Abstract
There has been considerable interest in understanding what may have led to Uganda's dramatic decline in HIV prevalence, one of the world's earliest and most compelling AIDS prevention successes. Survey and other data suggest that a decline in multi-partner sexual behavior is the behavioral change most likely associated with HIV decline. It appears that behavior change programs, particularly involving extensive promotion of “zero grazing” (faithfulness and partner reduction), largely developed by the Ugandan government and local NGOs including faith-based, women’s, people-living-with-AIDS and other community-based groups, contributed to the early declines in casual/multiple sexual partnerships and HIV incidence and, along with other factors including condom use, to the subsequent sharp decline in HIV prevalence. Yet the debate over “what happened in Uganda” continues, often involving divisive abstinence-versus-condoms rhetoric, which appears more related to the culture wars in the USA than to African social reality.
KEY WORDS: HIV-AIDS prevention, Africa, behavior change, ABC, partner reduction, multi-sectoral response.
INTRODUCTION
Much debate over HIV prevention has arisen in recent years. While both international and locally-based AIDS organizations continue to seek funds to scale up prevention efforts, researchers and policymakers have debated the meaning of Uganda's unprecedented HIV prevalence decline. One school of thought, including Stoneburner and Low-Beer (2004), Shelton et al.(2004), Hearst and Chen (2004), Green (2003), Wilson (2004), Epstein (2004, 2005b), and Cohen (2004), conclude that a decrease in casual/multiple sexual partner behavior, rather than mainly condom use or increases in mortality, was primarily responsible for Uganda's success. Others have argued in favor of the more prevailing prevention approach that has centered on condom promotion and HIV testing as well as an array of broader structural factors, such as poverty, gender violence and conflict (Fenton, 2004; Halperin and Allen, 2000; Singh et al., 2003; Wawer et al., 2005; Shelton et al., 2005).
It is important to note that the behavior change-based analysis of the Uganda prevention success, much of it now published in leading scientific journals, has not argued that such broader factors, as well as condom use, were unimportant; rather, the argument has focused more on the relative impact of the different “ABC” factors (Abstinence, Being faithful and Condom use), especially in more generalized epidemics driven mainly by heterosexual transmission. Moreover, it is worth noting that most of the critics of the partner reduction-focused analysis likewise do not take extreme positions (i.e., condoms only, with no role for partner reduction), although it appears that some of these critics have, perhaps inadvertently, helped to re-polarize what has come to be called the ABC debate – a discourse which has often centered on divisive arguments between “A” versus “C” (Epstein, 2004, 2005b; Halperin et al., 2004; Shelton et al., 2004; Shelton, 2005; Wilson; 2004, Cohen, 2004).
HIV PREVALENCE DECLINE IN UGANDA
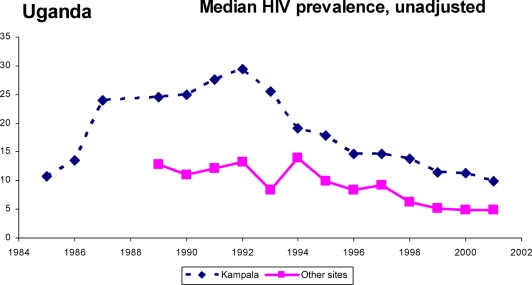
Uganda is considered by UNAIDS (2004) and others to be one of the world's earliest and most compelling national success stories in combating the spread of HIV. This paper attempts to understand, based on the available evidence, what may have happened to bring about a decline in HIV prevalence (and more to the point, HIV incidence) in Uganda, not only epidemiologically but, at least as importantly, programattically as well. The east African country has experienced a dramatic decline in prevalence during the past decade, especially among younger age cohorts. According to Ministry of Health and other data (Okware et al., 2001), prevalence among pregnant women attending antenatal clinics has declined consistently since the early 1990s at nearly all of the country's sentinel sites (see Fig. 1). Similarly large—and even earlier—declines have been observed among military recruits, blood donors and other population-level cohorts (Low-Beer, 2002; Stoneburner and Low-Beer, 2004). Although it is true that there have been some exaggerated estimates of prevalence decline, as noted even by the skeptic Parkhurst (2002), this does not detract from Uganda's genuine prevention success.
Fig. 1.
HIV prevalence among pregnant women in Uganda. Source: HIV/AIDS surveillance report, STD/AIDS control programme, Ministry of Health, Uganda, June 2001.
While there is not much data available regarding trends in HIV incidence it also appears to have fallen significantly. In one rural site, Masaka, seroincidence fell from 7.6 per thousand per year in 1990 to 3.2 per thousand per year by 1998 (Mbulaiteye et al., 2002). As with prevalence, the decline was especially pronounced among younger women. At most Ugandan antenatal clinic sites, seroprevalence among 15–19-year-old pregnant women, somewhat of a rough proxy for HIV incidence, tended to decrease significantly from the early 1990s, when these data were first collected, until the mid to late 1990s and it has remained low since then (although there has been an increase recently, for the first time in a decade). Population-based data from Masaka suggests that prevalence among all young women (ie, not only sexually active/pregnant females) ages 15–19 began declining by the end of the 1980s (Mbulaiteye et al., 2002).
Based on such trends and the fact that national seroprevalence among pregnant women (of all ages) peaked in 1992 and furthermore that epidemiological analysis and modeling suggests there would have been a lag of several years between the initiation of behavior change/incidence decline (especially among men) and the subsequent prevalence decline (in pregnant women) (Shelton et al., 2006), it is most probable that HIV incidence in Uganda peaked sometime during the late 1980s (Low-Beer, 2002; Stoneburner and Low-Beer, 2004; Shelton et al., 2004). Regarding HIV prevalence, the U.S. Census Bureau/Joint United Nations Programme on HIV/AIDS (UNAIDS 2004) estimates that national HIV prevalence for all adults peaked at around 15% in the early 1990s and fell to about 4% by 2003 (although a 2004 population-based survey found approximately 7% adult prevalence; Measure DHS 2005). This degree of national prevalence decline is unique worldwide and has been the subject of curiosity and controversy since the late-1990s and more recently has come under even more intense scientific scrutiny (Allen and Heald, 2004; Green, 2003; Parkhurst, 2002; Stoneburner and Low-Beer, 2004; Wawer et al., 2005).
