Abstract
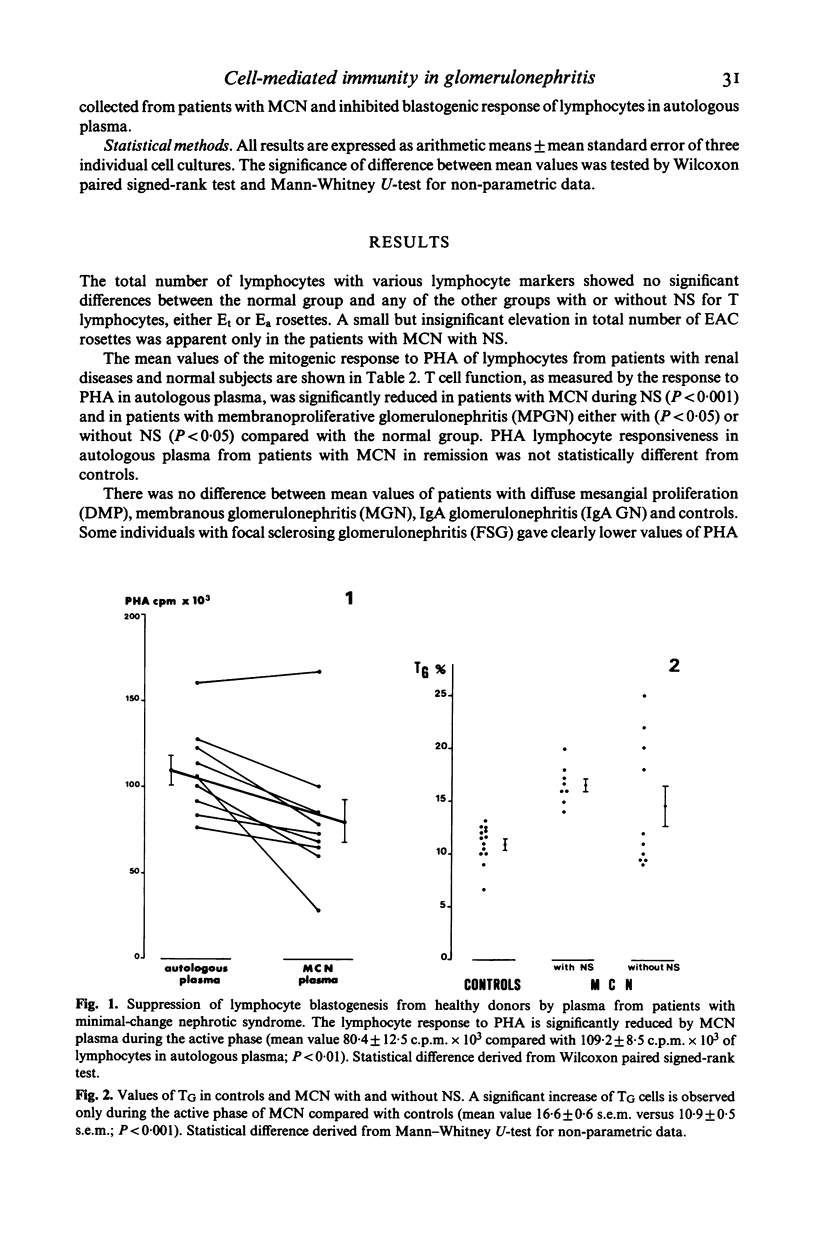
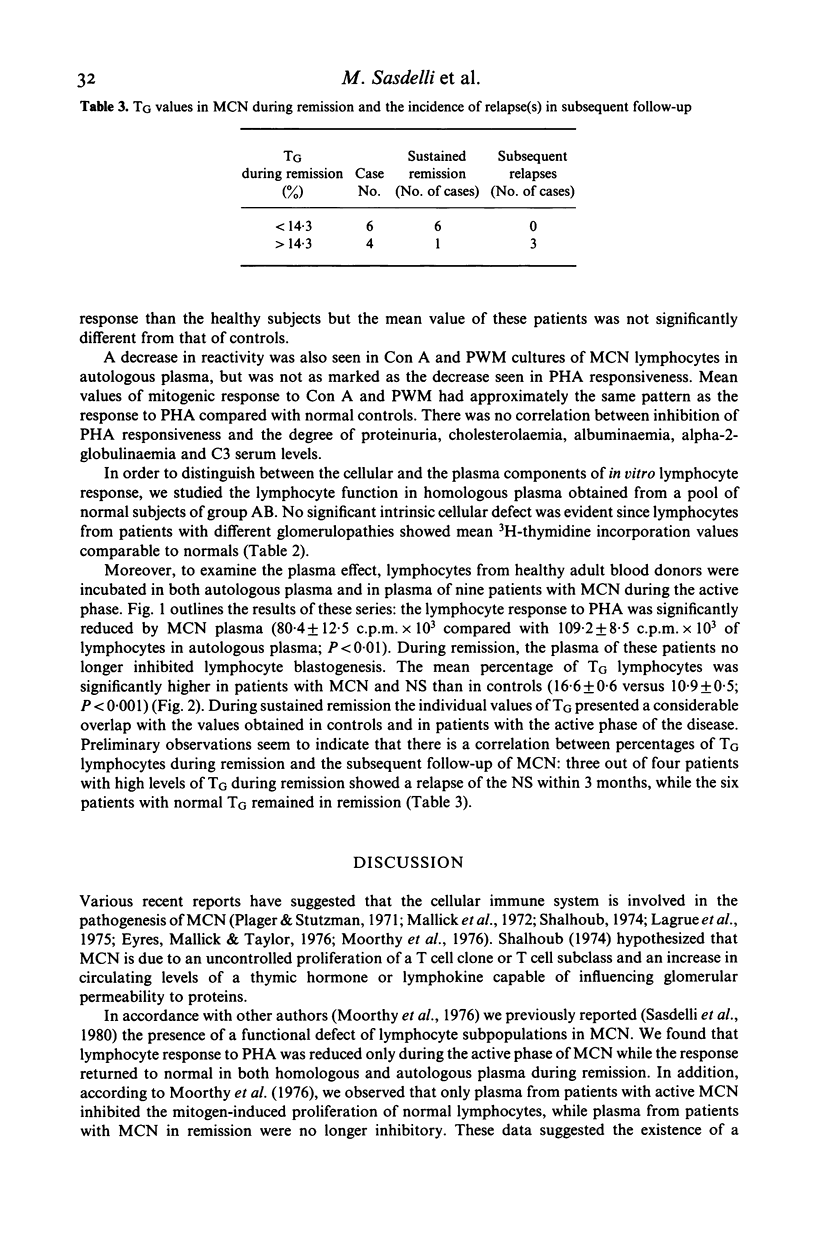
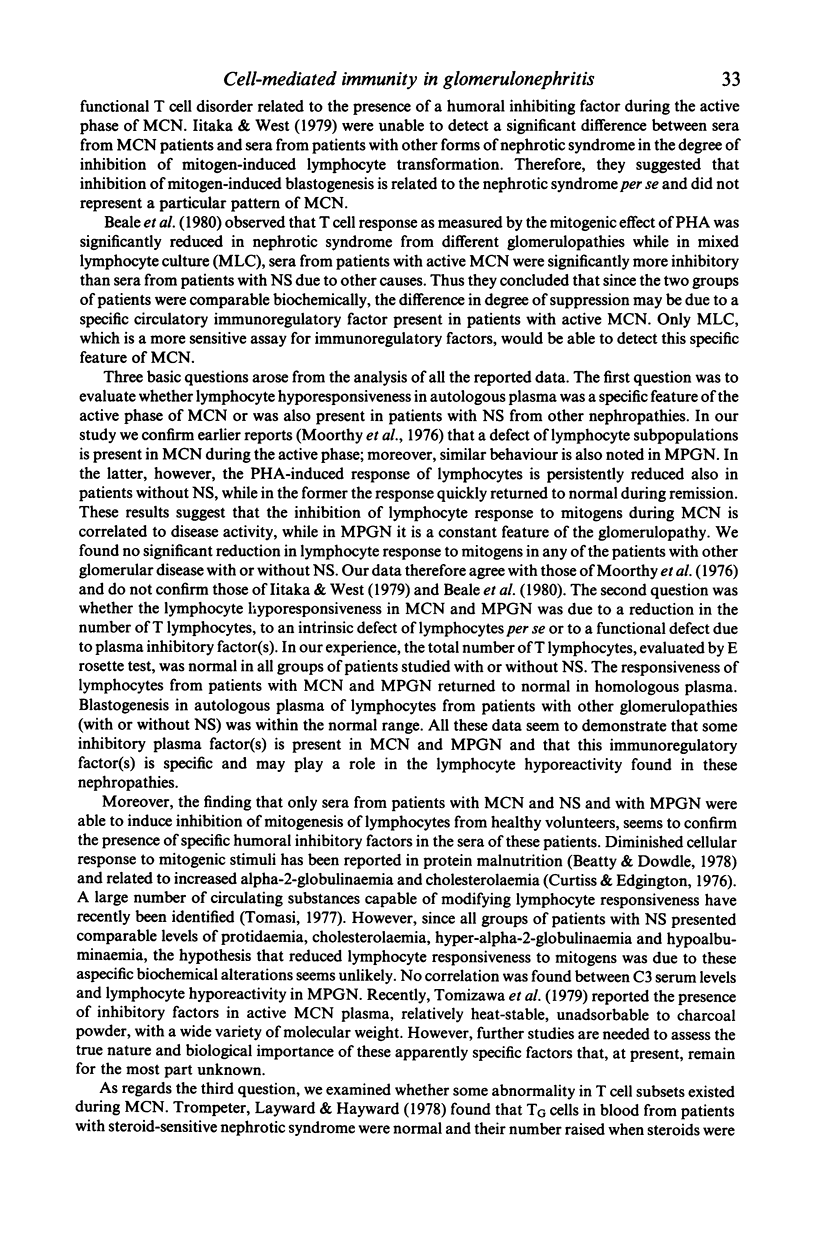
Various recent reports have suggested the presence of a functional defect of lymphocyte subpopulations in minimal-change nephropathy during the active phase. A probable role of inhibitory humoral factor(s) has been hypothesized. However, other authors have been unable to detect a significant difference between plasma from patients with nephrotic syndrome due to minimal-change nephropathy and plasma from other glomerulonephritis in the degree of inhibition of mitogen-induced lymphocyte transformation. In our study, T cell function, as measured by the response to PHA in autologous plasma, was depressed only in patients with minimal-change nephrotic syndrome and in patients with membranoproliferative glomerulonephritis. The lymphocyte function returned to normal when lymphocytes were cultured in homologous plasma. The lymphocyte responsiveness of patients with other glomerulonephritis with or without nephrotic syndrome was normal in both autologous and homologous plasma. Moreover, only plasma from patients with minimal-change nephropathy in the active phase and with membranoproliferative glomerulonephritis were able to induce inhibition of mitogenesis of lymphocytes from