Abstract
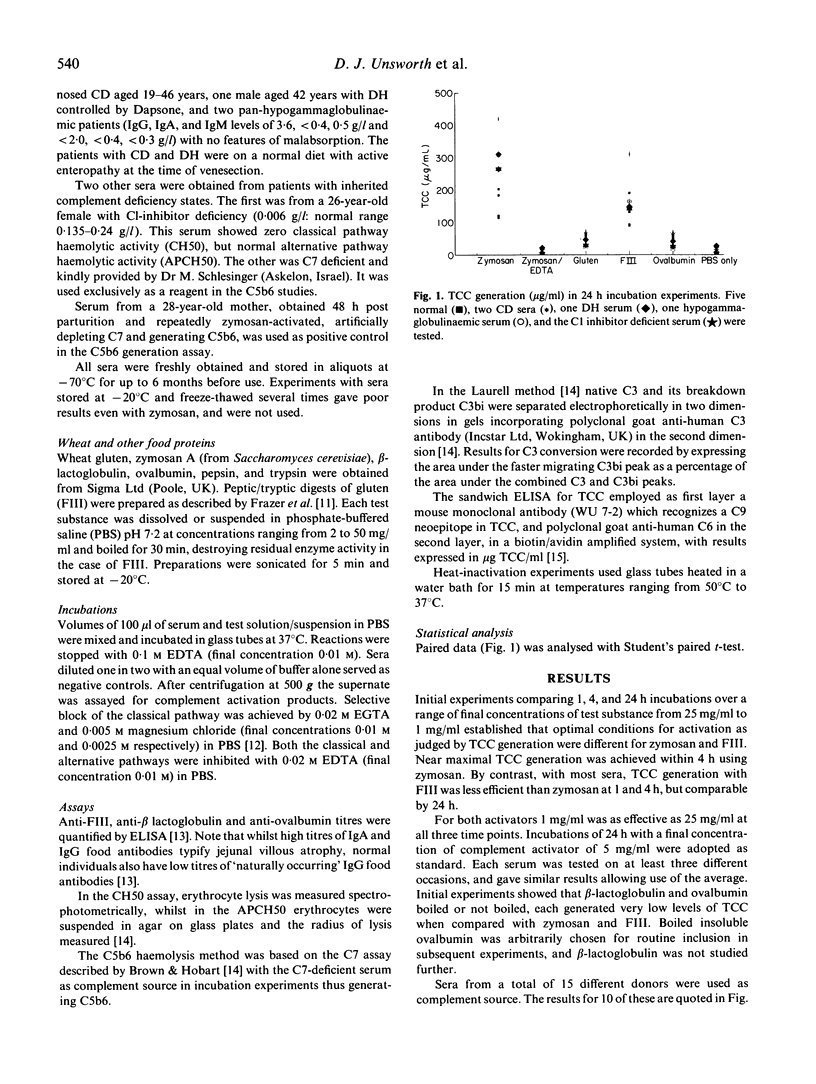
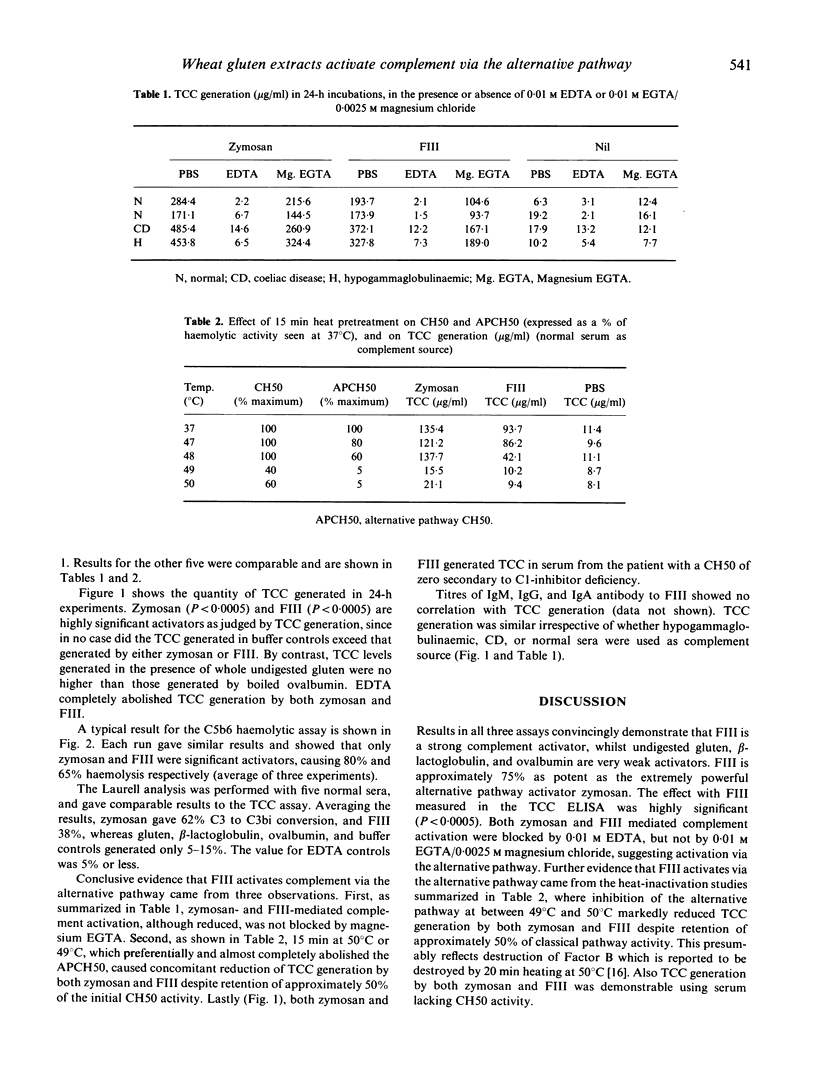
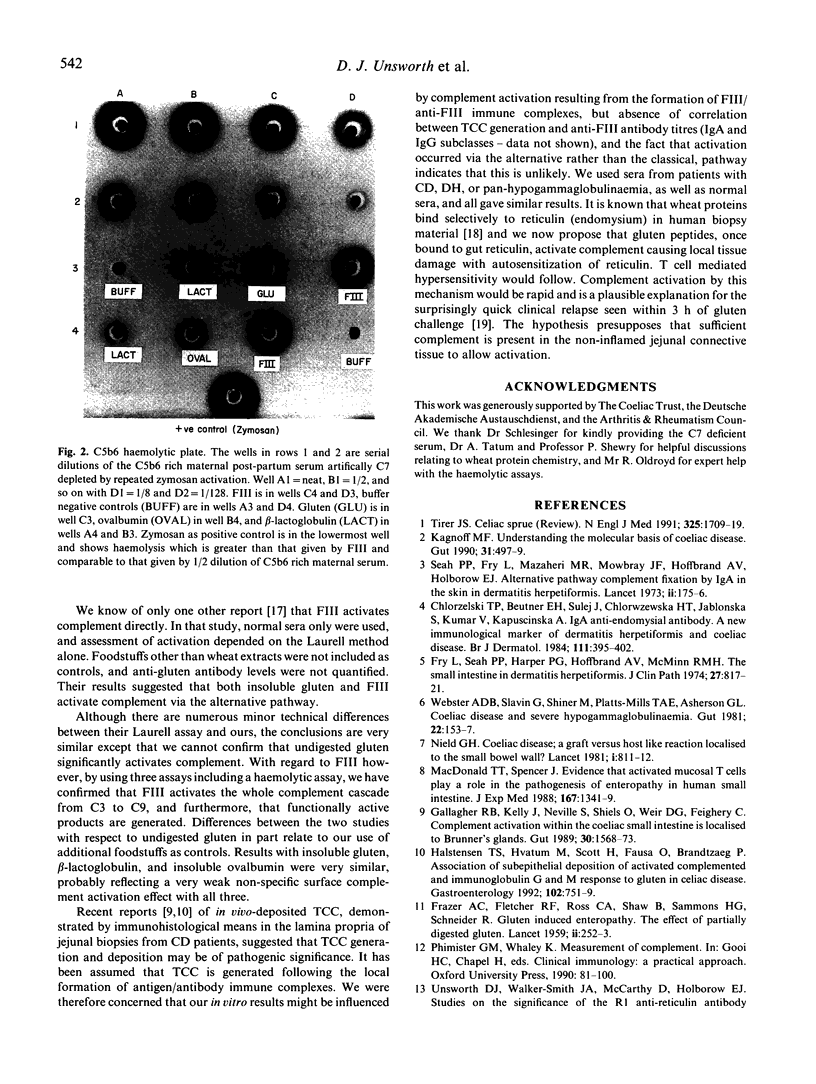
We studied the ability of wheat gluten and its subfractions to activate complement directly. A sensitive sandwich ELISA employing a monoclonal antibody (MoAb) to a C9 neoepitope exposed in the terminal complement complex (TCC), a functional haemolytic assay for C5b6 generation, and Laurell's electrophoretic method of estimating C3 conversion to C3bi were used. On a weight-for-weight basis, enzyme solubilized Frazer's fraction three of gluten (FIII) produced approximately 75% of the complement activation seen with the potent activator zymosan. By contrast, activation with whole insoluble undigested gluten was very weak and similar to that seen with ovalbumin or beta-lactoglobulin. The results were the same using normal human serum or sera from patients with coeliac disease, dermatitis herpetiformis, or hypogammaglobulinaemia as the complement source. Activation by both zymosan and FIII was blocked in 0.01 M EDTA, but not in 0.01 M EGTA with 0.0025 M magnesium chloride. Zymosan and FIII activated complement in a serum from a patient with an intact alternative pathway but classical pathway haemolytic activity (CH50) of zero. Preferential heat inactivation of the alternative pathway inhibited both zymosan- and FIII-induced activation. Our results confirm that FIII is a strong activator of the alternative pathway. We discuss how gluten enteropathy might be initiated by complement.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chorzelski T. P., Beutner E. H., Sulej J., Tchorzewska H., Jablonska S., Kumar V., Kapuscinska A. IgA anti-endomysium antibody. A new immunological marker of dermatitis herpetiformis and coeliac disease. Br J Dermatol. 1984 Oct;111(4):395–402. doi: 10.1111/j.1365-2133.1984.tb06601.x. [DOI] [PubMed] [Google Scholar]
