Abstract
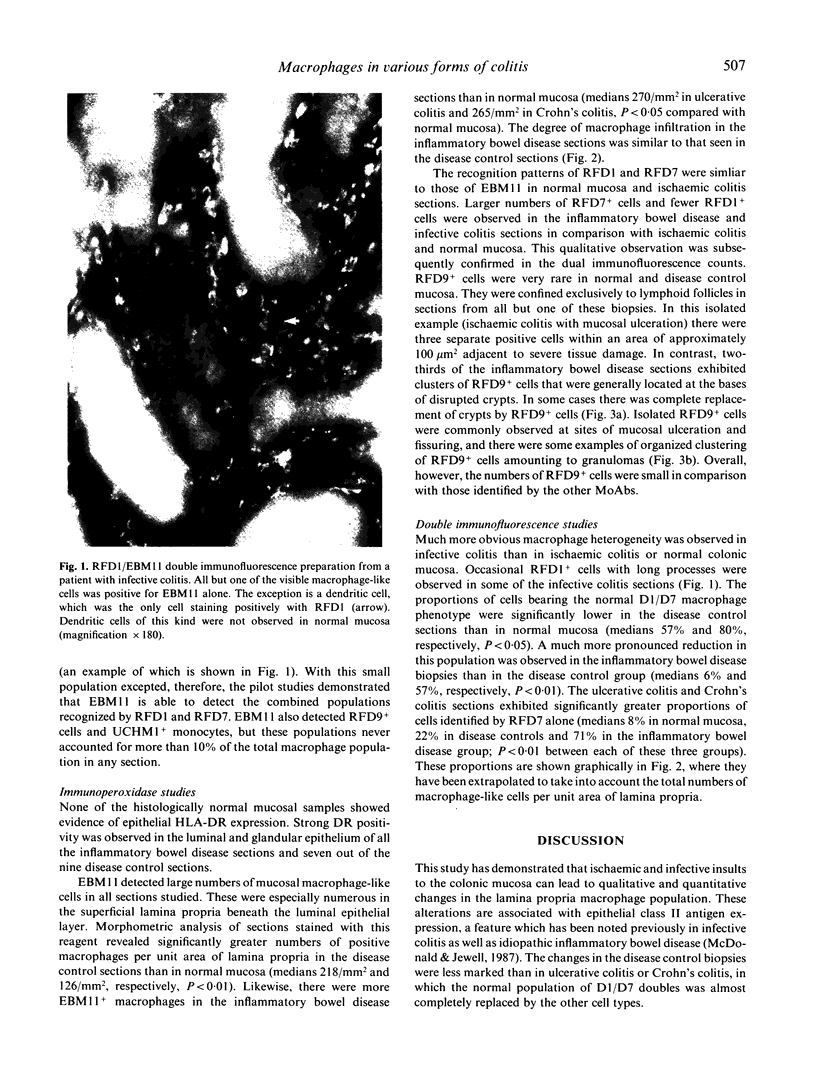
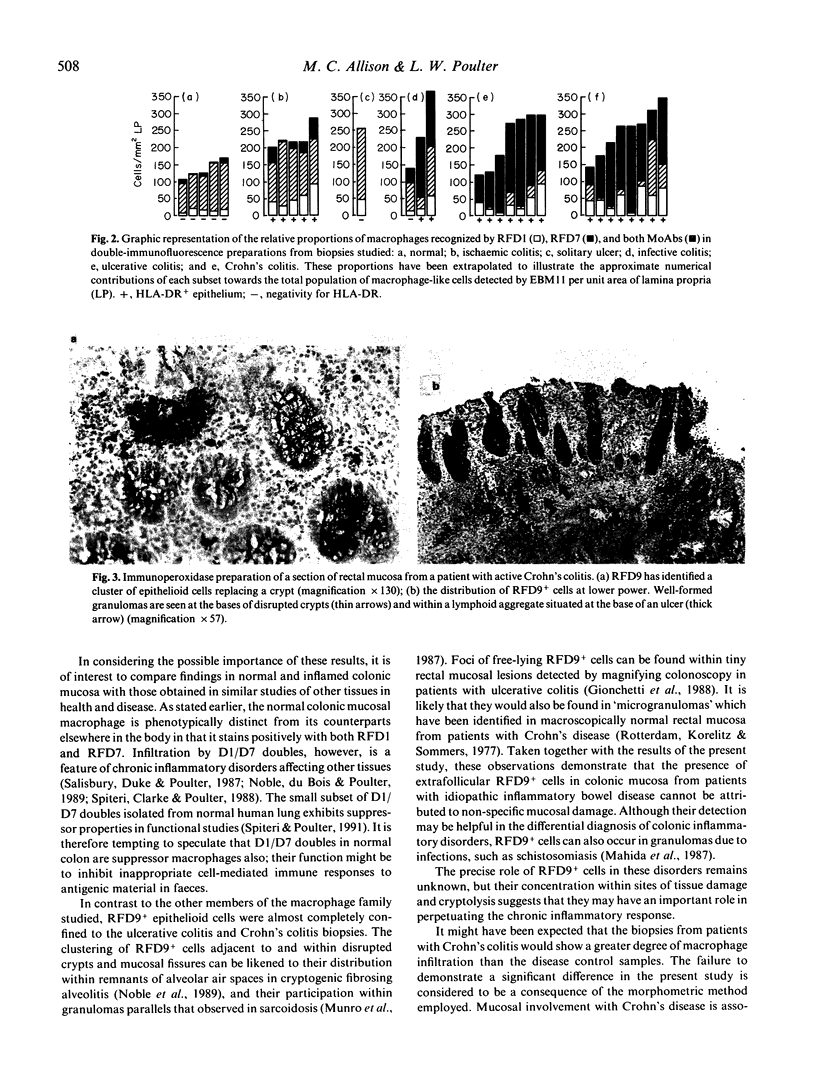
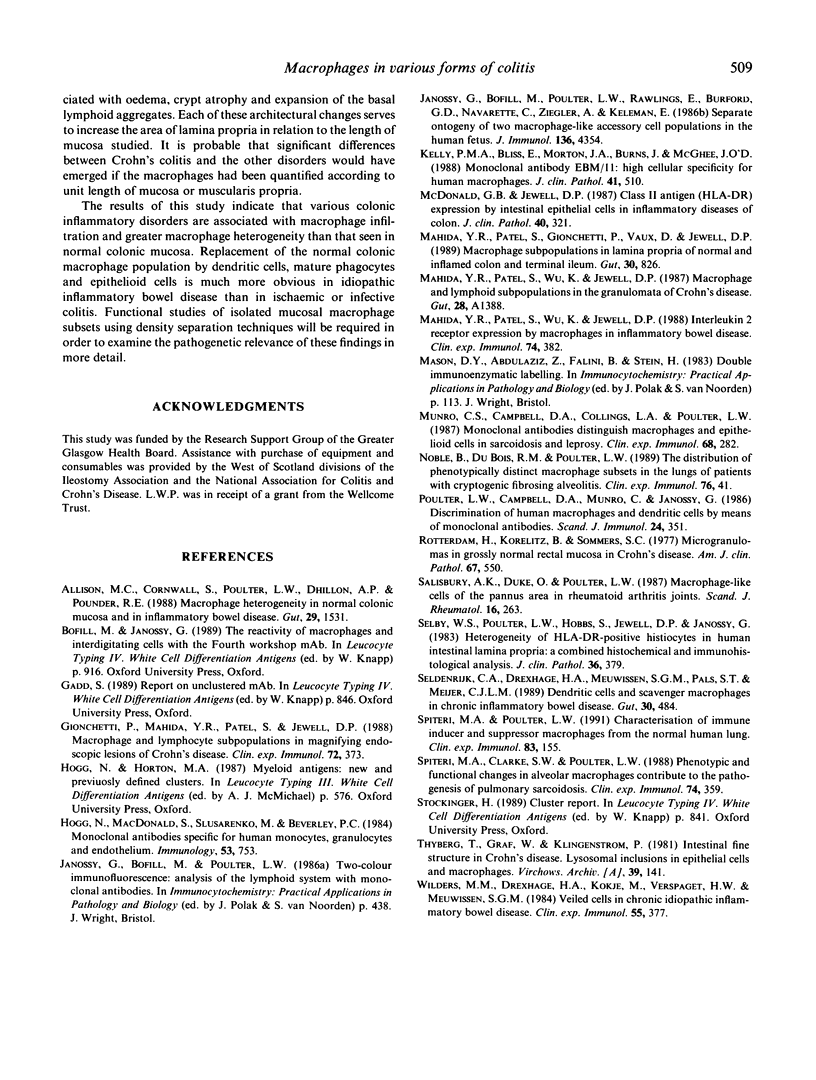
Previous studies have demonstrated the presence of much more marked macrophage heterogeneity in colonic mucosa affected by the idiopathic inflammatory bowel diseases (ulcerative colitis and Crohn's disease) than in normal mucosa. This study examines the morphology, distribution and phenotypic expression of mucosal macrophage-like cells in biopsies from patients with idiopathic inflammatory bowel disease in comparison with disease control samples from patients with colonic infection or ischaemia. Approximately 80% of macrophage-like cells in histologically normal mucosa co-express the antigens recognized by the monoclonal antibodies RFD1 (an interdigitating cell marker) and RFD7 (a marker for mature tissue macrophages). In idiopathic inflammatory bowel disease, the normal colonic macrophage population is partly replaced by cells staining positively with RFD7 alone, and, to a lesser extent, with RFD1+ dendritic cells. Sections from patients with infections and ischaemia exhibited epithelial HLA-DR positivity and infiltration of the lamina propria by a more heterogeneous population of macrophages than that seen in histologically normal mucosa. However, the displacement of the normal colonic macrophage phenotype by RFD7+ tissue macrophages occurred to a significantly greater extent in idiopathic inflammatory bowel disease than in disease control mucosa. A pathognomonic feature of the ulcerative colitis and Crohn's colitis sections was the clustering