Abstract
Interleukin 6 (IL-6) has manifold biological functions involved in the immune or inflammatory responses of the host to various stimuli. Here we asked whether IL-6 might be responsible for manifestations of Kawasaki disease (KD), such as immunoglobulin hypersecretion, lymphocyte activation and systemic vasculitis. IL-6 activity in the serum was determined by a sensitive colorimetric assay using an IL-6-dependent murine hybridoma clone. Usually sera from healthy or afebrile donors contained only negligible levels of IL-6 activity below the detection threshold of the assay. Importantly it was found that serum IL-6 was markedly elevated in all patients with acute KD. Serum levels of IL-6 activity gradually diminished during the course of the disease and reached undetectable or lower levels at the convalescent phase. However, such elevated levels of serum IL-6 activity were also observed in the majority of other febrile diseases, such as bacterial or viral infections, indicating that the appearance of IL-6 in the serum could generally occur in febrile or inflammatory disease conditions. Serum IL-6 activity correlated with serum concentrations of some acute phase proteins (APP), such as C-reactive protein, haptoglobin and alpha 1-acid glycoprotein, implying its role for modulating induction of APP in vivo. IL-6 is well known to be secreted by a variety of cell types. Further studies, including immunohistochemical analysis using anti-IL-6 antibody, will be necessary to examine whether the source of serum IL-6 in KD might be different from that seen in other diseases.
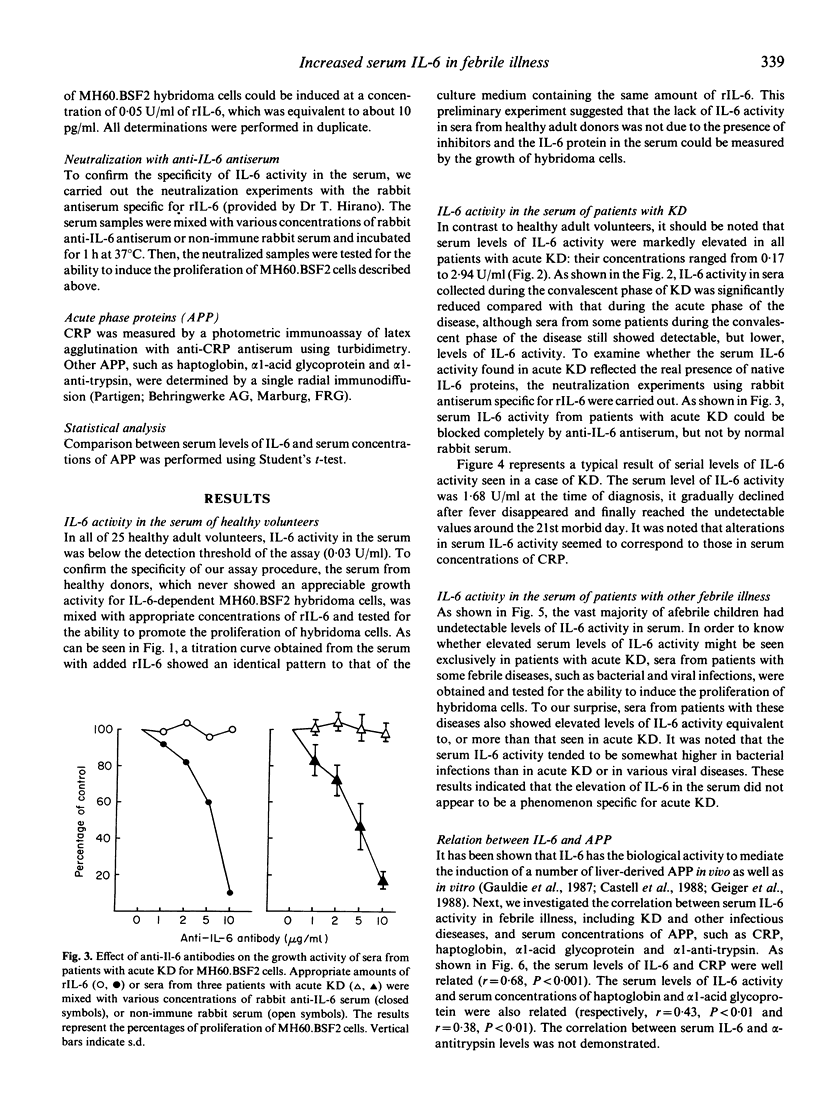
Full text
PDF




Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aarden L. A., De Groot E. R., Schaap O. L., Lansdorp P. M. Production of hybridoma growth factor by human monocytes. Eur J Immunol. 1987 Oct;17(10):1411–1416. doi: 10.1002/eji.1830171004. [DOI] [PubMed] [Google Scholar]
- Astaldi G. C., Janssen M. C., Lansdorp P., Willems C., Zeijlemaker W. P., Oosterhof F. Human endothelial culture supernatant (HECS): a growth factor for hybridomas. J Immunol. 1980 Oct;125(4):1411–1414. [PubMed] [Google Scholar]
- Baumann H., Jahreis G. P., Sauder D. N., Koj A. Human keratinocytes and monocytes release factors which regulate the synthesis of major acute phase plasma proteins in hepatic cells from man, rat, and mouse. J Biol Chem. 1984 Jun 10;259(11):7331–7342. [PubMed] [Google Scholar]
- Castell J. V., Gómez-Lechón M. J., David M., Hirano T., Kishimoto T., Heinrich P. C. Recombinant human interleukin-6 (IL-6/BSF-2/HSF) regulates the synthesis of acute phase proteins in human hepatocytes. FEBS Lett. 1988 May 23;232(2):347–350. doi: 10.1016/0014-5793(88)80766-x. [DOI] [PubMed] [Google Scholar]
- Content J., De Wit L., Poupart P., Opdenakker G., Van Damme J., Billiau A. Induction of a 26-kDa-protein mRNA in human cells treated with an interleukin-1-related, leukocyte-derived factor. Eur J Biochem. 1985 Oct 15;152(2):253–257. doi: 10.1111/j.1432-1033.1985.tb09191.x. [DOI] [PubMed] [Google Scholar]
