Abstract
Several vaccine technologies were evaluated for their abilities to induce anti-human immunodeficiency virus Gag immune responses in rhesus macaques. While no vaccine alone was able to induce broad and strong immune responses, these were achieved by priming with Gag DNA and boosting with Gag protein adsorbed to polylactide coglycolide microparticles. This regimen elicited strong antibodies, helper T cells, and cytotoxic T lymphocytes and thus holds promise as an effective vaccination scheme.
Various immune effector mechanisms are considered to be important for protection against human immunodeficiency virus (HIV). Neutralizing antibodies are thought to be sufficient for protection against challenge in primate models, as passive transfer of various human monoclonal antibodies protects animals from subsequent challenge (16-18). In addition, partial protection of macaques was achieved by vaccination with DNA and adjuvant protein vaccines in a priming-boosting regimen, despite depletion of CD8+ T cells at the time of challenge (5). Similarly, cytotoxic T lymphocyte (CTL) responses are sufficient for partial protection in these models. Such protective CTL responses have been conferred by various vaccine technologies, without the induction of detectable neutralizing antibodies (1, 2, 9, 14, 19, 25, 29). In addition, certain vaccines based on Gag and/or Pol, which would not be expected to induce virus-neutralizing activity, are partially protective (7, 33, 34). Finally, depletion of CD8+ T cells through infusion of anti-CD8 antibodies decreases the control of viremia in infected macaques (11, 20, 32). Thus, both humoral and cellular immunity seem to play a role in protection in primate disease models. The importance of CTLs in protection from AIDS in humans is suggested by the inverse correlation between anti-HIV CTLs and virus load (3, 4, 15, 39) and the high levels of CTLs in chronically exposed, but protected, individuals (8). In addition to antibodies and CTLs, a robust helper-T-cell response is likely important for the expansion of antigen-specific B-cell and CTL populations and possibly also for provision of antiviral cytokines. Thus, an effective preventative HIV vaccine will likely require the ability to induce broad and potent immune responses, including neutralizing antibodies, CD4+-T-cell responses, and CTLs.
To this end, various vaccine technologies have been tested as potential HIV vaccines, with various results. In this study, we have compared several distinct vaccine technologies for their abilities to induce anti-HIV immune responses. First, recombinant proteins, by themselves, are not usually particularly immunogenic and require adjuvants for effectiveness. We have found recently that particle-based delivery systems, such as polylactide coglycolide (PLG), are very effective in small-animal models at enhancing immune responses induced by protein-based vaccines (13). Specifically, anti-HIV Gag antibody responses were increased and, interestingly, CTL responses were induced, which is not typically seen with protein-based vaccines alone. Second, virus-like particles have been found to be effective for inducing antibody and CTL responses in various animal models, including primate models of HIV (21, 23, 26). To enhance these responses, we have incorporated the adjuvant LTK63, which is a mutated form of Escherichia coli heat-labile enterotoxin that retains adjuvant activity while eliminating toxicity (27). We have recently shown this adjuvant to be effective at inducing CTLs in mice when it was administered in combination with HIV Gag protein (22). Finally, DNA vaccines have been demonstrated to be very effective at priming CTL responses in species ranging from mice (6, 10, 36) to humans (31, 37). Thus, we evaluated each of these distinct technologies (Table 1) for the induction of immune responses in rhesus macaques.
TABLE 1.
Immunization regimena
| Group | No. of macaques | Vaccine | Time of vaccination (wk) |
|---|---|---|---|
| 1 | 3 | p55Gag | 0, 4, 8 |
| 2 | 4 | p55Gag-PLG + LTK63 | 0, 4, 8, 41 |
| 3 | 4 | VLP | 0, 4, 8 |
| 4 | 4 | VLP + LTK63 | 0, 4, 8 |
| 5 | 4 | pCMVgagmod | 0, 4, 8, 41b |
Rhesus macaques (Southwest Foundation for Biomedical Research, San Antonio, Tex.) were immunized in the quadriceps and/or deltoid muscles. Yeast-derived recombinant p55Gag protein was administered in saline (group 1) or adsorbed to PLG microparticles (17, 29) and mixed with 0.1 mg of a purified recombinant mutant form of E. coli heat-labile enterotoxin (LTK63) at a final dose of 0.2 mg of Gag (group 2). VLP were produced in and purified from a Tn5 baculovirus expression system (10, 28, 40) and administered in phosphate-buffered saline (group 3) or mixed with 0.1 mg of LTK63 at a final dose of 0.2 mg of VLP (group 4). The pCMV gagmod DNA vaccine, containing a sequence-modified HIV-1 Gag protein from SF2 (40), was administered at a dose of 1 mg of DNA (group 5).
At week 41, all four animals primed with Gag DNA were given a booster injection with p55Gag=PLG.
Priming immune responses.