Observed consistently over time and across many different geographic and demographic populations, Uganda's falling HIV prevalence is unlikely to be due merely to measurement bias or only to a “natural die-off syndrome,” but at least in large part to a number of behavioral changes that have been identified in various population-based surveys as well as qualitative studies. While some have postulated that the prevalence decline was primarily a result of so many people succumbing to the disease that the rate of new infections was simply outweighed by the numbers of AIDS deaths (e.g., Wawer et al., 2005), a number of other African regions have experienced nearly as old—and at least as severe—epidemics as Uganda’s, yet prevalence has yet to decline substantially at the population level. Moreover, the large decline in prevalence among younger age cohorts in Uganda cannot be explained by AIDS mortality, as very few people under age 20 die of AIDS.
TRENDS IN DECLINING CASUAL/MULTIPLE SEXUAL PARTNERSHIPS
Given that HIV seroincidence probably peaked sometime in the late 1980s, it is important to compare data on sexual behavior from that period to subsequent findings from the 1990s. It is not particularly useful to compare mainly between the 1995 and 2000 Demographic and Health (DHS) surveys, as some analysts have proposed (e.g. Singh et al., 2002), since much of Uganda's prevention “miracle” appears to have occurred in the late 1980s and probably into the early 1990s. Thus, some of the widely publicized conclusions of a recent study in Rakai district, focusing on HIV surveillance and behavioral trends after 1994 (Wawer et al., 2005), although of interest in explaining some more recent trends, are of little help in understanding the main historical HIV decline in Uganda (see Bessinger et al., 2003; Shelton, 2005; Mosley, 2005; footnote on Wawer et al. study in Epstein, 2005a).
Unfortunately, little HIV-related data was collected in the 1988/9 DHS survey (and no males were then surveyed). The WHO's Global Program on AIDS (GPA) surveys from 1988/9 and 1995, although not fully nationally representative (Bessinger et al., 2003), nonetheless did sample large numbers of people in the most HIV affected parts of the country. In the GPA surveys, the proportion of single males ages 15–24 reporting premarital sex decreased from 60% in 1989 to 23% in 1995. There were similarly large declines in the number of respondents in the GPA surveys reporting casual sex in the previous year, from 35 to 15% among men and from 16 to 6% among women. Furthermore–and this appears particularly critical given the epidemiological importance of multiple partnership/sexual networking dynamics (Bernstein et al., 1998; Halperin and Epstein, 2004; Shelton et al., 2004; Wilson, 2004; Auvert et al., 2000), the proportion of males reporting three or more non-regular partners fell even more dramatically between 1989 and 1995 (Fig. 2). The particular significance of partner reduction trends in Uganda will be explored below.
Fig. 2.
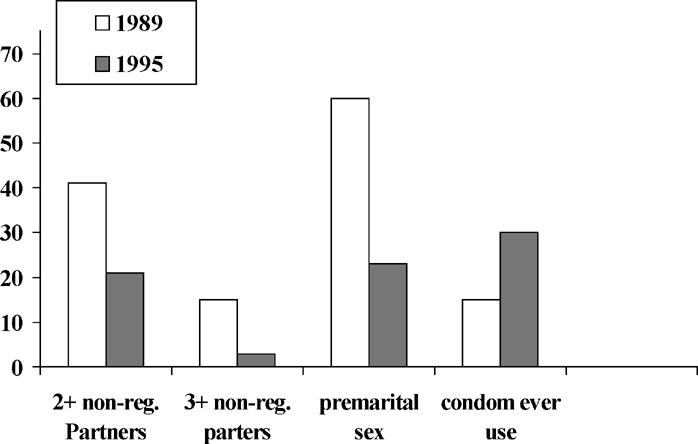
Changes in sexual behavior among men in Uganda. Source: WHO/GPA surveys, 1989 &1995.
KEY ELEMENTS OF THE NATIONAL RESPONSE
The relationships between the various behavior change interventions that were implemented in Uganda and the ensuing decline in HIV prevalence are complex and not yet completely understood. However, changes in age of sexual debut, casual and commercial sex trends, partner reduction and condom use all appear to have played key roles in the continuing declines. Although it is believed that HIV knowledge, risk perception and risk avoidance/risk reduction options can ultimately lead to reduced HIV incidence, there is a complex set of epidemiological, socio-cultural, political and other elements that likely affected the course of the epidemic in Uganda. Many of these elements appear to be absent or less evident in those African countries that have not yet experienced significant national prevalence declines, such as South Africa, Botswana and Malawi (Allen and Heald, 2004; Bessinger et al., 2003; Cohen, 2004; Epstein, 2004; Green, 2003; Hearst and Chen, 2004; Stoneburner and Low-Beer, 2004). These key elements are summarized in roughly chronological order below:
High-Level Political Support and Multi-Sectoral Response
In 1986, after 15 years of civil strife, Uganda's new head of state President Yoweri Museveni responded to evidence of a serious emerging disease epidemic with a proactive commitment to prevention. In face-to-face interactions with Ugandans at all levels, he emphasized that fighting AIDS was a “patriotic duty” requiring openness, communication and strong leadership from the village level to the State House. His charismatic directness in addressing the threat placed HIV/AIDS on the development agenda and encouraged constant and candid national media coverage of all aspects of the epidemic, including/emphasizing behavior change. This early, high-level support fostered a multi-sectoral response, prioritizing HIV/AIDS and enlisting a wide variety of national participants in the “war” against the decimating disease popularly known as “Slim” (Epstein, 2004; Green, 2003; Kaleeba et al., 2000).
In 1986, Uganda established a National AIDS Control Program (ACP) and the national sentinel surveillance system, which has tracked the epidemic since 1987, began with four sites and by 2000 included 15; also of importance, there has been surveillance of AIDS cases since 1986. Eventually, in 1992, the multi-sectoral Uganda AIDS Commission (UAC) was created to more closely coordinate and monitor the national AIDS strategy. The UAC prepared a National Operational Plan to guide implementing agencies, sponsored task forces and encouraged the establishment of AIDS Control Programs in other ministries including Defense, Education, Gender and Social Affairs. As of 2001, there were also at least 700 agencies—governmental and nongovernmental—working on HIV/AIDS issues across all districts in Uganda (Kirby, 2003).
Decentralized Planning and Implementation for Behavior Change Communication
Beginning in 1986, the Ugandan ACP (which later became the STD/AIDS Control Program, in 1994) launched an aggressive public media campaign that included print materials, radio, billboards and community mobilization for a grass-roots offensive against HIV and has since then trained thousands of community-based AIDS counselors, health educators, peer educators and other types of specialists. Led by their leaders’ examples, the general population in both urban and rural areas eventually also joined the fight against AIDS, so that it became a “patriotic duty” to support the effort. Spreading the word involved not just “information and education” but rather a fundamental behavior change-based approach to communicating and motivating. Decentralization itself was actually a type of local empowerment that involved local allocation of resources—in and of itself a motivating force (Kaleeba et al., 2000; Marum, 2002; Wilson, 2004).
