 | 2/8 | ||||
| Gu2 | Ra2, Eu2 | 1 | Neg | 1 | 0/1 | |
| Ra2 | Gu2 | Eu2 | 1 | Neg | 1 | 1/1 |
| Ra2 | Eu2, Gu2 | 4 | Neg | 4 | 0/4 | |
| Eu2 | Gu2, Ra2 | 1 | Neg | 1 | 1/1 | |
| Ra2 | Eu2, Gu2 | 1 | Neg | 1 | 0/1 | |
| Eu2, Gu2, Ra2 | 84 | Neg | 84 | 1/81c | ||
Pos, positive; neg, negative.
Sera were tested when the in-house confirmatory assay was evaluated.
Only HSV-positive sera (n = 81) were retested with the in-house confirmatory assay.
A total of 108 sera from female prostitutes were reactive in at least one gG-2-based ELISA. Of these, only 52 were shown to be consistently positive in all assays; 84 were consistently negative in all gG-2-based ELISAs, and 10 gave repeatedly equivocal results in gG-2-based ELISAs. Of the 194 sera from female prostitutes, 90 were recognized as HSV-2 seropositive by EuW.
Agreement of commercial gG-2-based seroassays.
Compared to the outcome of gG-2-based ELISAs, positive results in immunoblot EuW were obtained for 51 of 52 sera concordantly positive by Eu2, Gu2, and Ra2, in all six sera positive by Eu2 and Gu2 and equivocal by Ra2, in 27 of 30 sera positive by Eu2 and Gu2, in a single serum positive by Eu2 and equivocal by Gu2, and in 5 of 13 sera solely positive by Eu2. All sera concordantly negative by Eu2, Gu2, and Ra2 (n = 84) were also negative by EuW. Only 135 of 194 sera (69.6%) from female prostitutes gave concordant results in all commercial HSV-2-specific assays employed. Ra2 showed the highest rate of discrepant results. When the outcome of Ra2 was disregarded, concordant results were obtained in 173 sera (89.2%), i.e., 84 (48.6%) sera were positive and 89 were negative. Of the remaining 21 sera with discrepant results, 6 were positive by EuW. Four sera were negative by EuW but positive by Eu2 and Gu2, and one of these sera was additionally positive by Ra2.
Overall performance of the commercial assays.
When a formal PGS was established as described in Materials and Methods, i.e., a “majority decision” of the four commercial assays, the EuW being decisive in stand-off situations, 91 true-positive and 103 true-negative sera were identified in the prostitute sample collective (n = 194; prevalence, 46.91%). Based on this standard, the sensitivities, specificities, negative predictive values (NPVs), and positive predictive values (PPVs) of the commercial assays were as follows (Table 3): Eu2, 100, 89.22, 89.22, and 100%; Gu2, 94.44, 96.08, 95.51, and 95.15%; Ra2, 61.18, 95.10, 91.23, and 74.62%; and EuW, 98.9, 100, 100, and 99.04%. When a low-risk collective with a hypothetical prevalence of 10% was assumed for the calculation of predictive values, the PPVs and NPVs for the commercial tests were 50.75 and 100% (Eu2), 72.80 and 99.36% (Gu2), 58.10 and 95.66% (Ra2), and 100 and 99.88% (EuW).
TABLE 3.
Performance of commercial HSV type-specific assays
| Standard and assay | Value (%)
|
|||||
|---|---|---|---|---|---|---|
| Sensitivity | Specificity | PPV | NPV | PPVa | NPVa | |
| PGS | ||||||
| Eu2 | 100.00 | 89.22 | 89.22 | 100.00 | 50.75 | 100.00 |
| Gu2 | 94.44 | 96.08 | 95.51 | 95.15 | 72.80 | 99.36 |
| Ra2 | 61.18 | 95.10 | 91.23 | 74.62 | 58.10 | 95.66 |
| EuW | 98.90 | 100.00 | 100.00 | 99.04 | 100.00 | 99.88 |
| RGS | ||||||
| Eu2 | 97.92 | 91.75 | 92.16 | 97.80 | 56.88 | 99.75 |
| Gu2 | 90.53 | 96.91 | 96.63 | 91.26 | 76.48 | 98.93 |
| Ra2 | 58.24 | 95.83 | 92.98 | 70.77 | 60.83 | 95.38 |
| EuW | 92.78 | 100.00 | 100.00 | 93.27 | 100.00 | 99.20 |
Value obtained assuming a hypothetical HSV-2 seroprevalence of 10%.