First, as one indicator of vaccine potency, anti-Gag antibodies were measured by enzyme-linked immunosorbent assay. As shown in Table 2, two vaccinations with p55Gag adsorbed to PLG microparticles (Gag-PLG) (group 2) induced high Gag-specific plasma antibody titers in all four macaques (geometric mean titer [GMT], 16,200). After a third dose of Gag-PLG, Gag-specific titers exceeded 100,000 in two of four animals. As expected, Gag protein alone (group 1) was only weakly immunogenic, indicating that the PLG microparticle formulation conferred a substantial benefit (P = 0.03; one-tailed t test), as was seen previously for small animals (31, 35). Gag virus-like particles (VLP) (group 3) induced low to moderate antibody titers (the GMT was 2,300 at 2 weeks after the second immunization) that were not increased by coadministration of LTK63 (for group 4, the GMT was 400). A third vaccination with VLP or VLP plus LTK63 did not increase Gag-specific antibody titers, indicating the relatively modest immunogenicity of VLP. As has been observed with various other DNA vaccines, vaccination with the pCMVgagmod plasmid DNA (group 5) induced a low level of Gag-specific antibody in only one of four rhesus macaques.
TABLE 2.
Antibody responses
| Vaccine | Macaque | Antibody titera
|
|||||
|---|---|---|---|---|---|---|---|
| Wk 6, 2 wks after second vaccination | Wk 10, 2 wks after third vaccination | Wk 14, 6 wks after third vaccination | Wk 22, 14 wks after third vaccination | Wk 43, 2 wks after booster injection | Wk 49, 6 wks after booster injection | ||
| p55Gag | 59 | 9,300 | 5,600 | 1,300 | 300 | ||
| 69 | 1,400 | 2,400 | 400 | <25 | |||
| 74 | 100 | 100 | <25 | <25 | |||
| p55Gag-PLG + LTK63b | 62 | 9,100 | 3,100 | 900 | 100 | 5,800 | 2,000 |
| 67 | 14,600 | 111,100 | 22,600 | 3,900 | 48,600 | 16,300 | |
| 72d | 35,800 | 159,900 | 26,300 | 11,400 | 51,700 | 17,200 | |
| 73 | 14,600 | 5,900 | 1,200 | 100 | 6,700 | 3,100 | |
| VLP | 61 | 2,300 | 2,400 | 300 | 200 | ||
| 66 | 2,100 | 1,700 | 400 | 200 | |||
| 71 | 4,100 | 1,500 | 600 | 100 | |||
| 76 | 1,300 | 400 | <25 | <25 | |||
| VLP + LTK63 | 60 | 1,100 | 400 | 100 | <25 | ||
| 65 | 200 | 100 | <25 | <25 | |||
| 70 | 400 | 200 | <25 | <25 | |||
| 75 | 300 | 800 | 100 | 100 | |||
| pCMV gagmodc | 63 | 200 | 900 | 500 | 200 | 17,300 | 13,600 |
| 68 | <25 | <25 | <25 | <25 | 800 | 600 | |
| 77 | <25 | <25 | <25 | <25 | 400 | 400 | |
| 78 | <25 | 100 | <25 | <25 | 1,600 | 900 | |
Anti-Gag antibodies were measured by enzyme-linked immunosorbent assay. Plasma antibody titers (reciprocal of serum dilution at an absorbance value of 0.5) are rounded to the nearest 100. All animals before vaccination showed no reactivity at the lowest dilution (1:25).
Animals were given a booster injection at week 41 of 0.2 mg of p55Gag protein adsorbed to sodium dodecyl sulfate (SDS)-PLG microparticles plus 0.1 mg of LTK63.
Animals were given a booster injection at week 41 of 0.2 mg of p55Gag, protein adsorbed to SDS-PLG microparticles (without LTK63).
Rhesus macaque 72 also received VLP at the time of the third immunization.
Second, to determine the magnitude of T-cell responses and the spectrum of p55Gag epitopes recognized by T cells, we utilized recombinant Gag protein and synthetic peptides that were 20 amino acids (aa) in length, overlapped each other by 10 aa, and derived from p55Gag of HIV-1SF2. Beginning 6 weeks after the third immunization, we determined Gag-specific lymphoproliferative responses as a measure of antigen-specific CD4+8−-T-cell activity (Table 3). All four rhesus macaques given Gag-PLG plus LTK63 (group 2) demonstrated proliferative responses to p55Gag (stimulation index [SI] range, 4 to 138) that were maintained for at least 14 weeks after the third immunization (SI range, 4 to 68). Interestingly, those with the highest proliferative responses (macaques 67 and 72) also had the highest titers of anti-Gag antibodies (Table 2). Gag-specific proliferation was not observed in animals immunized with Gag protein alone (group 1) or VLP (group 3), and only weak responses were observed in two animals immunized with VLP plus LTK63 (group 4) (macaques 65 and 70). Marginal Gag-specific lymphoproliferation was observed in the plasmid DNA-immunized rhesus macaque 14 weeks after the third immunization, with the exception of rhesus macaque 63, which had an SI of 22. Interestingly, this animal was the only one of its group to show a consistently positive antibody titer (Table 2).
TABLE 3.
Gag-specific lymphoproliferation
| Vaccine | Macaque | SIa
|
|||
|---|---|---|---|---|---|
| Wk 14, 6 wks after third vaccination | Wk 22, 14 wks after third vaccination | Wk 43, 2 wks after booster injection | Wk 49, 6 wks after booster injection | ||
| p55Gag | 59 | 2 | |||
| 69 | 1 | ||||
| 74 | 1 | ||||
| p55Gag-PLG + LTK63b | 62 | 4 | 11 | 13 | 6 |
| 67 | 41 | 56 | 110 | 162 | |
| 72d | 138 | 68 | 40 | 92 | |
| 73 | 16 | 4 | 39 | 28 | |
| VLP | 61 | 1 | |||
| 66 | 1 | ||||
| 71 | 2 | ||||
| 76 | 1 | ||||
| VLP + LTK63 | 60 | 1 | |||
| 65 | 4 | ||||
| 70 | 10 | ||||
| 75 | 1 | ||||
| pCMVgagmodc | 63 | 22 | 37 | 17 | |
| 68 | 3 | 4 | 4 | 12 | |
| 77 | 4 | 25 | 29 | ||
| 78 | 2 | 21 | 9 | ||
Lymphoproliferation was measured in PBMC (5), and results are presented as SIs. Because of the limited amounts of blood that could be obtained, it was not possible to assess proliferative activity in all the animals at all time points.
Animals were given a booster injection at week 41 of 0.2 mg of p55Gag protein adsorbed to SDS-PLG microparticles plus 0.1 mg of LTK63.
Animals were given a booster injection at week 41 of 0.2 mg of p55Gag protein adsorbed to SDS-PLG microparticles (without LTK63).
Rhesus macaque 72 also received VLP at the time of the third immunization.
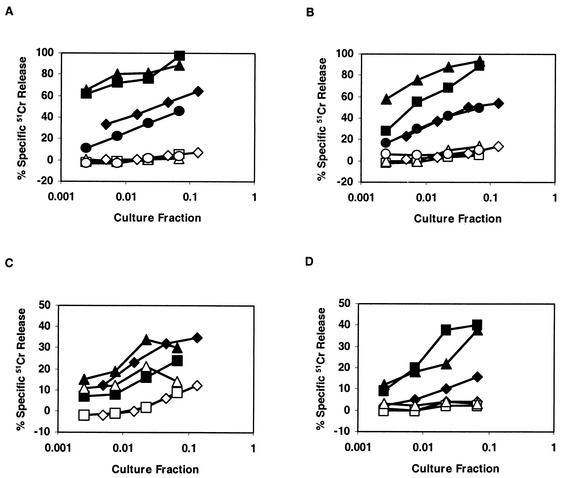
Beginning 2 weeks after the second immunization, animals were evaluated for CTL activity by a 51Cr release assay using peripheral blood mononuclear cells (PBMC) cultured for 8 days in the presence of autologous recombinant vaccinia virus (rVV) gag-pol-infected PBMC or individual pools of overlapping Gag peptides. The cultures were harvested and assayed for cytolytic activity against autologous 51Cr-labeled B-lymphoblastoid cell line (B-LCL) targets that were pulsed with Gag peptide pools. As shown in Table 4, immunization with Gag protein (alone) did not induce CTLs, with the exception of a weak response (macaque 74) (19% Gag-specific 51Cr release maximum) in a single instance. Likewise, only one of the four animals (macaque 72) that was vaccinated with Gag-PLG microparticles plus LTK63 showed CTL activity and only after the third immunization; however, this animal had mistakenly also received a dose of VLP at the time of its third immunization. Hence, we cannot be certain that any CTLs were induced by the p55Gag-PLG plus LTK63 vaccine alone. Gag-specific CTL activity was detected in approximately half of the animals vaccinated with VLP or VLP plus LTK63 and in all four rhesus macaques vaccinated with plasmid DNA. With the exception of macaque 72, all animals that showed CTL activity 2 weeks after the third immunization maintained that activity for at least 12 additional weeks (14 weeks after the third immunization) (Table 4). Moreover, when the DNA-immunized rhesus macaques were evaluated 23 to 24 weeks after the third dose, all four animals remained CTL positive. In general, it appears that CTL activity was boosted by the third immunization, as was seen by higher levels of lytic activity at 6 and 14 weeks after the third immunization than at 2 weeks after the second immunization (Fig. 1). However, CTL responses eventually declined, as was seen by lower levels of lytic activity by 23 weeks after the third immunization. Because the 51Cr-labeled B-LCL targets were pulsed with peptide pools spanning distinct portions of the entire Gag protein sequence, we could determine whether Gag vaccines induced CTL populations that reacted with single or multiple discrete epitopes. As shown in Table 5, Gag peptide pools 1, 2, 4, 5, and 8 contained epitopes recognized by one or more of the CTL-positive rhesus macaques. In addition, two of the plasmid-immunized rhesus macaques (macaque 63 and macaque 77) contained CTLs that reacted with three separate Gag peptide pools. Further analysis using target cells pulsed with individual peptides revealed the presence of multiple epitopes. Three peptides in pool 1 (p55Gag aa 1 to 80) and at least two peptides in pool 5 (p55Gag aa 194 to 263) were recognized; however, only a single peptide in pool 4 (p55Gag aa 254 to 323) was identified. In the case of DNA immunization, priming of Gag-specific CTLs in vivo resulted from the CTL precursor recognition of Gag epitopes derived from the processing and presentation of endogenously synthesized Gag. However, CTL effectors were derived by culture with synthetic Gag peptides and were assayed against peptide-pulsed autologous target cells. Nevertheless, peptide-stimulated CTLs derived from the PBMC of DNA-immunized rhesus macaques were also able to recognize and lyse target cells that expressed Gag endogenously (data not shown).
TABLE 4.
Peripheral blood CTL responses
| Vaccine | Macaque | Gag-specific CTL activitya
|
|||||
|---|---|---|---|---|---|---|---|
| Wk 6, 2 wks after second vaccination | Wk 10, 2 wks after third vaccination | Wk 14, 6 wks after third vaccination | Wk 22, 14 wks after third vaccination | Wk 32, 24 wks after third vaccination | Wk 43, 2 wks after booster injection | ||
| p55Gag | 59 | − | − | ||||
| 69 | − | − | |||||
| 74 | − | − | + | ||||
| p55Gag-PLG + LTK63 | 62 | − | − | ||||
| 67 | − | − | |||||
| 72b | − | − | + | + | − | ||
| 73 | − | − | |||||
| 61 | − | − | − | ||||
| VLP | 66 | + | − | + | + | ||
| 71 | + | + | + | + | |||
| 76 | − | − | + | ||||
| 60 | − | − | |||||
| VLP + LTK63 | 65 | − | − | ||||
| 70 | + | + | + | + | |||
| 75 | + | + | + | + | |||
| PCMVgagmodc | 63 | + | + | + | + | + | + |
| 68 | + | + | + | + | + | + | |
| 77 | + | + | + | + | |||
| 78 | + | + | + | + | − | ||
Cytolysis was measured in peptide-pulsed or rVV gag-pol-infected autologous B-LCL that had been stimulated with PBMC treated with Gag peptides or infected with rVV gag-pol. All animals showed no Gag-specific 51Cr release before vaccinations. +, ≥10% Gag-specific 51Cr release at two consecutive effector-to-target ratios; no + or −, data not determined.
Rhesus macaque 72 was also given VLP at the time of the third immunization.
Animals received booster immunization of p55Gag protein (0.2 mg)-PLG.
FIG. 1.
Durable cytolytic activity from cultured PBMC collected after two or three vaccinations. Filled symbols: antigen-specific CTLs, open symbols: negative control. (A) Pool 4 (aa 254 to 323)-specific CTLs from rhesus macaque 63 2 weeks after the second vaccination (⧫, ◊), 6 weeks after the third vaccination (▪, □), 14 weeks after the third vaccination (▴, Δ), and 23 weeks after the third vaccination (•, ○); (B) pool 4-specific CTLs from rhesus macaque 68 2 weeks after the second vaccination (⧫, ◊), 2 weeks after the third vaccination (▪, □), 6 weeks after the third vaccination (▴, Δ), and 23 weeks after the third vaccination (•, ○); (C) pool 5 (aa 314 to 365)-specific CTLs from rhesus macaque 66 2 weeks after the second vaccination (⧫, ◊), 6 weeks after the third vaccination (▪, □), and 14 weeks after the third vaccination (▴, Δ); (D) pool 4-specific CTLs from rhesus macaque 70 2 weeks after the third vaccination (⧫, ◊), 6 weeks after the third vaccination (▪, □), and 14 weeks after the third vaccination (▴, Δ).
TABLE 5.
Gag-specific CTL repertoire
| Macaque | Vaccine | CTL reactivity in p55Gag peptide poola:
|
||||
|---|---|---|---|---|---|---|
| 1 | 2 | 4 | 5 | 8 | ||
| 74 | p55Gag | + | ||||
| 72b | p55Gag-PLG + LTK63 | + | ||||
| 66 | VLP | p24.13 | ||||
| p24.14 | ||||||
| 71 | VLP | p17.6 | ||||
| 76 | VLP | + | ||||
| 70 | VLP + LTK63 | p24.9 | ||||
| 75 | VLP + LTK63 | p24.13 | ||||
| 63 | pCMVgagmod | p17.4 | p24.9 | + | ||
| 68 | pCMVgagmod | p24.9 | ||||
| 77 | pCMVgagmod | p17.3 | p24.17 | + | ||
| 78 | pCMVgagmod | p17.13 | ||||
There was no CTL reactivity with pools 3, 6, and 7. +, there was CTL reactivity with the peptide pool, but the specific peptide was not identified. CTL reactivities with specific peptides were as follows: with LRPGGKKKYKLKHIVWASRE, p17.3; with LKHIVWASRELERFAVNPGI, p17.4; with LETSEGCRQILGQLQPSLQT, p17.6; with AAGTGNSSQVSQNYPIVQNI, p17.13; with WDRVHPVHAGPIAPGQMREP, p24.9; with NNPPIPVGEIYKRWIILGLN, p24.13; with YRRWIILGLNKIVRMYSPTS, p24.14; and with PFRDYVDRFYKTLRAEQASO, p24.17.
Rhesus macaque 72 also received VLP at the time of the third immunization.
Broadening of immune responses by priming with DNA and boosting with Gag-PLG.
Although plasmid DNA was the best of the vaccines at inducing CTLs, it is likely that a successful HIV vaccine must also induce CD4+ T cells with the capacity for providing help for proliferation and differentiation of HIV-reactive CTLs and B cells (12, 28, 30). To determine if lymphoproliferative and antibody responses could be increased in the plasmid DNA-immunized rhesus macaques, the animals were given a single dose of Gag protein adsorbed to PLG microparticles at week 41. In this case, the LTK63 adjuvant was not included since it did not enhance the proliferative or antibody responses after immunization with VLP. Lymphoproliferation assays were performed at 2 and 6 weeks after the booster dose. After protein boosting, four DNA-primed animals had increased Gag-specific lymphoproliferation and concomitant increases in antibodies. For the group, the geometric mean SI (Table 3) increased from 5 (week 22) to 15 to 17 (weeks 43 and 49) (P = 0.07; one-tailed t test). Likewise, Gag antibody titers (Table 2) increased 16- to 90-fold (P = 0.004; one-tailed t test). Interestingly, animal 63, the only one to exhibit Gag-specific antibodies after DNA immunization alone, showed the highest levels of antigen-specific proliferation and antibodies after the boosting.
Because the animals primed with the Gag-PLG plus LTK63 protein-adjuvant combination had strong lymphoproliferative and antibody responses, they were given a boosting dose at week 41. As shown in Tables 2 and 3, 2 weeks after the fourth immunization with Gag-PLG plus LTK63, all four animals showed strong proliferative responses (SI range, 13 to 110) and high antibody titers (5,800 to 51,700). These responses changed very little by 6 weeks after the fourth immunization. Using the Gag peptide pools to elicit lymphoproliferation, we identified several stimulatory peptide pools, and in animals 67 and 72 we observed proliferation in response to several distinct pools, indicating a polyepitope-specific repertoire (data not shown). A limited analysis of the frequency and phenotype of the Gag-specific T-cell response by flow cytometry demonstrated gamma interferon and tumor necrosis factor alpha production with a frequency of up to 0.8% of CD4 T cells (data not shown).
The vaccine technologies that we evaluated for this rhesus macaque study included recombinant protein administered with a microparticle-based delivery system (PLG), LTK63 adjuvant, VLP, and plasmid DNA. Each of these technologies was chosen for its potential to overcome the hurdle of priming CTL responses without the use of a live vector system (based on results of small-animal studies) (13, 21-24, 26, 35, 40), thereby providing broad immune responses with a relatively simple vaccine. However, as is clear from the data reported here, these technologies had very different abilities to prime immune responses in rhesus macaques, with none of them alone being able to prime broad and strong immune responses. Gag DNA was the most potent technology for CTL induction, while Gag protein adsorbed to PLG microparticles was best for antibody and helper-T-cell responses. These results suggested possible synergy between the DNA and Gag-PLG vaccine technologies for providing strong and broad immune responses. Indeed, priming with Gag DNA and boosting with Gag-PLG achieved high levels of anti-Gag antibodies, helper T cells, and CTLs. It is likely that these broad responses were due, at least in part, to the complementary nature of the two technologies. DNA vaccines produce small amounts of antigen expressed appropriately for efficient priming of CTLs, and Gag-PLG provides a bolus of antigen delivered efficiently for the induction of robust antibodies and helper T cells. The strong synergy with Gag DNA priming and boosting with Gag protein adsorbed to PLG microparticles suggests the utility of this vaccine strategy for providing broad and strong immune responses without the need for a live vector system. Furthermore, this strategy is amenable to additional enhancement with improved DNA vaccine delivery, as has been recently observed (24, 35, 38).
Acknowledgments
We thank Steve Hardy for recombinant adenovirus, Barbara Doe for assistance with CTL assays, and Robert Geiger and Kathy Brasky (Southwest Foundation for Biomedical Research) for vaccinations, phlebotomy, and animal care.
REFERENCES
- 1.Barouch, D. H., S. Santra, M. J. Kuroda, J. E. Schmitz, R. Plishka, A. Buckler-White, A. E. Gaitan, R. Zin, J. H. Nam, L. S. Wyatt, M. A. Lifton, C. E. Nickerson, B. Moss, D. C. Montefiori, V. M. Hirsch, and N. L. Letvin. 2001. Reduction of simian-human immunodeficiency virus 89.6P viremia in rhesus monkeys by recombinant modified vaccinia virus Ankara vaccination. J. Virol. 75:5151-5158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barouch, D. H., S. Santra, J. E. Schmitz, M. J. Kuroda, T. M. Fu, W. Wagner, M. Bilska, A. Craiu, X. X. Zheng, G. R. Krivulka, K. Beaudry, M. A. Lifton, C. E. Nickerson, W. L. Trigona, K. Punt, D. C. Freed, L. Guan, S. Dubey, D. Casimiro, A. Simon, M. E. Davies, M. Chastain, T. B. Strom, R. S. Gelman, D. C. Montefiori, M. G. Lewis, E. A. Emini, J. W. Shiver, and N. L. Letvin. 2000. Control of viremia and prevention of clinical AIDS in rhesus monkeys by cytokine-augmented DNA vaccination Science 290:486-492. [DOI] [PubMed] [Google Scholar]
- 3.Betts, M. R., J. F. Krowka, T. B. Kepler, M. Davidian, C. Christopherson, S. Kwok, L. Louie, J. Eron, H. Sheppard, and J. A. Frelinger. 1999. Human immunodeficiency virus type 1-specific cytotoxic T lymphocyte activity is inversely correlated with HIV type 1 viral load in HIV type 1-infected long-term survivors. AIDS Res. Hum. Retrovir. 15:1219-1228. [DOI] [PubMed] [Google Scholar]
- 4.Borrow, P., H. Lewicki, B. H. Hahn, G. M. Shaw, and M. B. Oldstone. 1994. Virus-specific CD8+ cytotoxic T-lymphocyte activity associated with control of viremia in primary human immunodeficiency virus type 1 infection. J. Virol. 68:6103-6110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cherpelis, S., I. Shrivastava, A. Gettie, X. Jin, D. D. Ho, S. W. Barnett, and L. Stamatatos. 2001. DNA vaccination with the human immunodeficiency virus type 1 SF162ΔV2 envelope elicits immune responses that offer partial protection from simian/human immunodeficiency virus infection to CD8+-T-cell-depleted rhesus macaques. J. Virol. 75:1547-1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donnelly, J. J., J. B. Ulmer, J. W. Shiver, and M. A. Liu. 1997. DNA vaccines. Annu. Rev. Immunol. 15:617-648. [DOI] [PubMed] [Google Scholar]
- 7.Egan, M. A., W. A. Charini, M. J. Kuroda, J. E. Schmitz, P. Racz, K. Tenner-Racz, K. Manson, M. Wyand, M. A. Lifton, C. E. Nickerson, T. Fu, J. W. Shiver, and N. L. Letvin. 2000. Simian immunodeficiency virus (SIV) gag DNA-vaccinated rhesus monkeys develop secondary cytotoxic T-lymphocyte responses and control viral replication after pathogenic SIV infection. J. Virol. 74:7485-7495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fowke, K. R., R. Kaul, K. L. Rosenthal, J. Oyugi, J. Kimani, W. J. Rutherford, N. J. Nagelkerke, T. B. Ball, J. J. Bwayo, J. N. Simonsen, G. M. Shearer, and F. A. Plummer. 2000. HIV-1-specific cellular immune responses among HIV-1-resistant sex workers. Immunol. Cell Biol. 78:586-595. [DOI] [PubMed] [Google Scholar]
- 9.Fuller, D. H., P. A. Rajakumar, L. A. Wilson, A. M. Trichel, J. T. Fuller, T. Shipley, M. S. Wu, K. Weis, C. R. Rinaldo, J. R. Haynes, and M. Murphey-Corb. 2002. Induction of mucosal protection against primary, heterologous simian immunodeficiency virus by a DNA vaccine. J. Virol. 76:3309-3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gurunathan, S., D. M. Klinman, and R. A. Seder. 2000. DNA vaccines: immunology, application, and optimization. Annu. Rev. Immunol. 18:927-974. [DOI] [PubMed] [Google Scholar]
- 11.Jin, X., D. E. Bauer, S. E. Tuttleton, S. Lewin, A. Gettie, J. Blanchard, C. E. Irwin, J. T. Safrit, J. Mittler, L. Weinberger, L. G. Kostrikis, L. Zhang, A. S. Perelson, and D. D. Ho. 1999. Dramatic rise in plasma viremia after CD8+ T cell depletion in simian immunodeficiency virus-infected macaques J. Exp. Med. 189:991-998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kalams, S. A., S. P. Buchbinder, E. S. Rosenberg, J. M. Billingsley, D. S. Colbert, N. G. Jones, A. K. Shea, A. K. Trocha, and B. D. Walker. 1999. Association between virus-specific cytotoxic T-lymphocyte and helper responses in human immunodeficiency virus type 1 infection. J. Virol. 73:6715-6720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kazzaz, J., J. Neidleman, M. Singh, G. Ott, and D. T. O'Hagan. 2000. Novel anionic microparticles are a potent adjuvant for the induction of cytotoxic T lymphocytes against recombinant p55 gag from HIV-1. J. Control. Release 67:347-356. [DOI] [PubMed] [Google Scholar]
- 14.Kim, J. J., J. S. Yang, L. K. Nottingham, D. J. Lee, M. Lee, K. H. Manson, M. S. Wyand, J. D. Boyer, K. E. Ugen, and D. B. Weiner. 2001. Protection from immunodeficiency virus challenges in rhesus macaques by multicomponent DNA immunization. Virology 285:204-217. [DOI] [PubMed] [Google Scholar]
- 15.Koup, R. A., J. T. Safrit, Y. Cao, C. A. Andrews, G. McLeod, W. Borkowsky, C. Farthing, and D. D. Ho. 1994. Temporal association of cellular immune responses with the initial control of viremia in primary human immunodeficiency virus type 1 syndrome. J. Virol. 68:4650-4655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mascola, J. R. 2002. Passive transfer studies to elucidate the role of antibody-mediated protection against HIV-1. Vaccine 20:1922-1925. [DOI] [PubMed] [Google Scholar]
- 17.Mascola, J. R., M. G. Lewis, G. Stiegler, D. Harris, T. C. VanCott, D. Hayes, M. K. Louder, C. R. Brown, C. V. Sapan, S. S. Frankel, Y. Lu, M. L. Robb, H. Katinger, and D. L. Birx. 1999. Protection of macaques against pathogenic simian/human immunodeficiency virus 89.6PD by passive transfer of neutralizing antibodies. J. Virol. 73:4009-4018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mascola, J. R., G. Stiegler, T. C. VanCott, H. Katinger, C. B. Carpenter, C. E. Hanson, H. Beary, D. Hayes, S. S. Frankel, D. L. Birx, and M. G. Lewis. 2000. Protection of macaques against vaginal transmission of a pathogenic HIV-1/SIV chimeric virus by passive infusion of neutralizing antibodies. Nat. Med. 6:207-210. [DOI] [PubMed] [Google Scholar]
- 19.Matano, T., M. Kano, H. Nakamura, A. Takeda, and Y. Nagai. 2001. Rapid appearance of secondary immune responses and protection from acute CD4 depletion after a highly pathogenic immunodeficiency virus challenge in macaques vaccinated with a DNA prime/Sendai virus vector boost regimen. J. Virol. 75:11891-11896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matano, T., R. Shibata, C. Siemon, M. Connors, H. C. Lane, and M. A. Martin. 1998. Administration of an anti-CD8 monoclonal antibody interferes with the clearance of chimeric simian/human immunodeficiency virus during primary infections of rhesus macaques. J. Virol. 72:164-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Montefiori, D. C., J. T. Safrit, S. L. Lydy, A. P. Barry, M. Bilska, H. T. Vo, M. Klein, J. Tartaglia, H. L. Robinson, and B. Rovinski. 2001. Induction of neutralizing antibodies and gag-specific cellular immune responses to an R5 primary isolate of human immunodeficiency virus type 1 in rhesus macaques. J. Virol. 75:5879-5890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neidleman, J. A., M. Vajdy, M. Ugozzoli, G. Ott, and D. O'Hagan. 2000. Genetically detoxified mutants of heat-labile enterotoxin from Escherichia coli are effective adjuvants for induction of cytotoxic T cell responses against HIV-1 gag-p55. Immunology 101:154-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Notka, F., C. Stahl-Hennig, U. Dittmer, H. Wolf, and R. Wagner. 1999. Accelerated clearance of SHIV in rhesus monkeys by virus-like particle vaccines is dependent on induction of neutralizing antibodies. Vaccine 18:291-301. [DOI] [PubMed] [Google Scholar]
- 24.O'Hagan, D., M. Singh, M. Ugozzoli, C. Wild, S. Barnett, M. Chen, G. R. Otten, and J. B. Ulmer. 2001. Induction of potent immune responses by cationic microparticles with adsorbed HIV DNA vaccines. J. Virol. 75:9037-9043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pal, R., D. Venzon, N. L. Letvin, S. Santra, D. C. Montefiori, N. R. Miller, E. Tryniszewska, M. G. Lewis, T. C. VanCott, V. Hirsch, R. Woodward, A. Gibson, M. Grace, E. Dobratz, P. D. Markham, Z. Hel, J. Nacsa, M. Klein, J. Tartaglia, and G. Franchini. 2002. ALVAC-SIV-gag-pol-env-based vaccination and macaque major histocompatibility complex class I (A*01) delay simian immunodeficiency virus SIVmac-induced immunodeficiency. J. Virol. 76:292-302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paliard, X., Y. Liu, R. Wagner, H. Wolf, J. Baenziger, and C. M. Walker. 2000. Priming of strong, broad, and long-lived HIV type 1 p55gag-specific CD8+ cytotoxic T cells after administration of a virus-like particle vaccine in rhesus macaques. AIDS Res. Hum. Retrovirus. 16:273-282. [DOI] [PubMed] [Google Scholar]
- 27.Pizza, M., M. M. Giuliani, M. R. Fontana, G. Douce, G. Dougan, and R. Rappuoli. 2000. LTK63 and LTR72, two mucosal adjuvants ready for clinical trials. Int. J. Med. Microbiol. 290:455-461. [DOI] [PubMed] [Google Scholar]
- 28.Reusser, P., S. R. Riddell, J. D. Meyers, and P. D. Greenberg. 1991. Cytotoxic T-lymphocyte response to cytomegalovirus after human allogeneic bone marrow transplantation: pattern of recovery and correlation with cytomegalovirus infection and disease. Blood 78:1373-1380. [PubMed] [Google Scholar]
- 29.Robinson, H. L., D. C. Montefiori, R. P. Johnson, K. H. Manson, M. L. Kalish, J. D. Lifson, T. A. Rizvi, S. Lu, S. L. Hu, G. P. Mazzara, D. L. Panicali, J. G. Herndon, R. Glickman, M. A. Candido, S. L. Lydy, M. S. Wyand, and H. M. McClure. 1999. Neutralizing antibody-independent containment of immunodeficiency virus challenges by DNA priming and recombinant pox virus booster immunizations. Nat. Med. 5:526-534. [DOI] [PubMed] [Google Scholar]
- 30.Rosenberg, E. S., J. M. Billingsley, A. M. Caliendo, S. L. Boswell, P. E. Sax, S. A. Kalams, and B. D. Walker. 1997. Vigorous HIV-1-specific CD4+ T cell responses associated with control of viremia. Science 278:1447-1450. [DOI] [PubMed] [Google Scholar]
- 31.Roy, M. J., M. S. Wu, L. J. Barr, J. T. Fuller, L. G. Tussey, S. Speller, J. Culp, J. K. Burkholder, W. F. Swain, R. M. Dixon, G. Widera, R. Vessey, A. King, G. Ogg, A. Gallimore, J. R. Haynes, and D. Heydenburg Fuller. 2000. Induction of antigen-specific CD8+ T cells, T helper cells, and protective levels of antibody in humans by particle-mediated administration of a hepatitis B virus DNA vaccine. Vaccine 19:764-778. [DOI] [PubMed] [Google Scholar]
- 32.Schmitz, J. E., M. J. Kuroda, S. Santra, V. G. Sasseville, M. A. Simon, M. A. Lifton, P. Racz, K. Tenner-Racz, M. Dalesandro, B. J. Scallon, J. Ghrayeb, M. A. Forman, D. C. Montefiori, E. P. Rieber, N. L. Letvin, and K. A. Reimann. 1999. Control of viremia in simian immunodeficiency virus infection by CD8+ lymphocytes. Science 283:857-860. [DOI] [PubMed] [Google Scholar]
- 33.Seth, A., I. Ourmanov, J. E. Schmitz, M. J. Kuroda, M. A. Lifton, C. E. Nickerson, L. Wyatt, M. Carroll, B. Moss, D. Venzon, N. L. Letvin, and V. M. Hirsch. 2000. Immunization with a modified vaccinia virus expressing simian immunodeficiency virus (SIV) Gag-Pol primes for an anamnestic Gag-specific cytotoxic T-lymphocyte response and is associated with reduction of viremia after SIV challenge. J. Virol. 74:2502-2509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shiver, J. W., T. M. Fu, L. Chen, D. R. Casimiro, M. E. Davies, R. K. Evans, Z. Q. Zhang, A. J. Simon, W. L. Trigona, S. A. Dubey, L. Huang, V. A. Harris, R. S. Long, X. Liang, L. Handt, W. A. Schleif, L. Zhu, D. C. Freed, N. V. Persaud, L. Guan, K. S. Punt, A. Tang, M. Chen, K. A. Wilson, K. B. Collins, G. J. Heidecker, V. R. Fernandez, H. C. Perry, J. G. Joyce, K. M. Grimm, J. C. Cook, P. M. Keller, D. S. Kresock, H. Mach, R. D. Troutman, L. A. Isopi, D. M. Williams, Z. Xu, K. E. Bohannon, D. B. Volkin, D. C. Montefiori, A. Miura, G. R. Krivulka, M. A. Lifton, M. J. Kuroda, J. E. Schmitz, N. L. Letvin, M. J. Caulfield, A. J. Bett, R. Youil, D. C. Kaslow, and E. A. Emini. 2002. Replication-incompetent adenoviral vaccine vector elicits effective anti-immunodeficiency-virus immunity. Nature 415:331-335. [DOI] [PubMed] [Google Scholar]
- 35.Singh, M., M. Briones, G. Ott, and D. O'Hagan. 2000. Cationic microparticles: a potent delivery system for DNA vaccines. Proc. Natl. Acad. Sci. USA 97:811-816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ulmer, J. B., J. J. Donnelly, S. E. Parker, G. H. Rhodes, P. L. Felgner, V. J. Dwarki, S. H. Gromkowski, R. R. Deck, C. M. DeWitt, A. Friedman, et al. 1993. Heterologous protection against influenza by injection of DNA encoding a viral protein. Science 259:1745-1749. [DOI] [PubMed] [Google Scholar]
- 37.Wang, R., D. L. Doolan, T. P. Le, R. C. Hedstrom, K. M. Coonan, Y. Charoenvit, T. R. Jones, P. Hobart, M. Margalith, J. Ng, W. R. Weiss, M. Sedegah, C. de Taisne, J. A. Norman, and S. L. Hoffman. 1998. Induction of antigen-specific cytotoxic T lymphocytes in humans by a malaria DNA vaccine. Science 282:476-480. [DOI] [PubMed] [Google Scholar]
- 38.Widera, G., M. Austin, D. Rabussay, C. Goldbeck, S. W. Barnett, M. Chen, L. Leung, G. R. Otten, K. Thudium, M. J. Selby, and J. B. Ulmer. 2000. Increased DNA vaccine delivery and immunogenicity by electroporation in vivo. J. Immunol. 164:4635-4640. [DOI] [PubMed] [Google Scholar]
- 39.Wilson, J. D., G. S. Ogg, R. L. Allen, C. Davis, S. Shaunak, J. Downie, W. Dyer, C. Workman, S. Sullivan, A. J. McMichael, and S. L. Rowland-Jones. 2000. Direct visualization of HIV-1-specific cytotoxic T lymphocytes during primary infection. AIDS 14:225-233. [DOI] [PubMed] [Google Scholar]
- 40.zur Megede, J., M. C. Chen, B. Doe, M. Schaefer, C. E. Greer, M. Selby, G. R. Otten, and S. W. Barnett. 2000. Increased expression and immunogenicity of sequence-modified human immunodeficiency virus type 1 gag gene. J. Virol. 74:2628-2635. [DOI] [PMC free article] [PubMed] [Google Scholar]