Although media—both mass media (e.g., the ominous, daily drum-beating on the radio in the late 1980s, still vividly recalled by Ugandans; Kirby, 2003) as well as various locally developed forms such as community dramas—clearly were important vehicles for raising awareness and fostering changes in behavioral norms, Uganda's approach to behavioral change relied primarily on community-based and face-to-face communication (Allen and Heald, 2004; Stoneburner and Low-Beer, 2004; Wilson, 2004). Strong nongovernmental organization (NGO) and community-based support led to flexible, creative and culturally appropriate interventions that helped facilitate individual behavior change as well as changes in community norms, despite extreme levels of household poverty following the civil war period. Such “low-tech” approaches also led to the sensitization and subsequent involvement in AIDS awareness and education of not only health personnel, traditional healers and traditional birth attendants, but influential people normally not involved in health issues such as political, community and religious leaders, teachers and administrators, traders, leaders of women's and youth associations and other representatives of key grassroots community groups (Green, 2003; Kirby, 2003; Wilson, 2004). One of the contributions of international donors such as USAID was in supporting community-level BCC by directly funding salaries or in-kind support of peer educators and others at the local level (Marum, 2002). In other countries, community health workers and peer educators are often expected to work as volunteers, without salary (Green, 1996).
Sustained interpersonal communication interventions reached not only the general population, but also key target groups including female sex workers and their clients, soldiers, fishermen, long-distance drivers, traders, bar girls, police and students and without generally creating a highly stigmatizing climate. In comparing DHS data from the mid-1990s, Uganda stands out among all African countries for which such data exist, in the proportion of respondents who cite either friends, relatives, or community meetings as sources of AIDS information (99.2%). This rate is twice that of many African countries and it seems to be a measure of Uganda's interpersonal BCC strategy (Green, 2003; Kaleeba et al., 2000; Stoneburner and Low-Beer, 2004).
Religious Leaders and Faith-Based Organizations on the Front Lines
Mainstream faith-based organizations wield enormous influence in Africa. Early and significant mobilization of Ugandan religious leaders and organizations resulted in their active participation in AIDS education and prevention activities (Kaleeba et al., 2000; Kagimu et al., 1998; Kirby, 2003; Sabatier, 1988). Also, Mission hospitals were among the first to develop AIDS care and support programs in Uganda; for example, the Catholic Church and Catholic mission hospitals provided leadership in designing AIDS mobile home care projects and special programs for AIDS widows and orphans (Kaleeba et al., 2000). The three chairpersons of the Uganda AIDS Commission have included an Anglican and a Catholic Bishop. In 1990, the Islamic Medical Association of Uganda (IMAU) piloted an AIDS education project in rural Muslim communities that evolved into a larger effort to train local religious leaders and lay community workers. Documenting increases in correct knowledge and decreases in risky behaviors, the IMAU project was selected as a “Best Practices Case Study” by UNAIDS (Kagimu et al., 1998; UNAIDS, 1999; Wabwire-Mangen et al., 1998).
In the early 1990s, the Anglican Church implemented an AIDS prevention program in 10 out of (then) 40 districts of Uganda. Clergy and laity were trained in AIDS prevention, using a peer education approach. AIDS education messages were delivered from the pulpit in sermons, as well as at funerals, weddings and other occasions. A USAID-funded evaluation of populations reached by this “CHUSA” project found a dramatic change in reported levels of risky behavior, especially partner reduction, during the early 1990s (Ruteikara et al., 1995). These survey findings were supported by focus group discussions involving community leaders and youth, where it was asserted that, for example, “Before the onset of AIDS, one could have five sexual partners, or even have sex on a chain basis, but these days you realize that there is a lot of self-constraint. Burials, people falling sick from AIDS and religious leaders have awakened people … The number of sexual partners has [been] reduced.” (Ruteikara et al., 1995).
Addressing Women, Youth, and Stigma and Discrimination
Linked to high-level political support and grassroots-level communication for behavior change was a strong emphasis on greater empowerment of women and girls; targeting youth both in and out of school; and aggressively fighting stigma and discrimination against people living with HIV/AIDS (PLWHAs). Since 1987, the first year of the School Health Education Program, teachers have been trained to integrate HIV education and sexual behavior change messages into curricula (Green, 2003; Kaleeba et al., 2000). At the same time, the country's President and his political party have attempted to empower women and youth by giving them more political voice, including in Parliament where by law women make up a minimum one-third of the members (in addition to four members elected by youth caucuses). At least as importantly, grassroots women's organizations have fought to empower women socially, economically and legally. Their campaigns have resulted in legal reforms pertinent to the fight against AIDS, including strengthening of rape and defilement laws and laws governing property rights for women.
With regard to behavior change, many women and women's empowerment organizations supported approaches like “Zero Grazing,” which were aimed mainly at the behavior of males, particularly those older men with disposable income who were likely the principal “core transmitters” of the epidemic (Green, 2003: 169–172, Wilson, 2004; Murphy et al., 2003)
Youth-friendly approaches, such as Straight Talk, eventually supported behavior change through promoting delay of sexual debut, remaining abstinent, remaining faithful to one uninfected person if “you’ve already started,” “zero-grazing,” and using condoms if “you’re going to move around.” In an African Medical and Research Foundation study in Soroti District (n=400), in 1994 nearly 60% of boys and girls ages 13–16 reported having experienced intercourse, but in 2001 that proportion had decreased to below 5% (AMREF, 2001). While it is entirely possible that such a magnitude of self-reported behavior change is somewhat exaggerated, such findings–coupled with various other behavioral data–suggest that a substantial shift in behavioral norms likely has occurred in Uganda.
Respecting and protecting the rights of those infected by HIV has been central to AIDS prevention since 1988, exemplified by a number of prominent openly HIV-positive Ugandans and by public events such as candlelight memorials and World AIDS Day observances. In the late 1980s, Philly Lutaya, a celebrated European-based Ugandan musician who went public about his HIV status, returned home and devoted his last months of life to giving testimonies in schools, community organizations, churches and elsewhere. Of critical importance, The AIDS Support Organization (TASO) was organized in 1988 and has advocated against discrimination and stigma while pioneering a community-based approach for care of PLWHAs. The work of TASO and other care organizations have also made important contributions to prevention efforts, exemplifying the concept of a prevention-to-care continuum. Other national spokespersons included a Major in the Ugandan army who talked openly about his infection and how he used condoms to avoid infecting his wife and a Protestant bishop who disclosed that he learned of his infection when his first wife died and talked publicly about using condoms to avoid infecting his new wife or future children.