healthy donors. These data seem to confirm the presence of specific humoral inhibitory factor(s) in the plasma of these patients. Finally, preliminary findings seem to demonstrate an increase of the number of TG cells in patients with minimal-change nephropathy in remission who relapse early in the subsequent follow-up.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beale M. G., Hoffsten P. E., Robson A. M., MacDermott R. P. Inhibitory factors of lymphocyte transformation in sera from patients with minimal change nephrotic syndrome. Clin Nephrol. 1980 Jun;13(6):271–276. [PubMed] [Google Scholar]
- Beatty D. W., Dowdle E. B. The effects of kwashiorkor serum on lymphocyte transformation in vitro. Clin Exp Immunol. 1978 Apr;32(1):134–143. [PMC free article] [PubMed] [Google Scholar]
- Curtiss L. K., Edgington T. S. Regulatory serum lipoproteins: regulation of lymphocyte stimulation by a species of low density lipoprotein. J Immunol. 1976 May;116(5):1452–1458. [PubMed] [Google Scholar]
- Eyres K., Mallick N. P., Taylor G. Evidence for cell-mediated immunity to renal antigens in minimal-change nephrotic syndrome. Lancet. 1976 May 29;1(7970):1158–1159. doi: 10.1016/s0140-6736(76)91544-0. [DOI] [PubMed] [Google Scholar]
