Abstract
We compared the performance characteristics of a standardized direct sequencing method (TRUGENE HCV 5′NC; Visible Genetics Inc., Toronto, Ontario, Canada) and a reverse hybridization line probe assay (INNO-LiPA HCV II; Bayer Corp., Tarrytown, N.Y.) for genotyping of hepatitis C virus (HCV). Both methods are based on detection of sequence heterogeneity in the 5′ noncoding (5′NC) region. Concordance between the genotyping methods was assessed by testing 172 samples representing the six major genotypes. Sequence analysis of the more phylogenetically informative nonstructural 5B (NS5B) region was also done with 148 (86%) samples to confirm the accuracy of and resolve discrepancies between the 5′NC genotyping results. The sensitivities of the methods were assessed by using the 5′NC amplicon from both the qualitative and quantitative AMPLICOR HCV tests (Roche Diagnostics Corp., Indianapolis, Ind.). The ability of the methods to detect mixed-genotype infections was determined with mixtures of two different genotypes at relative concentrations ranging from 1 to 50%. Both 5′NC methods were able to genotype 99.4% of the samples with type agreement for 99.5% and subtype agreement for 68.2% of the samples. No or ambiguous subtype results were found by the line probe assay for 16.5% and by the TRUGENE 5′NC test for 17.1% of the samples. Discrepancies occurred between the line probe assay and NS5B results at the type level for 1.4% of the samples and at the subtype level for 14.2% of the samples. Discrepancies also occurred between the TRUGENE 5′NC and NS5B results at the type level for 2% of the samples and at the subtype level for 8.1% of the samples. We also found two distinct strains of HCV classified as type 2 by analysis of the 5′NC region that were type 1 by analysis of the NS5B region. The sensitivities of the two 5′NC genotyping methods were comparable and dependent on the amplification test used (∼103 IU/ml with the qualitative HCV RNA tests and ∼105 IU/ml with the quantitative HCV RNA tests). Genotype mixtures were successfully identified at a relative concentration of 5% by the line probe assay and 10% by the TRUGENE 5′NC test. In conclusion, the performance characteristics of the 5′NC methods were similar and both methods produced accurate results at the genotype level but neither method should be used for subtyping.
Hepatitis C virus (HCV) chronically infects at least 1% of the world's population. Chronically infected individuals are at increased risk for developing liver cirrhosis and hepatocellular carcinoma. In the United States, end stage liver disease caused by chronic HCV infection is the leading reason for liver transplantation.
HCV is a positive-sense, single-stranded RNA virus that represents the third genus of the family Flaviviridae. Shortly after its discovery in 1989, it became clear that HCV had substantial nucleotide sequence diversity, with only 66 to 80% overall sequence similarity among strains belonging to different genotypes or subtypes (4). Analysis of the nucleotide sequence homology of different viral genomic regions such as the 5′ noncoding (5′NC) region and regions coding for the envelope (E1), core, and nonstructural 5B (NS5B) proteins led to the identification of six major genotypes and numerous subtypes within the genotypes (20). The genotypes and subtypes of HCV differ in geographic distribution, but genotypes 1, 2, and 3 are by far the most common. These three genotypes are responsible for more than 90% of the infections in North and South America, Europe, and Japan.
The best available therapy for HCV infection, alpha interferon in combination with ribavirin, is not highly effective. The sustained virologic response rates of treated patients range from 30 to 70% and are dependent on several key clinical and virologic factors (12, 16). The HCV genotype has emerged as an important factor both in predicting a sustained response to and in determining the duration of antiviral therapy, with genotype 1 infections having the lowest response rates and requiring the longest therapy (17). HCV genotyping is firmly established as part of the pretreatment evaluation of patients with chronic infections, and a current procedural terminology (CPT) code for HCV genotyping (87902) was created by the American Medical Association effective 1 January 2002 (1).
A variety of methods are used to genotype HCV, including direct nucleic acid sequencing (21), a reverse hybridization line probe assay (LiPA) (25), subtype-specific reverse transcription (RT)-PCR (15), DNA restriction fragment length polymorphism (13), heteroduplex mobility analysis (26), primer-specific and mispair extension analysis (8), melting curve analysis with fluorescence resonance energy transfer probes (19), and serologic genotyping (5). Nucleic acid sequencing and phylogenetic analysis of an appropriate subgenomic region remains the reference method. All of the methods are technically complex and costly, many lack standardization, and none are cleared for use by the U.S. Food and Drug Administration.
Genotyping schemes based on variable regions such as the E1, core, and NS5B regions provide enough resolution to reliably determine types and subtypes; however, the 5′NC region is too conserved for accurate discrimination of all subtypes (23). Nevertheless, the conserved nature of the 5′NC region has made it the preferred target for pangenomic HCV RNA detection tests, and sequence analysis of amplicons from these tests is the most efficient way to genotype HCV in a clinical laboratory setting since both tests can be completed with the product from a single amplification reaction.
We compared the performance characteristics of a standardized direct sequencing method (TRUGENE HCV 5′NC; Visible Genetics Inc., Toronto, Ontario, Canada) with those of a reverse hybridization LiPA (INNO-LiPA HCV II; Bayer Corp., Tarrytown, N.Y.) for HCV genotyping. Both tests are based on detection of sequence heterogeneity in the 5′NC region. The concordance, accuracies, sensitivities, and abilities to identify mixed-genotype infections of the two methods were assessed in this clinical evaluation.