Openness on the part of the President, other government and community leaders and prominent activists has led, relatively speaking, to a remarkably accepting and non-discriminatory response to AIDS, in stark contrast to the situation in most other African countries (Halperin, 2006). This is important to recognize because some critics of the “Uganda model” have asserted that promotion of fundamental changes in sexual behavior will lead to more discrimination and AIDS associated stigma.
Africa's First Confidential Voluntary Counseling and Testing (VCT) Services
In 1991, the first AIDS Information Center (AIC) for anonymous VCT opened in Kampala. By the mid-1990s, AIC was increasingly active in several urban areas as people increasingly became interested in knowing their serostatus. AIC pioneered providing “same day results” using rapid HIV tests, as well as the concept of “Post-test Clubs” to provide long-term support for behavior change to anyone who had been tested, regardless of serostatus. Uganda was nearly unique in Africa in the emphasis it placed on VCT, at a time when the WHO/GPA and other international organizations were not yet recommending it as a prevention strategy.
Although a three-country randomized trial of the effect of VCT on STI incidence found no biological effect, some people, especially those testing HIV-positive, reported behavior change (Coates et al., 2000; Moses et al., 2000). However, two rigorous reviews/meta-analyses of dozens of developing country studies (Glick, 2005; Weinhardt et al., 1999), as well as a literature review (Wolitski et al., 1997) suggest that while VCT can motivate positive behavior change in some people, especially among those who test HIV positive, most clients do not report significant changes in sexual behavior as a result of undergoing VCT. A recent large, population-based study in Rakai, Uganda similarly found essentially no behavior change—nor HIV incidence decline—associated with VCT (Matovu et al., 2005). In any case, widespread accessibility of VCT services did not exist in most of Uganda until relatively more recently, certainly well after HIV incidence began declining during the late 1980s/early 1990s period. While there is no evidence that VCT led directly to the national reduction in HIV incidence, its increasing availability probably contributed to the overall environment of greater openness surrounding the disease (Marum, 2002), as well as generally to care and support, anti-stigma and prevention efforts in Uganda's successful response to AIDS.
Condom Promotion
Promotion of condom use was also not a central element in Uganda's earlier response to AIDS (1986–1991), certainly in comparison to many other countries in eastern and southern Africa (Epstein, 2004; Kaleeba et al., 2000; Stoneburner and Low-Beer, 2000, 2004; Hearst and Chen, 2004). In fact, until the early to mid 1990s, there was resistance on the part of President Museveni and some religious leaders to promoting condom use (Kaleeba et al., 2000). The first edition of a government handbook on AIDS prevention advised, “The government does not recommend using condoms as a way to fight AIDS.” (UNICEF/Uganda, 1988: 32) (This language was later softened to state that one “can still get AIDS even if a condom is used.”) A recent analysis concluded that this initial antipathy toward condoms might, ironically, have helped promote more fundamental changes in behavior: “In Uganda, the fact that condoms were not initially introduced and also the president's negative attitude towards them, played a part in the social acceptance of sexual behavioral change messages” (Allen and Heald, 2004, p. 1151).
Condom social marketing, under the SOMARC project, began in 1991, but condom sales did not reach substantial levels until the later 1990s; Population Services International (PSI) began its more successful condom sales program in 1997. However, beginning in the early to mid-1990s, millions of condoms have been distributed by the Ministry of Health through health centers and NGO projects, purchased mainly with external donor funding. In the DHS surveys, ever-use of condoms reported by women increased from 1% in 1989 to 6% in 1995 and 16% in 2000. Male ever-use of condoms was 16% in 1995 and 40% in 2000. Nearly all of the decline in HIV incidence (and much of the decline in prevalence) had already occurred by 1995 and, furthermore, epidemiological analysis including some modeling exercises suggest that very high levels of consistent condom use would be necessary to achieve significant reductions of prevalence in a generalized-level epidemic (Bernstein et al., 1998; Hearst and Chen, 2004; Robinson et al., 1995; Stover, 2002). According to the 1995 DHS, about 6% of sexually active Ugandans used a condom with some regularity (condom use, last intercourse with any partner). This proportion rose to 11% of sexually active Ugandans, or 8% of all Ugandan adults, by 2000 (Macro International, 1995, 2001). However, these low figures obscure the fact that condom use has now become quite high among those people who need them most, namely those still having multiple partners: in the 2000 DHS, 59% of men and 38% of women who reported having a non-regular partner said they had used a condom during last sex with such partners. (see the 2004 Uganda HIV/AIDS Sero-Behavioral Survey, DHS, 2005.) Condom use had reportedly risen to nearly 100% among commercial sex workers in Kampala by the late 1990s (Asiimwe-Okiror et al., 1998).
While condom sales and reported use have increased significantly during the past decade, it is noteworthy that condom use in high risk sex was not higher in Uganda than levels found in other countries in the region (Stoneburner and Low-Beer, 2000, 2004), including some that have considerably higher levels of HIV. And using a measure of condom use in the general population, namely condom use at last sex with any partner, among those sexually active, current levels in Uganda are actually lower than in several other countries in the region, including some with higher HIV prevalence rates (Measure DHS; Hearst and Chen, 2004). That said, the experience of Uganda also suggests the need for widespread availability of condoms to both “high risk” groups as well as the sexually active general population (Cohen, 2004; Halperin et al., 2004; Kirby, 2003; Shelton et al., 2004).
LOWER LEVELS OF MULTIPLE PARTNERSHIPS AND REDUCED SEXUAL NETWORKS IN UGANDA COMPARED TO MANY OTHER AFRICAN COUNTRIES
By the mid-1990s, in general Ugandans had considerably fewer non-regular sexual partners across all age groups. Population-level sexual behavior, including the proportion of people reporting more than one partner, were comparable in Kenya (1998), Zambia (1996) and Malawi (1996), for example, to levels reported in Uganda back in 1988–1989 (Stoneburner and Low-Beer, 2004). In comparison with men in these countries, Ugandan males in 1995 were less likely to have ever had sex (in the 15–19-year-old range), more likely to be married and to keep sex within the marriage and much less likely to have multiple partners, particularly if never married. Strikingly, the proportion of men reporting three or more non-regular partners in the previous year fell from 15 to 3% between the 1989 and 1995 GPA surveys. The latter figure was identical in both that GPA survey and the 1995 Uganda DHS (Bessinger et al., 2003). This apparently radical shift in behavior (even if the exact magnitude of change is uncertain due to sample size limitations, etc.) suggests a rather dramatic shift in behavioral trends within the important “core transmitter” population of men with multiple sexual partners (Bernstein et al., 1998; Epstein, 2004; Shelton et al., 2004; Auvert et al., 2000).