IhW.
The performance of the IhW, that is, the efficacy of the preabsorption protocol for the stepwise removal of cross-reactive and HSV type-specific antibodies, was evaluated with 14 sera concordantly positive in the commercial HSV-2-specific seroassays and 14 sera consistently negative in these seroassays. In all these sera, the presence or absence of HSV-2-specific antibodies was detected: specific antibody reactivity with HSV-2 antigens remained after preabsorption with HSV-1 antigens but was abolished completely by preabsorption with HSV-2 antigens in gG-2-reactive sera, whereas preabsorption of gG-2-nonreactive sera with HSV-1 antigens completely abolished antibody reactivity with HSV-2 antigens (Fig. 1). All HSV-positive sera with discrepant (n = 59) or concordant negative (n = 81) results in the commercial HSV-2-specific seroassays were retested by the IhW. In 44 of 59 sera with discordant results in the commercial HSV-2-specific seroassays and in a single serum out of 81 HSV-positive sera without evidence of HSV-2-specific antibodies in gG-2-based commercial seroassays, the presence of HSV-2-specific antibodies was shown by the IhW (Table 2). In summary, six samples identified as HSV-2 negative by the PGS gave positive results in the IhW. The portion of additional IhW-positive samples increased with the number of commercial ELISAs positive for the respective samples: 1 of 81 (1.23%) when no commercial test was positive but 4 of 18 (22.22%) when one or two ELISAs were positive.
According to the outcome of IhW, a revised gold standard (RGS) was defined, including the samples additionally positive by the IhW. Based on this RGS, the HSV-2 seroprevalence in female prostitutes was 50% (97 of 194). A reranking of the HSV-2-specific commercial seroassays based on the RGS led to better specificities of ELISAs and revealed a general decrease of sensitivity of all commercial assays (Table 3).
Assessment of confirmatory strategies.
By using both gold standards as described above for comparative calculations, the performance of combinations of the commercial HSV-2-specific seroassays Eu2, Gu2, and EuW was investigated. For reasons of cost, we considered only approaches employing an ELISA for screening. The performances of the six confirmatory strategies considered here are summarized in Table 4. Due to its obviously poor diagnostic performance, the Ra2 ELISA was not further considered in this context.
TABLE 4.
Evaluation of confirmatory strategies
| Standard and strategya | Value (%)b
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | PPV | NPV | Costd | Coste | 10% Prevalencec
|
|||||
| PPV | NPV | Costd | Coste | ||||||||
| PGS | |||||||||||
| 1 | 100.00 | 89.32 | 89.22 | 100.00 | 1.73 | 335.16 | 50.99 | 100.00 | ND | ND | |
| 2 | 98.90 | 100.00 | 100.00 | 99.04 | 177.92 | 3,138.34 | 100.00 | 99.88 | 66.01 | 680.63 | |
| 3 | 94.51 | 96.12 | 95.56 | 95.19 | 3.46 | 335.16 | 73.00 | 99.37 | ND | ND | |
| 4 | 93.41 | 100.00 | 100.00 | 94.50 | 157.20 | 6,099.93 | 100.00 | 99.27 | 43.49 | 1,232.35 | |
| 5 | 100.00 | 97.09 | 96.81 | 100.00 | 129.39 | 2,788.63 | 79.23 | 100.00 | ND | ND | |
| 6 | 100.00 | 97.09 | 96.81 | 100.00 | 79.02 | 1,703.03 | 79.23 | 100.00 | 29.35 | 413.85 | |
| RGS | |||||||||||
| 1 | 97.94 | 91.75 | 92.23 | 97.80 | 335.16 | 56.89 | 99.75 | ND | ND | ||
| 2 | 92.78 | 100.00 | 100.00 | 93.27 | 6,904.31 | 100.00 | 99.20 | 57.71 | 777.16 | ||
| 3 | 89.69 | 96.91 | 96.67 | 90.38 | 335.16 | 76.32 | 98.83 | ND | ND | ||
| 4 | 87.63 | 100.00 | 100.00 | 88.99 | 15,249.82 | 100.00 | 98.64 | 39.66 | 1,426.21 | ||
| 5 | 94.85 | 97.94 | 97.87 | 95.00 | 6,274.45 | 83.64 | 99.42 | ND | ND | ||
| 6 | 94.85 | 97.94 | 97.87 | 95.00 | 1,915.94 | 83.64 | 99.42 | 25.58 | 459.25 | ||
Strategies are as follows: 1, screening with Eu2 and confirming equivocal results with EuW; 2, screening with Eu2 and confirming all positive and equivocal results with EuW; 3, screening with Gu2 and confirming all equivocal results with EuW; 4, screening with Gu2 and confirming all positive and equivocal results with EuW; 5, screening with Eu2 and Gu2 in parallel and resolving all discordant results with EuW; 6, screening with Eu2, retesting all positive and equivocal results with Gu2, and resolving the remaining discordant results with EuW.
