Abstract
The capsule of Bacillus anthracis, composed of poly-γ-d-glutamic acid (γDPGA), is an essential virulence factor of B. anthracis. The capsule inhibits innate host defense through its antiphagocytic action. γDPGA is a poor immunogen, but when covalently bound to a carrier protein, it elicits serum antibodies. To identify the optimal construct for clinical use, synthetic γDPGAs of different lengths were bound to carrier proteins at different densities. The advantages of the synthetic over the natural polypeptide are the homogeneous chain length and end groups, allowing conjugates to be accurately characterized and standardized and their chemical compositions to be related to their immunogenicities. In the present study, we evaluated, in addition to methods reported by us, hydrazone, oxime, and thioether linkages between γDPGA and several proteins, including bovine serum albumin, recombinant Pseudomonas aeruginosa exotoxin A, recombinant B. anthracis protective antigen (rPA), and tetanus toxoid (TT). The effects of the dosage and formulation on the immunogenicities of the conjugates were evaluated in mice. All conjugates were immunogenic. The optimal γDPGA chain length of 10 to 15 amino acids and the density, an average of 15 mol γDPGA per mol of protein, were confirmed. The thioether bond was the optimal linkage type, and TT and rPA were the best carriers. The optimal dosage was 1.2 to 2.5 μg of γDPGA per mouse, and adsorption of the conjugates onto aluminum hydroxide significantly increased the antibody response to the protein with a lesser effect on anti-γDPGA levels.
Anthrax, a potentially lethal human disease, is a zoonotic infection that under natural conditions is contracted by humans directly or indirectly from animals. The causative organism, Bacillus anthracis, exists in vegetative or spore forms, the latter being the infecting agent. A veterinary vaccine based on a capsule-negative, toxin-positive strain (Sterne) is available and is routinely used throughout the world (25). In addition, anthrax vaccine adsorbed, containing the protective antigen, is licensed and used by veterinarians, animal by-product handlers, and the U.S. Army (2, 5). Anthrax is endemic in countries that do not immunize domesticated animals (9, 12, 24). Because of the ease of cultivating the organism and improved technology of spore preparation, B. anthracis is a potential bioterrorism agent. In 2001, B. anthracis spores were used successfully via the U.S. mail, though few people were affected. A major bioterrorism attack may be airborne, with a number of spores far exceeding a natural exposure, causing inhalation anthrax and affecting a large number of people, including children. These facts warrant devising an improved anthrax vaccine.
The addition of components other than those of anthrax toxin to improve vaccine-induced protection has been considered (22). The capsule, composed of poly-γ-d-glutamic acid (γDPGA), is an essential virulence factor and antiphagocytic, and antibodies to this polypeptide have been shown to be opsonophagocytic and protective in mice (3, 10, 22). γDPGA by itself is a poor immunogen and does not induce booster responses, probably because of its simple homopolymeric structure, similar to those of capsular polysaccharides; it is a T-cell-independent antigen and of d-amino acid composition (7). These immunologic properties can be overcome by covalent binding of the T-cell-independent antigen to immunogenic proteins (22). Because of the success in inducing protective levels of antibodies in infants against systemic infection with capsulated pathogens, we developed conjugates of γDPGA with several carrier proteins, including bovine serum albumin (BSA), recombinant B. anthracis protective antigen (rPA), and recombinant Pseudomonas aeruginosa exoprotein A (rEPA). Unlike γDPGA alone, these conjugates were immunogenic in mice, with booster responses upon reinjection. Conjugate-induced antibodies were opsonophagocytic (22, 27). This study describes additional synthetic schemes in an attempt to develop the most immunogenic conjugates.
MATERIALS AND METHODS
Analyses.
Amino acid analysis was done by gas-liquid chromatography-mass spectrometry (GLC-MS) after hydrolysis with 6 N HCl at 150°C for 1 h and derivatization to N-heptafluorobutyryl R-(−)-isobutyl esters and assay with a Hewlett-Packard apparatus (model HP 6890) with an HP-5 0.32- by 30-mm glass capillary column with temperature programming at 8°C/min from 125 to 250°C in the electron ionization (106-eV) mode (22). The number of peptide chains in the conjugates was calculated by the ratio between l- and d-glutamic acids. The protein concentration was measured by the method of Lowry et al. (16), free ɛ amino groups by Fields' assay (6), benzaldehyde groups by colorimetric reaction with 2-hydrazinopyridine (Solulink, San Diego, CA), hydrazide was measured as reported previously (23), and thiolation was measured by release of 2-pyridylthio groups (A343) (1). Sodium dodecyl sulfate-polyacrylamide gel electrophoresis used 14% gels according to the manufacturer's instructions (Bio-Rad, Hercules, CA). Double immunodiffusion was performed in 1.0% agarose gels in phosphate-buffered saline (PBS) with rabbit anti-γDPGA, rabbit anti-BSA (Sigma, St. Louis, MO), goat anti-exotoxin A (List Biological Laboratories, Inc.), anti-tetanus toxoid (obtained from W. Vann, FDA, Bethesda MD), and anti-B. anthracis protective antigen (obtained from S. Leppla, NIH/NIAID, Bethesda, MD). Aluminum hydroxide was used as Alhydrogel (Staten Serum Institut, Copenhagen, Denmark).
MALDI-TOF.
Mass spectra were obtained with an OmniFlex matrix-assisted laser desorption ionization-time of flight (MALDI-TOF) instrument (Bruker Daltonics) operated in the linear mode. Samples for analysis were desalted, and 1 μl was mixed with 20 μl of sinapinic acid matrix made in 30% CH3CN and 0.1% trifluoroacetic acid. Then, 1 μl of the mixture was dried on the sample stage and placed in the mass spectrometer.
Antigens.
BSA (66.5 kDa; Sigma, St. Louis, MO) was dialyzed against pyrogen-free water, sterile filtered, and freeze-dried. rPA (83 kDa) from B. anthracis and rEPA (67 kDa) from P. aeruginosa were prepared and characterized (8, 21). Tetanus toxoid (TT) (150 kDa) was obtained from Merieux, Lyon, France.
γDPGA was purified from the culture supernatant of B. anthracis strain A34 toxin-negative by cetavlon precipitation, acidification to pH 1.5, precipitation with ethanol, and passage through a 2.5- by 100-cm Sephacryl S-1000 column in 0.2 M NaCl (26). Its structure was confirmed by 1H nuclear magnetic resonance and 13C nuclear magnetic resonance, and its enantiomeric composition was determined by GLC-MS spectroscopy. γDPGA peptides were synthesized by the method of Merrifield (AnaSpec, San Jose, CA). Peptides were divided into groups depending on the types of linkages through which they were bound to proteins: (i) thioether linkage, NAc-γDPGA10-Gly3-l-Cys-CONH2 (γDPGA10-Cys) or NBrAc-Gly3-γDPGA10-COOH (Br-γDPGA10); (ii) hydrazone linkage, 4-formylbenzoyl-Gly3-γDPGA10-COOH (CHO-γDPGA10), NAc-γDPGA10-Gly3-CO-NH-NH-CO-(CH2)4-CO-NH-NH2 (γDPGA10-AH), or NAc-γDPGA15-CO-NH-NH-CO-(CH2)4-CO-NH-NH2 (γDPGA15-AH), where AH is adipic acid hydrazide; and (iii) oxime linkage, 4-formylbenzoyl-Gly3-γDPGA10-COOH (CHO-PGA10).
Conjugation. (i) Thioether linkage.
First, protein was bromoacylated using succinimidyl 3-(bromoacetamido)propionate (SBAP) (Pierce, Rockford, IL) and reacted with peptides equipped with a terminal cysteine residue as reported previously (22) (protein/S-Cys-Gly3-γDPGA10-NAc, protein/S-Cys-γDPGA10-NAc, or protein/S-Cys-γDPGA15-NAc).
Second, protein was derivatized with an N-hydroxysuccinimide ester of 3-(2-pyridyldithio)propionic acid (SPDP) (Pierce, Rockford, IL) and reacted with bromoacylated peptide (22) (protein-S/Gly3-γDPGA10-COOH).
Third, sulfhydryl groups were introduced into the protein using 2-iminothiolane (ITL) (ScienceLab, Houston, TX). Protein (20 mg) was derivatized with 2.8 mg ITL in 1.5 ml of buffer A (PBS, 0.1% glycerol, 0.005 M EDTA, pH 7.4) for 60 min. Next, a solution of Br-γDPGA10 (35 mg) in 300 μl of 1 M K2HPO4 was added while the pH was maintained at 7.4 with the addition of 0.2 N NaOH at room temperature. After 90 min, the reaction mixture was passed through a Sepharose CL-6B column (1 by 120 cm) and eluted with 0.2 M NaCl. Fractions reacting with anti-protein and anti-γDPGA were pooled (protein-ITL/Gly3-γDPGA10-COOH).
(ii) Hydrazone linkage.
First, protein was derivatized with succinimidyl 4-formylbenzoate (SFB) (Solulink, San Diego, CA). To a solution of protein (30 mg) in 1.2 ml buffer A, SFB (7.5 mg) in 100 μl dimethyl sulfoxide was added and reacted for 2 h at pH 7.4. The product 4-formylbenzoyl-protein was passed through a Sephadex G-50 column (1 by 100 cm) in 0.2 M NaCl. Protein-containing fractions were pooled and assayed for the presence of benzaldehyde, antigenicity, and protein concentration. To 4-formylbenzoyl-protein (20 mg) in 1.25 ml buffer A, a solution of 15 mg of AH-γDPGA10 or AH-γDPGA15 in 200 μl 1 M K2HPO4 was added. The pH of the reaction mixture was adjusted to 7.4, and the mixture was incubated overnight at room temperature and then passed through a Sepharose CL-6B column as described above. Fractions reacting with anti-protein and anti-γDPGA were pooled and assayed (protein-SFB/AH-Gly3-γDPGA10-NAc or protein-SFB/AH-γDPGA15-NAc).