Such reported behavioral changes are consistent with the dominant AIDS prevention messages of Uganda's early response (i.e., 1986–1991), specifically: “stick to one partner,” and the ubiquitous “love faithfully” and “zero-grazing” admonitions readily understood even by the many illiterate residents of this largely rural nation. Such changes also seem related to the aforementioned more open personal communication networks for acquiring AIDS knowledge, which have been argued to more effectively personalize risk and thereby result in greater levels of behavior change (Allen and Heald 2004; Low-Beer et al., 2000). Comparing DHS survey data with that from other African countries, Ugandans are considerably more likely to receive AIDS information through friendships and other personal networks than through mass media or other sources and are significantly more likely to know of a friend or relative with AIDS (Stoneburner and Low-Beer, 2004).
CONCLUSION: A “SOCIAL VACCINE” FOR AFRICA?
Many of the elements of Uganda's response, such as high-level political support, decentralized planning and multi-sectoral organization, do not affect HIV infection rates directly. Rather, sexual behavior itself must change in order for seroincidence to change. The “ABC” factors are what can be termed proximate determinants of sexually transmitted HIV infection, i.e, means of avoiding or reducing the risk of infection. One lesson from Uganda seems to be: address the ABC factors through multiple interventions and do this through the means exemplified (and often pioneered) by Uganda: empowering women, mobilizing PLWAs and involving them in prevention, fighting stigma, involving faith-based organizations and the like. Another important element may have been the deliberate policy of fear arousal in order to combat denial, dramatize that AIDS is real and provoke Ugandans to feel at personal risk of HIV infection, unless they were willing to change behavior. The first director of TASO recounted, “Most of these initial campaigns adopted a ‘fear approach’ to HIV prevention, based on the theme: “Beware of AIDS. AIDS kills” (Kaleeba et al., 2000: 12). Members of the AIDS Control Programme involved in the early days of the ACP likewise recounted, “At first, we focused on instilling fear in the population…”, after which options for avoidance of risk were promoted, starting with “avoidance of sexual contacts” (Okware et al., 2001: 1114). In short, the strategy was to instill fear of the consequences of AIDS, engendering a perception of personal vulnerability to HIV infection, while at the same time clearly providing ways to avoid the feared outcome (Kirby, 2003; Green and Witte, 2006; Wilson, 2004) as well as working vigorously to reduce HIV-related stigma (Halperin, 2006).
According to modeling by Stoneburner and Low-Beer (2004), behavior change, particularly partner reduction, since the late 1980s in Uganda appears to have had a similar impact as a potential medical vaccine of 80% efficacy. The historical and socio-cultural context, the various interventions and other factors are complex and may have been somewhat unique to Uganda and it is not clear to what extent this success can be replicated elsewhere in Africa (not to mention in very different, more concentrated epidemics such as those in Asia or Latin America). However, it makes epidemiological sense to address all three ABC behaviors rather than to promote only one or two components of “ABC.” A great deal of resources have gone into primarily biomedical-based interventions (i.e., VCT, STI treatment, condoms) in South Africa, Botswana and other southern African countries, yet without apparent impact on national HIV infection rates (Allen and Heald, 2004; Epstein, 2004; Green, 2003; Hearst and Chen, 2004; Wilson, 2004).
In conclusion, the data from Uganda would suggest that pervasive, fundamental changes in sexual behavior can take place, perhaps contrary to previous expectations about the feasibility of such change. And epidemiological analysis, including modeling studies, suggests that significant reductions in numbers of partners would have significant impact on reducing HIV infection rates at the population level (Auvert and Ferry, 2002; Bernstein et al., 1998; Robinson et al., 1995; Auvert et al., 2000). As the Zimbabwean researcher David Wilson argued in the British Medical Journal, “Partner reduction is good epidemiology, not good ideology” (Wilson, 2004: 849). There will always be a need for condom promotion to individuals and groups, especially (though not only) to those at highest risk, and, indeed, Uganda more recently has also achieved relatively high levels of condom use with just such populations.
While we may never fully know “what really happened in Uganda,” the available evidence, bolstered by more recent and similarly encouraging findings from places such as Kenya (Kenya DHS, 2003; Green, 2003), Addis Ababa (Mekonnen et al., 2003; Shelton et al., 2004) Zambia (Agha, 2002; Bessinger et al., 2003; Fylkesnes et al., 2001; Shelton et al., 2004), and Zimbabwe (HAYES and Weiss, 2006), suggests that a comprehensive, behavior change-based strategy, ideally involving high-level political commitment and a diverse spectrum of community-based participation, may be the most effective prevention approach. A “consensus statement” published for the 2004 World AIDS Day in The Lancet (Halperin et al., 2004), which was endorsed by some 150 global AIDS professionals, including representatives of five UN agencies, WHO, World Bank, etc., as well as President Museveni of Uganda and various religious leaders including Archbishop Desmond Tutu, proposed that mutual faithfulness with an uninfected partner should be the primary behavioral approach promoted for sexually active adults in generalized epidemics. This appears to represent a fairly marked departure from many previous prevention approaches, which have tended to promote more biomedical strategies as the first line of defense for sexually active adults in all types of epidemics. A recent study of over 3,000 men who have sex with men in 6 US cities found, in multi-variate analysis using time-dependent covariates, that the primary independent risk factor for HIV seroconversion was greater numbers of sexual partners (Buchbinder et al., 2005). The authors suggested addressing this and other risk factors, including male circumcision, in prevention efforts.
Meanwhile, a paper presented in February 2005 at the 12th Conference on Retroviruses and Opportunistic Infections (Wawer et al., 2005) seemed to perhaps challenge the main tenets of both the Lancet consensus statement and the present paper. As mentioned earlier, the authors (one of whom, Ron Gray, signed the Lancet statement) concluded that mortality and condom use were mainly responsible for the HIV prevalence declines in the Rakai district between 1994 and 2003. Whatever the authors’ intent with this presentation, much of the world press was quick to jump to the conclusion that the “ABC model” of AIDS prevention had now been invalidated. Representative headlines that appeared within days of this conference presentation included: “Uganda's HIV success has more to do with condoms than abstinence” (The Advocate, CA—February 25, 2005); “Uganda: Condoms Outshine Abstinence in Aids Battle” (AllAfrica.com, Africa—February 24, 2005); “Uganda's Decline in HIV/AIDS Prevalence Attributed to Increased Condom Use” (Medical News Today, UK—February 26, 2005); “HIV study downplays abstinence in Uganda” (Newsday, NY—February 25, 2005). There was similar coverage as well as editorials in the New York Times, Washington Post and elsewhere. These reactions appear to mainly reflect the “culture wars” in the United States and Europe between partisans of abstinence vs. those of condoms, omitting the factor that was so crucial in Uganda's HIV decline: partner reduction and fidelity, or what in Uganda was widely termed “zero grazing” (Epstein, 2004, 2005b; Hearst and Chen, 2004; Shelton et al., 2004; Shelton, 2005; Wilson, 2004).