ND, not determined.
Assuming a hypothetical 10% HSV-2 seroprevalence.
Additional cost of the confirmatory strategy per sample relative to the cost of screening only; in the high-risk collective identical values are obtained for PGS and RGS.
Additional cost of the confirmatory strategy per additional correctly diagnosed sample relative to the cost of screening only.
A simple and economic strategy would be to employ Eu2 or Gu2 as a screening test and to confirm only equivocal results by EuW (strategies 1 and 3; additional cost per sample, 1.72 and 3.47%, respectively). However, in the high-risk collective tested, this confirmatory strategy would have no or little effect on the overall sensitivity and specificity of HSV-2-specific serology compared to the use of a sensitive gG-2-based ELISA alone, irrespective of the gold standard applied. In contrast, confirmation of all equivocal and positive results by Eu2 and Gu2, respectively, by EuW (strategies 2 and 4) would allow a significant improvement in the overall specificity (89.22 to 100% for Eu2 and 96.08 to 100% for Gu2), but at the cost of a loss of sensitivity due to false-negative results in EuW. This effect was even more pronounced when calculations were based on the RGS. Following this confirmatory strategy in the prostitute sample collective, approximately one-half of the serum panel would have to be retested by immunoblotting, thereby greatly increasing the costs per sample compared to screening with an ELISA only (strategy 2, 177.92%; strategy 4, 157.2%).
A strategy comprising the simultaneous testing of all samples by Eu2 and Gu2 and retesting of all samples with discrepant or equivocal results with EuW can be expected to possess a reasonable sensitivity and specificity in the high-risk collective tested here (strategy 5). This approach entails additional costs of 129.39% per sample. Similar performance, albeit with a significantly lower number of assays and significantly less additional cost (79.02%), can be obtained with a three-step approach: all sera with positive or equivocal results by Eu2 are first retested with Gu2, and sera negative or equivocal by Gu2 are confirmed by EuW (strategy 6).
As a rule of thumb, all confirmatory strategies improved specificity at constant or only slightly reduced sensitivity compared to a single ELISA when the PGS was applied. If the RGS was applied, all confirmatory strategies led to a more pronounced loss of sensitivity and a gain in specificity (strategies 1, 3, 5, and 6) compared to the screening ELISAs. The costs per additional correct diagnosis (Table 4) roughly correlated with the respective additional costs per sample.
DISCUSSION
Identification of undiagnosed HSV-2 carriers by type-specific seroassays is an important measure to prevent virus transmission and monitor virus spread within the population (9). In recent years a number of seroassays based on gG-2 as the diagnostic antigen have been established and introduced into the market, most of which have proved to be useful diagnostic tools, allowing sensitive and specific detection of HSV-2-specific antibodies in human sera (1, 3, 10, 13, 15). Our results show that this holds true also for both newly developed commercial HSV-2-specific seroassays evaluated in the present study, i.e., Eu2 and EuW. There is evidence in the literature, however, that the reliability of actual gG-based HSV type-specific seroassays should not be overestimated because of (i) the effects of acyclovir treatment on anti-gG-2 antibody induction (6), (ii) occurrence of gG-2-negative HSV-2 strains (23), (iii) general genetic variability of gG (29), and (iv) positive-to-negative shifts in gG-1- and gG-2-based type-specific seroassays independently of the test format used in a significant percentage of individuals (31). Thus, actual gG-based type-specific seroassays may be well suited to cross-sectional analyses of the seroprevalence of both HSV types in defined collectives. However, there still appear to be deficits in the reliable determination of the individual type-specific serostatus.
As a basis for calculating the performance parameters for the commercial type-specific assays, we first defined a gold standard based exclusively on the results of the commercial assays (PGS; see above). The 46.91% HSV-2 seroprevalence found with this standard in the sera from prostitutes and the fact that all HSV type-common negative sera were also negative by this standard made it highly plausible. All considerations below refer to this PGS unless stated otherwise.
Of the commercial HSV-2-specific seroassays used in this study, Eu2 had the highest sensitivity (100%) and EuW had the highest specificity (100%).
Gu2 has already been evaluated in a number of previous studies and found to be highly sensitive and specific. Its sensitivity and specificity have been reported to be 98 and 97% (3), 96 and 96.2% (10), and 99.7 and 96.7% (13). In the present study, the diagnostic performance of this assay was found to be slightly lower (94.44% sensitivity and 96.08% specificity); however, this may be due to different patient collectives and different definitions of the gold standard.
In accordance to an earlier report (30), the diagnostic performance of Ra2 was poor. Due to its unacceptably low sensitivity of 61.18%, the use of this assay cannot be recommended, and it was not further considered during evaluation of confirmatory strategies.
The observed differences in the specificity between the commercial type-specific assays may become more accentuated in a low-risk collective. Thus, calculating the predictive values for a hypothetical collective with 10% HSV-2 seroprevalence, as found in German pregnant women (10, 34), suggested a significant drop in the PPVs of the screening ELISAs, whereas the PPV of the EuW remained unchanged (for details see Table 3).
Calculation of the overall agreement of the commercial HSV-2-specific assays demonstrated that only roughly two-thirds of sera gave concordant results in all commercial assays (135 of 194; 69.59%). Thus, in order to finally resolve the individual HSV-2-specific serostatus, we studied the diagnostic benefit of potential confirmatory strategies as has been proposed previously (9), employing the commercial assays evaluated in this study.
With respect to technical and economical expenses, HSV-2-specific ELISAs appear to be the most suitable for screening purposes, particularly when large patient collectives are to be tested. As reported earlier (5), immunoblotting and related techniques offer the highest specificity for the detection of HSV-2-specific antibodies, especially in the presence of high levels of cross-reactive antibodies, and therefore appear to be highly suitable as confirmatory assays. Accordingly, EuW showed the highest specificity (100%) of all commercial HSV-2-specific seroassays.
Due to the low number of equivocal results in the screening ELISAs, solely retesting sera with equivocal results in the screening assay by EuW had little or no effect on overall performance (confirmatory strategies 1 and 3) (Table 4). Confirmation by EuW of all positive and equivocal results obtained in a screening ELISA was found to increase significantly the PPVs and to reduce slightly the sensitivity of HSV-2-specific antibody detection (strategies 2 and 4) (Table 4). The additional costs of the latter two confirmatory strategies are the highest of all options evaluated (177.92% with Eu2 as the screening assay and 157.20% with Gu2 as the screening assay), because of the high number of immunoblots to be performed in the high-prevalence collective. Thus, confirmatory strategies involving a gG-2-based screening assay and a gG-2-based immunoblot will be most applicable in low-risk collectives where the number of additional immunoblots to be performed is low, e.g., 57.71 or 39.66% additional cost for Eu2 or Gu2 used as a screening assay, respectively, in a collective with a hypothetical 10% HSV-2 seroprevalence. The combination of two ELISAs for screening, either by testing all sera in parallel or by retesting all sera with positive or equivocal results in the first assay by a second screening assay and confirmation of discrepant results by a gG-2-based immunoblot, may be particularly suitable for achieving a reasonable sensitivity and specificity in a high-risk collective without the need for retesting a large number of sera by immunoblotting (strategies 5 and 6; additional costs, 129.39 and 79.02%, respectively) (Table 4). Although the latter strategy is associated with the least additional cost in a hypothetical low-prevalence collective (strategy 6; 29.35% additional cost per sample) (Table 4), it exhibits a PPV of 79.23%, which is significantly less than the 100% PPV of strategies 2 and 4. Thus, a slightly more expensive confirmatory approach (e.g., approximately 30% additional cost of strategy 6 versus 42% additional cost of strategy 4) may be justified by a considerable gain in PPV in low-prevalence collectives.
