Abstract
A HeLa cell line continuously expressing recombinant nucleoprotein (rNP) of the Crimean-Congo hemorrhagic fever virus (CCHFV) was established by transfection with an expression vector containing the cDNA of CCHFV NP (pKS336-CCHFV-NP). These cells were used as antigens for indirect immunofluorescence (IF) to detect immunoglobulin G antibodies to CCHFV. The sensitivity and specificity of this IF technique were examined by using serum samples and were compared to those of the IF technique using CCHFV-infected Vero E6 cells (authentic antigen). Staining of the CCHFV rNP expressed in HeLa cells showed a unique granular pattern similar to that of CCHFV-infected Vero E6 cells. Positive staining could easily be distinguished from a negative result. All 13 serum samples determined to be positive by using the authentic antigen were also determined to be positive by using CCHFV rNP-expressing HeLa cells (recombinant antigen). The 108 serum samples determined to be negative by using the authentic antigen were also determined to be negative by using the recombinant antigen. Thus, both the sensitivity and the specificity of this IF technique were 100% compared to the IF with authentic antigen. The novel IF technique using CCHFV rNP-expressing HeLa cells can be used not only for diagnosis of CCHF but also for epidemiological studies on CCHFV infections.
Crimean-Congo hemorrhagic fever virus (CCHFV) is a member of the genus Nairovirus in the family Bunyaviridae and is the causative agent of a severe hemorrhagic fever known as Crimean-Congo hemorrhagic fever (CCHF). The mortality rate of CCHF is as high as 50% in humans (8). CCHFV is prevalent from Africa through to the western part of China, including Eastern European and Middle Eastern countries (9). CCHFV is a tick-borne virus, and wild and domestic animals including sheep, cattle, goats, and ostriches are the reservoirs for zoonoses (8). The virus can be transmitted to humans either by bites of ixodid ticks (genus Hyalomma) or by direct contact with blood and tissues from viremic livestock (6, 21, 22; J. F. Saluzzo, J. P. Digoutte, M. Cornet, D. Baudon, J. Roux, and V. Robert, Letter, Lancet i:1179, 1984). The ticks are reservoirs and vectors for livestock, wild animals, and humans. CCHFV can also be spread from CCHF patients to other persons, resulting in nosocomial outbreaks (2, 7, 20, 25). Outbreaks of CCHF among shepherds, agricultural workers, and abattoir workers have often been reported (11, 21); therefore, these occupations present a high risk of infection in areas of CCHF endemicity. Because of the high mortality rate of CCHF and the person-to-person transmission, early diagnosis of suspected cases and use of appropriate barrier measures by health care workers are necessary for the prevention of nosocomial infections.
A CCHF epidemic in the United Arab Emirates was reported to have been caused by CCHFV introduced from Somalia and Nigeria through imported livestock and ticks (17). Furthermore, it is possible that a traveler with CCHF could, during the virus's incubation period, visit areas previously known to be free of CCHF. Therefore, development of diagnostic methods for CCHFV infections is necessary even in countries hitherto free from outbreaks of CCHF.
Because of its virulence to humans, CCHFV should be handled in a high-containment laboratory. This restriction makes it difficult to prepare diagnostic methods using live CCHFV. In the present study, we developed an indirect immunofluorescence (IF) technique using HeLa cells stably expressing recombinant nucleoprotein (CCHFV rNP) to detect specific immunoglobulin G (IgG). This new IF technique is useful both for the diagnosis of CCHF and for seroepidemiological studies on CCHFV infections.
MATERIALS AND METHODS
Virus and cell lines.
CCHFV (Chinese strain 66019) isolated from a patient with CCHF in the western part of the Xinjiang Autonomous Region in 1966 (26) was used in this study. The S-segment RNA gene of strain 66019 has been deposited in GenBank under accession no. AJ010648. Vero E6 and HeLa 229 cell lines were purchased from the American Type Culture Collection and used. These cells were cultured in Dulbecco's minimum essential medium (DMEM; Life Technologies, Grand Island, N.Y.) containing 5% heat-inactivated fetal bovine serum and antibiotics such as penicillin and streptomycin (DMEM-5FBS).
Sera.
Twenty-five serum samples were collected from donors with or without a history of CCHF in the Xinjiang Autonomous Region (26), an area of CCHF endemicity in the People's Republic of China. Ninety-six serum samples collected from healthy Japanese adults were used as controls. Further, a monkey (Macaca fascicularis) was immunized with purified CCHFV rNP by using an adjuvant (Inject Alum; Pierce, Rockford, Ill.), and the serum was collected and used as a positive control. The monkey serum collected before the immunization was used as a negative control.
CCHFV NP expression vector.
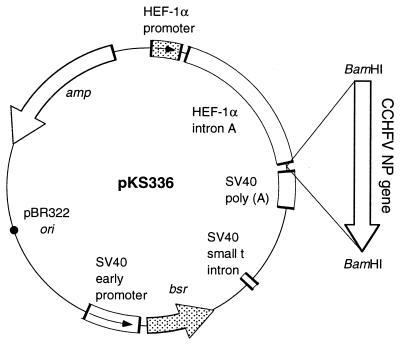
The pKS336 expression vector was constructed from the pSV2 bsr and pEF321 β-T plasmids (12, 13). A map of this vector is shown in Fig. 1. The nucleotide sequence of the vector is available in GenBank under accession no. AF403737. The blasticidin S deaminase (bsr) gene was under the control of the simian virus 40 early promoter. The DNA of interest was under the control of the human elongation factor-1α (HEF-1α) gene promoter.
FIG. 1.
Structure of pKS336-CCHFV-NP. The gene, a cDNA of the NP gene of CCHFV strain 8402, was inserted into the BamHI restriction site within the multicloning site.
The cDNA encoding the nucleoprotein (NP) was amplified by reverse transcription-PCR from the cDNA of the S segment of the Chinese CCHFV strain 8402 (accession no. AJ010649), with the designed primer set CCHF F/Bam (5"-GT GCT GGA TCC ATG GAG AAT AAA ATC-3") and CCHF R/Bam (5"-C GGA TCC TCA GAT GAT GTT GGC AC-3"), in order to add the BamHI restriction site (underlined) to both ends. PCR conditions were as follows: 5 cycles of denaturing at 94°C for 40 s, annealing at 40°C for 30 s, annealing at 50°C for 30 s, and extension at 72°C for 2 min; 15 cycles of denaturing at 94°C for 40 s, annealing at 55°C for 30 s, and extension at 72°C for 2 min; and an additional extension at 72°C for 5 min. The PCR product was purified, digested with BamHI, and subcloned into the BamHI site of the pKS336 vector (Fig. 1). The CCHFV NP gene inserted into pKS336 (pKS336-CCHFV-NP) was confirmed to be in the correct orientation to the promoter, sequenced by using appropriate primers with an ABI PRISM 310 Genetic Analyzer (Perkin-Elmer Applied Biosystems, Foster City, Calif.), and confirmed to be identical to the original sequence.
Transfection.
HeLa cells were transfected with pKS336-CCHFV-NP using the FuGENE 6 Transfection reagent (Roche Diagnostics, Mannheim, Germany) according to the manufacturer's instructions. The cells transfected with the plasmid were selected with 3 μg of blasticidin S-hydrochloride/ml in DMEM-5FBS. HeLa cell clones were analyzed for expression of CCHFV rNP by indirect IF using the monkey serum raised against CCHFV rNP. Cells expressing CCHFV rNP were subcloned and used as IF antigens.
Antigens.
Vero E6 cells either infected with CCHFV (strain 66019) or mock infected were cultured for 4 days. CCHFV-and mock-infected cells were then harvested by trypsinization and washed with phosphate-buffered saline (PBS). The cells were spotted onto 14-well HT-coated slide glasses (AR Brown Co., Ltd., Tokyo, Japan) and fixed with acetone at room temperature for 5 min. CCHFV antigen-negative slides were prepared as a negative control for IF antigen. IF antigen slides were stored at −70°C until use. These IF antigens (CCHFV slides) were used as the authentic CCHFV antigens. CCHFV slides were prepared according to the regulations of the Institute of Epidemiology and Microbiology, Chinese Academy of Preventive Medicine.
Recombinant IF antigens were prepared as follows. HeLa cells expressing CCHFV rNP were mixed with parent HeLa cells at a ratio of 1:3 and washed with PBS. The cells were then spotted onto 14-well slide glasses, air dried, and fixed with acetone at room temperature for 5 min. CCHFV rNP slides were stored at −70°C until use. Antigen-negative slides were prepared similarly by using HeLa cells and were used as the control antigen for the IF test. These IF slides were thawed and dried immediately prior to use.
