Abstract
Enterovirus characterization and typing require an integrated technological approach, using both immunological and molecular methods. The seventy-nine enteroviruses included in this study were isolated from cell cultures and classified as enteroviruses on the basis of an indirect immunofluorescence assay (IFA) against common enterovirus antigens and a neutralization test based on the Lim Benyesh-Melnick (LBM) pool. The final identification was carried out using a number of different molecular approaches, including reverse transcription (RT)-PCR, restriction fragment length polymorphism (RFLP) analysis, and nucleotide sequence analysis of amplicons from various regions of the genome. Twenty-seven poliovirus strains (set A) were identified using LBM pool analysis, RFLP analysis, and IFA. Use of the LBM pool method showed that 35 out of 79 strains were nonpoliovirus (set B), while 17 specimens tested negative (set C). Sets B and C were further investigated. Twenty-five specimens from set B and 8 from set C were identified by IFA. Six specimens from set B and five from set C were identified by RFLP analysis. Specimens in sets B and C were treated using RT-PCR; the resulting amplicons were subjected to nucleotide sequence analysis. The VP1 region was analyzed using two sets of deoxyinosine degenerate primers. Where the VP1 test gave no signal, the VP4-VP2 region was analyzed. Where both tests were negative, a 5′ noncoding region analysis was performed. Interestingly, analysis of the VP1 region showed that two specimens from set C were strains of enterovirus 71, whose presence was unexpected in Italy. As in other European epidemiological studies, the strain found most frequently was echovirus 30.
Human enteroviruses (EVs) comprise a large genus belonging to Picornaviridae. Sixty-six immunologically distinct serotypes are known to cause infection in humans. Most infections are mild or asymptomatic. In some cases, however, EVs may cause serious and even fatal disease; they are the major cause of acute febrile illness in infants and young children. EV infections can also affect numerous organ systems. EVs are the viral agents most commonly implicated in acute myocarditis and aseptic meningitis. Congenital infections also occur, although their frequency is unknown (12, 18).
The determination of the relationships between EVs and clinical syndromes and the investigation of their molecular epidemiology and phylogeny usually requires the typing of the viruses.
The traditional “gold standard” for the diagnosis of EV infections is virus isolation from clinical specimens in cell culture, followed by analysis with neutralizing antisera (7, 15, 16). Although the majority of cultures yield a positive result within the first week, EV typing by neutralization assay is time-consuming, expensive, and often futile (17, 18, 26).
It has been shown that viral infections can be reliably diagnosed by using monoclonal antibodies and indirect immunofluorescence assay (IFA) to identify EVs grown in cell culture. The simplicity and rapidity of this technique have led to suggestions that it could be helpful in clinical diagnosis (26). The static character of the method means, however, that it is unreliable in detecting new antigenic variants or emerging serotypes; it should also be noted that building a complete panel of monoclonal antibodies against specific viral strains is not easy and can be expensive.
More recent, molecular approaches (1, 5, 9, 10, 11, 21, 23, 24) have been developed and successfully used to detect most of the EVs, including nontypeable isolates and EVs which cannot readily be propagated in cell culture. In this study we compare immunological and molecular methods for the characterization and classification of human EVs isolated from clinical specimens over a 15-year period. While there is universal agreement that the results of VP1 classification are consistent with those of serum typing (3), there is general mistrust of analyses based on the VP2-VP4 region; the 5′ noncoding region (5′NC) is generally thought to be even less reliable (20). This is reasonable, given that different regions of the EV genome have different mutation rates. The implication is that, in comparisons between partial sequences of field isolates and prototype strains, the only way to achieve reliable results is by applying different evaluation criteria for each sequence. In the present work, we took this limitation into account, using VP1, VP4-VP2, and 5′NC typing methods together. This enabled us to successfully type all the specimens in our collection. The primers used have all been previously described with the exception of the upstream VP4-VP2 primer pairs. This suggests that, where an updated database of molecular sequences is available, the best way of investigating the nontypeable strains frequently found in clinical practice is to use molecular methods.
MATERIALS AND METHODS
Field isolates.
In this study we analyzed 79 viral strains isolated from 1,447 clinical specimens from patients who had received medical care at the A. Gemelli Hospital (Catholic University Medical School of Rome). The specimens, which had been collected and stored over the previous 15 years, included cerebrospinal fluid, stools, and throat swabs.
Cell cultures.
Viral isolation and in vitro propagation used the following cell lines: human diploid fibroblast (MRC5), green monkey kidney (Vero), rhesus monkey kidney (LLC-MK2), and human epidermoid carcinoma (HEp-2). Preliminary identification was based on the appearance of a characteristic cytopathic effect. Definitive identification and virus typing were accomplished by testing infected cell cultures as described below.
Neutralization assays with LBM pools.
Serotype identification was performed by neutralization using Lim Benyesh-Melnick (LBM) pools of type-specific antisera (Statens Seruminstitut, Copenhagen, Denmark); the neutralization results were used as the gold standard for the study. The EV was propagated in the same cell culture where it had grown, and virus titration was performed for each strain. A neutralization assay was then performed according to the standard procedure, as previously described (13).
IFA.