Since actual commercial HSV-2-specific seroassays are based exclusively on gG-2 as the diagnostic antigen, only in-house assays come into consideration for a gG-2-independent confirmation of the type-specific humoral immune response. As a gG-2-independent assay we developed an HSV-2 immunoblot combined with an additional preabsorption protocol for the removal of cross-reactive antibodies and control of the specificity of antibody reaction observed. By design, this assay should allow the detection of HSV-2-specific antibodies directed against viral proteins other than gG-2. Inclusion of the additionally positive samples identified by this assay to revise the PGS appeared to be justified with respect to (i) its good overall accordance with the PGS (150 of 157 sera tested; 95.54%) and (ii) the fact that five of six additionally positive samples were also positive by one or more type-specific commercial assays. The remaining sample positive in IhW but concordantly negative in all commercial assays did not contain HSV IgM antibodies, a marker of primary HSV-2 infection. This case may represent infection with a gG-2-negative HSV-2 strain (23). Only a single sample positive according to the PGS was negative in the IhW. Although this discrepancy could theoretically be due to an immune response to type-common epitopes on gG-2, recent studies strongly suggest that this is most probably only a hypothetical possibility (21, 24, 32), and we therefore considered this result a false-negative IhW result.
Based on the RGS, recalculation of the performances of the type-specific commercial assays and confirmatory strategies (Tables 3 and 4) indicated a slight loss in sensitivity of all commercial assays and confirmatory strategies, with the changes being most pronounced for EuW (98.9 to 92.78%). Correspondingly, all commercial HSV-2-specific ELISAs and all confirmatory strategies exhibited an increase in specificity. The slight specificity gains of the screening ELISAs and the loss of sensitivity of the EuW can be interpreted as a probable lack of sensitivity of the EuW in this context. The occurrence of false-negative results has therefore to be considered if both the screening assay and the confirmatory assay rely on gG-2 as the diagnostic antigen. It might therefore be expected that the use of assays like the IhW for confirmation would improve the sensitivity of confirmatory strategies. It should be noted, however, that half of the additional positive samples (three of six) would have already been missed at the screening stage.
In conclusion, our results show that contemporary gG-2-based commercial assays and confirmatory strategies based on them exhibit favorable diagnostic performances. Further improvements especially with regard to sensitivity seem possible but can probably be achieved only if antigens other than gG-2 are added to these tests.
Recommendations for potential confirmatory strategies may vary significantly with respect to the commercial assays employed and patient collectives analyzed. Therefore, further studies are needed which focus specifically on the evaluation of confirmatory strategies for type-specific HSV serology and their diagnostic benefit in various clinical and epidemiological settings.
Acknowledgments
We thank Elke Meier and Gisela Wehling for their excellent technical assistance. We are indebted to Waltraud Suer and Sandra Schmal for their support and to Jaqueline Gosink, Euroimmun, for proofreading the manuscript.