IF test.
Human serum samples and monkey control serum samples were twofold serially diluted from 1:20 to 1:1,280 and placed on both CCHFV slides and CCHFV rNP slides. The slides were incubated under humidified conditions at 37°C for 1 h. After the slides were washed with PBS, the antigens on the slides were treated with fluorescein isothiocyanate (FITC)-conjugated goat anti-human IgG antibody (Zymed Laboratories, San Francisco, Calif.) at a dilution of 1:70. The FITC-conjugated anti-human IgG antibody was used not only for the human serum samples but also for the monkey control sera. After another wash with PBS, the slides were examined for staining patterns under a fluorescent microscope (Olympus, Tokyo, Japan) with an appropriate barrier and excitation filters for FITC visualization. CCHFV antibody-positive and -negative controls were included in each assay. The titers of tested samples were recorded as the reciprocals of the highest dilutions producing positive staining.
Statistical analysis.
The differences in the antibody titers determined by the IF techniques using authentic and recombinant antigens were compared by the Wilcoxon signed-rank test. The relationship between the antibody titers determined by these two methods was evaluated by Spearman's rank correlation coefficient.
RESULTS
Immunofluorescence of CCHFV rNP-expressing HeLa cells.
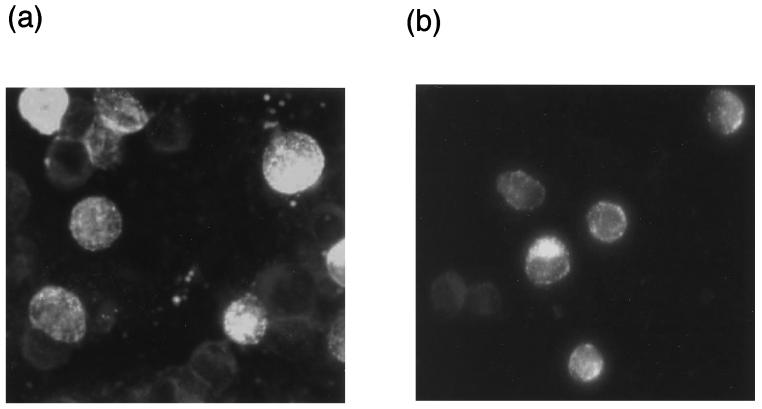
Positive-control monkey sera showed IF staining as a granular pattern, while negative-control sera showed no specific staining (data not shown). The antibody titers of the positive-control monkey serum determined by the IF techniques with recombinant and authentic antigens were both 160. Positive IF staining of CCHFV rNP antigens expressed in HeLa cells with a single CCHF patient serum sample is shown in Fig. 2a. CCHFV rNP was stained as granular aggregates (Fig. 2a), while control cells showed no staining (data not shown). The staining pattern of authentic virus antigens in Vero E6 cells with the same human serum sample was similar to that of CCHFV rNP in HeLa cells (Fig. 2b), while control cells failed to show any specific staining (data not shown).
FIG. 2.
Positive IF staining of CCHFV rNP-expressing HeLa cells (a) and CCHFV-infected Vero E6 cells (b) with a CCHF antibody-positive serum sample.
Sensitivity and specificity of IF staining of CCHFV rNP in human serum samples.
The sensitivity and specificity of the IF technique using CCHFV rNP slides were evaluated in comparison with those of the IF technique using authentic CCHFV antigens. Thirteen of 25 serum samples collected in an area of CCHF endemicity in the Xinjiang Autonomous Region showed a positive reaction to the IF technique using authentic CCHFV slides, while 12 serum samples showed a negative reaction. Ninety-six Japanese serum samples were also determined to be negative for CCHFV. All 13 serum samples determined to be CCHFV IgG antibody positive with authentic CCHFV slides also showed a positive reaction with CCHFV rNP slides. Furthermore, all 108 serum samples (comprising 12 Chinese and 96 Japanese samples) determined to be CCHFV IgG negative with the authentic CCHFV slides also showed a negative reaction with CCHFV rNP slides. These results indicate that both the sensitivity and the specificity of the IF technique using CCHFV rNP slides were 100%, compared to the IF technique using CCHFV slides.