Second, derivatization of protein with adipic acid dihydrazide using a water-soluble carbodiimide was done as reported previously (23). The incorporation of hydrazide residues was 2 to 5% per protein. To protein-AH (20 mg) in 1.3 ml buffer A, a solution of 20 mg of CHO-γDPGA10 in 200 μl 1 M K2HPO4 was added. The pH was adjusted to 7.4, and the solution was incubated overnight at room temperature and then passed through a Sepharose CL-6B column as described above. Fractions reacting with anti-protein and anti-γDPGA were pooled and assayed (protein-AH/SFB-Gly3-γDPGA15-COOH).
(iii) Oxime linkage.
BSA was first bromoacylated with SBAP and then reacted with O-(3-thiolpropyl)hydroxylamine, a heterobifunctional aminooxy-thiol linker (11). To 20 mg of aminooxylated protein (protein-ONH2) in 1.3 ml buffer A, a solution of 20 mg of CHO-PGA in 200 μl 1 M K2HPO4 was added. The pH was adjusted to 7.4, and the mixture was incubated overnight at room temperature and then passed through a Sepharose CL-6B column as described above. Fractions reacting with anti-protein and anti-γDPGA were pooled and assayed (protein-ONH2/SFB-Gly3-γDPGA10-COOH).
Immunization.
All animal experiments were approved by the National Institute of Child Health and Human Development (NICHD) Animal Care and Use Committee. Five- to 6-week-old female NIH general-purpose mice were immunized subcutaneously three times at 2-week intervals with 2.5 μg γDPGA as a conjugate in 0.1 ml PBS. Groups of 10 were exsanguinated 7 days after the second or third injection (23). Controls received PBS.
Antibodies.
Serum immunoglobulin G (IgG) antibodies were measured by enzyme-linked immunosorbent assay (ELISA) (23). Nunc Maxisorb plates were coated with B. anthracis γDPGA, 20 μg/ml PBS, or 4 μg protein/ml PBS (determined by checkerboard titration). The plates were blocked with 0.5% BSA (or with 0.5% HSA for assay of BSA conjugates) in PBS for 2 h at room temperature. An MRX Dynatech reader was used. Antibody levels were calculated relative to standard sera: for γDPGA, a hyperimmune murine serum (22); for PA, a monoclonal antibody containing 4.7 mg antibody/ml (15); for BSA and rEPA, a pool of highest-titer sera obtained from mice immunized three times and assigned a value of 100 EU. The results were computed with an ELISA data-processing program provided by the Biostatistics and Information Management Branch, CDC (19). IgG levels are expressed as geometric means (GM).
Statistics.
The Bonferroni multiple-comparison test was used for different groups of mice.
RESULTS
Characterization of conjugates.
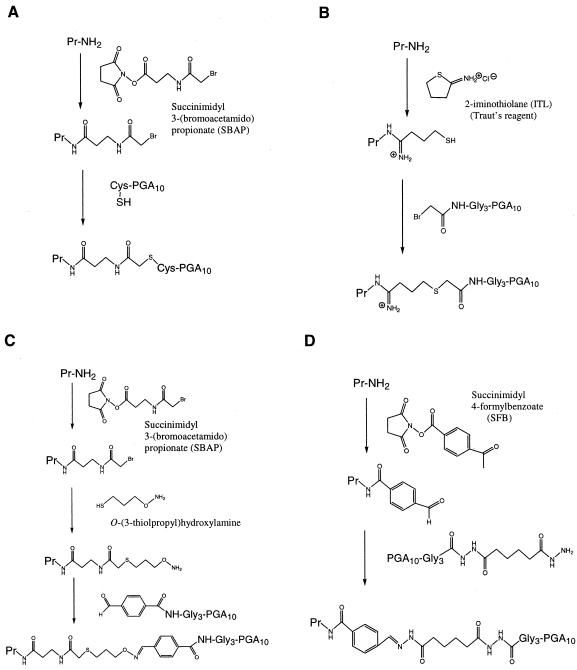
The conjugation methods used in the study for binding γDPGA to protein carriers are illustrated in Fig. 1. The purity of the conjugates and the absence of free protein were confirmed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis and by MALDI-TOF spectroscopy. The molar ratio of γDPGA to protein in conjugates, calculated by GLC-MS analysis, was based on the ratio of d-glutamic acid to l-glutamic acid in the conjugate and by the increase in molecular mass, measured by MALDI-TOF, of the conjugate compared to that of the protein derivatized with the appropriate linker.
FIG. 1.
Examples of linkage types used for conjugation of poly-γ-d-glutamic acid (γDPGA) peptides to protein carriers. (A and B) Thioether linkage. (C) Oxime linkage. (D) Hydrazone linkage.
Antibodies to γDPGA.
Conjugates varied in γDPGA chain length, density on the protein, carrier proteins, and types of linkage between γDPGA and the protein. Additional variables were the formulation and the dosage injected into mice. All conjugates reacted with anti-γDPGA and anti-protein sera with a line of identity. All conjugates were highly immunogenic in mice; most immune sera precipitated B. anthracis γDPGA by double immunodiffusion (results not shown).