REFERENCES
- 1.Ashley, R. L., M. Eagleton, and N. Pfeiffer. 1999. Ability of a rapid serology test to detect seroconversion to herpes simplex virus type 2 glycoprotein G soon after infection. J. Clin. Microbiol. 37:1632-1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ashley, R. L., J. Militoni, F. Lee, A. Nahmias, and L. Corey. 1988. Comparison of Western blot (immunoblot) and glycoprotein G-specific immunodot enzyme assay for detecting antibodies to herpes simplex virus types 1 and 2 in human sera. J. Clin. Microbiol. 26:662-667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ashley, R. L., L. Wu, J. W. Pickering, M. C. Tu, and L. Schnorenberg. 1998. Premarket evaluation of a commercial glycoprotein G-based enzyme immunoassay for herpes simplex virus type-specific antibodies. J. Clin. Microbiol. 36:294-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benedetti, J. K., J. Zeh, and L. Corey. 1999. Clinical reactivation of genital herpes simplex virus infection decreases in frequency over time. Ann. Intern. Med. 131:14-20. [DOI] [PubMed] [Google Scholar]
- 5.Bergström, T., and E. Trybala. 1996. Antigenic differences between HSV-1 and HSV-2 glycoproteins and their importance for type-specific serology. Intervirology 39:176-184. [DOI] [PubMed] [Google Scholar]
- 6.Bernstein, D. I., M. A. Lovett, and Y. J. Bryson. 1984. The effects of acyclovir on antibody response to herpes simplex virus in primary genital herpetic infections. J. Infect. Dis. 150:7-13. [DOI] [PubMed] [Google Scholar]
- 7.Brugha, R., K. Keersmaekers, A. Renton, and A. Meheus. 1997. Genital herpes infection: a review. Int. J. Epidemiol. 26:698-709. [DOI] [PubMed] [Google Scholar]
- 8.Corey, L. 1994. The current trend in genital herpes. Progress in prevention. Sex. Transm. Dis. 21:S38-S44. [PubMed]
- 9.Corey, L., and H. H. Handsfield. 2000. Genital herpes and public health: addressing a global problem. JAMA 283:791-794. [DOI] [PubMed] [Google Scholar]
- 10.Eis-Hübinger, A. M., M. Daumer, B. Matz, and K. E. Schneweis. 1999. Evaluation of three glycoprotein G2-based enzyme immunoassays for detection of antibodies to herpes simplex virus type 2 in human sera. J. Clin. Microbiol. 37:1242-1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fleming, D. T., G. M. McQuillan, R. E. Johnson, A. J. Nahmias, S. O. Aral, F. K. Lee, and M. E. St. Louis. 1997. Herpes simplex virus type 2 in the United States, 1976 to 1994. N. Engl. J. Med. 337:1105-1111. [DOI] [PubMed] [Google Scholar]
- 12.Forsgren, M., E. Skoog, S. Jeansson, S. Olofsson, and J. Giesecke. 1994. Prevalence of antibodies to herpes simplex virus in pregnant women in Stockholm in 1969, 1983 and 1989: implications for STD epidemiology. Int. J. STD AIDS 5:113-116. [DOI] [PubMed] [Google Scholar]
- 13.Groen, J., G. van Dijk, H. G. Niesters, W. I. Van Der Meijden, and A. D. Osterhaus. 1998. Comparison of two enzyme-linked immunosorbent assays and one rapid immunoblot assay for detection of herpes simplex virus type 2-specific antibodies in serum. J. Clin. Microbiol. 36:845-847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Halioua, B., and J. E. Malkin. 1999. Epidemiology of genital herpes--recent advances. Eur. J. Dermatol. 9:177-184. [PubMed] [Google Scholar]
- 15.Ho, D. W., P. R. Field, W. L. Irving, D. R. Packham, and A. L. Cunningham. 1993. Detection of immunoglobulin M antibodies to glycoprotein G-2 by Western blot (immunoblot) for diagnosis of initial herpes simplex virus type 2 genital infections. J. Clin. Microbiol. 31:3157-3164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ho, D. W., P. R. Field, E. Sjogren-Jansson, S. Jeansson, and A. L. Cunningham. 1992. Indirect ELISA for the detection of HSV-2 specific IgG and IgM antibodies with glycoprotein G (gG-2). J. Virol. Methods 36:249-264. [DOI] [PubMed] [Google Scholar]
- 17.Janier, M., F. Lassau, J. Bloch, E. Spindler, P. Morel, P. Gerard, and A. Aufrere. 1999. Seroprevalence of herpes simplex virus type 2 antibodies in an STD clinic in Paris. Int. J. STD AIDS 10:522-526. [PubMed] [Google Scholar]
- 18.Kinghorn, G. R. 1994. Epidemiology of genital herpes. J. Int. Med. Res. 2(Suppl. 1):14A-23A. [PubMed]
- 19.Kühn, J. E., K. Klaffke, K. Munk, and R. W. Braun. 1990. HSV-1 gB and VZV gp-II crossreactive antibodies in human sera. Arch. Virol. 112:203-213. [DOI] [PubMed] [Google Scholar]
- 20.Lafferty, W. E., R. W. Coombs, J. Benedetti, C. Critchlow, and L. Corey. 1987. Recurrences after oral and genital herpes simplex virus infection. Influence of site of infection and viral type. N. Engl. J. Med. 316:1444-1449. [DOI] [PubMed] [Google Scholar]
- 21.Lee, F. K., R. M. Coleman, L. Pereira, P. D. Bailey, M. Tatsuno, and A. J. Nahmias. 1985. Detection of herpes simplex virus type 2-specific antibody with glycoprotein G. J. Clin. Microbiol. 22:641-644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee, F. K., L. Pereira, C. Griffin, E. Reid, and A. Nahmias. 1986. A novel glycoprotein for detection of herpes simplex virus type 1-specific antibodies. J. Virol. Methods 14:111-118. [DOI] [PubMed] [Google Scholar]
- 23.Liljeqvist, J. A., B. Svennerholm, and T. Bergström. 1999. Herpes simplex virus type 2 glycoprotein G-negative clinical isolates are generated by single frameshift mutations. J. Virol. 73:9796-9802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liljeqvist, J. A., E. Trybala, B. Svennerholm, S. Jeansson, E. Sjogren-Jansson, and T. Bergström. 1998. Localization of type-specific epitopes of herpes simplex virus type 2 glycoprotein G recognized by human and mouse antibodies. J. Gen. Virol. 79:1215-1224. [DOI] [PubMed] [Google Scholar]
- 25.McGeoch, D. J., H. W. Moss, D. McNab, and M. C. Frame. 1987. DNA sequence and genetic content of the HindIII l region in the short unique component of the herpes simplex virus type 2 genome: identification of the gene encoding glycoprotein G, and evolutionary comparisons. J. Gen. Virol. 68:19-38. [DOI] [PubMed] [Google Scholar]
- 26.Mertz, G. J., J. Benedetti, R. Ashley, S. A. Selke, and L. Corey. 1992. Risk factors for the sexual transmission of genital herpes. Ann. Intern. Med. 116:197-202. [DOI] [PubMed] [Google Scholar]
- 27.Mindel, A. 1996. Psychological and psychosexual implications of herpes simplex virus infections. Scand. J. Infect. Dis. Suppl. 100:27-32. [PubMed] [Google Scholar]
- 28.Nahmias, A. J., F. K. Lee, and S. Beckman-Nahmias. 1990. Sero-epidemiological and -sociological patterns of herpes simplex virus infection in the world. Scand. J. Infect. Dis. Suppl. 69:19-36. [PubMed] [Google Scholar]
- 29.Rekabdar, E., P. Tunback, J. A. Liljeqvist, and T. Bergström. 1999. Variability of the glycoprotein G gene in clinical isolates of herpes simplex virus type 1. Clin. Diagn. Lab. Immunol. 6:826-831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schieferstein, C. 1997. Type-specific herpes simplex virus antibodies: comparison of different ELISA systems and a Western blot. J. Lab. Med. 21:107-118. [Google Scholar]
- 31.Schmid, D. S., D. R. Brown, R. Nisenbaum, R. L. Burke, D. Alexander, R. Ashley, P. E. Pellett, and W. C. Reeves. 1999. Limits in reliability of glycoprotein G-based type-specific serologic assays for herpes simplex virus types 1 and 2. J. Clin. Microbiol. 37:376-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tunback, P., J. A. Liljeqvist, G. B. Lowhagen, and T. Bergstrom. 2000. Glycoprotein G of herpes simplex virus type 1: identification of type-specific epitopes by human antibodies. J. Gen. Virol. 81:1033-1040. [DOI] [PubMed] [Google Scholar]
- 33.Wald, A. 1999. New therapies and prevention strategies for genital herpes. Clin. Infect. Dis. 28(Suppl. 1):S4-S13. [DOI] [PubMed]
- 34.Wutzler, P., H. W. Doerr, I. Farber, U. Eichhorn, B. Helbig, A. Sauerbrei, A. Brandstadt, and H. F. Rabenau. 2000. Seroprevalence of herpes simplex virus type 1 and type 2 in selected German populations--relevance for the incidence of genital herpes. J. Med. Virol. 61:201-207. [DOI] [PubMed] [Google Scholar]