- Ferrarini M., Moretta L., Abrile R., Durante M. L. Receptors for IgG molecules on human lymphocytes forming spontaneous rosettes with sheep red cells. Eur J Immunol. 1975 Jan;5(1):70–72. doi: 10.1002/eji.1830050115. [DOI] [PubMed] [Google Scholar]
- Iitaka K., West C. D. A serum inhibitor of blastogenesis in idiopathic nephrotic syndrome transferred by lymphocytes. Clin Immunol Immunopathol. 1979 Jan;12(1):62–71. doi: 10.1016/0090-1229(79)90111-9. [DOI] [PubMed] [Google Scholar]
- Kaplan M. E., Clark C. An improved rosetting assay for detection of human T lymphocytes. J Immunol Methods. 1974 Jul;5(2):131–135. doi: 10.1016/0022-1759(74)90003-9. [DOI] [PubMed] [Google Scholar]
- Lagrue G., Xheneumont S., Branellec A., Weil B. Letter: Lymphokines and nephrotic syndrome. Lancet. 1975 Feb 1;1(7901):271–272. doi: 10.1016/s0140-6736(75)91164-2. [DOI] [PubMed] [Google Scholar]
- Mallick N. P., Williams R. J., McFarlane H., Orr W. M., Taylor G., Williams G. Cell-mediated immunity in nephrotic syndrome. Lancet. 1972 Mar 4;1(7749):507–509. doi: 10.1016/s0140-6736(72)90174-2. [DOI] [PubMed] [Google Scholar]
- Moorthy A. V., Zimmerman S. W., Burkholder P. M. Inhibition of lymphocyte blastogenesis by plasma of patients with minimal-change nephrotic syndrome. Lancet. 1976 May 29;1(7970):1160–1162. doi: 10.1016/s0140-6736(76)91545-2. [DOI] [PubMed] [Google Scholar]
