Abstract
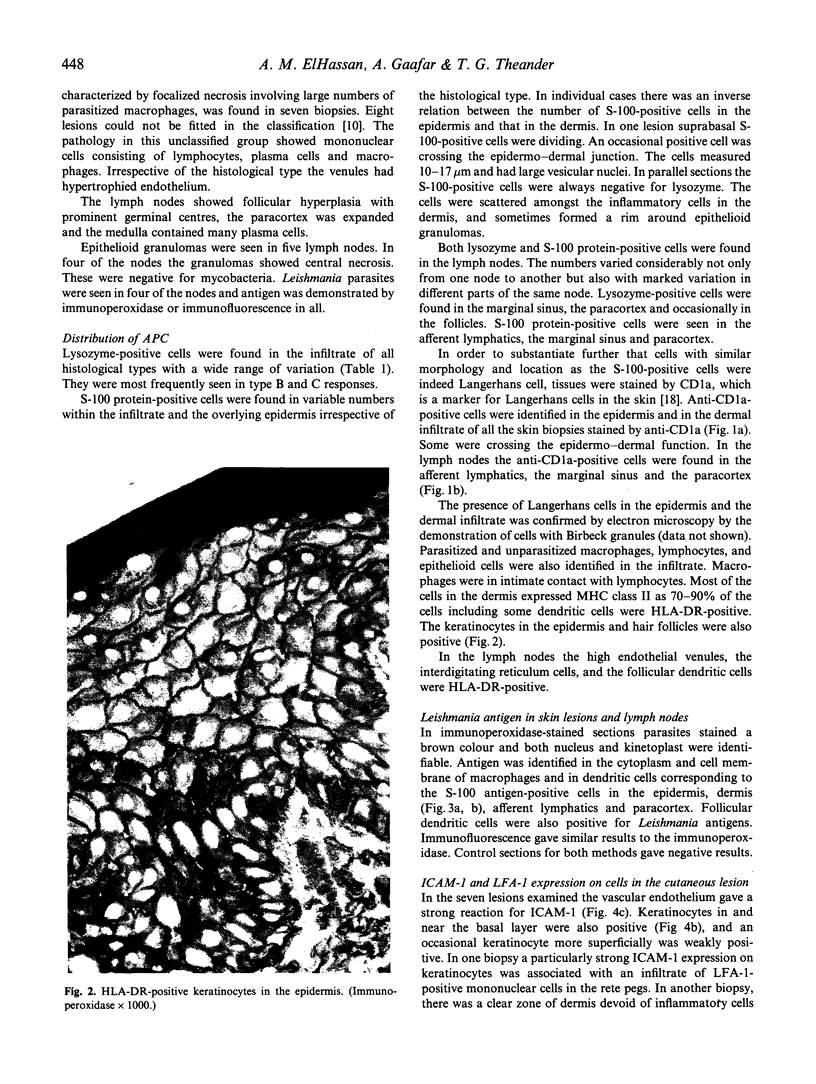
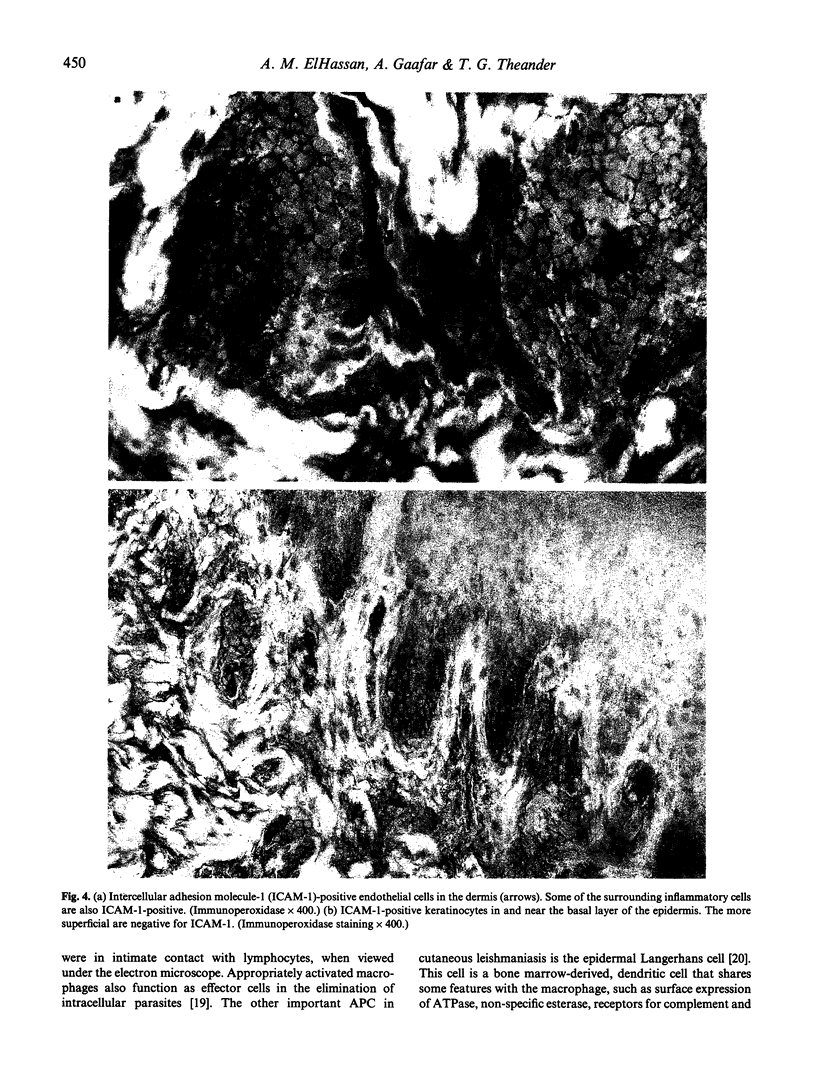
In this study biopsies from skin lesions and draining lymph nodes of patients suffering from cutaneous leishmaniasis caused by Leishmania major were examined by immunohistochemistry, and by light and electron microscopy to identify the types of antigen-presenting cells (APC) and their location. APC, identified morphologically and by their expression of specific cell markers, included Langerhans cells, macrophages, follicular dendritic cells, and interdigitating reticulum cells of the paracortex of lymph nodes. These cells expressed MHC class II antigens and contained Leishmania antigen. Since some keratinocytes and endothelial cells also showed these characteristics, they may also act as APC. By examining tissue samples from skin lesions and draining lymph nodes it was possible to follow the probable route of trafficking of various inflammatory cells between the skin lesion and lymph nodes. Leishmania antigen containing Langerhans cells were found in the epidermis, dermis and the regional lymph nodes. We believe these cells translocate from the epidermis to the dermis, where they take up antigen and migrate to the paracortex of the regional lymph nodes. There they are intimately associated with cells of the paracortex, and could be involved in the generation of Leishmania-specific T memory cells. LFA-1-positive T cells of the CD45RO phenotype were found in the skin lesion. Venular endothelium in the skin lesions expressed intercellular adhesion molecule-1 (ICAM-1), which is the ligand for LFA-1. The migration of lymphocytes from the vascular lumen to the site of inflammation is possibly a result of the interaction of these two adhesion molecules.
Full text
PDF






Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bjercke S., Elgø J., Braathen L., Thorsby E. Enriched epidermal Langerhans cells are potent antigen-presenting cells for T cells. J Invest Dermatol. 1984 Oct;83(4):286–289. doi: 10.1111/1523-1747.ep12340417. [DOI] [PubMed] [Google Scholar]
- Blank C., Fuchs H., Rappersberger K., Röllinghoff M., Moll H. Parasitism of epidermal Langerhans cells in experimental cutaneous leishmaniasis with Leishmania major. J Infect Dis. 1993 Feb;167(2):418–425. doi: 10.1093/infdis/167.2.418. [DOI] [PubMed] [Google Scholar]
- Coutinho S. G., Louis J. A., Mauel J., Engers H. D. Induction by specific T lymphocytes of intracellular destruction of Leishmania major in infected murine macrophages. Parasite Immunol. 1984 Mar;6(2):157–169. doi: 10.1111/j.1365-3024.1984.tb00789.x. [DOI] [PubMed] [Google Scholar]
- Csató M., Bozóky B., Hunyadi J., Dobozy A. Candida albicans phagocytosis by separated human epidermal cells. Arch Dermatol Res. 1986;279(2):136–139. doi: 10.1007/BF00417535. [DOI] [PubMed] [Google Scholar]
- Hsu S. M., Soban E. Color modification of diaminobenzidine (DAB) precipitation by metallic ions and its application for double immunohistochemistry. J Histochem Cytochem. 1982 Oct;30(10):1079–1082. doi: 10.1177/30.10.6182185. [DOI] [PubMed] [Google Scholar]
- Kadaro A. Y., Ghalib H. W., Ali M. S., Eltoum I., Ismail A., Gaafar A., Kemp M., Kordofani A. A., Reed S. G., el-Hassan A. M. Prevalence of cutaneous leishmaniasis along the Nile River north of Khartoum (Sudan) in the aftermath of an epidemic in 1985. Am J Trop Med Hyg. 1993 Jan;48(1):44–49. doi: 10.4269/ajtmh.1993.48.44. [DOI] [PubMed] [Google Scholar]
- Kemp M., Hey A. S., Kurtzhals J. A., Christensen C. B., Gaafar A., Mustafa M. D., Kordofani A. A., Ismail A., Kharazmi A., Theander T. G. Dichotomy of the human T cell response to Leishmania antigens. I. Th1-like response to Leishmania major promastigote antigens in individuals recovered from cutaneous leishmaniasis. Clin Exp Immunol. 1994 Jun;96(3):410–415. doi: 10.1111/j.1365-2249.1994.tb06043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moll H. Epidermal Langerhans cells are critical for immunoregulation of cutaneous leishmaniasis. Immunol Today. 1993 Aug;14(8):383–387. doi: 10.1016/0167-5699(93)90138-B. [DOI] [PubMed] [Google Scholar]
- Moll H., Fuchs H., Blank C., Röllinghoff M. Langerhans cells transport Leishmania major from the infected skin to the draining lymph node for presentation to antigen-specific T cells. Eur J Immunol. 1993 Jul;23(7):1595–1601. doi: 10.1002/eji.1830230730. [DOI] [PubMed] [Google Scholar]
- Mutis T., De Bueger M., Bakker A., Ottenhoff T. H. HLA class II+ human keratinocytes present Mycobacterium leprae antigens to CD4+ Th1-like cells. Scand J Immunol. 1993 Jan;37(1):43–51. doi: 10.1111/j.1365-3083.1993.tb01663.x. [DOI] [PubMed] [Google Scholar]
- Nacy C. A., Fortier A. H., Meltzer M. S., Buchmeier N. A., Schreiber R. D. Macrophage activation to kill Leishmania major: activation of macrophages for intracellular destruction of amastigotes can be induced by both recombinant interferon-gamma and non-interferon lymphokines. J Immunol. 1985 Nov;135(5):3505–3511. [PubMed] [Google Scholar]
- Nickoloff B. J., Turka L. A. Keratinocytes: key immunocytes of the integument. Am J Pathol. 1993 Aug;143(2):325–331. [PMC free article] [PubMed] [Google Scholar]
- Olsen W. M., Elgjo K. UVB-induced epidermal hyperproliferation is modified by a single, topical treatment with a mitosis inhibitory epidermal pentapeptide. J Invest Dermatol. 1990 Jan;94(1):101–106. doi: 10.1111/1523-1747.ep12873961. [DOI] [PubMed] [Google Scholar]