- Darlington G. J., Wilson D. R., Lachman L. B. Monocyte-conditioned medium, interleukin-1, and tumor necrosis factor stimulate the acute phase response in human hepatoma cells in vitro. J Cell Biol. 1986 Sep;103(3):787–793. doi: 10.1083/jcb.103.3.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa S., Matsubara T., Jujoh K., Yone K., Sugawara T., Sasai K., Kato H., Yabuta K. Peripheral blood monocyte/macrophages and serum tumor necrosis factor in Kawasaki disease. Clin Immunol Immunopathol. 1988 Aug;48(2):247–251. doi: 10.1016/0090-1229(88)90088-8. [DOI] [PubMed] [Google Scholar]
- Ganapathi M. K., Schultz D., Mackiewicz A., Samols D., Hu S. I., Brabenec A., Macintyre S. S., Kushner I. Heterogeneous nature of the acute phase response. Differential regulation of human serum amyloid A, C-reactive protein, and other acute phase proteins by cytokines in Hep 3B cells. J Immunol. 1988 Jul 15;141(2):564–569. [PubMed] [Google Scholar]
- Geiger T., Andus T., Klapproth J., Hirano T., Kishimoto T., Heinrich P. C. Induction of rat acute-phase proteins by interleukin 6 in vivo. Eur J Immunol. 1988 May;18(5):717–721. doi: 10.1002/eji.1830180510. [DOI] [PubMed] [Google Scholar]
- Green L. M., Reade J. L., Ware C. F. Rapid colorimetric assay for cell viability: application to the quantitation of cytotoxic and growth inhibitory lymphokines. J Immunol Methods. 1984 May 25;70(2):257–268. doi: 10.1016/0022-1759(84)90190-x. [DOI] [PubMed] [Google Scholar]
- Hirano T., Yasukawa K., Harada H., Taga T., Watanabe Y., Matsuda T., Kashiwamura S., Nakajima K., Koyama K., Iwamatsu A. Complementary DNA for a novel human interleukin (BSF-2) that induces B lymphocytes to produce immunoglobulin. Nature. 1986 Nov 6;324(6092):73–76. doi: 10.1038/324073a0. [DOI] [PubMed] [Google Scholar]
- Hirose S., Hamashima Y. Morphological observations on the vasculitis in the mucocutaneous lymph node syndrome. A skin biopsy study of 27 patients. Eur J Pediatr. 1978 Aug 17;129(1):17–27. doi: 10.1007/BF00441370. [DOI] [PubMed] [Google Scholar]
- Houssiau F. A., Bukasa K., Sindic C. J., Van Damme J., Van Snick J. Elevated levels of the 26K human hybridoma growth factor (interleukin 6) in cerebrospinal fluid of patients with acute infection of the central nervous system. Clin Exp Immunol. 1988 Feb;71(2):320–323. [PMC free article] [PubMed] [Google Scholar]
- Kato H., Koike S., Yamamoto M., Ito Y., Yano E. Coronary aneurysms in infants and young children with acute febrile mucocutaneous lymph node syndrome. J Pediatr. 1975 Jun;86(6):892–898. doi: 10.1016/s0022-3476(75)80220-4. [DOI] [PubMed] [Google Scholar]
- Kawasaki T. [Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children]. Arerugi. 1967 Mar;16(3):178–222. [PubMed] [Google Scholar]
- Kishimoto T., Hirano T. Molecular regulation of B lymphocyte response. Annu Rev Immunol. 1988;6:485–512. doi: 10.1146/annurev.iy.06.040188.002413. [DOI] [PubMed] [Google Scholar]