To identify the most immunogenic conjugates, we compared the immunogenicities of new constructs with those reported previously (22). Our previous results showed that protein conjugates of 10-mers of γDPGA were more immunogenic than the conjugates of 5- or 20-mers (22). Here, we have used 10-mers with three glycine residues (Gly3-γDPGA10) at the end linked to protein as before and 10-mers (γDPGA10) and 15-mers (γDPGA15) without glycine to avoid the generation of antibodies to the glycine linker. There were no statistical differences in the anti-γDPGA levels between the conjugates of the three peptides after three injections (Table 1). For example, the two conjugates TT/Cys-γDPGA10 and TT/Cys-γDPGA15, having the same average density of γDPGA on the protein (16 chains), gave similar responses, irrespective of the peptide chain length (after the second injection, the TT/Cys-γDPGA10 GM was 6,868 and the TT/Cys-γDPGA15 GM was 6,547; after the third injection, the TT/Cys-γDPGA10 GM was 6,667 and the TT/Cys-γDPGA15 GM was 7,688). Conjugate TT/Cys-Gly3-γDPGA10, with an average density of 11 γDPGA chains per protein, induced a lower level of antibodies after the second injection (GM = 421; P < 0.001), but after the third injection, the GM antibody level was similar to that of the conjugate without the glycine linker (GM = 7,762).
TABLE 1.
Density/immunogenicity relationships of conjugates prepared with 10- and 15-mers of γDPGA bound to TT or rPAa
| Conjugate | γDPGA (mol)/ protein (mol) | Protein/γDPGA (wt/wt) | Anti-γDPGA (EU)
|
Anti-rPA (μg/ml)
|
||
|---|---|---|---|---|---|---|
| 2nd injection | 3rd injection | 2nd injection | 3rd injection | |||
| TT/Cys-Gly3-γDPGA10 | 11 | 1:0.10 | 420 | 7,800 | NTb | NT |
| TT/Cys-γDPGA10 | 16 | 1:0.16 | 6,900 | 6,700 | NT | NT |
| TT/Cys-γDPGA15 | 16 | 1:0.22 | 6,500 | 7,700 | NT | NT |
| TT-CHO/AH-γDPGA15 | 37 | 1:0.48 | 1,900 | 2,300 | NT | NT |
| rPA-CHO/AH-γDPGA15 | 5 | 1:0.12 | 120 | 320 | 0.2 | 4 |
| rPA-CHO/AH-γDPGA15 | 11 | 1:0.26 | 3,600 | 5,200 | 0.1 | 13 |
| rPA-CHO/AH-Gly3-γDPGA10 | 29 | 1:0.45 | 210 | 1,300 | 0.1 | 2 |
| rPA-AH/CHO-Gly3-γDPGA10 | 22 | 1:0.34 | 1,000 | 2,500 | 0.3 | 28 |
| rPA/Cys-Gly3-γDPGA10 | 15 | 1:0.24 | 2,100 | 4,000 | 37 | 170 |
| rPA-ITL/Br-Gly3-γDPGA10 | 8 | 1:0.13 | 2,300 | 3,700 | 4.7 | 61 |
| rPA-ITL/Br-Gly3-γDPGA10 | 18 | 1:0.29 | 2,400 | 3,000 | 0.2 | 41 |
Five- to 6-week-old NIH general-purpose mice (n = 10) were injected subcutaneously with 2.5 μg of γDPGA as a conjugate 2 weeks apart and exsanguinated 7 days after the second or third injection. IgG anti-γDPGA and anti-rPA were measured by ELISA, and the results are expressed as the geometric means.
NT, not tested.
Table 1 summarizes the influence of the γDPGA chain density on the protein on the conjugate's immunogenicity. The best responses were achieved with an average of 10 to 15 chains per protein. The antibody level induced by TT/Cys-γDPGA15 with 16 chains per protein (GM = 7,688) was significantly higher than that induced by TT-CHO/AH-γDPGA15 with 37 chains per protein (GM = 2,322; P < 0.001). Similarly, conjugate rPA-CHO/AH-γDPGA15 with 11 chains (GM = 5,225) induced a higher level of antibodies than the conjugate with an average of 5 chains per protein (GM = 315; P < 0.001) or rPA-CHO/AH-Gly3-γDPGA10 with 29 chains per protein (GM = 1,256; P < 0.001). There were no statistical differences between rPA-ITL/Br-Gly3-γDPGA10 with either 8 or 18 chains per protein and rPA/Cys-Gly3-γDPGA10 with 15 chains per protein.