- Peters W., Elbihari S., Liu C., Le Blancq S. M., Evans D. A., Killick-Kendrick R., Smith V., Baldwin C. I. Leishmania infecting man and wild animals in Saudi Arabia. 1. General survey. Trans R Soc Trop Med Hyg. 1985;79(6):831–839. doi: 10.1016/0035-9203(85)90130-0. [DOI] [PubMed] [Google Scholar]
- Pober J. S., Gimbrone M. A., Jr, Lapierre L. A., Mendrick D. L., Fiers W., Rothlein R., Springer T. A. Overlapping patterns of activation of human endothelial cells by interleukin 1, tumor necrosis factor, and immune interferon. J Immunol. 1986 Sep 15;137(6):1893–1896. [PubMed] [Google Scholar]
- Ridel P. R., Esterre P., Dedet J. P., Pradinaud R., Santoro F., Capron A. Killer cells in human cutaneous leishmaniasis. Trans R Soc Trop Med Hyg. 1988;82(2):223–226. doi: 10.1016/0035-9203(88)90419-1. [DOI] [PubMed] [Google Scholar]
- Ridley D. S. A histological classification of cutaneous leishmaniasis and its geographical expression. Trans R Soc Trop Med Hyg. 1980;74(4):515–521. doi: 10.1016/0035-9203(80)90069-3. [DOI] [PubMed] [Google Scholar]
- Ridley M. J., Ridley D. S. Cutaneous leishmaniasis: immune complex formation and necrosis in the acute phase. Br J Exp Pathol. 1984 Jun;65(3):327–336. [PMC free article] [PubMed] [Google Scholar]
- Sells P. G., Burton M. Identification of Leishmania amastigotes and their antigens in formalin fixed tissue by immunoperoxidase staining. Trans R Soc Trop Med Hyg. 1981;75(3):461–468. doi: 10.1016/0035-9203(81)90121-8. [DOI] [PubMed] [Google Scholar]
- Springer T. A. Adhesion receptors of the immune system. Nature. 1990 Aug 2;346(6283):425–434. doi: 10.1038/346425a0. [DOI] [PubMed] [Google Scholar]
- Teunissen M. B. Dynamic nature and function of epidermal Langerhans cells in vivo and in vitro: a review, with emphasis on human Langerhans cells. Histochem J. 1992 Oct;24(10):697–716. doi: 10.1007/BF01460823. [DOI] [PubMed] [Google Scholar]
- Van Voorhis W. C., Kaplan G., Sarno E. N., Horwitz M. A., Steinman R. M., Levis W. R., Nogueira N., Hair L. S., Gattass C. R., Arrick B. A. The cutaneous infiltrates of leprosy: cellular characteristics and the predominant T-cell phenotypes. N Engl J Med. 1982 Dec 23;307(26):1593–1597. doi: 10.1056/NEJM198212233072601. [DOI] [PubMed] [Google Scholar]
- Veress B., el Hassan A. M. Immunohistochemical demonstration of S-100 protein antigen-containing cells in chronic cutaneous leishmaniasis. Acta Pathol Microbiol Immunol Scand A. 1985 Nov;93(6):331–334. doi: 10.1111/j.1699-0463.1985.tb03959.x. [DOI] [PubMed] [Google Scholar]
- Wawryk S. O., Novotny J. R., Wicks I. P., Wilkinson D., Maher D., Salvaris E., Welch K., Fecondo J., Boyd A. W. The role of the LFA-1/ICAM-1 interaction in human leukocyte homing and adhesion. Immunol Rev. 1989 Apr;108:135–161. doi: 10.1111/j.1600-065x.1989.tb00016.x. [DOI] [PubMed] [Google Scholar]
- Wood G. S., Warner N. L., Warnke R. A. Anti-Leu-3/T4 antibodies react with cells of monocyte/macrophage and Langerhans lineage. J Immunol. 1983 Jul;131(1):212–216. [PubMed] [Google Scholar]
- el Hassan A. M., Veress B., Kutty M. K. The ultrastructural morphology of human cutaneous leishmaniasis of low parasite load. Acta Derm Venereol. 1984;64(6):501–505. [PubMed] [Google Scholar]
- el-Safi S. H., Peters W. Studies on the leishmaniases in the Sudan. 1. Epidemic of cutaneous leishmaniasis in Khartoum. Trans R Soc Trop Med Hyg. 1991 Jan-Feb;85(1):44–47. doi: 10.1016/0035-9203(91)90151-n. [DOI] [PubMed] [Google Scholar]
- el-Safi S. H., Peters W., el-Toam B., el-Kadarow A., Evans D. A. Studies on the leishmaniases in the Sudan. 2. Clinical and parasitological studies on cutaneous leishmaniasis. Trans R Soc Trop Med Hyg. 1991 Jul-Aug;85(4):457–464. doi: 10.1016/0035-9203(91)90218-n. [DOI] [PubMed] [Google Scholar]