- Ciclitira P. J., Evans D. J., Fagg N. L., Lennox E. S., Dowling R. H. Clinical testing of gliadin fractions in coeliac patients. Clin Sci (Lond) 1984 Mar;66(3):357–364. doi: 10.1042/cs0660357. [DOI] [PubMed] [Google Scholar]
- FRAZER A. C., FLETCHER R. F., ROSS C. A., SHAW B., SAMMONS H. G., SCHNEIDER R. Gluten-induced enteropathy: the effect of partially digested gluten. Lancet. 1959 Sep 5;2(7097):252–255. doi: 10.1016/s0140-6736(59)92051-3. [DOI] [PubMed] [Google Scholar]
- Fry L., Seah P. P., Harper P. G., Hoffbrand A. V., McMinn R. M. The small intestine in dermatitis herpetiformis. J Clin Pathol. 1974 Oct;27(10):817–824. doi: 10.1136/jcp.27.10.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher R. B., Kelly C. P., Neville S., Sheils O., Weir D. G., Feighery C. F. Complement activation within the coeliac small intestine is localised to Brunner's glands. Gut. 1989 Nov;30(11):1568–1573. doi: 10.1136/gut.30.11.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halstensen T. S., Hvatum M., Scott H., Fausa O., Brandtzaeg P. Association of subepithelial deposition of activated complement and immunoglobulin G and M response to gluten in celiac disease. Gastroenterology. 1992 Mar;102(3):751–759. doi: 10.1016/0016-5085(92)90155-r. [DOI] [PubMed] [Google Scholar]
- Kagnoff M. F. Understanding the molecular basis of coeliac disease. Gut. 1990 May;31(5):497–499. doi: 10.1136/gut.31.5.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald T. T., Spencer J. Evidence that activated mucosal T cells play a role in the pathogenesis of enteropathy in human small intestine. J Exp Med. 1988 Apr 1;167(4):1341–1349. doi: 10.1084/jem.167.4.1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey A., Capner P. M., Mowbray J. F. Activation of the alternative pathway by gluten. A possible aetiological factor in dermatitis herpetiformis. Immunology. 1977 Sep;33(3):339–342. [PMC free article] [PubMed] [Google Scholar]