The authors of the Rakai study report that because after 1994 there were higher levels of condom use and lower levels of monogamy and abstinence, therefore condom use (and mortality rates) ought to account for the continuing HIV prevalence decline. However, analysis of the period 1994–2003 is too late to meaningfully explain the large decline in incidence in Uganda (see Epstein, 2005a; Mosley, 2005; Shelton, 2005) and in fact HIV prevalence in Rakai trading centers was considerably higher in 1990 (Wawer et al., 1997). In an earlier study in Rakai by some of the same authors as the new study, only 4.4% of the population reported consistent condom use while 16.5% reported inconsistent use during the prior year (Ahmed et al., 2001) and HIV incidence among inconsistent users was similar to that among non-users (with STI incidence being significantly higher among the inconsistent users). During the pre-1994 period when HIV incidence fell the most in Rakai, there were higher levels of “A” and (especially) “B” behaviors and relatively very little condom use. After 1994, people in Rakai appear to have moved increasingly toward condom use and away from partner fidelity and abstinence as primary HIV prevention strategies, according to the new Rakai study (Wawer et al., 2005).
Whatever the reason for this shift in prevention strategies, HIV seroincidence may have risen a little in Rakai in recent years, suggesting that Uganda's earlier strategy of emphasizing fidelity and partner reduction may have been the crucial type of behavioral change and intervention responsible for Uganda's historical HIV prevalence decline (Hearst and Chen, 2004; Shelton et al., 2004; Stoneburner and Low-Beer, 2004; Epstein, 2004; Cohen, 2004). It is unfortunate that even the British Medical Journal referred to Uganda's pre-1994 interventions as an “abstinence program” (Roehr, 2005). This only helps to perpetuate the confusion and allow Uganda's achievement to become lost in the polemics of abstinence-versus-condoms raging in the north American “culture wars.”
In fact, such polemics may continue and even increase in intensity if HIV prevalence rates were to increase in Uganda, since competing interpretations would be invoked to explain such a rise. The 2004 Ugandan HIV/AIDS Sero-Behavioral Survey (UHSBS), which included a population-based serologic survey along with standard behavioral questions similar to those contained in the DHS surveys, found an estimated 7% adult HIV prevalence rate (Measure DHS, 2005). This surprised some analysts, who had been expecting the population-based rate to be at or below 4–5%, if for no other reason than similar population-based serosurveys in Africa have generally yielded lower rates than estimates based upon sentinel surveillance data from antenatal clinics (Halperin and Post, 2004).
Although this curiously somewhat different result in Uganda may be due to unexplained methodological or other factors, the 7% prevalence finding may also suggest the possibility that HIV incidence has risen a little in recent years, consistent with some other data, such as (mostly relatively small) increases in prevalence among young antenatal clients at some ANC sites in recent years. In comparing behavioral data between the 2000 Uganda DHS and the 2004 UHSBS (Measure DHS, 2005: 13–15), the level of multiple sexual partnerships appears to have increased somewhat (consistent with the Rakai data; Wawer et al., 2005), while condom use has remained fairly steady (and age of sexual debut may have continued to increase a bit). Since declines in casual and multiple partner sex appear to have been particularly important in explaining Uganda's historic HIV prevalence decline, any rise in this measure would be troubling and calls for further quantitative and qualitative investigation.
AUTHOR'S CONTRIBUTIONS
Green has been investigating the Uganda behavioral data since 1993, and various main aspects of this paper result from his work; in addition, he drafted the original outline for the paper, composed several sections, and was considerably involved in the editing/revision process. Halperin originally conceptualized the paper, wrote most of the sections, and was responsible for most of the editing and revision. Nantulya, who contributed to the early development of the prevention strategy in his native Uganda, assisted in the initial conceptualization and with other aspects of the paper. Hogle composed the first draft by synthesizing the main research contributions of the other authors and of some other key researchers on this topic.
ACKNOWLEDGMENTS
The authors acknowledge Paul Delay, Helen Epstein, Doug Kirby, Jim Shelton, Jeff Spieler, David Stanton, Rand Stoneburner, John Stover and three anonymous reviewers for their helpful comments and input
References
- Agha, S. (2002). Declines in casual sex in Lusaka, Zambia: 1996–1999. AIDS, 16, 291–293. [DOI] [PubMed]
- Ahmed, S., Lutalo, T., Wawer, M., Serwadda, D., and Sewankambo, N. K. (2001). HIV incidence and sexually transmitted disease prevalence associated with condom use: a population study in Rakai, Uganda. AIDS, 15, 2171–2179. [DOI] [PubMed]
- Allen, T., and Heald. S. (2004). HIV/AIDS policy in Africa: what has worked in Uganda and what has failed in Botswana? Journal of International Development, 16, 1141–1154. [DOI]
- AMREF (2001). The Effects of the Katakwi/Soroti School Health and AIDS Prevention Project. African Medical and Research Foundation (AMREF) Report, Kampala.
- Ankrah, E. M., Asingwiire, N., and Wangalwa, S. S. (1990). Sexual Behaviors in Eastern Uganda. Paper Presented at 7th Annual AIDS Conference, Florence, Italy.
- Asiimwe-Okiror, J., Musinguzi, C., Agaba, A., Opio, E., and Madraa, E. (1998). Results of a KABP Survey on HIV, AIDS and STDS among Commercial Sex Workers (CSWs) in Kampala, Uganda. Kampala: STD/AIDS control programme, Ministry of Health.
- Auvert, B., and Ferry, B. (2002). Modeling the spread of HIV infection in four cities of sub-Saharan Africa. Oral presentation at the XIV International AIDS Conference, Barcelona, Spain, July 7–12.
- Auvert, B., Buonamico, G., Lagarde, E., and Williams, B. (2000). Sexual behavior, heterosexual transmission and the spread of HIV in sub-Saharan Africa: a simulation study. Computers and Biomedical Research, 33, 84–96. [DOI] [PubMed]
- Bernstein, R. S., Sokal, D. C., Seitz, S. T., Auvert, B., Naamara, W., and Stover, J. (1998). Simulating the control of a heterosexual HIV epidemic in a severely affected east African city. Interfaces, 28, 101–126.
