In August 2000, a 3-year-old boy was brought to our infectious disease clinic 10 days after a camping trip in eastern Ontario. Earlier in the week, his parents had sought medical advice because a mosquito bite on the boy's left cheek, one of several he had sustained while camping, had been expanding and becoming more erythematous. Antibiotics had been prescribed for presumed cellulitis, but the lesion had continued to expand and had begun to drain serosanguinous fluid. The parents became concerned when they noticed movement under the skin in the area of the nodular swelling (1 х 1 cm) (Fig. 1). They squeezed the furuncle, and a small white larva (Fig. 2) was discharged.

Figure 1. Photo: Audiovisual Services, CHEO, Ottawa
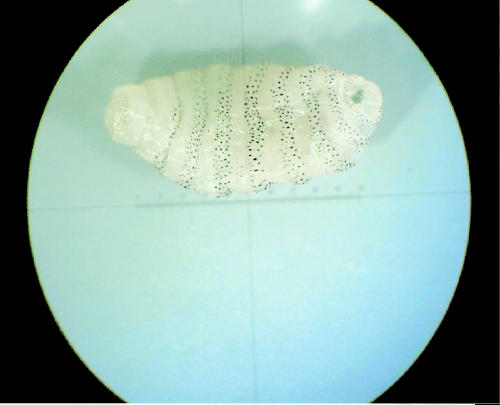
Figure 2. Photo: Dr. Donald Martin, Parasitology Laboratory, Etobicoke, Ont.
At the clinic, we diagnosed furuncular myiasis. The Central Public Health Laboratory in Toronto later identified the larva as an immature botfly of the Cuterebridae family, probably the rodent botfly. The boy's cheek nodule resolved without further treatment over the next few months, and there was no scarring.
Myiasis refers to tissue infestation by flies of the order Diptera (2 winged). There are 3 cutaneous forms of myiasis: furuncular, wound and dermal. Furuncular myiasis occurs when a lesion resembling a furuncle or boil develops after fly larvae enter the skin. Wound myiasis occurs when the larvae infest dead wound tissue, and dermal myiasis results when live dermal tissue is infested. All 3 types have been reported in Canada,1,2 but furuncular myiasis is most common, often occurring in travellers returning to Canada from endemic regions such as Central and South America and Africa.3
In North America, furuncular myiasis is often due to Cuterebra species.4,5,6,7 Infected individuals are often children from rural areas.6 Rodents and rabbits are the natural hosts for the fly, which lays its eggs in the animal's nest or vegetation in the environment. Humans who touch the vegetation inadvertently acquire mature eggs or larvae on their fingers, and infection occurs when these are introduced into facial orifices or broken skin. The larvae breathe and excrete waste through a hole, or operculum. In our patient, a mosquito bite may have created a portal of entry for the larva.
Furuncular lesions due to Cuterebra botflies commonly present as single papules on an exposed skin area, most often on the head, neck or chest.6 Single lesions can also be seen with Dermatobia botflies in South America, whereas Cordylobia flies in Africa may cause multiple skin lesions. Wound and dermal myiasis are diagnosed when larvae are seen on the wound surface, or when there is erythematous tracking and pain as larvae migrate through the skin. Rarely, such larvae can migrate throughout the body, causing cerebral myiasis or blindness from retinal detachment.5
Occlusion of the larva's breathing hole forces the larva to migrate from the lesion completely or to a point where it can be readily extracted with forceps and sent for identification.7 Petroleum jelly under a dressing is a commonly used occlusive agent. Other agents, including bacon fat,8 have also been used. Traumatic means, such as attempting to expel the larva with pressure or surgical excision, are not recommended. Complications such as secondary bacterial infection are uncommon. Although some authors recommend antibiotic prophylaxis,9 most do not prescribe antibiotics if the larva is removed intact and the wound appears clean with no surrounding cellulitis or drainage. General insect avoidance measures (wearing of protective clothing and footwear, use of insect repellents) reduce the risk of myiasis.
Appropriate recognition and management of cutaneous myiasis may save patients from multiple medical visits and courses of antibiotics for presumed bactarial furunculosis.
Robert Slinger Division of Infectious Disease Children's Hospital of Eastern Ontario Ottawa, Ont. Theodore Scholten Former Head of the Parasitology Laboratory Ontario Ministry of Health and Long-Term Care Toronto, Ont.
Footnotes
This article has been peer reviewed.
References
- 1.Scholten T, Brunsdon DF, Rogan WM, Richards RN. Three unusual cases of parasitic infections. CMAJ 1977;117(4):368-9. [PMC free article] [PubMed]
- 2.Scholten T, Chrom VH. Myiasis due to Cuterebra in humans. CMAJ 1979;120(11):1392-3. [PMC free article] [PubMed]
- 3.Gyorkos T. A review of human myiasis in Canada. Can Dis Wkly Rep 1977;3:101-4.
- 4.Josephson RL, Krajden S. An unusual nosocomial infection: nasotracheal myiasis. J Otolaryngol 1993;22:46-7. [PubMed]
- 5.Millikan LE. Myiasis. Clin Dermatol 1999;17: 191-5. [DOI] [PubMed]
- 6.Baird JK, Baird CR, Sabrosky CW. North American cuterebrid myiasis. Report of seventeen new infections of human beings and review of the disease. J Am Acad Dermatol 1989;21:763-72. [PubMed]
- 7.Schiff TA. Furuncular cutaneous myiasis caused by Cuterebra larva. J Am Acad Dermatol 1993;28:261-3. [DOI] [PubMed]
- 8.Brewer TF, Wilson ME, Gonzalez E, Felsenstein D. Bacon therapy and furuncular myiasis. JAMA 1993;270:2087-8. [PubMed]
- 9.Hubler WR Jr, Rudolph AH, Dougherty EF. Dermal myiasis. Arch Dermatol 1974;110:109-10. [PubMed]