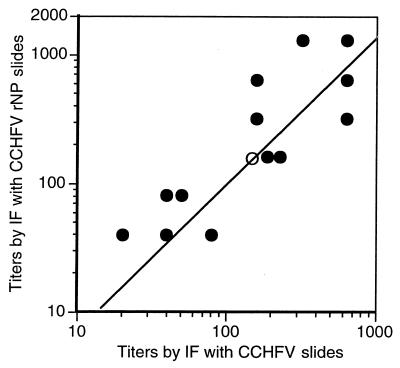
The titers determined by the IF technique with CCHFV rNP slides were positively correlated with those determined by the IF technique with authentic antigens (P < 0.01) (Fig. 3). The titers determined using CCHFV rNP slides were statistically significant at the same level as those determined using CCHFV slides (P = 0.07).
FIG. 3.
Relationship between the titers of IgG antibody to CCHFV determined by IF using CCHFV slides and those determined by IF using CCHFV rNP slides. Serum from the monkey, which was immunized with the purified CCHFV rNP, was also tested by IF using authentic and recombinant antigens. The titers of the positive-control monkey serum sample (○) and the 13 CCHFV antibody-positive human serum samples (•) were plotted. Each data point represents one serum sample.
DISCUSSION
We established a HeLa cell line continuously expressing CCHFV rNP by using a novel vector, pKS336. The cells expressed CCHFV rNP in the cytoplasm in granular aggregate form, which was indistinguishable from that of CCHFV-infected Vero E6 cells (Fig. 2). The IF technique using these CCHFV rNP-expressing cells was highly sensitive and specific for the detection of IgG antibodies to CCHFV.
CCHFV-infected cells, e.g., Vero cells, or mouse brain cells have been mainly used as antigens for the detection of IgG to CCHFV (1, 5, 10, 16, 24). In one study, a CCHFV rNP was used for the detection of IgG antibodies to CCHFV (15). The investigators used CCHFV rNP derived from a European strain of CCHFV (AP92; GenBank accession no. U04958) as an antigen for an enzyme-linked immunosorbent assay (ELISA) and proved that CCHFV rNP was efficacious in detecting CCHFV antibodies in the ELISA. The amino acid homology of CCHFV rNP from strain 8401 with that from strain AP92 was 91.9%. It was revealed that the antibodies to Dugbe and Hazara viruses, related nairoviruses, did not cross-react with CCHFV rNP in the ELISA (15). Therefore, CCHFV rNP in HeLa cells seemed not to cross-react with the antibodies to these viruses in IF, although further study is needed. The sensitivity and/or specificity of the ELISA using CCHFV rNP was not evaluated in that report (15). In this paper, we confirmed the efficacy of CCHFV rNP as an antigen and also clarified the sensitivity and specificity of the IF with CCHFV rNP in comparison to the IF with authentic CCHFV antigen in detecting specific CCHFV antibodies.
It has been reported that IgG antibodies to CCHFV can be detected within 9 days in all patients with CCHF (3). IgG antibodies to CCHFV were also demonstrated by the IF method within 8 days for two CCHF patients who were not treated with anti-CCHFV serum (19). The IgG and IgM antibodies to CCHFV were not detected in sera from patients with CCHF within the first 3 days from onset (3). Based on these results, we can diagnose a patient as having CCHF by detecting a significant rise in the titers of IgG antibody to CCHFV in serum samples obtained on the 9th day or later and within the first 3 days from onset. However, the IgG antibody response was weak or was not detected in fatal CCHF cases (3, 19). In this regard, antigen detection (14, 23), virus isolation, and reverse transcription-PCR (4, 17, 18) are also necessary for the rapid and accurate diagnosis of CCHF.
In summary, we established an efficacious IF technique using HeLa cells expressing CCHFV rNP for the diagnosis of CCHF and for seroepidemiological studies on CCHFV infections.
Acknowledgments
We thank M. Ogata, Department of Virology 1, National Institute of Infectious Diseases, and X. Zhao and X. Tao of the Second Division of Viral Hemorrhagic Fever, Institute of Epidemiology and Microbiology, Chinese Academy of Preventive Medicine, for technical assistance.
This work is supported by grants-in-aid from the Ministry of Health, Labor and Welfare of Japan, from the Japan Food Hygiene Association, Tokyo, Japan, and from the Japan Health Science Foundation.