of RFD9+ epithelioid cells at the bases of disrupted crypts and adjacent to areas of mucosal damage. It is concluded that a degree of macrophage heterogeneity and macrophage infiltration can occur as a non-specific response to colonic mucosal damage. The distinctive feature of idiopathic inflammatory bowel disease mucosa is the almost complete replacement of the normal colonic mucosal macrophage population by tissue macrophages and epithelioid cells, and this phenomenon may be important in promoting the development of a chronic inflammatory state.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allison M. C., Cornwall S., Poulter L. W., Dhillon A. P., Pounder R. E. Macrophage heterogeneity in normal colonic mucosa and in inflammatory bowel disease. Gut. 1988 Nov;29(11):1531–1538. doi: 10.1136/gut.29.11.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gionchetti P., Mahida Y. R., Patel S., Jewell D. P. Macrophage and lymphocyte subpopulations in magnifying endoscopic lesions of Crohn's disease. Clin Exp Immunol. 1988 Jun;72(3):373–376. [PMC free article] [PubMed] [Google Scholar]
- Hogg N., MacDonald S., Slusarenko M., Beverley P. C. Monoclonal antibodies specific for human monocytes, granulocytes and endothelium. Immunology. 1984 Dec;53(4):753–767. [PMC free article] [PubMed] [Google Scholar]
- Janossy G., Bofill M., Poulter L. W., Rawlings E., Burford G. D., Navarrete C., Ziegler A., Kelemen E. Separate ontogeny of two macrophage-like accessory cell populations in the human fetus. J Immunol. 1986 Jun 15;136(12):4354–4361. [PubMed] [Google Scholar]
- Kelly P. M., Bliss E., Morton J. A., Burns J., McGee J. O. Monoclonal antibody EBM/11: high cellular specificity for human macrophages. J Clin Pathol. 1988 May;41(5):510–515. doi: 10.1136/jcp.41.5.510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahida Y. R., Patel S., Gionchetti P., Vaux D., Jewell D. P. Macrophage subpopulations in lamina propria of normal and inflamed colon and terminal ileum. Gut. 1989 Jun;30(6):826–834. doi: 10.1136/gut.30.6.826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahida Y. R., Patel S., Wu K., Jewell D. P. Interleukin 2 receptor expression by macrophages in inflammatory bowel disease. Clin Exp Immunol. 1988 Dec;74(3):382–386. [PMC free article] [PubMed] [Google Scholar]
- Munro C. S., Campbell D. A., Collings L. A., Poulter L. W. Monoclonal antibodies distinguish macrophages and epithelioid cells in sarcoidosis and leprosy. Clin Exp Immunol. 1987 May;68(2):282–287. [PMC free article] [PubMed] [Google Scholar]
- Noble B., Du Bois R. M., Poulter L. W. The distribution of phenotypically distinct macrophage subsets in the lungs of patients with cryptogenic fibrosing alveolitis. Clin Exp Immunol. 1989 Apr;76(1):41–46. [PMC free article] [PubMed] [Google Scholar]
- Poulter L. W., Campbell D. A., Munro C., Janossy G. Discrimination of human macrophages and dendritic cells by means of monoclonal antibodies. Scand J Immunol. 1986 Sep;24(3):351–357. doi: 10.1111/j.1365-3083.1986.tb02104.x. [DOI] [PubMed] [Google Scholar]
- Rotterdam H., Korelitz B. I., Sommers S. C. Microgranulomas in grossly normal rectal mucosa in Crohn's disease. Am J Clin Pathol. 1977 Jun;67(6):550–554. doi: 10.1093/ajcp/67.6.550. [DOI] [PubMed] [Google Scholar]