(Part of this work was presented in abstract form at the Association for Molecular Pathology Annual Meeting in Philadelphia, Pa., in 2001.)
MATERIALS AND METHODS
Specimens.
A total of 172 clinical specimens were analyzed. Eighty-two percent of the serum samples (n = 141) were submitted to Emory Medical Laboratories for HCV genotyping and included serum samples containing HCV genotypes 1, 2, and 3. The other 18% (31 serum samples), containing HCV genotypes 3, 4, 5, and 6, were obtained from the Visible Genetics sample bank. All serum samples were stored at −70°C prior to testing.
HCV RNA amplification.
The qualitative AMPLICOR HCV Test v2.0 (Roche Diagnostics Corp., Indianapolis, Ind.) was used to amplify a 244-nucleotide (nt) sequence within the 5′NC region of the HCV genome (11). The biotinylated amplicon from this test was used for both the LiPA and the TRUGENE 5′NC sequencing method. The AMPLICOR MONITOR HCV Test v2.0 (Roche Diagnostics Corp.) (11) was also used to quantitate HCV RNA in some samples and in a comparison of the relative sensitivities of the two 5′NC genotyping methods using the amplicons from both AMPLICOR tests. Both AMPLICOR tests were performed in accordance with the manufacturer's instructions and amplify the same sequence within the 5′NC region. Prior to genotyping with the TRUGENE 5′NC kit, denatured amplicons from the AMPLICOR tests were purified by using the QIAquick PCR purification kit (Qiagen, Valencia, Calif.) in accordance with the manufacturer's instructions. PCR amplicons were used directly without purification in the LiPA.
INNO-LiPA HCV II.
The INNO-LiPA HCV II method uses 19 type-specific oligonucleotide probes attached to nitrocellulose strips to detect sequence variations found in the 5′NC region of HCV (25). The biotin-labeled PCR product is hybridized to the probes on the strip under stringent conditions. After hybridization and washing, streptavidin-labeled alkaline phosphatase is added; followed by incubation with a chromogen, which results in the development of a purple-brown precipitate when there is a match between the probe and the biotinylated PCR product. Hybridization of the amplicon with one or more lines on the strip allows the classification of six major genotypes and their most common subtypes. The test was performed in accordance with the manufacturer's instructions, and the probe reactivity patterns were interpreted by using the chart provided by the manufacturer.
TRUGENE sequencing.
Sequencing products were generated from HCV amplicons by using the bidirectional CLIP sequencing method (27). The CLIP sequencing method uses a set of four reaction mixtures containing standard dideoxynucleotide terminators and primers labeled with two different cyanine dyes to sequence both strands of the target amplicon simultaneously in the same tube. The PCR sequencing reaction is performed for 30 cycles and generates chain termination reaction products for each primer. The reaction products are detected in four lanes of an ultrathin polyacrylamide gel by using the Long-Read Tower sequencer. Analysis of the electropherograms was done with the GeneObjects 3.1 software. The forward and reverse sequences are combined to form a query sequence that is compared to previously characterized HCV sequences in the GeneLibrarian module to determine the HCV subtype and the closest isolate. The TRUGENE 5′NC sequencing reaction analyzes a 183-nt fragment from nt −278 to nt −96 (numbering according to reference 4) and compares the query sequence to a library containing sequences representing the six major genotypes and the 24 most common subtypes. The report lists the 10 closest (or identical) sequences in the database and gives the GenBank accession number, percent homology, and score. The homology is expressed as the percentage of identical bases within the sequenced region between the sample and the reference sequence. The score indicates the number of identical bases at known polymorphic positions. There are 78 such positions in the library.
The TRUGENE HCV NS5B assay generated a 450-nt amplicon that was CLIP sequenced, and a 157-nt fragment (shown in Fig. 1) was analyzed by using the NS5B GeneLibrarian module. The NS5B primers amplify all of the genotypes. A 400-nt segment of a 1,800-nt amplicon of the E1 gene (nt 900 to 1,300 relative to the full genome sequence) was CLIP sequenced for E1 genotyping. The E1 primers amplify type 1 and 4 strains well but give weaker signals with type 2 strains. The 5′ and 3′ combined sequence was used with a basic local alignment search tool (BLAST; National Center for Biotechnology Information; www.ncbi.nlm.nih.gov) to find the best-matched 5′NC, core, E1, and NS5B sequences in the GenBank database for some samples.
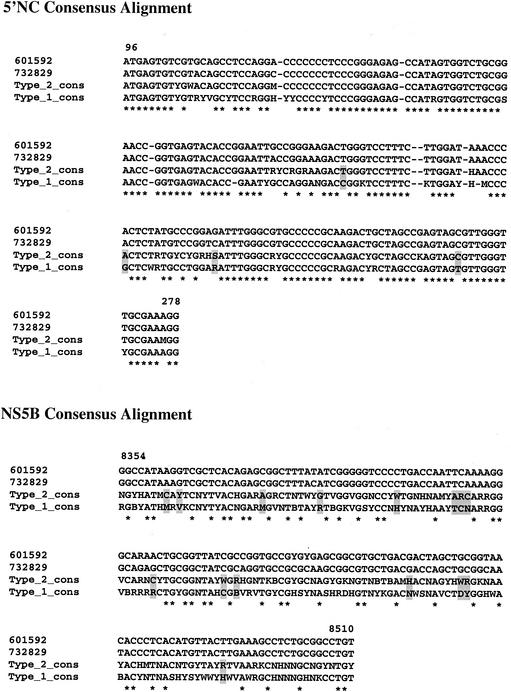
FIG. 1.