REFERENCES
- 1.Al Tikiriti, S. K., F. K. Hassan, I. M. Moslih, F. Jurji, M. I. A. Mahmud, and H. H. Tantawi. 1981. Congo/Crimean haemorrhagic fever in Iraq: a seroepidemiological survey. J. Trop. Med. Hyg. 84:117-120. [PubMed] [Google Scholar]
- 2.Burney, M. I., A. Ghafoor, M. Saleen, P. A. Webb, and J. Casals. 1980. Nosocomial outbreak of viral hemorrhagic fever caused by Crimean hemorrhagic fever-Congo virus in Pakistan, January 1976. Am. J. Trop. Med. Hyg. 29:941-947. [DOI] [PubMed] [Google Scholar]
- 3.Burt, F. J., P. A. Leman, J. C. Abbott, and R. Swanepoel. 1994. Serodiagnosis of Crimean-Congo haemorrhagic fever. Epidemiol. Infect. 113:551-562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burt, F. J., P. A. Leman, J. F. Smith, and R. Swanepoel. 1998. The use of a reverse transcription-polymerase chain reaction for the detection of viral nucleic acid in the diagnosis of Crimean-Congo haemorrhagic fever. J. Virol. Methods 70:129-137. [DOI] [PubMed] [Google Scholar]
- 5.Burt, F. J., R. Swanepoel, and L. E. O. Braack. 1993. Enzyme-linked immunosorbent assays for the detection of antibody to Crimean-Congo haemorrhagic fever virus in the sera of livestock and wild vertebrates. Epidemiol. Infect. 111:547-557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chapman, L. E., M. L. Wilson, D. B. Hall, B. LeGuenno, E. A. Dykstra, K. Ba, and S. P. Fisher-Hoch. 1991. Risk factors for Crimean-Congo hemorrhagic fever in rural northern Senegal. J. Infect. Dis. 164:686-692. [DOI] [PubMed] [Google Scholar]
- 7.Fisher-Hoch, S. P., J. A. Khan, S. Rehman, S. Mirza, M. Khurshid, and J. B. McCormick. 1995. Crimean Congo-haemorrhagic fever treated with oral ribavirin. Lancet 346:472-475. [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez-Scarano, F., and N. Nathanson. 1996. Bunyaviridae, p. 1473-1504. In B. N. Fields, D. M. Knipe, and P. M. Howley (ed.), Fields virology, 3rd ed. Lippincott-Raven, Philadelphia, Pa.
- 9.Hoogstraal, H. 1979. The epidemiology of tick-borne Crimean-Congo hemorrhagic fever in Asia, Europe, and Africa. J. Med. Entomol. 15:307-417. [DOI] [PubMed] [Google Scholar]
- 10.Johnson, B. K., D. Ocheng, A. Gichogo, M. Okiro, D. Libondo, P. M. Tukei, M. Ho, M. Mugambi, G. L. Timms, and M. French. 1983. Antibodies against haemorrhagic fever viruses in Kenya populations. Trans. R. Soc. Trop. Med. Hyg. 77:731-733. [DOI] [PubMed] [Google Scholar]
- 11.Khan, A. S., G. O. Maupin, P. E. Rollin, A. M. Noor, H. H. Shurie, A. G. Shalabi, S. Wasef, Y. M. Haddad, R. Sadek, K. Ijaz, C. J. Peters, and T. G. Ksiazek. 1997. An outbreak of Crimean-Congo hemorrhagic fever in the United Arab Emirates, 1994-1995. Am. J. Trop. Med. Hyg. 57:519-525. [DOI] [PubMed] [Google Scholar]
- 12.Kim, D. W., T. Uetsuki, Y. Kaziro, N. Yamaguchi, and S. Sugano. 1990. Use of the human elongation factor 1α promoter as a versatile and efficient expression system. Gene 91:217-223. [DOI] [PubMed] [Google Scholar]
- 13.Kimura, M., A. Takatsuki, and I. Yamaguchi. 1994. Blasticidin S deaminase gene from Aspergillus terreus (BSD): a new drug resistance gene for transfection of mammalian cells. Biochim. Biophys. Acta 22:653-659. [DOI] [PubMed] [Google Scholar]
- 14.Logan, T. M., K. J. Linthicum, J. R. Moulton, and T. G. Ksiazek. 1993. Antigen-capture enzyme-linked immunosorbent assay for detection and quantification of Crimean-Congo hemorrhagic fever virus in the tick, Hyalomma truncatum. J. Virol. Methods 42:33-44. [DOI] [PubMed] [Google Scholar]