A comparison of different linkage methods, including those tested previously (22), is presented in Table 2. The best results were obtained by thioether-linked conjugates created between thiolated protein with SPDP and bromoacylated γDPGA or, conversely, bromoacylated protein and SH-γDPGA. These antibody levels were significantly higher over thioether-linked conjugates created using 2-iminothiolane and over hydrazone-linked conjugates (rPA-SH/Br-Gly3-γDPGA10 [GM = 7,206] versus rPA-ITL/Br-Gly3-γDPGA10 [GM = 3,726; P < 0.05]; rPA-SH/Br-Gly3-γDPGA10 versus rPA-CHO/AH-γDPGA15 [GM = 3,004; P < 0.01]; rPA-SH/Br-Gly3-γDPGA10 versus rPA-AH/CHO-Gly3-γDPGA10 [GM = 2,478; P < 0.001]; rPA-Br/Cys-Gly3-γDPGA10 [GM = 5,822] versus rPA-CHO/AH-γDPGA15 [GM = 3,004; P < 0.05]; and rPA-Br/Cys-Gly3-γDPGA10 versus rPA-AH/CHO-Gly3-γDPGA10 [GM = 2,478; P < 0.05]). There were no statistically significant differences between the best thioether-linked conjugate (GM = 7,206) and the aminooxy-linked conjugate (GM = 4,257), but the higher level of antibodies and the ease with which the thioether bond is formed (one less step is required) make the first the better choice.
TABLE 2.
Conjugation method/immunogenicity relationships of conjugates prepared with a 10-mer of γDPGA bound to rPAa
| Conjugate | γDPGA (mol)/ protein (mol) | Protein/γDPGA (wt/wt) | Anti-γDPGA (EU)
|
Anti-rPA (μg/ml)
|
||
|---|---|---|---|---|---|---|
| 2nd injection | 3rd injection | 2nd injection | 3rd injection | |||
| Thioether linkage | ||||||
| rPA-SH/Br-Gly3-γDPGA10 | 14 | 1:0.22 | 4,400 | 7,200 | 0.3 | 66 |
| rPA-Br/Cys-Gly3-γDPGA10 | 22 | 1:0.35 | 2,200 | 5,800 | 2 | 210 |
| rPA-ITL/Br-Gly3-γDPGA10 | 8 | 1:0.13 | 2,300 | 3,700 | 4.7 | 61 |
| Oxime linkage | ||||||
| rPA-CONH2/CHO-Gly3-γDPGA10 | 20 | 1:0.32 | 2,000 | 4,300 | 0.4 | 25 |
| Hydrazone linkage | ||||||
| rPA-CHO/AH-γDPGA15 | 15 | 1:0.36 | 2,200 | 3,000 | 0.2 | 6 |
| rPA-AH/CHO-Gly3-γDPGA10 | 22 | 1:0.34 | 1,000 | 2,500 | 0.3 | 28 |
Five- to 6-week-old NIH general-purpose mice (n = 10) were injected subcutaneously with 2.5 μg of γDPGA as a conjugate 2 weeks apart and exsanguinated 7 days after the second or third injection. IgG anti-γDPGA and anti-rPA were measured by ELISA, and the results are expressed as the geometric means.
The effects of the carrier proteins on immunogenicity are summarized in Table 3. Among all carriers, rPA and TT conjugates produced the best responses to γDPGA (rPA and TT versus BSA [P < 0.001]; rPA and TT versus rEPA [P < 0.01]; and rEPA versus BSA [no statistical difference]). Formulation of the vaccine with aluminum hydroxide significantly increased the antibody response to the carrier protein with minimal significant effect upon the response to γDPGA (Table 4). In only one case (TT/Cys-γDPGA15) did the aluminum hydroxide significantly (P < 0.01) increase the response to γDPGA, rendering it the best conjugate, inducing 14,950 EU. The optimal dose of conjugated γDPGA was between 1.2 and 2.5 μg per mouse (Table 5).
TABLE 3.
Protein carrier/immunogenicity relationships of conjugates prepared with a 10-mer of γDPGA bound to BSA, rPA, rEPA, or TTa
| Conjugate | γDPGA (mol)/ protein (mol) | Anti-γDPGA (EU)
|
Anti-proteinc
|
||
|---|---|---|---|---|---|
| 2nd injection | 3rd injection | 2nd injection | 3rd injection | ||
| BSA/Br-Gly3-γDPGA10 | 18 | 1,900 | 1,800 | 5 | 19 |
| rEPA/Br-Gly3-γDPGA10 | 9 | 930 | 3,200 | 0.6 | 6 |
| rPA/Br-Gly3-γDPGA10 | 14 | 4,400 | 7,200 | 1 | 96 |
| rPA/Cys-Gly3-γDPGA10 | 21 | 5,500 | 7,500 | 0.1 | 2.2 |
| TT/Cys-Gly3-γDPGA10 | 11 | 420 | 7,800 | NTb | NT |
Five- to 6-week-old NIH general-purpose mice (n = 10) were injected subcutaneously with 2.5 μg of γDPGA as a conjugate 2 weeks apart and exsanguinated 7 days after the second or third injection. IgG anti-γDPGA and anti-rPA were measured by ELISA, and the results are expressed as the geometric means.
NT, not tested.
EU for anti-BSA and anti-rEPA and μg/ml for anti-rPA.
TABLE 4.
Formulation/immunogenicity relationships of conjugates prepared with a 10-mer of γDPGA bound to rPA or TTa
| Conjugate | γDPGA (mol)/rPA (mol) | Dose (μg/mouse)b | Anti-γDPGA (EU)
|
Anti-protein (μg/ml)
|
||
|---|---|---|---|---|---|---|
| 2nd injection | 3rd injection | 2nd injection | 3rd injection | |||
| rPA/Cys-Gly3-γDPGA10 | 22 | 2.5 | 2,200 | 5,800 | 2 | 210 |
| 2.5 + al | 3,500 | 6,200 | 80 | 280 | ||
| rPA/Cys-Gly3-γDPGA10 | 13 | 1 | NTc | 2,900 | NT | 61 |
| 1 + form | NT | 2,600 | NT | 23 | ||
| 1 + al | NT | 4,000 | NT | 260 | ||
| 1 + al & form | NT | 3,300 | NT | 300 | ||
| rPA-ITL/Br-Gly3-γDPGA10 | 18 | 2.5 | 2,400 | 3,000 | 0.2 | 41 |
| 2.5 + al | 5,600 | 5,400 | 250 | 680 | ||
| TT/Cys-γDPGA10 | 16 | 2.5 | 6,900 | 6,700 | NT | NT |
| 2.5 + al | 8,310 | NT | NT | NT | ||
| TT/Cys-γDPGA15 | 16 | 2.5 | 6,500 | 7,700 | NT | NT |
| 2.5 + al | 7,800 | 15,000 | NT | NT | ||
Five- to 6-week-old NIH general-purpose mice (n = 10) were injected subcutaneously with 2.5 μg of γDPGA as a conjugate 2 weeks apart and exsanguinated 7 days after the second or third injection. IgG anti-γDPGA and anti-rPA were measured by ELISA, and the results are expressed as the geometric means.
al, aluminium hydroxide (Alhydrogel); form, formaldehyde treatment according to the methods of Porro et al. (19a) and Nencioni et al. (17a).
NT, not tested.
TABLE 5.
Dose/immunogenicity relationships of conjugates prepared with a 10-mer of γDPGA bound to rPAa
| Conjugate | γDPGA (mol)/rPA (mol) | Dose (μg/mouse) | Anti-γDPGA (EU)
|
Anti-rPA (μg/ml)
|
||
|---|---|---|---|---|---|---|
| 2nd injection | 3rd injection | 2nd injection | 3rd injection | |||
| rPA/Cys-Gly3- γDPGA10 | 22 | 0.31 | 490 | 3,500 | 0.3 | 9 |
| 0.63 | 980 | 4,900 | 0.6 | 37 | ||
| 1.25 | 2,300 | 6,200 | 2 | 120 | ||
| 2.5 | 2,200 | 5,800 | 2 | 200 | ||
| 20 | NTb | 3,700 | NT | 440 | ||
Five- to 6-week-old NIH general-purpose mice (n = 10) were injected subcutaneously with 2.5 μg of γDPGA as a conjugate 2 weeks apart and exsanguinated 7 days after the second or third injection. IgG anti-γDPGA and anti-rPA were measured by ELISA, and the results are expressed as the geometric means.
NT, not tested.
Antibody to the protein carrier.
The antibody levels were calculated in ELISA units relative to a standard for each protein, arbitrarily assigned a value of 100 EU for BSA and rEPA and μg/ml for rPA. Therefore, the comparison is possible only within each type of carrier. The responses to protein varied among the conjugates, since the dosage was always based on the amount of γDPGA in the conjugate. Overall, the highest levels were induced by conjugates prepared by thioether linkage between bromoacylated protein and peptide containing terminal cysteine formulated with aluminum hydroxide. The antibody response was directly related to the dosage of the carrier protein.
DISCUSSION
The pathogenicity of B. anthracis requires two essential virulence factors: the tripartite toxin and the γDPGA capsule. The licensed vaccine against anthrax (Anthrax Vaccine Adsorbed) contains the protective antigen, the binding component of the toxin complex (14). The protective effects of the anticapsular antibodies were investigated recently (3, 10, 22).
We have described the preparation of conjugates of synthetic γDPGA peptides with several carrier proteins bound through thioether linkages (22). Peptides of different lengths were used, at an average of 5 to 32 mol of peptide per mol of protein. Unlike γDPGA alone, these conjugates were immunogenic in 5- to 6-week old general-purpose mice when injected at a dosage and schedule relevant for use in humans, and the antibodies induced opsonophagocytic killing of B. anthracis. This finding was confirmed by others (27).