Alignment of HCV genotype 1 and 2 consensus nucleotide sequences with sequences obtained from two samples (601592 and 732829) with discrepant genotypes as determined by analysis of partial 5′NC and NS5B sequences. The nucleotide numbering is based on the HCV type 1 genome sequence (GenBank accession number M62321). *, same nucleotide at that position for all sequences; shaded box, phylogenetically informative position; R = A or G; M = A or C; W = A or T; S = G or C; K = G or T; Y = C or T; B = C, G, or T; D = A, C, or T; H = A, C, or T; V = A, C, or G; N = A, C, G, or T.
Study design.
All clinical specimens were genotyped with both the LiPA and the TRUGENE 5′NC kit from aliquots of a single RT-PCR. Sequence analysis of the more informative NS5B region was also done for 86% of the specimens to confirm the accuracy of and resolve discrepancies between the 5′NC genotyping results. E1 genotyping was performed on some samples to help resolve discrepancies between the 5′NC and NS5B genotyping results.
Sensitivity panels were prepared by serially diluting clinical specimens containing HCV genotypes 1a, 1b, and 3a in normal human plasma. Each panel member was tested with both the AMPLICOR HCV (qualitative) and AMPLICOR HCV MONITOR (quantitative) tests, and an aliquot of the amplicon for each test was used for genotyping.
Mixtures of genotypes 1b and 1a, 2b and 1a, and 3a and 1a at relative proportions of 1, 5, 10, 25, and 50% were prepared at a final concentration of approximately 105 IU/ml. Each mixture was amplified with the AMPLICOR HCV Test, and aliquots of the amplicon were genotyped by both 5′NC genotyping methods to assess the abilities of these methods to detected mixed infections.
Timing studies were performed to determine the labor components of both genotyping methods for a batch of 20 samples processed by one technician. The time required to produce the PCR product was not included because this step is common to both genotyping methods.
RESULTS
Both 5′NC genotyping methods were able to genotype 171 (99.4%) of the 172 samples. One sample that was genotype 1 by LiPA could not be typed by TRUGENE 5′NC, and one sample that was genotype 4a by TRUGENE 5′NC could not be typed by LiPA. The genotype distribution by method is shown in Table 1. Essential agreement between the methods at the genotype level was 99.5% (169 of 170). One sample was identified as genotype 1b by TRUGENE 5′NC and as genotype 2a/c by LiPA. Analysis of the NS5B region of this sample indicated that it was genotype 2a. Complete agreement between the methods at the subtype level was 68.2% (116 of 170). No or ambiguous subtype calls (e.g., 1, 1a/b, and 2a/c) were made for 16.5% of the samples by LiPA and for 17.1% by TRUGENE 5′NC.
TABLE 1.
Comparison of HCV genotyping results obtained with the LiPA and the TRUGENE 5′NC kit for 172 clinical specimensa
| LiPA type | No. of specimens with TRUGENE 5′NC type:
|
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 1a | 1b | 1c | 2 | 2a | 2b | 3 | 3a | 3c | 4 | 4a | 4e | 4g | 4f | 5a | 6a | NTb | Total | |
| 1a | 3 | 50 | 1 | 54 | |||||||||||||||
| 1b | 8 | 3 | 32 | 1 | 44 | ||||||||||||||
| 1a/b | 2 | 10 | 1 | 13 | |||||||||||||||
| 1a, 1b | 1 | 3 | 4 | ||||||||||||||||
| 2 | 1 | 1 | 2 | ||||||||||||||||
| 2a/c | 1 | 6 | 7 | ||||||||||||||||
| 2b | 9 | 9 | |||||||||||||||||
| 3a | 4 | 14 | 1 | 19 | |||||||||||||||
| 4 | 1 | 1 | |||||||||||||||||
| 4c/d | 4 | 1 | 5 | ||||||||||||||||
| 4h | 1 | 1 | |||||||||||||||||
| 5a | 7 | 7 | |||||||||||||||||
| 6a | 5 | 5 | |||||||||||||||||
| NT | 1 | 1 | |||||||||||||||||
| Total | 14 | 66 | 33 | 2 | 7 | 0 | 10 | 4 | 14 | 1 | 4 | 1 | 1 | 1 | 1 | 7 | 5 | 1 | 172 |
Specimens with agreement at the subtype level are underlined, and the specimen with disagreement at the genotype level is in boldface.
NT, not typeable.
Sequence analysis of the NS5B region was performed on 148 (86%) of the clinical samples representing genotypes 1, 2, 3, 4, and 6. The LiPA and NS5B typing results of the discordant samples are shown in Table 2. Discrepancies were found between the LiPA and NS5B genotyping results at the subtype level for 21 samples (14.2%) and at the genotype level for 2 samples (1.4%). The TRUGENE 5′NC and NS5B typing results of the discordant samples are shown in Table 3. Discrepancies between the TRUGENE 5′NC and NS5B genotyping results were found at the subtype level for 12 (8.1%) samples and at the type level for 3 (2%) samples. The overall accuracies of the 5′NC tests, as defined by agreement with the NS5B results, were 84.5% for LiPA and 89.9% for TRUGENE 5′NC.
TABLE 2.
Clinical samples with discordant genotypes by LiPA and NS5B sequencing
Genotype 2 by direct sequencing of the E1 region and genotype 2c by sequencing of the core region.
Genotype 2b by direct sequencing of the E1 region.
TABLE 3.
Clinical samples with discordant genotypes by TRUGENE 5′NC kit and NS5B sequencing
| No. of samples | TRUGENE 5′NC genotype | NS5B genotype |
|---|---|---|
| 5 | 1b | 1a |
| 2 | 1a | 1b |
| 1 | 1c | 1a |
| 1 | 1c | 1b |
| 1 | 1b/c | 1a |
| 1 | 1b | 2aa |
| 1 | 2 | 1bb |
| 1 | 2b | 1bc |
| 1 | 3c | 3a |
| 1 | 4e | 4a |
Genotype 2a by sequencing of the E1 region.
Genotype 2 by sequencing of the E1 region and genotype 2c by sequencing of the core region.
Genotype 2b by direct sequencing of the E1 region.
In total, there were three samples for which the 5′NC genotyping methods did not agree with NS5B sequence analysis at the type level. Sample 811000 was classified type 2a/c by LiPA, type 1b by TRUGENE 5′NC, and type 2a by both NS5B and E1 analyses. Unfortunately, none of this sample remained for repeated TRUGENE 5′NC typing. It is possible that the sample sequenced by the TRUGENE 5′NC method was mislabeled.
Two samples, 601592 and 732829, were classified as type 2 by both LiPA and TRUGENE 5′NC and genotype 1 by analysis of the NS5B region. The alignments of these sequences with type 1 and 2 consensus sequences for the 5′NC and NS5B regions are shown in Fig. 1. Both samples matched the consensus type 1 sequence at all four informative positions in the 5′NC region. The 5′NC sequences from the two samples had no polymorphic positions. Both samples matched the consensus type 2 sequence at 14 of 15 informative positions in the NS5B region. The NS5B sequence from sample 601592 had two polymorphic sites, and the sequence from sample 732829 had none.
The genotype assignments of these samples were confirmed by BLAST searches (Table 4). The 5′NC sequence from sample 601592 showed 99% homology with a type 2 sequence (accession no. D497550), and the same region from sample 732829 showed 100% homology with a type 2b sequence (accession no. M84836). The NS5B sequence from sample 601592 showed 97% homology with a type 1b sequence (accession no. Z74503), and the same region from sample 732829 showed 96% homology with another type 1b sequence (accession no. AY030985).
TABLE 4.
BLAST results for nucleic acid sequences found in two samples with discordant genotypes determined by analysis of 5′NC and NS5B regions
| Region (size [nt]) | Parameter(s) | Result(s) for sample no.:
|
|
|---|---|---|---|
| 601592 | 732829 | ||
| 5′NC (183) | Subtype/% homology | 2/99 | 2b/100 |
| Accession no. | D49755 | M84836 | |
| Core (384) | Subtype/% homology | 2c/63 | NDa |
| Accession no. | D31998 | ND | |
| E1 (406) | Subtype/% homology | 2/31 | 2b/86 |
| Accession no. | D49745 | AB030985 | |
| NS5B (157) | Subtype/% homology | 1b/97 | 1b/96 |
| Accession no. | Z74503 | AY003977 | |
ND, not done.
BLAST searches of E1 sequences (not shown) found that the closest matches for these samples were type 2 sequences. Sample 601592 had 31% sequence homology with accession no. D46745 (type 2), and sample 732829 had 86% homology with accession no. AB030985 (type 2b). A BLAST search for sequences matching 384 nt of the core region from sample 601592 (not shown) found a best match with accession no. D31998 (type 2c), with 63% homology. Core region sequencing was not done for sample 732829. Each sequencing reaction described above for samples 601592 and 732829 was performed at least twice.
Samples from four patients hybridized to the two type 1-specific probes (lines 3 and 4), the subtype 1a probe (line 5), and one of two subtype 1b probes (line 6) on the LiPA strip, suggesting coinfections with genotypes 1a and 1b. The line 5 and 6 probe sequences on the LiPA strip were designed to detect the A/G polymorphism at nt −99 (25). In general, the subtype 1a-specific motif contains an A at position −99 and most subtype 1b viruses have a G at this position. Three of these samples were called type 1a, and the remaining one was called type 1 by TRUGENE 5′NC. The 5′NC sequencing revealed an A/G polymorphism at nt −99 in three of the samples. NS5B sequence analysis identified all four samples as genotype 1a, with no evidence of polymorphisms at phylogenetically informative sites within this region.
The analytical sensitivities of the two 5′NC genotyping methods were similar and depended on the amplification test used (Table 5). The sensitivity was approximately 103 IU/ml with the qualitative test amplicon and approximately 105 IU/ml with the quantitative test amplicon.
TABLE 5.
Analytical sensitivities of LiPA and TRUGENE 5′NC using amplicons from AMPLICOR and AMPLICOR MONITOR HCV tests
| Genotype and HCV RNA concn (IU/ml) | AMPLICOR
|
AMPLICOR MONITOR
|
||
|---|---|---|---|---|
| LiPA genotype | TRUGENE genotype | LiPA genotype | TRUGENE genotype | |
| 1a | ||||
| 119,000 | 1a | 1 | 1a | 1 |
| 17,800 | 1a | 1 | NT | NT |
| 4,100 | 1a | 1 | NT | NT |
| <600a | NTb | NT | NT | NT |
| 1b | ||||
| 54,300 | 1b | 1b | 1b | 1b |
| 8,650 | 1b | 1b | NT | NT |
| 730 | 1b | 1b | NT | NT |
| <600a | NT | NT | NT | NT |
| 3a | ||||
| 64,500 | 3a | 3a | 3a | 3a |
| 7,660 | 3a | 3a | NT | NT |
| 770 | 3a | 3a | NT | NT |
| <600a | NT | NT | NT | NT |
HCV RNA detected with the AMPLICOR HCV test at a concentration below the limit of quantitation in the AMPLICOR MONITOR HCV test.
Not typeable because of insufficient amount of amplicon.
Known mixtures of genotypes were recognized by polymorphisms at informative sites in the 5′NC region with the sequencing method and by reactivity with more than one type or subtype probe with the LiPA (data not shown). A mixture of type 1b, 2b, or 3a with type 1a was correctly identified by TRUGENE 5′NC genotyping when one type represented at least 10% of the population (∼104 IU/ml). LiPA correctly identified these same mixtures when one type represented at least 5% of the population (∼103 IU/ml).
Both the LiPA and TRUGENE 5′NC sequencing required approximately 4 h after PCR amplification of the target sequence to complete. The labor component, on the basis of a batch of 20 samples, was calculated to be 5.52 min/sample for LiPA and 11.24 min/sample for TRUGENE 5′NC.
DISCUSSION
Clinical laboratories are under increased pressure to perform HCV genotyping because of the importance of the HCV genotype as a predictor of treatment response. Nucleotide sequence analysis is the “gold standard” for the identification of different HCV types and subtypes but, in the absence of commercially available methods, was considered impractical for many clinical laboratories. Therefore, a number of surrogate typing methods were developed, including LiPA, subtype-specific RT-PCR, DNA restriction fragment length polymorphism, heteroduplex mobility analysis, melting curve analysis, and serologic genotyping. The most widely used of these surrogate typing methods in clinical laboratories is the LiPA.
We compared the HCV genotyping results obtained with a commercially available sequencing system with those obtained with the LiPA. We found a very high level of agreement (99.5%) between the results of the two methods at the genotype level, but only moderate agreement (68.2%) at the subtype level was seen when a large number of clinical specimens representing all of the major types and subtypes of HCV were used. The lack of agreement between the subtype calls is not surprising considering that both methods target the 5′NC region. The 5′NC region is among the most highly conserved regions of the viral genome, and in several cases, only one or two nucleotide changes distinguish unique subtypes (23).
By using sequence analysis of the less-conserved NS5B region as the gold standard, we found that the accuracies of LiPA and TRUGENE 5′NC genotype calls were 98.6 and 98%, respectively, but were only 85.8 and 91.9% accurate, respectively, at the subtype level. Our findings are consistent with other studies that have compared genotyping results from analyses of different subgenomic regions (3, 10, 14, 22, 24). These data suggest that clinical laboratories should not call HCV subtypes from analysis of the 5′NC regardless of the method employed because of the inherent inaccuracy of the calls. There are no recognized subtype-specific differences in disease progression or response to therapy that would warrant these designations.
Our results are similar to two previously published comparisons of the TRUGENE HCV 5′NC kit and the LiPA (2, 7). Both studies found a high level of concordance between the results of the two methods at the genotype level and that neither method could reliably discriminate subtypes of HCV. A third study compared the results of the TRUGENE assay with a core region microwell hybridization assay and found an overall concordance of 91% between the results of the two genotyping methods, with no genotype miscalls with the TRUGENE assay (18). We extend and expand the observations made in these previous studies. Ours is the first study to critically evaluate the sensitivities, abilities to detected mixed genotype infections, and laboratory costs of these methods. Our study is also the first evaluation of the TRUGENE method with specimens obtained from patients in the United States. In addition, we identified two distinct HCV strains that were assigned different genotypes on the basis of sequence analysis of different subgenomic regions.
In practice, sequence analysis of a single subgenomic region is used to genotype HCV because full genome sequencing is impractical in a clinical setting. The underlying assumption is that the region analyzed is representative of the entire HCV genome. The assumption is supported by studies that have compared genotype assignments based on the sequencing of different regions of the HCV genome (10, 14, 22, 24). However, it would be challenged if recombination between different HCV genotypes in patients with coinfections occurred during replication, producing viable hybrid viruses.
A naturally occurring intergenotypic recombinant of HCV was recently identified in St. Petersburg, Russia (9). This virus was found to belong to two different genotypes, 2 and 1, by sequence analysis of the 5′NC region and NS5B regions, respectively. The crossover point for this virus was mapped within the NS2 region. This recombinant virus now accounts for 5% of the HCV infections in St. Petersburg. Recombination may play a role in creating genetic diversity in HCV that may be important in understanding the natural history and treatment of hepatitis C.
We also found two distinct strains of HCV classified as type 2 by analysis of the 5′NC region that were clearly type 1 by analysis of the NS5B region. These sequencing results were reproducible, and little or no polymorphism at key sites within these regions was observed in the electropherograms. Consequently, sample mislabeling or mixed-genotype infections, with selective amplification of one type, are unlikely explanations for our observations. These viruses, like the St. Petersburg strains, may also be examples of hybrids that were produced by separate intertype recombination events. However, further sequence analysis and mapping of the crossover junction are required to prove that these two strains are indeed hybrid viruses. Discrepancy of HCV genotypes as determined by analysis of partial NS5 (genotype 3a) and core sequences (genotype 1a) were also reported for two Honduran HCV strains (28). However, the low frequency of discordant results at the type level does not justify sequencing of multiple regions for routine genotype assignments in most patient populations.
We used the AMPLICOR and AMPLICOR MONITOR tests to generate the 5′NC amplicons for genotyping. These tests are widely used in clinical laboratories to detect and quantitate HCV RNA, and the amplicons from these tests can used for genotyping in both the LiPA and the TRUGENE 5′NC test. However, genotypes can be determined from specimens with lower viral loads if the qualitative HCV RNA test is used to generate the amplicons for genotyping. The qualitative RNA test is carried through more thermal cycles than the quantitative test, and as a result, more PCR product accumulates for a given viral load. Genotypes can be determined from samples with viral loads as low as 103 IU/ml when amplicons from the qualitative test are used. However, the genotyping methods will likely fail for specimens with viral loads of <105 IU/ml when amplicons from the quantitative test are used.
The reported prevalence of HCV mixed-genotype infections varies widely from 0 to more than 20% and appears to be influenced by both the patient population studied and the genotyping method employed (6, 8, 10). Reliable detection of mixed-genotype infections may have broad applications in studies of epidemiology, natural history, pathogenesis, and treatment of hepatitis C. PCR amplification, followed by cloning of the PCR products and sequence analysis of the individual clones, is the only way to establish with certainty that a patient is infected with more than one genotype of HCV but is impractical in a clinical setting. We demonstrated that both the LiPA and the TRUGENE 5′NC method can detect mixtures of two different HCV genotypes. Mixtures of genotypes were recognized as long as the minority population represented at least 5% of the total virus population with the LiPA and at least 10% of the total virus population with the TRUGENE 5′NC method. Although we showed that both methods could reliably detect mixtures of different genotypes prepared in the laboratory, neither method provided convincing evidence of mixed infections in any of the clinical specimens tested.
The LiPA identified four clinical specimens that potentially contained mixtures of genotypes 1a and 1b. All four specimens shared the same unusual pattern of reactivity with the probes in the LiPA (lines 1, 2, 3, 4, 5, and 6). This pattern of probe reactivity was not one of the 58 reactivity patterns predicted by Stuyver et al. (25) on the basis of their analysis of 448 sequences present in several large databases. Probes 5 and 6 are used to detect a subtype-defining A/G polymorphism at position −99. Sequencing of the 5′NC region demonstrated that three of these viruses had both G and A at that position. This apparent G/A polymorphism could result from natural genome divergence during replication (quasispecies), base misincorporation during RT-PCR, or mixed-genotype infection. Chen and Weck (3) recently provided evidence that the A/G polymorphism at position −99 cannot differentiate subtype 1a from subtype 1b. We found no evidence of mixed infection when the NS5B region was sequenced, and all viruses were subtyped as 1a, with no polymorphisms at key sites in this region. Furthermore, a recent update of the LiPA interpretation chart issued by the manufacturer after completion of this study identifies specimens with this pattern of reactivity as genotype 1 without any subtype designation.
In our laboratory, we estimated the direct costs per test (reagents and labor) of the LiPA and the TRUGENE 5′NC sequencing method for HCV genotyping to be comparable at approximately $100. These costs do not include the capital equipment costs, which are substantially greater for the sequencing method. However, in laboratories already using the TRUGENE HIV-1 genotyping assay, these costs could be avoided because the equipment required for HCV genotyping is the same. The Centers for Medicare and Medicaid Services recently decided to reimburse laboratories that bill under the HCV genotyping CPT code (87902) at the same rate as human immunodeficiency virus type 1 resistance genotyping (87901). In most regions of the United States, the Medicare reimbursement for CPT code 87901 is sufficient to cover the costs associated with HCV genotyping methods.
The two methods provide reliable HCV genotyping results at the type level and have similar analytical sensitivities and abilities to recognize mixed infections. The TRUGENE 5′NC method is more technically complex to perform than LiPA, but the more detailed information provided by the direct sequencing method could prove valuable in the detection of new viral types or in epidemiological investigations. In addition, the TRUGENE 5′NC system can be easily updated as new HCV sequence information becomes available and the platform offers users the option of generating sequence information from other regions of the HCV genome.
Acknowledgments
This study was supported in part by Visible Genetics Inc.
After the completion of this study and submission of the manuscript, Visible Genetics Inc. was acquired by Bayer Corp.