- 15.Marriott, A. C., T. Polyzoni, A. Antoniadis, and P. A. Nuttall. 1994. Detection of human antibodies to Crimean-Congo haemorrhagic fever virus using expressed viral nucleocapsid protein. J. Gen. Virol. 75:2157-2161. [DOI] [PubMed] [Google Scholar]
- 16.Morrill, J. C., A. K. Soliman, I. Z. Iman, B. A. M. Botros, M. I. Moussa, and D. M. Watts. 1990. Serological evidence of Crimean-Congo haemorrhagic fever viral infection among camels imported into Egypt. J. Trop. Med. Hyg. 93:201-204. [PubMed] [Google Scholar]
- 17.Rodriguez, L. L., G. O. Maupin, T. G. Ksiazek, P. E. Rollin, A. S. Khan, T. F. Schwarz, R. S. Lofts, J. F. Smith, A. M. Noor, C. J. Peters, and S. T. Nichol. 1997. Molecular investigation of a multisource outbreak of Crimean-Congo hemorrhagic fever in the United Arab Emirates. Am. J. Trop. Med. Hyg. 57:512-518. [DOI] [PubMed] [Google Scholar]
- 18.Schwarz, T. F., H. Nsanze, M. Longson, H. Nitschko, S. Gilch, H. Shurie, A. Ameen, A. R. M. Zahir, U. G. Acharya, and G. Jager. 1996. Polymerase chain reaction for diagnosis and identification of distant variants of Crimean-Congo hemorrhagic fever virus in the United Arab Emirates. Am. J. Trop. Med. Hyg. 55:190-196. [DOI] [PubMed] [Google Scholar]
- 19.Shepherd, A. J., R. Swanepoel, S. P. Shepherd, P. A. Leman, N. K. Blackburn, and A. F. Hallett. 1985. A nosocomial outbreak of Crimean-Congo haemorrhagic fever at Tygerberg Hospital. Part V. Virological and serological observations. S. Afr. Med. J. 68:733-776. [PubMed] [Google Scholar]
- 20.Suleiman, M. N., J. M. Muscat-Baron, J. R. Harries, A. G. Satti, G. S. Platt, E. T. Bowen, and D. I. Simpson. 1980. Congo/Crimean haemorrhagic fever in Dubai. An outbreak at the Rashid Hospital. Lancet ii:939-941. [PubMed]
- 21.Swanepoel, R., A. J. Shepherd, P. A. Leman, and S. P. Shepherd. 1985. A common-source outbreak of Crimean-Congo haemorrhagic fever on a dairy farm. S. Afr. Med. J. 68:635-637. [PubMed] [Google Scholar]
- 22.Swanepoel, R., A. J. Shepherd, P. A. Leman, and S. P. Shepherd. 1985. Investigations following initial recognition of Crimean-Congo haemorrhagic fever in South Africa and the diagnosis of 2 further cases. S. Afr. Med. J. 68:638-641. [PubMed] [Google Scholar]
- 23.Swanepoel, R., J. K. Struthers, and G. M. McGillivray. 1983. Reversed passive haemagglutination and inhibition with Rift Valley fever and Crimean-Congo hemorrhagic fever viruses. Am. J. Trop. Med. Hyg. 32:610-617. [DOI] [PubMed] [Google Scholar]
- 24.Swanepoel, R., J. K. Struthers, A. J. Shepherd, G. M. McGillivray, M. J. Nel, and P. G. Jupp. 1983. Crimean-Congo hemorrhagic fever in South Africa. Am. J. Trop. Med. Hyg. 32:1407-1415. [DOI] [PubMed] [Google Scholar]
- 25.van Eeden, P. J., J. R. Joubert, B. W. van de Wal, J. L. King, A. de Kock, and J. H. Groenewald. 1985. A nosocomial outbreak of viral hemorrhagic fever caused by Crimean-Congo haemorrhagic fever at Tygerberg Hospital. Part I. Clinical features. S. Afr. Med. J. 68:711-717. [PubMed] [Google Scholar]
- 26.Yen, Y. C., L. X. Kong, L. Lee, Y. Q. Zhang, F. Li, B. J. Cai, and S. Y. Gao. 1985. Characteristics of Crimean-Congo hemorrhagic fever virus (Xinjiang strain) in China. Am. J. Trop. Med. Hyg. 34:1179-1182. [PubMed] [Google Scholar]