The conjugation techniques, including the types of chemical linkages between the hapten and the protein, as well as the peptide/sugar chain length and the density on the protein, influence the serum antibody response to both components (4, 13, 17, 18, 20). Therefore, we studied several constructs for human use by employing additional methods and formulations of the γDPGA conjugates. Previously, we created thioether bonds between the protein and the γDPGA by introduction of a bromoacyl group (SBAP) or a thiol group (SPDP) into the protein. The activated protein was then bound to a peptide with a thiol or bromoacetyl group at its N or C terminus, respectively. In the present study, we tested (i) thioether bonds generated by derivatization of the protein with thiol groups using 2-iminothiolane, followed by binding to bromoacetyl-peptide; (ii) hydrazone bonds generated by derivatizing the proteins with adipic acid dihydrazide, followed by reaction with benzaldehyde-derivatized peptides or, alternatively, a benzaldehyde group was introduced into the protein using SFB and the formylated protein bound to a hydrazide-derivatized peptide; (iii) oxime bonds created by derivatization of the protein with SBAP, which was then coupled to an aminoxy-thiol linker; the aminooxylated protein was then bound to 4-formylbenzoyl-γDPGA. The immunogenicities of these conjugates in mice were similar to those previously prepared: the optimal density was ∼15 mol γDPGA per mol protein with a peptide chain length of 10 or 15 amino acids. Tetanus toxoid and rPA were better carriers than BSA or rEPA. The most successful and reproducible linkage was formed by introduction of bromoacetyl groups onto the lysine residues of the protein, followed by conjugation with γDPGA equipped with a terminal cysteine residue. A dosage of 1.2 to 2.5 μg of conjugated γDPGA per mouse gave the best γDPGA response. Aluminum hydroxide should be included in the formulation if a high response to rPA or to another carrier protein is needed.
The choice of an anthrax conjugate to be further studied can be evaluated by (i) its immunogenicity, (ii) its yield, and (iii) the ease of preparation. Based on our studies, a highly immunogenic and simple-to-prepare investigational vaccine, inducing antibody to either one γDPGA only (TT/Cys-γDPGA15) or two anthrax virulence factors, γDPGA and PA (rPA/Cys-Gly3-γDPGA10), can be prepared and considered for clinical testing.
Acknowledgments
This research was supported by the Intramural Research Program of the NIH, NICHD.
We thank Vince Pozsgay for synthesizing the oxime linker and Chunyan Gou for technical assistance.
Editor: D. L. Burns
REFERENCES
- 1.Carlsson, J., H. Drevin, and R. Axen. 1978. Protein thiolation and reversible protein-protein conjugation. N-Succinimidyl 3-(2-pyridyldithio)propionate, a new heterobifunctional reagent. Biochem. J. 173:723-737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. 2001. Human anthrax associated with an epizootic among livestock—North Dakota, 2000. Morb. Mortal. Wkly. Rep. 50:677-680. [PubMed] [Google Scholar]
- 3.Chabot, D. J., A. Scorpio, S. A. Tobery, S. F. Little, S. L. Norris, and A. M. Friedlander. 2004. Anthrax capsule vaccine protects against experimental infection. Vaccine 23:43-47. [DOI] [PubMed] [Google Scholar]
- 4.Dick, W. E., and M. Beurret, Jr. 1989. Glycoconjugates of bacterial carbohydrate antigens. A survey and consideration of design and preparation factors. Contrib. Microbiol. Immunol. 10:48-114. [PubMed] [Google Scholar]
- 5.Dragon, D. C., R. P. Rennie, and B. T. Elkin. 2001. Detection of anthrax spores in endemic regions of northern Canada. J. Appl. Microbiol. 91:435-441. [DOI] [PubMed] [Google Scholar]
- 6.Fields, R. 1971. The measurement of amino groups in proteins and peptides. Biochem. J. 124:581-590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goodman, J. W., and D. E. Nitecki. 1966. Immunochemical studies on the poly-gamma-d-glutamyl capsule of Bacillus anthracis. I. Characterization of the polypeptide and of the specificity of its reaction with rabbit antisera. Biochemistry 5:657-663. [DOI] [PubMed] [Google Scholar]
- 8.Johansson, H. J., C. Jagersten, and J. Shiloach. 1996. Large scale recovery and purification of periplasmic recombinant protein from E. coli using expanded bed adsorption chromatography followed by new ion exchange media. J. Biotechnol. 48:9-14. [DOI] [PubMed] [Google Scholar]
- 9.Kaya, A., M. A. Tasyaran, S. Erol, and Z. Ozkurt. 2002. Anthrax in adults and children: a review of 132 cases in Turkey. Eur. J. Clin. Microbiol. Infect. Dis. 21:258-261. [DOI] [PubMed] [Google Scholar]