When cytopathic effect was observed, infected cells were scraped off the vessels, washed in phosphate-buffered saline (pH 7.4), spotted on slides, air dried in a laminar-flow hood. and fixed in cold acetone for 10 min. Fixed cells were immediately incubated for 30 min at 37°C, in a humid chamber, with a blend of mouse antibodies specific for EVs (Pan-Enterovirus blend; Light Diagnostics, Temecula, Calif.). After incubation, slides were washed three times in phosphate-buffered saline for 5 min each time. The slides were then incubated for 30 min at 37°C with a prestandardized dilution of anti-mouse immunoglobulin G fluorescein-conjugated antibody. Slides were then examined under a fluorescence microscope. All positive specimens were further tested with EV group blends (poliovirus blend, coxsackievirus blend, and echovirus blend; Light Diagnostics). When positive results were obtained with one of the group blend antibodies, type-specific monoclonal antibodies (poliovirus antibody set, coxsackievirus antibody set, and echovirus antibody set, Light Diagnostics) were used for definitive identification.
Viral RNA extraction.
Aliquots of EV-positive cultures were collected and stored at −80°C for RNA extraction. Specimens were frozen and thawed three times and clarified by centrifugation at 14,000 rpm for 10 min at 4°C (Eppendorf centrifuge 5417R). Viral nucleic acid was extracted from the supernatant by the acid guanidinium thiocyanate method (RNA isolation kit; Stratagene, La Jolla, Calif.), according to the manufacturer's instructions.
RT-PCR and RFLP analysis.
Viral RNA reverse transcription (RT) and cDNA amplification by nested PCR were performed using the Coxprim primer set (10). Amplification products were analyzed by enzymatic digestion using a panel of restriction endonucleases, selected on the basis of published viral nucleotide sequences, including the enzymes described by Kammerer et al. (10) (StyI, MluI, NcoI, BglI, BamHI, NheI, XmnI, EcoRI, RsaI, and Sau3AI; Roche, Molecular Biochemicals, Milan, Italy). Briefly, 10-μl aliquots of nested-PCR products were incubated at 37°C for at least 2 h, using 5 to 10 U of restriction enzyme in a volume of 25 μl, according to the manufacturer's instructions. RFLP was analyzed using 3% agarose gel (Metaphor agarose; FMC, BioProducts, Risingevej, Denmark) electrophoresis and ethidium bromide staining, Big-Dye Terminator labeling, and PCR cycle sequencing. RNA from isolates was genetically characterized by additional RT-PCR coupled with amplicon sequencing, following a previously published protocol (19). The coding region was classified using a PCR primer pair with deoxyinosine in positions where codons display degeneracy. Primers specifically devised for the VP1 of a large range of EVs were used in the order 012-011 and then 187-222 (22, 23). The 012-011 primer pair amplified the region from position 2875 to 3292 (COXB1 numbering), while the 187-222 pair amplified the region from position 2612 to 2951 region. Other pairs of PCR primers from the same authors, such as 188-222, 189-222, and 040-011, were also tested but without success. In the remaining nontypeable specimens, the VP2 region was amplified using a downstream primer containing mixed-base residues [A(A/G)(T/A/C) GC(A/T) TC(G/T) GG A AGC TT C CAC CAC CA] spanning the highly conserved NC region from position 1200 to 1221 (the numbering is deduced from the poliovirus 1 genome). A 5′NC primer sequence was used as an upstream primer (5). Big-Dye Terminator labeling (Perkin-Elmer, Applied Biosystems) was carried out as previously described (19). Briefly, 30 to 90 ng of purified DNA and 3.2 pmol of the sequencing primer were mixed in a reaction tube with the necessary amount of premixed Big-Dye reagents. After the reaction, sequencing was performed by capillary electrophoresis using ABI PRISM310 sequencing equipment (Perkin-Elmer, Applied Biosystems), and the sequences were realigned with PILEUP. The PHYLIP format of the multiple sequence format file was obtained using Genetic Device Environment software. Phylogenetic relationships in the VP1 region were inferred using PUZZLE software (27). Support for specific tree homologies was estimated using 100 puzzling steps; the branch lengths of neighbor-joining trees were calculated by applying Kishino and Hasegawa's maximum-likelihood method. Treetool software was used to reformat the Newick format nexus in the outtree (free software created by Mike MacIukenas [RDP Project, University of Illinois]). The phenogram was obtained using TreeView version 1.5 (25); the Windows metafile format file produced by TreeView was given as input to CorelDraw 8, which was used to produce the final version. Forward and reverse electropherograms were compared using Navigator software (Perkin-Elmer, Applied Biosystems); ambiguous bases and compressed peaks were checked manually.
Phylogenetic analysis.
Consensus sequences were exported in Genetics Computer Group (GCG) format and analyzed using SeqWeb 1.1 (GCG, University of Wisconsin, Madison), a Web-based GCG package. Nucleotide and amino acid sequence identities were calculated using the GCG NETBLAST utility. The prototypes and field isolates with the highest scores were aligned using PILEUP. The resulting multiple sequence format files were manually checked using LINEUP, and corresponding sequences from VP4-V and 5′NC were not shown for reasons of brevity. The prototype with the highest score identity was considered to be the strongest candidate identification.
RESULTS
Data from the LBM pool analysis of 79 specimens are summarized as follows. For convenience the results are classified into three groups: set A (the polio group [n = 27]), set B (the nonpolio group [n = 35]), and set C (nondetectable specimens [n = 17]).
Subtyping of set A is shown in Table 1. Results from IFA and RFLP analysis agreed with the results from the LBM pool method; as a result it was not necessary to use sequencing to confirm the poliovirus identification.
TABLE 1.
Subtyping of the 27 samples in set A
| Serotype | No. of samples with indicated serotype according to: |
||
|---|---|---|---|
| LBM pool method | IFA | RT-PCR and RFLP analysisa | |
| