Abstract
Transcription of vesicular stomatitis virus is controlled by the position of a gene relative to the single 3′ genomic promoter: promoter-proximal genes are transcribed at higher levels than those in more 5′ distal positions. In previous work, we generated viruses having rearranged gene orders. These viruses had the promoter-proximal gene that encodes the nucleocapsid protein, N, moved to the second or fourth position in the genome in combination with the glycoprotein gene, G, moved from its usual promoter-distal fourth position to the first or third position. This resulted in three new viruses identified by the positions of the N and G genes in the gene order: G3N4, G1N4, and G1N2. The viruses G3N4 and G1N4 were attenuated for lethality in mice. In the present study, we addressed the basis of this attenuation by measuring the ability of each of the rearranged viruses to travel to and replicate in the olfactory bulb and brain following intranasal inoculation. In addition, the neuropathogenicity, serum cytokine levels, and immunoglobulin G isotype profiles in infected mice were determined. All the viruses reached the olfactory bulb and brain, but the outcomes of these infections were dramatically different. Viruses N1G4(wt) and G1N2 caused lethal encephalitis in 100% of animals within 7 days postinoculation; however, viruses G3N4 and G1N4 were cleared from the brain by 7 days postinoculation and all animals survived without apparent distress. The viruses differed in the distribution and intensity of lesions produced and the type and levels of cytokines induced. Animals inoculated with N1G4(wt) or G1N2 displayed extensive encephalitis and meningitis and had elevated levels of serum gamma interferon compared to what was seen with G3N4- or G1N4-infected mice. In contrast to what occurred with intranasal inoculation, all four viruses caused lethal encephalitis when administered by direct inoculation to the brain, a route that circumvents the majority of the host immune response, demonstrating that G3N4 and G1N4 were not deficient in their abilities to cause disease in the brain. These findings indicate that gene rearrangement and its consequent alteration of gene expression can, without any other changes, alter the viral spread and cytokine response following intranasal infection.
Vesicular stomatitis virus (VSV) is the prototypic virus of the order Mononegavirales, which is composed of four families, Rhabdoviridae, Paramyxoviridae, Filoviridae, and Bornaviridae. The viruses in these families are responsible for a wide range of significant diseases in animals, fish, and plants. Viruses in all four families have a single strand of nonsegmented negative-sense RNA as their genome (38). VSV is a member of the Rhabdoviridae, and its 11-kb genome has five genes encoding the five structural proteins of the virus: the nucleocapsid protein, N; the phosphoprotein, P; the matrix, M; the glycoprotein, G; and the RNA-dependent RNA polymerase, L. The order of the genes in the genome is 3′-N-P-M-G-L-5′, and the relative order of these basic genes is highly conserved among all the members of the Mononegavirales. Gene expression is controlled primarily at the level of transcription by the location of a gene relative to the single 3′-proximal polymerase entry site, and transcription is obligatorily sequential (1, 3). Due to transcriptional attenuation at each of the gene junctions, genes nearer the 3′ entry site are transcribed at higher levels than those positioned towards the 5′ end of the genome (21, 49).
We have taken advantage of this method of transcriptional control to generate viruses in which the level of expression of individual genes has been altered by moving the position of a gene relative to the single promoter. This was achieved by manipulation of an infectious cDNA clone. Infectious viruses having a variety of gene orders were recovered (4, 16, 52). For example, we moved the N gene, whose product is known to be important for viral replication (2, 18, 33, 34, 51), away from its 3′ promoter-proximal position to the fourth position in the genome, yielding the virus G3N4 with the gene order 3′-P-M-G-N-L-5′. This virus had reduced N gene expression, decreased replication ability in tissue culture, and decreased lethality in mice and was nonpathogenic in swine, a natural host for VSV (15, 52). Despite this attenuation of virulence, both mice and pigs inoculated with the G3N4 virus were protected from subsequent challenge by the wild-type (wt) virus.
To maintain attenuation of virulence and increase the immunogenicity, the position of the G gene, which encodes the viral attachment glycoprotein containing neutralizing (22, 27), helper T-cell (9), and cytotoxic T-cell (26, 44) epitopes of the virus, was altered also. The G gene was moved from the promoter-distal fourth position to the first, most promoter-proximal position in the genome. The resulting virus, referred to as G1N4, had the gene order 3′-G-P-M-N-L-5′. An additional construct also having the G gene in the first position and N in the second position, G1N2, with the gene order 3′-G-N-P-M-L-5′, was generated, and all the viruses were compared to the wt construct, N1G4, having the gene order 3′-N-P-M-G-L-5′. In previous work, viruses with N moved to promoter-distal positions, G3N4 and G1N4, were shown to have reduced lethality in mice while viruses with G moved forward showed a more rapid and higher level of antibody production (16).
Mice have long been used to study the pathogenesis of VSV and its mutants (32, 45, 50). Intranasal inoculation of Swiss Webster, C57BL/6, and BALB/c mice with VSV has been well characterized, and infection results in fatal encephalitis. After intranasal administration, VSV enters the central nervous system (CNS) via the receptor neurons of the olfactory nerve, followed by invasion of the olfactory bulb and finally an acute infection of the brain (10, 17, 19, 28, 32, 36, 40, 45). Animals given lethal doses of virus display hind-limb paralysis, meningitis, encephalitis, and death, which usually occurs within 6 to 10 days and is concurrent with a peak in viral titers in the brain. There is minimal involvement of respiratory tissue (17, 28) and an absence of viremia (46).
VSV infection is known to activate both the innate and adaptive immune systems (6), and while the CNS has been thought of as an immunologically privileged site, viral infection of the CNS can be controlled by mechanisms that involve both T cells and antibody. A number of cytokines produced by T cells are important in establishing the outcome of infection with wt VSV. Studies have shown that the cytokine interleukin-12 (IL-12) significantly enhanced recovery from VSV infection of the CNS (7, 23, 25). IL-12 mediates a broad range of effects on both the innate and the adaptive arms of the immune system. It plays an important role by stimulating gamma interferon (IFN-γ), a T helper (Th) type 1 cytokine, and inhibiting IL-4, a Th type 2 cytokine, thereby helping to define the Th profile generated after infection (29). Recently, it has been shown that IFN-γ-mediated noncytolytic clearance of Sindbis virus from neurons by T cells is possible (8), while an earlier study indicated that type I nitric oxide synthase activity induced by IFN-γ inhibited VSV replication in neurons (24).
In the present study, we examined the basis of the attenuation of lethality observed in young mice after intranasal inoculation with G1N4 or G3N4 virus compared with what was seen with the more pathogenic N1G4(wt) and G1N2 viruses. The abilities of the viruses to travel to and replicate in the lungs, olfactory bulbs, and brains of C57BL/6 mice were assessed. The severity of the neuropathogenesis in the olfactory bulb and brain was examined histochemically. The immunoglobulin G (IgG) isotype and serum cytokine profile generated after inoculation were determined. The results described below show that VSVs having the same gene complement but with rearranged gene orders differed in their replicative abilities, tissue localization, extent of lesions produced, and the types and levels of cytokines induced after intranasal inoculation.
MATERIALS AND METHODS
Cells and viruses.
The San Juan isolate of the Indiana serotype of VSV provided the RNA template for most of the cDNA clone used in this work, except for the G protein gene, which was derived from the Orsay isolate of VSV Indiana (4, 15, 16, 52, 53). The baby hamster kidney (BHK-21) cell line was used for the recovery and growth of viral pools, while viral titers were determined by plaque assay with the African green monkey kidney cell line, Vero 76.
Plasmid construction and recovery of infectious virus.
The construction of the full-length cDNA clones of the VSV Indiana genome and their use for the recovery of infectious virus have been described previously (52, 53). The infectious clone was manipulated by using methods that allowed the genome to be reassembled with the genes in a specific order (4, 52). No other changes were introduced into the genome except for a single nucleotide substitution in the intergenic region downstream of the P gene. This change from 3′-CA-5′ to 3′-GA-5′ has little effect on transcription (5). Viruses G1N2 and N1G4(wt) were recovered and propagated at 37°C, while viruses G3N4 and G1N4 were recovered only from cells transfected at 31°C as described previously (16). All studies with these viruses were performed at the respective temperatures unless otherwise stated.
Experimental infection of mice.
Specific-pathogen-free C57BL/6 mice, 3 to 4 weeks old, were purchased from Jackson Laboratory, Bar Harbor, Maine, and housed under biosafety level 2 conditions. In previous work, outbred Swiss Webster mice were used; however, in this study C57BL/6 mice were used because they are an inbred stain that have been shown to be susceptible to VSV infection (10). To determine the 50% lethal dose (LD50) for each of the rearranged viruses when administered intranasally or intracranially, groups of five mice, 3 weeks old, were lightly anesthetized with ketamine-xylazine and inoculated with serial 10-fold dilutions of each virus. Intranasally inoculated mice received 10 μl, while intracranially inoculated mice received a 30-μl volume of inoculum directly into the brain. Animals were observed daily, and the LD50 value for each virus was calculated by the method of Reed and Muench (39).
For all other studies, groups of four to six mice were lightly anesthetized with ketamine-xylazine and inoculated intranasally with 5,000 PFU of the individual viruses in a 10-μl volume of Dulbecco's modified Eagle medium (DMEM). Control animals were given a similar volume of DMEM.
Analysis of viral replication in mice.
At the indicated time points, groups of five mice were given a lethal dose of ketamine-xylazine and the lungs, olfactory bulb, and whole brain were aseptically removed. Specimens were placed in ice-cold DMEM containing antibiotics. Individual tissues from each mouse for each virus were homogenized, and the homogenates were aliquoted and stored at −70°C. In addition, serum was collected from animals on days 4, 7, and 14 postinoculation. Viral titers for each sample were determined by plaque assay on the Vero 76 cell line and expressed as log10 PFU per gram of tissue or per milliliter of serum.
Histological preparation and scoring.
At 7 days postinoculation, groups of four to six mice were sacrificed by the administration of a lethal dose of ketamine-xylazine. To minimize distortion, after removal of the dorsal calvarium, brains were fixed in situ by immersion for 24 h in buffered 10% formalin. After removal from the skull, each brain was trimmed by sectioning sagittally on the midline and approximately 3 mm to each side of the midline. The resulting four pieces of tissue were fixed in formalin for an additional 24 h and then processed and embedded in paraffin. Orientation of the tissues within the paraffin blocks was such that the medial surfaces of the trimmed tissues were sectioned. Sections were cut at 5 μm and stained with hematoxylin and eosin (H&E). Slides were examined by the pathologist in a blind fashion. Slight and mild cases of encephalitis were characterized primarily by lymphocytic perivascular cuffing, whereas the features of lesions classified as moderate and severe were chiefly necrosis and accumulation of neutrophils. Encephalitis and meningitis distribution and severity were evaluated according to a subjective scoring system devised in the following manner: based on the distribution of lesions in various parts of the brain, samples were scored 0, 1, 2, 3, or 4 for normal, slight, mild, moderate, or severe, respectively. For statistical analysis and graphic presentation of these data, the individual scores for various areas of the brain were combined by averaging. An overall score was calculated by summing the individual scores and dividing by the maximum possible score.
IgG isotype determination.
Seven days after virus inoculation, serum was collected from groups of four to five animals and the IgG isotype profile for each individual mouse was measured. Infected- and control-cell lysates were used for antigen in an enzyme-linked immunosorbent assay (ELISA) that was prepared as previously described (16). Sera were serially diluted, and the immunoglobulin G subclasses, IgG1, IgG2a, IgG2b, and IgG3, were detected by using goat anti-mouse specific antibodies (Southern Biotechnology Associates, Birmingham, Ala.). The optical density (OD) was read at 450 nm, and the antibody titers were calculated by linear regression analysis of a plot of OD versus serum dilution. The endpoint titers (log10) were deduced at an OD that was 1.5 times higher than that of serum from an uninfected control group.
Detection and quantitation of serum cytokines.
At days 4 and 7 postinoculation with the rearranged viruses or medium alone, serum was collected from groups of four mice. Murine IFN-γ, IL-12, and IL-4 ELISA kits were purchased from Amersham Pharmacia Biotech (Piscataway, N.J.), and assays were performed on the serum from each individual mouse as described by the manufacturer.
Statistical analysis.
Lesion scores were analyzed with the Kruskal-Wallis test (41) by using Statistix for Windows version 7 statistical software (Analytical Software, Tallahassee, Fla.). Supplemental comparisons among groups were done with Statistix software by parametric analysis of variance applied to ranks and use of critical Z values (42) to compare mean ranks.
RESULTS
Viral replication in mice.
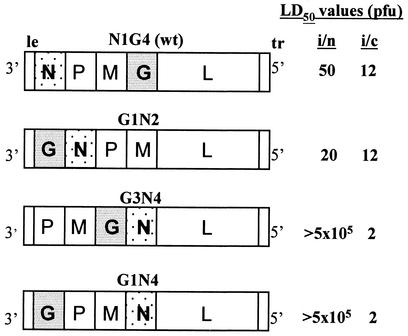
The construction, recovery, and initial characterization of viruses N1G4(wt), G1N2, G3N4, and G1N4 have been reported previously (16), and a diagram of the gene orders is shown in Fig. 1. We determined the LD50 value for each virus after intranasal inoculation of C57BL/6 mice. The LD50s for N1G4(wt) and G1N2 were 50 and 20 PFU, respectively. In contrast, no lethal encephalitis was observed following intranasal inoculation with G3N4 or G1N4, and consequently a lethal dose could not be determined (LD50, >500,000 PFU). Therefore, to test whether the G3N4 and G1N4 viruses were deficient for replication ability in the brain, mice were inoculated intracranially. The LD50 values for all the viruses were similar following intracranial inoculation (range, 2 to 12 PFU) (Fig. 1). These data show that when administered directly into the brain, a route that circumvents the majority of the host's immune defenses, all four viruses were highly lethal. Thus, by direct intracranial administration, the G3N4 and G1N4 viruses were not deficient in their ability to cause disease in the brain.
FIG. 1.
Gene orders of N1G4 (wt), G1N2, G3N4, and G1N4. Their LD50 values after intranasal (i/n) or intracranial (i/c) inoculation are expressed in terms of PFU per animal. LD50 values were calculated from mortality rates in groups of five animals inoculated with serial 10-fold dilutions of virus. le, leader; tr, trailer.
On the basis of the above-mentioned data, a single viral dose of 5,000 PFU administered intranasally was selected to examine relative viral pathogenesis and was used for all experiments in this study. At this dose, no clinical symptoms were observed in any G3N4- or G1N4-infected animals, while all G1N2- or N1G4(wt)-infected mice showed paralysis and death. At days 3 to 7, 10, and 14 postinoculation, lung, olfactory bulb, and brain samples were harvested from G3N4- or G1N4-infected mice. Because of the lethality of G1N2 and N1G4(wt) when administered at 5,000 PFU, samples were taken only at days 3 through 7. Tissue and serum samples were aseptically removed from groups of five animals for each virus and homogenized, and the viral titers were determined for each organ from each individual animal by plaque assay on Vero 76 cells.
Virus was not recovered from the sera of infected animals on days 4, 7, and 14 postinoculation (data not shown). This was in agreement with previous findings indicating no viremia after VSV infection (46). In addition, no virus was recovered from the lungs of animals infected with either G3N4 or G1N4 during the 11-day study period (Fig. 2A). A low level of virus, less than 1.6 log10 PFU/g of tissue, was found in the lungs of G1N2-infected animals on days 3 and 4, but no virus was detectable by day 5, while in N1G4(wt)-infected animals, virus was found in the lungs only at day 3 and at a titer similar to that seen in G1N2-infected mice. This indicates that the lung was not a major site for viral replication. It is possible that these low titers represent virus aspirated to the lungs during the intranasal instillation, although the inoculum volume (10 μl) was kept small to minimize this possibility.
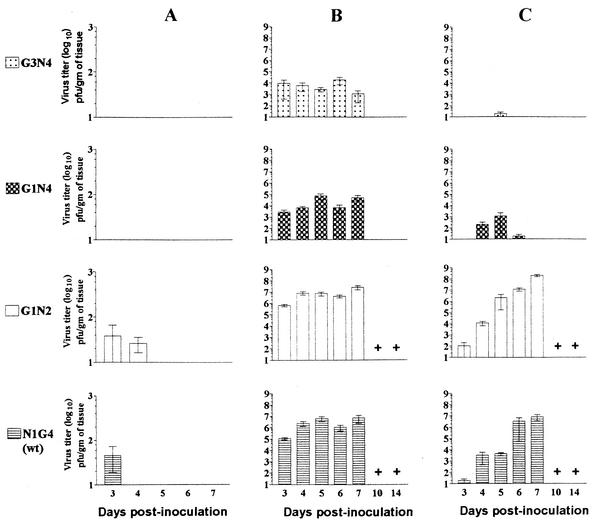
FIG. 2.
Viral titers in tissue after inoculation with the rearranged or wt viruses. Groups of five animals were inoculated intranasally with 5,000 PFU of N1G4(wt), G1N2, G3N4, or G1N4 per mouse. Lung (A), olfactory bulb (B), and brain (C) tissue were aseptically collected on days 3 to 7, 10, and 14 postinoculation and homogenized, and the viral titers were determined by plaque assay on the Vero 76 cell line. The viral loads are expressed as log10 PFU per gram of tissue. Graphs show the averages ± standard errors of the means (SEM). Crosses indicate that no samples were available due to death of animals.
In the olfactory bulb, however, viral titers increased with time after intranasal inoculation, as shown in Fig. 2B, indicating viral replication. Virus was detected in the olfactory bulb of all animals inoculated with any of the four viruses by day 3. Mean titers of G3N4 and G1N4 were 10- to 100-fold lower than those of N1G4(wt) and G1N2, respectively, on day 3. The mean titers of G3N4 and G1N4 increased to 4.3 log10 and 4.9 log10 PFU/g, respectively, by days 5 and 6.
Viruses G1N2 and N1G4(wt) attained 100- to 10,000-fold higher mean titers in the olfactory bulb than did G3N4 or G1N4 by day 7 (Fig. 2B). On day 7, titers in G3N4- or G1N4-infected animals were similar to those on day 3, while in G1N2- or N1G4(wt)-infected mice, viral titers continued to increase until day 4 or 5. By day 10, the levels of the G3N4 and G1N4 viruses were below the sensitivity of the assay, indicating that these animals had controlled the infection. In contrast, all the animals inoculated with G1N2 or N1G4(wt) were dead by day 10 (Fig. 2B).
Despite the replication of G3N4 and G1N4 in the olfactory bulb, only low levels of virus were detected in the brain (Fig. 2C). Virus G3N4 was detected only on day 5, with a mean titer of 1.3 log10 PFU/g. Virus G1N4 was first detected on day 4, and the titer increased to 3.0 log10 PFU/g by day 5. However, titers declined to very low levels by day 6 and had disappeared by day 7. This differed from the brains of animals given the G1N2 or N1G4(wt) virus, in which virus was first recovered by day 3 and viral levels increased to 8.3 log10 PFU/g and 6.9 log10 PFU/g, respectively, by day 7 (Fig. 2C).
In summary, viral replication occurred in the olfactory bulb and brain but not in the lungs. By 3 days postinoculation, G3N4, G1N4, G1N2, and N1G4(wt) were present and increasing in titers in the olfactory bulbs of all mice. Following intranasal inoculation, only low levels of G3N4 and G1N4 were found in the brains of infected mice, and both of these viruses were cleared by day 6. These findings with G3N4 and G1N4 differed considerably from our findings with G1N2- or N1G4(wt)-infected mice, in which virus was detected earlier in the brain and replicated to higher titers. These findings indicate that gene rearrangement alone influenced the invasiveness of VSV and the ability of inoculated animals to clear the infection.
Histology and severity of disease.
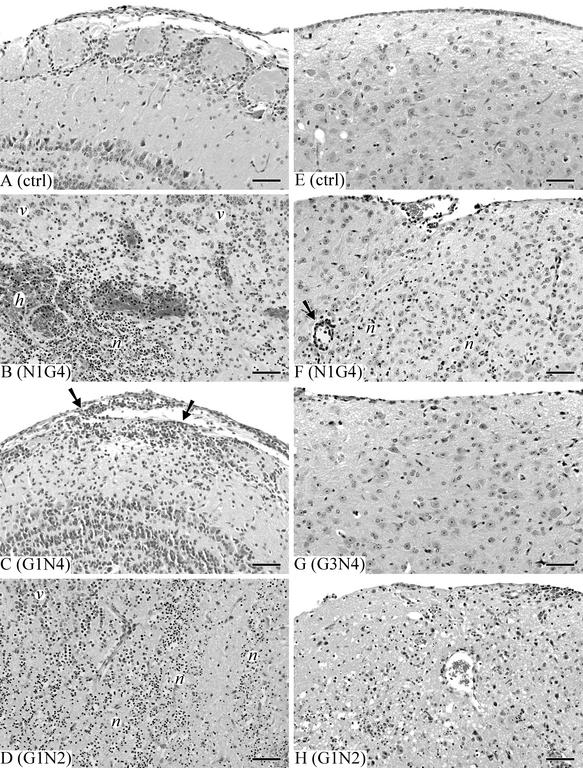
Lesions in mice inoculated with N1G4(wt) were as expected based on the results of previous studies (19, 32) and were characterized by the accumulation of lymphocytes in the leptomeninges and around vessels within the brain, accompanied by areas of necrosis and the accumulation of neutrophils (Fig. 3B and F). With all viruses, lesions were more intense in the olfactory bulb (Fig. 3B to D). In mice inoculated with either N1G4(wt) or G1N2 virus, lesions also were widespread in other areas of the brain (Fig. 3F and H), including the meninges, the ependyma, and choroid plexuses of the ventricles. Viruses G1N4 and G3N4 showed indistinguishable results and were clearly attenuated. Mice inoculated with either of these viruses had closely similar lesions that were restricted to the olfactory bulb and that consisted of mild meningitis or meningoencephalitis with mild inflammation of the superficial nervous tissue (Fig. 3C and G and data not shown). In contrast, the virulence of G1N2 appeared to be somewhat enhanced, as demonstrated by necrosis that was an especially prominent feature of lesions in the olfactory bulb and elsewhere in the brain tissue of mice inoculated with this virus (Fig. 3D and H). The microscopy findings corresponded well with the clinical observations.
FIG. 3.
Lesion development in the olfactory bulb and brain tissue of mice at 7 days postinoculation with the rearranged viruses. Groups of four to seven mice were inoculated intranasally with 5,000 PFU of N1G4(wt), G1N2, G3N4, or G1N4 per animal. Control animals were given medium only. Brains were fixed in situ, sectioned, and stained with H&E. (A) Olfactory bulb of uninfected control. (B) Olfactory bulb of N1G4(wt)-infected animal showing necrotizing encephalitis with necrosis (n), hemorrhage (h), and neutrophil accumulation. v, viable tissue. (C) Olfactory bulb of mouse inoculated with attenuated G1N4 virus showing lymphocytic meningoencephalitis, with lymphocytic infiltration of leptomeninges and superficial neutrophils (arrows). (D) Olfactory bulb of mouse given virulent G1N2 virus showing severe extensive necrotizing encephalitis (n). (E) Medulla of a sham-inoculated control. (F) Medulla of mouse given N1G4(wt) virus showing mild necrotizing encephalitis, with lymphocytic perivascular cuffing (arrow) and inflammatory cell infiltration and neuronal necrosis (n). (G) Medulla of mouse inoculated with attenuated G3N4 virus showing no abnormalities. (H) Medulla of mouse given virulent G1N2 virus showing necrotizing encephalitis with diffuse infiltration of neutrophils and lymphocytes. Bars, 65 μm.
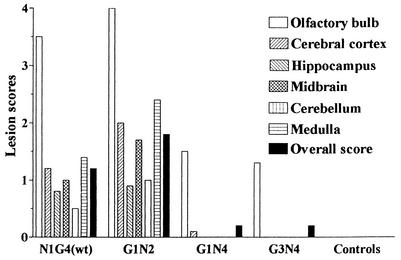
The severity of the resulting lesions was scored for analysis as detailed in Materials and Methods by using a scale from 0 to 4, with 0 for normal, 1 for slight, 2 for mild, 3 for moderate, and 4 for severe lesion development. In olfactory bulb tissue, scores in the range of 1 to 2 were determined for G3N4- and G1N4-infected mice while the scores for N1G4(wt)- and G1N2-infected mice were 3 to 4. After infection with G1N2 or N1G4(wt), similar areas of the brain were affected, with the medulla, cerebral cortex, and midbrain having higher scores than the hippocampus or cerebellum. In all areas where lesions were found, those resulting from G1N2 infection were more severe than those resulting from wt virus infection (Fig. 4), while infection with G1N4 or G3N4 resulted in fewer lesions that were confined to the olfactory bulb. No lesions were observed in uninfected control animals. The overall scores showed clearly that infection with G1N2 was more intense, based on the presence of meningitis and encephalitis, than infection with N1G4(wt), while G3N4 and G1N4 did not cause any encephalitis.
FIG. 4.
Severity of lesions in the olfactory bulb and brain of mice. Groups of four to seven mice were inoculated intranasally with 5,000 PFU of G1N4, G3N4, N1G4(wt), or G1N2 virus per animal. Control animals were given medium only. After 7 days, tissues were fixed and stained with H&E as outlined in Materials and Methods. The degrees of pathogenesis were evaluated according to a scoring system based on normal, slight, mild, moderate, or severe encephalitis and meningitis distribution. For graphic presentation, the individual scores for various areas of the brain were combined by averaging. An overall score was calculated by summing the individual scores and dividing by the maximum possible score.
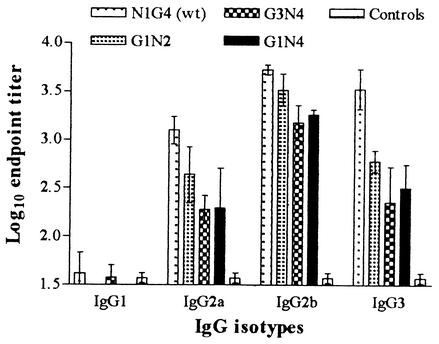
IgG isotype profile.
The IgG isotypes induced after inoculation with the G3N4, G1N4, G1N2, or N1G4(wt) virus were assayed. Serum was collected from individual animals at 7 days postinoculation, and isotype profiles for each animal were compared with those of an uninfected control group. Detergent-disrupted infected and uninfected whole-cell lysates were used as antigen in an ELISA, and the IgG isotype was determined by probing with an anti-mouse IgG1, IgG2a, IgG2b, or IgG3 antibody. All the viruses induced IgG2a, IgG2b, and IgG3 isotypes; however, IgG1 was only induced by N1G4(wt) and G3N4 and at very low titers (mean, <1.9 log10) (Fig. 5). The wt virus induced the highest level of IgG2a, with a mean titer of 3.2 log10, while the levels induced in G1N2-, G3N4-, and G1N4-infected animals were slightly lower. When the IgG2b isotype titers were determined, they were found to be similar in all infected groups. IgG3 levels were markedly higher in the serum from N1G4(wt)-inoculated mice than from mice inoculated with the other viruses. N1G4(wt)-infected animals had mean IgG3 titers of 3.6 log10, with the levels in G1N2-, G3N4-, and G1N4-infected animals being 2.7, 2.4, and 2.5 log10 PFU/g, respectively. These findings indicate that the rearranged viruses induced IgG isotypes similar to those found in wt virus-infected mice; however, the levels within each isotype differed depending on the virus inoculated.
FIG. 5.
Serum IgG isotype profile after inoculation with the rearranged viruses. Groups of four to five mice were inoculated intranasally with 5,000 PFU of G1N4, G3N4, N1G4(wt), or G1N2 virus per animal. Control animals were given medium only. After 7 days, serum was collected from individual animals. The level of each isotype was determined by titration on detergent-lysed VSV-infected cell antigen in an ELISA. The mean antibody titers ± SEM were recorded and expressed as log10 endpoint titers.
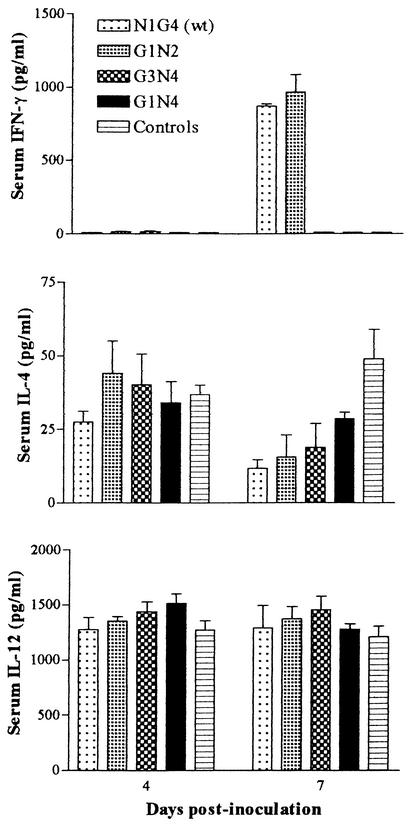
Serum cytokines.
Previous studies have shown that IFN-γ, a marker of a Th type 1 response, and IL-12 are important cytokines in the host defense against neurotropic viral infections (8, 20, 24, 25); therefore, we measured the levels of IFN-γ and IL-12 in the sera of individual animals at days 4 and 7 postinoculation. No IFN-γ was detected in any of the infected animals at 4 days postinoculation. By day 7, IFN-γ was found at high levels in N1G4(wt)- and G1N2-infected animals, while G3N4-infected, G1N4-infected, and uninfected control animals had undetectable titers (Fig. 6). Thus, to test the alternate possibility that the immune response against G3N4 and G1N4 was of a Th type 2 nature, the levels of IL-4, a cytokine indicative of Th type 2 immunity, were also measured. Unlike IFN-γ, IL-4 was identified in all animals infected with the rearranged viruses and the controls by day 4, with mean levels for the rearranged viruses and the controls being slightly higher than for the wt. On day 7, the IL-4 levels in all virus-inoculated animals were decreased compared to that in uninfected controls, with that in wt virus-infected animals being the lowest (Fig. 6). IL-12 was also detected by day 4 in all mice, with similar mean levels regardless of the rearranged virus administered. These titers were comparable to those seen in the control group and were also similar to those found on day 7 (Fig. 6).
FIG. 6.
Serum cytokine profile after inoculation with the rearranged viruses. Groups of four to five mice were inoculated intranasally with 5,000 PFU of G1N4, G3N4, N1G4(wt), or G1N2 virus per animal. Control animals were given medium only. After 4 and 7 days, serum was collected from individual animals and the levels of IFN-γ, IL-4, and IL-12 were determined. Results are expressed as the mean cytokine levels ± SEM.
DISCUSSION
We have shown that it is possible to manipulate the phenotype of VSV by rearranging the order of the genes, thereby taking advantage of the obligatorily sequential nature of transcription wherein the position of a gene relative to the single promoter determines the level of expression. For example, we have shown that translocation of the N gene to successive positions away from the promoter results in a progressive decrease in N expression, replication in cultured cells, and lethality in mice. In addition, moving the G gene towards the promoter yielded increased G expression and a more rapid and higher antiviral immune response. By combining these two alterations, moving N away from the promoter and moving G closer to the promoter, we generated viruses with rearranged genomes that were attenuated in mice and swine yet could stimulate a protective immune response. In the present work, we examined the basis for this attenuation.
Previous work has established that the pathogenesis in mice infected intranasally with VSV is due to infection of the brain that occurs via the olfactory nerve and olfactory bulb (10, 17, 19, 28, 32, 36, 45). The results presented here show that for the wt and all of the rearranged viruses examined, this was the mode of pathogenesis. There was no evidence for viremia or for replication in other tissues, for example, the lung, even though inoculation was via the intranasal route. Strikingly, however, despite great differences in their lethality, all the rearranged viruses traveled to the olfactory bulb and replicated there. Thus, all the viruses reached the olfactory bulb and, as evidenced by increasing titers over successive days, replicated there, showing that the attenuated viruses were not defective in their ability to reach or replicate in the olfactory bulb. Titers were lower, however, in G1N4- and G3N4-infected animals than in G1N2- and wt virus-inoculated groups.
All the viruses reached the brain. However, while G1N2 and N1G4(wt) replicated to high titers in the brain until death, the titers of G3N4 and G1N4 were low and the infection was quickly cleared. For example, G1N4 reached the brain and increased in titer by days 4 and 5, decreased on day 6, and was undetectable by day 7 (Fig. 2C). Similarly, low titers of G3N4 were detected only on day 5 (Fig. 2C). The time course of wt virus replication from the brain homogenates was consistent with past observations (17). Thus, the attenuated phenotype of the G1N4 and G3N4 viruses in mice correlated with the extent to which virus replicated in brain tissue or was cleared.
Nevertheless, we observed that after intranasal inoculation, viruses G3N4 and G1N4 were detected in the brains of animals on day 5 and days 4 to 6, respectively, at mean titers of 18 and 1,126 PFU/g of tissue. These titers are equal to, or approximately, 10- and 500-fold greater than the LD50 values determined for these viruses following direct intracranial inoculation. These data show that these viruses are not defective in their ability to reach and cause disease in the brain and thus indicate that the host is capable of controlling and clearing the infection from the brain when the route of inoculation is intranasal via the olfactory bulb but not when the brain is directly infected. Thus, these results suggest that rearrangement of the wt gene order alters the invasiveness of the virus such that the host is able to respond with a protective response.
Histopathologic evaluation of olfactory bulb and brain tissue showed distinct differences among the viruses in the extent and severity of meningitis and encephalitis. These findings correlated well with the data on extent of replication and demonstrated clear differences in the virulences of the viruses having different gene arrangements. The distribution and severity of the brain lesions were consistent with the G1N2 and N1G4(wt) viruses gaining entry to the cerebrospinal fluid and being disseminated from the initial sites of infection to other parts of the brain, as there was widespread meningitis and superficial areas of encephalitis. Spread via the cerebrospinal fluid has also been suggested by Van den Pol and colleagues (48). In this study, we did not assay specific areas of the brain for the presence of virus; however, the appearance of inflammation in limited regions suggests that not all the tissues of the olfactory system and the brain are equally infected after intranasal inoculation of mice. This is consistent with the results of previous studies (19, 28, 48). The reasons for this are unknown, but it may be due to the absence of the viral receptor or the inability of the virus to complete its replication processes.
The G1N2 virus appeared to be slightly more pathogenic than the wt virus and resulted in a higher lesion score. We speculate that the reason for this higher score is the higher expression of G protein and a level of replication similar to that of wt virus. In previous work, we found that cells infected with G1N2 synthesized 2.3-fold more G than cells infected with N1G4(wt) virus despite the fact that both viruses had similar replication kinetics (16). The G protein of VSV has been shown to prevent the synthesis of cellular DNA and RNA and is cytotoxic (31). The cellular RNAs inhibited could include those that encode proteins such as IFN-α/β, and the subsequent inability of the cell to synthesize such proteins could prevent the cell from limiting the infection. Therefore, infection with G1N2 may have resulted in an increased shutoff of host cell macromolecular synthesis due to increased synthesis of the glycoprotein. A combination of increased G synthesis and replication equivalent to or greater than that of the wt virus may have resulted in a more severe infection than that caused by infection with the N1G4(wt) virus.
The low titers and short duration of the G1N4 and G3N4 viruses in the brain suggest the stimulation of an immune factor(s) capable of controlling and eventually eliminating the virus. To investigate whether there were differences in the natures of the cytokine responses generated after infection with the G1N4, G3N4, G1N2, or N1G4(wt) virus, the levels of IFN-γ, IL-12, and IL-4 in the sera of mice were determined. IL-12 has been shown to promote the production of IFN-γ while inhibiting that of IL-4 (29); however, it is known that IFN-γ is not an absolute requirement for the clearance of VSV from brain tissue (23). Mice infected with G1N2 and N1G4(wt) had high levels of IFN-γ in their sera 7 days after inoculation, while no IFN-γ was detected in G3N4-infected, G1N4-infected, and uninfected control animals. The reasons for this strong IFN-γ response in moribund animals and an undetectable IFN-γ response in healthy animals are unknown, but there was a correlation with the viral load in the brain. At day 4 in brain tissue, the titers of all the viruses were at or below 4 log10 PFU/g and no IFN-γ was detected. On day 7, the G3N4 and G1N4 viruses were not detected and no IFN-γ was present; however, G1N2 and N1G4(wt) continued to replicate and increased to almost 8 log10 PFU/g, at which time high levels of IFN-γ were measured. The cell type(s) responsible for producing this IFN-γ has not yet been identified, but regardless of the source, the responses stimulated were not capable of controlling the virus.
Infection with each of the four viruses suppressed IL-4 production compared with that in the uninfected controls. In contrast to the observation for IFN-γ, the IL-4 levels in the sera of animals that received either G1N2 or N1G4(wt) were slightly lower than those found in G3N4- or G1N4-infected mice, which may indicate a suppression of IL-4 stimulation by IFN-γ. This combination of increased IFN-γ production and decreased IL-4 production is characteristic of a Th type 1 immune response. Further studies are under way to determine whether other cytokines are produced and the nature of the cellular immunity stimulated in response to infection. These studies may clarify the different Th subsets that were induced.
Although IL-12 is capable of influencing the stimulation of IFN-γ and IL-4 by their respective Th cell subsets, the IL-12 levels on days 4 and 7 in all virus-infected groups were unaffected compared with those in the uninfected controls. This suggests that IL-12 production was not stimulated after infection with the rearranged VSVs and did not influence the upregulation of IFN-γ or the inhibition of IL-4. The levels of IFN-α/β were not addressed in the present study, but as a prelude to this study, it had been shown that the rearranged viruses differed in their abilities to stimulate IFN-α and IFN-β in vitro (30). Work is under way to determine the interaction of the rearranged viruses with the IFN-α/β system in vivo. It should be noted that only the serum was analyzed for cytokines, and this may not be representative of the cytokine profile found at the sites of infection. Analysis of olfactory bulb and brain tissue after infection for locally produced cytokines may be more informative with regard to the immunity generated to these viruses. More detailed studies are under way which will help to clarify these observations.
Modulation of murine IgG antibody subclasses after viral infection has long been known (13). Responses after viral infection are predominately IgG2a and to a lesser extent IgG2b (14). These contrast with those directed against soluble protein or carbohydrates, which are normally restricted to the IgG1 or IgG3 subclass, respectively (35). The IgG subclass stimulated in response to viral infection is influenced by the cytokines produced. Previous work has shown that the stimulation of IFN-γ, a cytokine that is indicative of a Th type 1 response, increased the secretion of the IgG2a subclass, while IL-4, a Th type 2 cytokine, stimulates the production of IgG1 antibodies (47). In this study, the IgG2a and IgG2b levels were similar for all of the rearranged viruses and the wt virus. Thus, despite the differences in the IFN-γ and IL-4 levels observed after infection with the rearranged viruses, it does not appear that the IgG isotype profile was influenced.
In summary, these studies show that while all the rearranged viruses traffic to the olfactory bulb and into the brain, only the wt and G1N2 viruses replicate to high titers in the brain and cause extreme neuropathogenesis. Viruses having N translocated to the fourth position, G3N4 and G1N4, reach the brain, but they are rapidly cleared and cause little or no neuropathogenesis. Studies are under way to identify which factors are responsible for the control and eventual eradication from the brain of replicating G3N4 and G1N4 viruses.
The use of VSV as a live vector to deliver foreign genes and antigens shows promise (11, 12, 43). Changes to the genome such as the introduction of foreign genes or the rearrangement of the gene order have proven to be stable, and because these viruses do not undergo homologous recombination, such changes should be irreversible (37, 38). The results presented here expand our earlier observations that gene rearrangement can be used to attenuate these viruses. The basis of this attenuation involves complex interactions between the virus and host. For example, G3N4 and G1N4 may be attenuated because they can stimulate protective factors, or alternatively, they may fail to inhibit an antiviral response. Gene rearrangement of VSV can alter the rate of viral replication in vitro and its lethality and the kinetics of the antibody response, and as we have shown here, it also alters the tissue spread and levels of IFN-γ induced in vivo. Studies designed to identify other differences in the host response are under way in the hope that we can better understand the relationship between the pathogenicity and the immune response generated in response to infection with rearranged VSVs.
Acknowledgments
We thank Xiaoling Tang and Kevin Alexander for excellent technical assistance and our colleagues for constructive comments.
This work was supported by Public Health Service grant AI 12464 from NIAID to G.W.W.
REFERENCES
- 1.Abraham, G., and A. K. Banerjee. 1976. Sequential transcription of the genes of vesicular stomatitis virus. Proc. Natl. Acad. Sci. USA 73:1504-1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arnheiter, H., N. L. Davis, G. Wertz, M. Schubert, and R. A. Lazzarini. 1985. Role of the nucleocapsid protein in regulating vesicular stomatitis virus RNA synthesis. Cell 41:259-267. [DOI] [PubMed] [Google Scholar]
- 3.Ball, L. A., and C. N. White. 1976. Order of transcription of genes of vesicular stomatitis virus. Proc. Natl. Acad. Sci. USA 73:442-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ball, L. A., C. R. Pringle, B. Flanagan, V. P. Perepelitsa, and G. W. Wertz. 1999. Phenotypic consequences of rearranging the P, M, and G genes of vesicular stomatitis virus. J. Virol. 73:4705-4712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barr, J. N., S. P. J. Whelan, and G. W. Wertz. 1997. Role of the intergenic dinucleotide in vesicular stomatitis virus RNA transcription. J. Virol. 71:1794-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bi, Z., M. Barna, T. Komatsu, and C. S. Reiss. 1995. Vesicular stomatitis virus infection of the central nervous system activates both innate and acquired immunity. J. Virol. 69:6466-6472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bi, Z., P. Quandt, T. Komatsu, M. Barna, and C. S. Reiss. 1995. IL-12 promotes enhanced recovery from vesicular stomatitis virus infection of the central nervous system. J. Immunol. 155:5684-5689. [PubMed] [Google Scholar]
- 8.Binder, G. K., and D. E. Griffin. 2001. Interferon-γ-mediated site-specific clearance of alphavirus from CNS neurons. Science 293:303-306. [DOI] [PubMed] [Google Scholar]
- 9.Burkhart, C., G. Freer, R. Castro, L. Adorini, K.-H. Wiesmüller, R. M. Zinkernagel, and H. Hengartner. 1994. Characterization of T-helper epitopes of the glycoprotein of vesicular stomatitis virus. J. Virol. 68:1573-1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Christian, A. Y., M. Barna, Z. Bi, and C. S. Reiss. 1996. Host immune response to vesicular stomatitis virus infection of the central nervous system in C57BL/6 mice. Viral Immunol. 9:195-205. [DOI] [PubMed] [Google Scholar]
- 11.Conzelmann, K.-K. 1996. Genetic manipulation of non-segmented negative-strand RNA viruses. J. Gen. Virol. 77:381-389. [DOI] [PubMed] [Google Scholar]
- 12.Conzelmann, K.-K. 1998. Nonsegmented negative-strand RNA viruses: genetics and manipulation of viral genomes. Annu. Rev. Genet. 32:123-162. [DOI] [PubMed] [Google Scholar]
- 13.Coutelier, J.-P., J. T. M. van der Logt, F. W. A. Heessen, A. Vink, and J. van Snick. 1988. Virally induced modulation of murine IgG antibody subclasses. J. Exp. Med. 168:2373-2378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coutelier, J.-P., J. T. M. van der Logt, F. W. A. Heessen, G. Warnier, and J. van Snick. 1987. IgG2a restriction of murine antibodies elicited by viral infections. J. Exp. Med. 165:64-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flanagan, E. B., J. M. Zamparo, L. A. Ball, L. L. Rodriguez, and G. W. Wertz. 2001. Rearrangement of the genes of vesicular stomatitis virus eliminates clinical disease in the natural host: new strategy for vaccine development. J. Virol. 75:6107-6114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Flanagan, E. B., L. A. Ball, and G. W. Wertz. 2000. Moving the glycoprotein gene of vesicular stomatitis virus to promoter-proximal positions accelerates and enhances the protective immune response. J. Virol. 74:7895-7902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forger, J. M., III, R. T. Bronson, A. S. Huang, and C. S. Reiss. 1991. Murine infection by vesicular stomatitis virus: initial characterization of the H-2d system. J. Virol. 65:4950-4958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Howard, M., and G. Wertz. 1989. Vesicular stomatitis virus RNA replication: a role for the NS protein. J. Gen. Virol. 70:2683-2694. [DOI] [PubMed] [Google Scholar]
- 19.Huneycutt, B. S., I. V. Plakhov, Z. Shusterman, S. M. Bartido, A. Huang, C. S. Reiss, and C. Aoki. 1994. Distribution of vesicular stomatitis virus proteins in the brains of BALB/c mice following intranasal inoculation: an immunohistological analysis. Brain Res. 635:81-95. [DOI] [PubMed] [Google Scholar]
- 20.Ireland, D. D. C., T. Bang, T. Komatsu, and C. S. Reiss. 1999. Delayed administration of interleukin-12 is efficacious in promoting recovery from lethal viral encephalitis. Viral Immunol. 12:35-40. [DOI] [PubMed] [Google Scholar]
- 21.Iverson, L. E., and J. K. Rose. 1981. Localization attenuation and discontinuous synthesis during vesicular stomatitis virus transcription. Cell 23:477-484. [DOI] [PubMed] [Google Scholar]
- 22.Kelley, J. R., S. U. Emerson, and R. R. Wagner. 1972. The glycoprotein of vesicular stomatitis virus is the antigen that gives rise to and reacts with neutralizing antibody. J. Virol. 10:1231-1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Komatsu, T., and C. S. Reiss. 1997. IFN-γ is not required in the IL-12 response to vesicular stomatitis virus infection in the olfactory bulb. J. Immunol. 159:3444-3452. [PubMed] [Google Scholar]
- 24.Komatsu, T., Z. Bi, and C. S. Reiss. 1996. Interferon-γ induced type I nitric oxide synthase activity inhibits viral replication in neuron. J. Neuroimmunol. 68:101-108. [DOI] [PubMed] [Google Scholar]
- 25.Komatsu, T., M. Barna, and C. S. Reiss. 1997. Interleukin-12 promotes recovery from viral encephalitis. Viral Immunol. 10:35-47. [DOI] [PubMed] [Google Scholar]
- 26.Kündig, T. M., I. Castelmur, M. F. Bachmann, D. Abraham, D. Binder, H. Hengartner, and R. M. Zinkernagel. 1993. Fewer protective cytotoxic T-cell epitopes than T-helper cell epitopes on vesicular stomatitis virus. J. Virol. 67:3680-3683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lefrancois, L., and D. S. Lyles. 1982. The interaction of antibody with the major surface glycoprotein of vesicular stomatitis virus. I. Analysis of neutralizing epitopes with monoclonal antibodies. Virology 121:157-167. [PubMed] [Google Scholar]
- 28.Lundh, B., K. Kristensson, and E. Norrby. 1987. Selective infections of olfactory and respiratory epithelium by vesicular stomatitis virus and Sendai viruses. Neuropathol. Appl. Neurobiol. 13:111-122. [DOI] [PubMed] [Google Scholar]
- 29.Manetti, R., P. Parronchi, M. G. Giudizi, M. P. Piccinni, E. Maggi, G. Trinchieri, and S. Romagnani. 1993. Natural killer stimulatory factor (interleukin 12) induces T helper type-1 (Th1)-specific immune responses and inhibits the development of IL-4-producing cells. J. Exp. Med. 177:1199-1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marcus, P. I., M. J. Sekellick, L. A. Ball, and G. W. Wertz. 1999. Phenotypic variation in the interferon-inducing capacity of vesicular stomatitis virus with rearranged genomes. J. Interferon Res. 19:S101. [Google Scholar]
- 31.McSharry, J. J., and P. W. Choppin. 1978. Biological properties of the VSV glycoprotein. I. Effects of the isolated glycoprotein on host macromolecular synthesis. Virology 84:172-182. [DOI] [PubMed] [Google Scholar]
- 32.Miyoshi, K., D. H. Harter, and K. C. Hsu. 1971. Neuropathological and immunofluorescence studies of experimental vesicular stomatitis encephalitis in mice. J. Neuropathol. Exp. Neurol. 30:266-277. [DOI] [PubMed] [Google Scholar]
- 33.Patton, J. T., N. L. Davis, and G. W. Wertz. 1984. N protein alone satisfies the requirement for protein synthesis during RNA replication of vesicular stomatitis virus. J. Virol. 49:303-309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Peluso, R. W., and S. A. Moyer. 1988. Viral proteins required for the in vitro replication of vesicular stomatitis virus defective interfering particle genome RNA. Virology 162:369-376. [DOI] [PubMed] [Google Scholar]
- 35.Perlmutter, R. M., D. Hansburg, D. E. Briles, R. A. Nicolotti, and J. M. Davie. 1978. Subclass restriction of murine anti-carbohydrate antibodies. J. Immunol. 121:566-572. [PubMed] [Google Scholar]
- 36.Plakhov, I. V., E. E. Arlund, C. Aoki, and C. S. Reiss. 1995. The earliest events in vesicular stomatitis virus infection of the murine olfactory neuroepithelium and entry of the central nervous system. Virology 209:257-262. [DOI] [PubMed] [Google Scholar]
- 37.Pringle, C. R. 1991. The genetics of paramyxoviruses, p. 1-39. In D. Kingsbury (ed.), The paramyxoviruses. Plenum Press, New York, N.Y.
- 38.Pringle, C. R., and A. J. Easton. 1997. Monopartite negative strand RNA genomes. Semin. Virol. 8:49-57. [Google Scholar]
- 39.Reed, E. J., and H. Muench. 1938. A simple method for estimating fifty percent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 40.Reiss, C. S., I. V. Plakov, and T. Komatsu. 1998. Viral replication in olfactory receptor neurons and entry into the olfactory bulb and brain. Ann. N. Y. Acad. Sci. 30:752-761. [DOI] [PubMed] [Google Scholar]
- 41.Riffenburgh, R. H. 1999. Common tests on ranked data, p. 279-283. In Statistics in medicine. Academic Press, San Diego, Calif.
- 42.Riffenburgh, R. H. 1999. Medical decisions: statistical testing, risks, and odds, p. 121-127. In Statistics in medicine. Academic Press, San Diego, Calif.
- 43.Roberts, A., L. Buonocore, R. Price, J. Foreman, and J. K. Rose. 1999. Attenuated vesicular stomatitis viruses as vaccine vectors. J. Virol. 73:3723-3732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rosenthal, K. L., M. B. Oldstone, H. Hengartner, and R. M. Zinkernagel. 1983. Specificity of in vitro cytotoxic T cell clones directed against vesicular stomatitis virus. J. Immunol. 131:475-478. [PubMed] [Google Scholar]
- 45.Sabin, A., and P. Olitsky. 1938. Influence of host factors on neuroinvasiveness of vesicular stomatitis virus. I. Effect of age on the invasion of the brain by virus instilled in the nose. J. Exp. Med. 66:15-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sabin, A., and P. Olitsky. 1938. Influence of host factors on neuroinvasiveness of vesicular stomatitis virus. III. Effect of age and pathway of infection on the character and localization of lesions in the central nervous systems. J. Exp. Med. 67:201-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stevens, T. L., A. Bossie, V. M. Sanders, R. Fernandez-Botran, R. L. Coffman, T. R. Mosmann, and E. S. Vitetta. 1988. Regulation of antibody isotype secretion by subsets of antigen-specific helper T cells. Nature 334:255-258. [DOI] [PubMed] [Google Scholar]
- 48.Van den Pol, A. N., K. P. Dalton, and J. K. Rose. 2002. Relative neurotropism of a recombinant rhabdovirus expressing a green fluorescent envelope glycoprotein. J. Virol. 76:1309-1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Villarreal, L. P., M. Breindl, and J. J. Holland. 1976. Determination of molar ratios of vesicular stomatitis virus induced RNA species in BHK21 cells. Biochemistry 15:1663-1667. [DOI] [PubMed] [Google Scholar]
- 50.Wagner, R. R. 1974. Pathogenicity and immunogenicity for mice of temperature-sensitive mutants of vesicular stomatitis virus. Infect. Immun. 10:309-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wertz, G. W., M. B. Howard, N. Davis, and J. Patton. 1987. The switch from transcription to replication of a negative-strand RNA virus. Cold Spring Harbor Symp. Quant. Biol. 52:367-371. [DOI] [PubMed] [Google Scholar]
- 52.Wertz, G. W., V. P. Perepelitsa, and L. A. Ball. 1998. Gene rearrangement attenuates expression and lethality of a nonsegmented negative strand RNA virus. Proc. Natl. Acad. Sci. USA 95:3501-3506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Whelan, S. P. J., L. A. Ball, J. N. Barr, and G. T. W. Wertz. 1995. Recovery of infectious vesicular stomatitis virus entirely from cDNA clones. Proc. Natl. Acad. Sci. USA 92:8388-8392. [DOI] [PMC free article] [PubMed] [Google Scholar]