REFERENCES
- 1.American Medical Association. 2001. Current procedural terminology 2002. American Medical Association, Chicago, Ill.
- 2.Ansaldi, F., F. Torre, B. M. Bruzzone, A. Picciotto, P. Crovari, and G. Icardi. 2001. Evaluation of a new hepatitis C virus sequencing assay as a routine method for genotyping. J. Med. Virol. 63:17-21. [PubMed] [Google Scholar]
- 3.Chen, Z., and K. E. Weck. 2002. Hepatitis C virus genotyping: interrogation of the 5′ untranslated region cannot accurately distinguish genotypes 1a and 1b. J. Clin. Microbiol. 40:3127-3134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choo, Q. L., K. H. Richman, J. H. Han, K. Berger, C. Lee, C. Dong, C. Gallegos, D. Coit, R. Medina-Selby, P. J. Barr, A. J. Weiner, D. W. Bradley, G. Kuo, and M. Houghton. 1991. Genetic organization and diversity of the hepatitis C virus. Proc. Natl. Acad. Sci. USA 88:2451-2455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dixit, V., S. Quan, P. Martin, D. Larson, M. Brezina, R. DiNello, K. Sra, J. Y. Lau, D. Chien, and J. Kolberg. 1995. Evaluation of a novel serotyping system for hepatitis C virus: strong correlation with standard genotyping methodologies. J. Clin. Microbiol. 33:2978-2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eyster, M. E., K. E. Sherman, J. J. Goedert, A. Katsoulidou, and A. Hatzakis. 1999. Prevalence and changes in hepatitis C virus genotypes among multitransfused persons with hemophilia: the multicenter hemophilia cohort study. J. Infect. Dis. 179:1062-1069. [DOI] [PubMed] [Google Scholar]
- 7.Halfon, P., P. Trimoulet, M. Bourliere, H. Khiri, V. deLedinghen, P. Couzigou, J. M. Feryn, P. Alcaraz, C. Renou, H. J. A. Fleury, and D. Ouza. 2001. Hepatitis C virus genotyping based on 5′ noncoding sequence analysis (Trugene). J. Clin. Microbiol. 39:1771-1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu, Y.-W., E. Balaskas, M. Furione, P.-H. Yen, G. Kessler, V. Scalia, L. Chui, and G. Sher. 2000. Comparison and application of a novel genotyping method, semiautomated primer-specific and mispair extension analysis, and four other genotyping assays for detection of hepatitis C virus mixed-genotype infections. J. Clin. Microbiol. 38:2807-2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kalinina, O., H. Norder, S. Mukomolov, and L. O. Magnius. 2002. A natural intergenotypic recombinant of hepatitis C virus identified in St. Petersburg. J. Virol. 76:4034-4043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lau, J. Y., M. Mizokami, J. A. Kolberg, G. L. Davis, L. E. Prescott, T. Ohno, R. P. Perrillo, K. L. Lindsay, R. G. Gish, and K. P. Qian. 1995. Application of six hepatitis C virus genotyping systems to serum samples from chronic hepatitis C patients in the United States. J. Infect. Dis. 171:281-289. [DOI] [PubMed] [Google Scholar]
- 11.Lee, S. C., A. Anthony, N. Lee, J. Leibow, J. Q. Yang, S. Soviero, K. Gutekunst, and M. Rosenstraus. 2000. Improved version 2.0 qualitative and quantitative AMPLICOR reverse transcription-PCR tests for hepatitis C virus RNA: calibration to international units, enhanced genotype reactivity, and performance characteristics. J. Clin. Microbiol. 38:4171-4179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McHutchinson, J. G., S. C. Gordon, E. R. Schiff, M. L. Shiffman, W. M. Lee, V. K. Rustgi, Z. D. Goodman, M.-H. Ling, S. Cort, and J. K. Albrecht for The Hepatitis Interventional Therapy Group. 1998. Interferon alfa-2b alone or in combination with ribavirin as initial treatment for chronic hepatitis C. N. Engl. J. Med. 339:1485-1492. [DOI] [PubMed] [Google Scholar]
- 13.Nakao, T., N. Enomoto, N. Takada, A. Takada, and T. Date. 1991. Typing of hepatitis C virus genomes by restriction fragment length polymorphism. J. Gen. Virol. 72:2105-2112. [DOI] [PubMed] [Google Scholar]
- 14.Ohba, K.-I., M. Mizokami, T. Ohno, K. Suzuki, E. Orito, Y. Ina, J. Y. N. Lau, and T. Gojobori. 1995. Classification of hepatitis C virus into major types and subtypes based on molecular evolutionary analysis. Virus Res. 36:201-214. [DOI] [PubMed] [Google Scholar]
- 15.Okamoto, H., Y. Sugiyama, S. Okada, K. Kurai, Y. Akahane, Y. Sugai, T. Tanaka, K. Sato, F. Tsuda, and Y. Miyakawa. 1992. Typing hepatitis C virus by polymerase chain reaction with type-specific primers: application to clinical surveys and tracing infectious sources. J. Gen. Virol. 73:673-679. [DOI] [PubMed] [Google Scholar]