- Bessinger, R., Akwara, P., and Halperin, D. (2003). Sexual behavior, HIV and fertility trends: A comparative analysis of six countries; Phase I of the ABC study. Measure Evaluation; USAID. (http://www.cpc.unc.edu/measure/publications/pdf/sr-03-21b.pdf).
- Buchbinder, S. P., Vittinghoff, E., Heagerty, P. J., Celum, C. L., Seage, G. R., Judson, F. N., McKirnan, D., Mayer, K. H., and Koblin, B. A. (2005). Sexual risk, nitrite inhalant use and lack of circumcision associated with HIV seroconversion in men who have sex with men in the United States. Journal of Acquired Immune Deficiency Syndromes, 39, 82–89. [DOI] [PubMed]
- Coates et al. The Voluntary HIV-1 Counselling and Testing Efficacy Study Group. (2000). Efficacy of voluntary HIV-1 counselling and testing in individuals and couples in Kenya, Tanzania and Trinidad: a randomised trial. Lancet, 356, 103–112. [DOI] [PubMed]
- Cohen, S. (2004). Promoting the ‘‘B’’ in ABC: its value and limitations in fostering reproductive health. The Guttmacher Report on Public Policy, 7: October 2004 http://www.guttmacher.org/pubs/tgr/07/4/index.html
- Epstein, H. (2004). The Fidelity Fix. New York Times Magazine. June 13.
- Epstein, H. (2005a). God and the Fight Against AIDS. NY Rev of Books, 52(7), 4/28/05.
- Epstein, H. (2005b). God and AIDS (letter response). NY Rev of Books, 52(9), 5/26/05.
- Fenton, L. (2004). Preventing HIV/AIDS through poverty reduction: the only sustainable solution? Lancet, 364, 1186–1187. [DOI] [PubMed]
- Fylkesnes, K., Musonda, R. M., Sichone, M., Ndhlovu, Z., Tembo, F., and Monze, M. (2001). Declining HIV prevalence and risk behaviors in Zambia: Evidence from surveillance and population-based surveys. AIDS, 15, 907–916. [DOI] [PubMed]
- Glick, P. (2005). Scaling up HIV voluntary counseling and testing in Africa: What can evaluation studies tell us about potential prevention impacts? Strategies and Analysis for Growth and Access (SAGA) Working Paper, Cornell University, March 2005. [DOI] [PubMed]
- Green, E. C. (1996). Indigenous Healers and the African State, New York: Pact Publications.
- Green, E. C. (2003). Rethinking AIDS Prevention. Westport, Ct.: Praeger.
- Green, E. C., and Witte, K. (2006). Fear arousal, sexual behavior change and AIDS prevention. Journal of Health Communication. May 2006, in press.
- Kagimu, M., Marum, E., Wabwire-Mangen, F., Nakyanjo, N., Walakira, Y., and Hogle, J. (1998). Evaluation of the effectiveness of AIDS health education interventions in the Muslim community in Uganda. AIDS Education and Prevention, 10, 215–228. [PubMed]
- Halperin, D. T., Steiner, M., Cassell, M., Green, E. C., Kirby, D., Hearst, N., Gayle, H., and Cates, W. (2004). The Time Has Come for Common Ground on Preventing Sexual Transmission of HIV. Lancet, 364, 1913–1915. (http:// www.iasociety.org/images/upload/Lancet%20HIV%20 prevention.pdf) [DOI] [PubMed]
- Halperin, D. T. (2006). Commentary on “Fear arousal, sexual behavior change and AIDS prevention,” by EC Green and K Witte. Journal of Health Communication. May 2006, in press.
- Halperin, D. T., and Epstein, H. (2004). Concurrent sexual partnerships help to explain Africa's high HIV prevalence: implications for prevention. Lancet, 364, 4–6. [DOI] [PubMed]
- Halperin, D. T., and Post, G. L. (2004). Global HIV prevalence: The good news might be even better. Lancet, 364, 1035–1036. [DOI] [PubMed]
- Halperin, D., and Allen, A. (2000). Is poverty the root cause of African AIDS? AIDS Analysis Africa, 11, 1–15, (http://sfgate.com/cgi-bin/article.cgi?file=/chronicle/archive/2000/11/30/ED113453.DTL)
- Hayes, R., and Weiss, R. (2006). Understanding HIV epidemic trends in Africa. Science 320, 620–21. [DOI] [PubMed]
- Hearst, N., and Chen, S. (2004). Condom promotion for AIDS prevention in the developing world: is it working? Family Planning Studies, 35, 39–47. [DOI] [PubMed]
- Kaleeba, N., Namulondo, J., Kalinki, D., and Williams, G. (2000). Open secret: People facing up to HIV and AIDS in Uganda (Strategies for Hope Series no. 15). London: ACTIONAID.
- Kirby, D. (2003). Presentation on USAID's ABC Study, USAID, Washington DC, October 23, 2003.
- Low-Beer, D. (2002). HIV-1 incidence and prevalence trends in Uganda [letter]. Lancet, 360, 1788. [DOI] [PubMed]
- Low-Beer, D., Stoneburner, R., Barnett, T., and Whiteside, M. (2000). Knowledge Diffusion and Personalizing Risk: Key Indicators of Behavior Change in Uganda Compared to South Africa [abstract]. XIII International AIDS Conference, July 9–14, 2000, Durban, South Africa.
- Macro International (1995). Uganda Demographic and Health Survey 1995.Calverton, MD: ORC Macro International.
- Macro International (2001). Uganda Demographic and Health Survey 2000–2001. Calverton, MD: ORC Macro International.
- Marum, E. (2002). USAID-Uganda's ABC experience. Paper presented at the “ABC” Technical Experts Meeting, USAID, Washington DC, September 17, 2002. (www.usaid.gov/pop_health/aids/TechAreas/prevention/index.html).
- Matovu, J. K. B., Gray, R. H., Makumbi, F., Wawer, M. J., Serwadda, D., and Kigozi, G. (2005). Voluntary HIV counseling and testing acceptance, sexual risk behavior and HIV incidence in Rakai, Uganda. AIDS, 19, 503–511. [DOI] [PubMed]
- Mbulaiteye, S. M., Mahe, C., Whitworth, J. A. G., Ruberantwari, A., Nakiyingi, J. S., Ojwiya, A., and Kamali, A. (2002). Declining HIV-1 incidence and associated prevalence over 10 years in a rural population in south-west Uganda: a cohort study. Lancet, 360, 41–44. [DOI] [PubMed]
- Measure DHS (2005). Uganda HIV/AIDS Sero-Behavioral Survey. 2004–2005 Preliminary Report. Ministry of Health, Kampala, Uganda and Measure DHS/ORC Macro, Calverton, Maryland.