- Salisbury A. K., Duke O., Poulter L. W. Macrophage-like cells of the pannus area in rheumatoid arthritic joints. Scand J Rheumatol. 1987;16(4):263–272. doi: 10.3109/03009748709102927. [DOI] [PubMed] [Google Scholar]
- Selby W. S., Poulter L. W., Hobbs S., Jewell D. P., Janossy G. Heterogeneity of HLA-DR-positive histiocytes in human intestinal lamina propria: a combined histochemical and immunohistological analysis. J Clin Pathol. 1983 Apr;36(4):379–384. doi: 10.1136/jcp.36.4.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seldenrijk C. A., Drexhage H. A., Meuwissen S. G., Pals S. T., Meijer C. J. Dendritic cells and scavenger macrophages in chronic inflammatory bowel disease. Gut. 1989 Apr;30(4):484–491. doi: 10.1136/gut.30.4.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiteri M. A., Clarke S. W., Poulter L. W. Phenotypic and functional changes in alveolar macrophages contribute to the pathogenesis of pulmonary sarcoidosis. Clin Exp Immunol. 1988 Dec;74(3):359–364. [PMC free article] [PubMed] [Google Scholar]
- Thyberg J., Graf W., Klingenström P. Intestinal fine structure in Crohn's disease. Lysosomal inclusions in epithelial cells and macrophages. Virchows Arch A Pathol Anat Histol. 1981;391(2):141–152. doi: 10.1007/BF00437592. [DOI] [PubMed] [Google Scholar]
- Wilders M. M., Drexhage H. A., Kokjé M., Verspaget H. W., Meuwissen S. G. Veiled cells in chronic idiopathic inflammatory bowel disease. Clin Exp Immunol. 1984 Feb;55(2):377–387. [PMC free article] [PubMed] [Google Scholar]