- 10.Kozel, T. R., W. J. Murphy, S. Brandt, B. R. Blazar, J. A. Lovchik, P. Thorkildson, A. Percival, and C. R. Lyons. 2004. mAbs to Bacillus anthracis capsular antigen for immunoprotection in anthrax and detection of antigenemia. Proc. Natl. Acad. Sci. USA 101:5042-5047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kubler-Kielb, J., and V. Pozsgay. 2005. Synthesis of neoglycoproteins by chemoselective ligation through an aminoxy-thiol heterbifunctional reagent. J. Org. Chem. 70:6987-6990. [DOI] [PubMed] [Google Scholar]
- 12.Kumar, A., R. Kanugo, S. Bhattacharia, S. Badrinath, and R. P. Swaminathan. 2000. Human anthrax in India. J. Commun. Dis. 32:240-246. [PubMed] [Google Scholar]
- 13.Laferriere, C. A., R. K. Sood, J. M. de Muys, F. Michon, and H. J. Jennings. 1998. Streptococcus pneumoniae type 14 polysaccharide-conjugate vaccines: length stabilization of opsonophagocytic conformational polysaccharide epitopes. Infect. Immun. 66:2441-2446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Little, S. F., B. E. Ivins, P. F. Fellows, M. L. M. Pitt, S. L. W. Norris, and G. P. Andrews. 2004. Defining a serological correlate of protection in rabbits for a recombinant anthrax vaccine. Vaccine 22:422-430. [DOI] [PubMed] [Google Scholar]
- 15.Little, S. F., S. H. Leppla, and E. Cora. 1988. Production and characterization of monoclonal antibodies to the protective antigen component of Bacillus anthracis toxin. Infect. Immun. 56:1807-1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lowry, J. O., N. J. Rosenbrough, A. L. Farr, and R. Randall. 1951. Protein measurement with the Folin phenol reagent. J. Biol. Chem. 193:265-275. [PubMed] [Google Scholar]
- 17.Mawas, F., J. Niggemann, C. Jones, M. J. Corbel, J. P. Kamerling, and J. F. Vliegenthart. 2002. Immunogenicity in a mouse model of a conjugate vaccine made with a synthetic single repeating unit of type 14 pneumococcal polysaccharide coupled to CRM197. Infect. Immun. 70:5107-5114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17a.Nencioni, L., G. Volpini, S. Peppoloni, M. Bugnoli, T. De Magistris, I. Marsili, and R. Rappuoli. 1991. Properties of pertussis toxin mutant PT-9K/129G after formaldehyde treatment. Infect. Immun. 59:625-630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nussenzweig, R. S., and V. Nussenzweig. 1989. Antisporozoite vaccine for malaria: experimental basis and current status. Rev. Infect. Dis. Suppl. 3:S579-S585. [DOI] [PubMed] [Google Scholar]
- 19.Plikaytis, B. D., P. F. Holder, and G. M. Carlone. 1996. User's manual 12, version 1.00. Centers for Disease Control and Prevention, Atlanta, Ga.
- 19a.Porro, M., M. Saletti, L. Nencioni, L. Tagliaferri, and I. Marsili. 1980. Immunogenic correlation between cross-reacting material (CRM197) produced by a mutant of Corynebacterium diphtheriae and diphtheria toxoid. J. Infect. Dis. 142:716-724. [DOI] [PubMed] [Google Scholar]
- 20.Pozsgay, V., C. Chu, L. Pannell, J. Wolfe, J. B. Robbins, and R. Schneerson. 1999. Protein conjugates of synthetic saccharides elicit higher levels of serum IgG lipopolysaccharide antibodies in mice than do those of the O-specific polysaccharide from Shigella dysenteriae type 1. Proc. Natl. Acad. Sci. USA 96:5194-5197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ramirez, D. M., S. H. Leppla, R. Schneerson, and J. Shiloach. 2002. Production, recovery and immunogenicity of the protective antigen from a recombinant strain of Bacillus anthracis. J. Ind. Microbiol. Biotechnol. 28:232-238. [DOI] [PubMed] [Google Scholar]
- 22.Schneerson, R., J. Kubler-Kielb, T. Y. Liu, Z. D. Dai, A. Yergey, P. Backlund, J. Shiloach, S. H. Leppla, F. Majadly, and J. B. Robbins. 2003. Poly-γ-d-glutamic acid protein conjugates induce IgG antibodies in mice to the capsule of Bacillus anthracis: a potential addition to the anthrax vaccine. Proc. Natl. Acad. Sci. USA 100:8945-8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schneerson, R., O. Barrera, A. Sutton, and J. B. Robbins. 1980. Preparation, characterization, and immunogenicity of Haemophilus influenzae type b polysaccharide-protein conjugates. J. Exp. Med. 152:361-376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Smego, R. A., B. Gebrian, and G. Desmangels. 1998. Cutaneous manifestations of anthrax in rural Haiti. Clin. Infect. Dis. 26:97-102. [DOI] [PubMed] [Google Scholar]
- 25.Sterne, M. 1939. The use of anthrax vaccines prepared from avirulent (unencapsulated) variants of Bacillus anthracis. Onerstepoort J. Vet. Sci. Anim. Ind. 13:307-312. [Google Scholar]
- 26.Troy, F. A. 1973. Chemistry and biosynthesis of the poly(gamma-d-glutamyl) capsule in Bacillus licheniformis. II. Characterization and structural properties of the enzymatically synthesized polymer. J. Biol. Chem. 248:305-315. [PubMed] [Google Scholar]
- 27.Wang, T. T., P. F. Fellows, T. J. Leighton, and A. H. Lucas. 2004. Induction of opsonic antibodies to the gamma-d-glutamic acid capsule of Bacillus anthracis by immunization with a synthetic peptide-carrier protein conjugate. FEMS Immunol. Med. Microbiol. 40:231-237. [DOI] [PubMed] [Google Scholar]