- Mekonnen, Y., Sanders, E., Aklilu, M., Tsegaye, A., Rinke de Wit, T. F. Schaap, A., Wolday, D., Geskus, R., Coutinho, R. A., and Fontanet, A. L. (2003). Evidence of changes in sexual behaviors among male factory workers in Ethiopia. AIDS, 17, 223–231. [DOI] [PubMed]
- Moses, S., Plummer, F. A., and Nagelkerke, N. (2000). Reducing HIV-1 in Kenya and Tanzania. Lancet, 356, 1602. [DOI] [PubMed]
- Mosley, W. H. (2005). Declining HIV in Uganda cannot be explained by mortality or condoms. (Letter) BMJ March 8, 2005, http://bmj.bmjjournals.com/cgi/eletters/330/7490/496-a#99730.
- Murphy E. (2003). Defending the ABCs: A feminist perspective on AIDS prevention. Presentation, USAID, Washington DC, April 2003.
- Okware, S., Opio, A., Musinguzi, J., and Waibale, P. (2001). Fighting HIV/AIDS: Is success possible? Bulletin of the World Health Organization, 79, 1113–1120. [PMC free article] [PubMed]
- Parkhurst, J. (2002). The Ugandan success story?: Evidence and claims of HIV-1 prevention. Lancet, 360, 78–80. [DOI] [PubMed]
- Roehr, R. (2005). Abstinence programmes do not reduce HIV prevalence in Uganda. British Medical Journal, 330, 496-a. [DOI] [PMC free article] [PubMed]
- Robinson, N. J., Mulder, D. W., Auvert, B., and Hayes, R. J. (1995). Modeling the impact of alternative HIV intervention strategies in rural Uganda. AIDS, 9, 1263–1270. [DOI] [PubMed]
- Ruteikara, S., Nassanga-Miiro, H., Byamugisha, G., and James, T. M. (1995). Church Human Services AIDS Prevention Programme (CHUSA) Project. Follow-up Evaluation Report. Church Human Services, The Church of the Province of Uganda, World Learning, Inc.
- Sabatier, R. (1988). Blaming Others: Prejudice, Race and Worldwide AIDS. London: Panos Institute.
- Shelton, J. D., Halperin, D., Nantulya, V., Potts, P., Gayle, H., and Holmes, K. (2004). Partner reduction is crucial for balanced “ABC” approach to HIV prevention. British Medial Journal, 328, 891–893. (http://bmj.bmj journals.com/cgi/content/full/bmj;328/7444/891) [DOI] [PMC free article] [PubMed]
- Shelton, J. D. (2005). Partner reduction remains the predominant explanation. (Letter) BMJ March 9, 2005, http://bmj.bmjjournals.com/cgi/eletters/330/7490/496-a#99730
- Shelton, J.D., Cassell, M.M., and Adejunji, J. (2005). Is poverty or wealth at the root of HIV? Lancet 366, 1057–58. [DOI] [PubMed]
- Shelton, J. D., Halperin, D. T., and Wilson, D. (2006). Has global HIV incidence peaked? Lancet, 367, 9517. [DOI] [PubMed]
- Singh, S., Darroch, J. E., and Bankole, A. (2002). The Role of Behavior Change in the Decline in HIV Prevalence in Uganda. New York: Alan Guttmacher Institute.
- Singh, S., Darroch, J. E., and Bankole, A. (2003). A, B and C in Uganda: The Roles of Abstinence, Monogamy and Condom Use in HIV Decline. Occasional Report No. 9 December 2003. New York: Allan Guttmacher Inst. [DOI] [PubMed]
- Stoneburner, R. L., and Low-Beer, D. (2000). Is condom use or decrease in sexual partners behind HIV declines in Uganda Presentation, XIIIth International AIDS Conference, 9–14 July, Durban, South Africa.
- Stoneburner, R. L., and Low-Beer, D. (2004). Population-Level HIV Declines and Behavioral Risk Avoidance in Uganda. Science. 304, 714–18. [DOI] [PubMed]
- Stover, J. (2002). The effects of behavior change on trends in HIV incidence in Uganda and Kenya. Presentation, USAID, Washington DC, February 2, 2002.
- Turner, R. (1993). Young Ugandans know condoms prevent STDs, but disagree on whether use shows respect for partner. International Family Planning Perspectives.19(2), 76–77. [DOI]
- UNAIDS/Uganda. (2000). Uganda: Epidemiological fact sheet on HIV/AIDS and sexually transmitted diseases. Geneva: UNAIDS.
- UNAIDS/WHO (2004). Report on the global HIV/AIDS epidemic. http://www.unaids.org/bangkok2004/report.html (accessed Dec 1, 2004).
- UNICEF/Uganda. (1988). Control of AIDS: Action for Survival. Guidelines for Resistance Committees. Kampala: UNICEF and Uganda Ministry of Health.
- Wawer, M. J., Gray, R. H., Sewankambo, N. K., Li, C. J., Serwadda D., Konde-Lule, J. K. (1997). Trends in HIV prevalence may not reflect current HIV incidence in mature epidemics. AIDS, 11, 1023–30. [DOI] [PubMed]
- Wawer, M. J., Sewankambo, N., Serwadda, D., et al. (1999). Control of sexually transmitted diseases for AIDS prevention in Uganda: A randomised community trial. Lancet, 353, 25–35. [DOI] [PubMed]
- Wawer, M. J., Gray, R., and Serwadda, D. (February 2005). Declines in HIV prevalence in Uganda: Not as simple as ABC. 12th Conference on Retroviruses and Opportunistic Infections. Boston, 22–25, [Abstract #27LB; http://www.retroconference.org].
- Weinhardt, L. S., Carey, M. P., Johnson, B. T., and Bickham, N. L. (1999). Effects of HIV counseling and testing on sexual risk behavior: A meta-analytic review of published research, 1985–1997. American Journal Public Health, 89, 1397–1405. [DOI] [PMC free article] [PubMed]
- Wilson, D. (2004). Partner reduction and the prevention of HIV/AIDS: the most effective strategies come from communities. British Medical Journal, 328,848–849. http:// bmj.bmjjournals.com/cgi/content/full/328/7444/848 [DOI] [PMC free article] [PubMed]
- Wolitski, R., MacGowan, R., Higgins, D., and Jorgensen, C. (1997). The effects of HIV counseling and testing on risk-related practices and help-seeking behavior. AIDS Education and Prevention, 9(Suppl B), 52–67. [PubMed]