- Neild G. H. Coeliac disease: a graft-versus-host-like reaction localised to the small bowel wall? Lancet. 1981 Apr 11;1(8224):811–812. doi: 10.1016/s0140-6736(81)92683-0. [DOI] [PubMed] [Google Scholar]
- Seah P. P., Fry L., Mazaheri M. R., Mowbray J. F., Hoffbrand A. V., Holborow E. J. Alternate-pathway complement fixation by IgA in the skin in dermatitis herpetiformis. Lancet. 1973 Jul;2(7822):175–177. doi: 10.1016/s0140-6736(73)93006-7. [DOI] [PubMed] [Google Scholar]
- Trier J. S. Celiac sprue. N Engl J Med. 1991 Dec 12;325(24):1709–1719. doi: 10.1056/NEJM199112123252406. [DOI] [PubMed] [Google Scholar]
- Unsworth D. J., Johnson G. D., Haffenden G., Fry L., Holborow E. J. Binding of wheat gliadin in vitro to reticulum in normal and dermatitis herpetiformis skin. J Invest Dermatol. 1981 Feb;76(2):88–93. doi: 10.1111/1523-1747.ep12525376. [DOI] [PubMed] [Google Scholar]
- Unsworth D. J., Walker-Smith J. A., McCarthy D., Holborow E. J. Studies on the significance of the R1 anti-reticulin antibody associated with gluten sensitivity. Int Arch Allergy Appl Immunol. 1985;76(1):47–51. doi: 10.1159/000233660. [DOI] [PubMed] [Google Scholar]
- Webster A. D., Slavin G., Shiner M., Platts-Mills T. A., Asherson G. L. Coeliac disease with severe hypogammaglobulinaemia. Gut. 1981 Feb;22(2):153–157. doi: 10.1136/gut.22.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Würzner R., Schulze M., Happe L., Franzke A., Bieber F. A., Oppermann M., Götze O. Inhibition of terminal complement complex formation and cell lysis by monoclonal antibodies. Complement Inflamm. 1991;8(5-6):328–340. doi: 10.1159/000463204. [DOI] [PubMed] [Google Scholar]