- Kohase M., Henriksen-DeStefano D., May L. T., Vilcek J., Sehgal P. B. Induction of beta 2-interferon by tumor necrosis factor: a homeostatic mechanism in the control of cell proliferation. Cell. 1986 Jun 6;45(5):659–666. doi: 10.1016/0092-8674(86)90780-4. [DOI] [PubMed] [Google Scholar]
- Landing B. H., Larson E. J. Are infantile periarteritis nodosa with coronary artery involvement and fatal mucocutaneous lymph node syndrome the same? Comparison of 20 patients from North America with patients from Hawaii and Japan. Pediatrics. 1977 May;59(5):651–662. [PubMed] [Google Scholar]
- Le J., Vilcek J. Tumor necrosis factor and interleukin 1: cytokines with multiple overlapping biological activities. Lab Invest. 1987 Mar;56(3):234–248. [PubMed] [Google Scholar]
- Lee L. A., Burns J., Glode M., Harmon C., Weston W. L. No autoantibodies to nuclear antigens in the Kawasaki syndrome. N Engl J Med. 1983 Apr 28;308(17):1034–1034. doi: 10.1056/NEJM198304283081718. [DOI] [PubMed] [Google Scholar]
- Leung D. Y., Chu E. T., Wood N., Grady S., Meade R., Geha R. S. Immunoregulatory T cell abnormalities in mucocutaneous lymph node syndrome. J Immunol. 1983 May;130(5):2002–2004. [PubMed] [Google Scholar]
- Leung D. Y., Geha R. S., Newburger J. W., Burns J. C., Fiers W., Lapierre L. A., Pober J. S. Two monokines, interleukin 1 and tumor necrosis factor, render cultured vascular endothelial cells susceptible to lysis by antibodies circulating during Kawasaki syndrome. J Exp Med. 1986 Dec 1;164(6):1958–1972. doi: 10.1084/jem.164.6.1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuda T., Hirano T., Kishimoto T. Establishment of an interleukin 6 (IL 6)/B cell stimulatory factor 2-dependent cell line and preparation of anti-IL 6 monoclonal antibodies. Eur J Immunol. 1988 Jun;18(6):951–956. doi: 10.1002/eji.1830180618. [DOI] [PubMed] [Google Scholar]
- May L. T., Ghrayeb J., Santhanam U., Tatter S. B., Sthoeger Z., Helfgott D. C., Chiorazzi N., Grieninger G., Sehgal P. B. Synthesis and secretion of multiple forms of beta 2-interferon/B-cell differentiation factor 2/hepatocyte-stimulating factor by human fibroblasts and monocytes. J Biol Chem. 1988 Jun 5;263(16):7760–7766. [PubMed] [Google Scholar]
- Nijsten M. W., de Groot E. R., ten Duis H. J., Klasen H. J., Hack C. E., Aarden L. A. Serum levels of interleukin-6 and acute phase responses. Lancet. 1987 Oct 17;2(8564):921–921. doi: 10.1016/s0140-6736(87)91413-9. [DOI] [PubMed] [Google Scholar]
- Ritchie D. G., Fuller G. M. Hepatocyte-stimulating factor: a monocyte-derived acute-phase regulatory protein. Ann N Y Acad Sci. 1983 Jun 27;408:490–502. doi: 10.1111/j.1749-6632.1983.tb23268.x. [DOI] [PubMed] [Google Scholar]
- Sugawara T., Hattori S., Hirose S., Furukawa S., Yabuta K., Shirai T. Immunopathology of the skin lesion of Kawasaki disease. Prog Clin Biol Res. 1987;250:185–192. [PubMed] [Google Scholar]
- Van Oers M. H., Van der Heyden A. A., Aarden L. A. Interleukin 6 (IL-6) in serum and urine of renal transplant recipients. Clin Exp Immunol. 1988 Feb;71(2):314–319. [PMC free article] [PubMed] [Google Scholar]