- Plager J., Stutzman L. Acute nephrotic syndrome as a manifestation of active Hodgkin's Disease. Report of four cases and review of the literature. Am J Med. 1971 Jan;50(1):56–66. doi: 10.1016/0002-9343(71)90205-1. [DOI] [PubMed] [Google Scholar]
- Sasdelli M., Rovinetti C., Cagnoli L., Beltrandi E., Barboni F., Zucchelli P. Lymphocyte subpopulations in minimal-change nephropathy. Nephron. 1980;25(2):72–76. doi: 10.1159/000181756. [DOI] [PubMed] [Google Scholar]
- Shalhoub R. J. Pathogenesis of lipoid nephrosis: a disorder of T-cell function. Lancet. 1974 Sep 7;2(7880):556–560. doi: 10.1016/s0140-6736(74)91880-7. [DOI] [PubMed] [Google Scholar]
- Tomizawa S., Suzuki S., Oguri M., Kuroume T. Studies of T lymphocyte function and inhibitory factors in minimal change nephrotic syndrome. Nephron. 1979;24(4):179–182. doi: 10.1159/000181712. [DOI] [PubMed] [Google Scholar]
- Trompeter R. S., Layward L., Hayward A. R. Primary and secondary abnormalities of T cell subpopulations. Clin Exp Immunol. 1978 Dec;34(3):388–392. [PMC free article] [PubMed] [Google Scholar]
- Wybran J., Fudenberg H. H. Thymus-derived rosette-forming cells in various human disease states: cancer, lymphoma, bacterial and viral infections, and other diseases. J Clin Invest. 1973 May;52(5):1026–1032. doi: 10.1172/JCI107267. [DOI] [PMC free article] [PubMed] [Google Scholar]