- 16.Poynard, T., P. Marcellin, S. S. Lee, C. Niederau, G. S. Minuk, G. Ideo, V. Bain, J. Heathcote, S. Zeuzem, C. Trepo, and J. Albrecht for The International Hepatitis Interventional Therapy Group. 1998. Randomised trial of interferon α2b plus ribavirin for 48 weeks or for 24 weeks versus interferon α2b plus placebo for 48 weeks for treatment of chronic infection with hepatitis C virus. Lancet 352:1426-1432. [DOI] [PubMed] [Google Scholar]
- 17.Poynard, T., J. G. McHutchison, Z. D. Goodman, M.-H. Ling, and J. Albrecht for The ALGOVIRC Project Group. 2000. Is an “a la carte” combination interferon alfa-2b plus ribavirin regimen possible for the first line treatment in patients with chronic hepatitis C? Hepatology 31:211-218. [DOI] [PubMed] [Google Scholar]
- 18.Ross, R. S., S. O. Viazov, C. D. Holtzer, A. Beyou, A. Monnet, C. Mazure, and M. Roggendorf. 2000. Genotyping of hepatitis C virus isolates using CLIP sequencing. J. Clin. Microbiol. 38:3581-3584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schroter, M., B. Zollner, P. Schafer, O. Landt, L. U., R. Laufs, and H.-H. Feucht. 2002. Genotyping of hepatitis C virus types 1, 2, 3, and 4 by a one-step LightCycler method using three different pairs of hybridization probes. J. Clin. Microbiol. 40:2046-2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simmonds, P., A. Alberti, H. J. Alter, F. Bonino, D. W. Bradley, C. Brechot, J. T. Brouwer, S. W. Chan, K. Chayama, D. S. Chen, Q. L. Choo, M. Colombo, T. Cuypers, T. Date, G. Dusheiko, J. I. Esteban, O. Fay, S. Hadziyannis, J. Han, A. Hatzakis, E. C. Holmes, H. Hotta, M. Houghton, B. Irvine, M. Kohara, J. A. Kolberg, G. Kuo, J. Y. N. Lau, P. N. Lelie, G. Maertens, F. McOmish, T. Miyamura, M. Mizokami, A. Nomoto, A. M. Prince, H. W. Reesink, C. Rice, M. Roggendorf, S. Schalm, T. Shikata, K. Shimotohno, L. Stuyver, C. Trepo, A. Weiner, P. L. Yap, and M. S. Urdea. 1994. A proposed system for the nomenclature of hepatitis C viral genotypes. Hepatology 19:1321-1324. [PubMed] [Google Scholar]
- 21.Simmonds, P., E. C. Holmes, T.-A. Cha, S.-W. Chan, F. McOmish, B. Irvine, E. Beall, P. L. Yap, J. Kolberg, and M. S. Urdea. 1993. Classification of hepatitis C virus into six major genotypes and a series of subtypes by phylogenetic analysis of the NS-5 region. J. Gen. Virol. 74:2391-2399. [DOI] [PubMed] [Google Scholar]
- 22.Simmonds, P., D. B. Smith, F. McOmish, P. L. Yap, J. Kolberg, M. S. Urdea, and E. C. Holmes. 1994. Identification of genotypes of hepatitis C virus by sequence comparisons in the core, E1 and NS-5 regions. J. Gen. Virol. 75:1053-1061. [DOI] [PubMed] [Google Scholar]
- 23.Smith, D. B., J. Mellor, L. M. Jarvis, F. Davidson, J. Kolberg, M. Urdea, P. L. Yap, and P. Simmonds. 1995. Variation of the hepatitis C virus 5′ noncoding region: implications for secondary structure, virus detection, and typing. J. Gen. Virol. 76:1749-1761. [DOI] [PubMed] [Google Scholar]
- 24.Stuyver, L., W. van Arnhem, A. Wyseur, F. Hernandez, E. Delaporte, and G. Maertens. 1994. Classification of hepatitis C viruses based on phylogenetic analysis of the envelope 1 and nonstructural 5B regions and identification of five additional subtypes. Proc. Natl. Acad. Sci. USA 91:10134-10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stuyver, L., A. Wyseur, W. van Arnhem, F. Hernandez, and G. Maertens. 1996. Second-generation line probe assay for hepatitis C virus genotyping. J. Clin. Microbiol. 34:2259-2266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.White, P. A., X. Zhai, I. Carter, Y. Zhao, and W. D. Rawlinson. 2000. Simplified hepatitis C virus genotyping by heteroduplex mobility analysis. J. Clin. Microbiol. 38:477-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yager, T. D., L. Baron, R. Batra, A. Bouevitch, D. Chan, K. Chan, S. Darasch, R. Gilchrist, A. Izmailov, J. M. Lacroix, K. Marchelleta, J. Renfrew, D. Rushlow, E. Steinbach, C. Ton, P. Waterhouse, H. Zaleski, J. M. Dunn, and J. Stevens. 1999. High performance DNA sequencing, and the detection of mutations and polymorphisms, on the Clipper sequencer. Electrophoresis 20:1280-1300. [DOI] [PubMed] [Google Scholar]
- 28.Yun, Z., C. Lara, B. Johannson, I. L. de Rivera, and A. Sonnerborg. 1996. Discrepancy of hepatitis C virus genotype as determined by phylogenetic analysis of partial NS5 and core sequences. J. Med. Virol 49:155-160. [DOI] [PubMed] [Google Scholar]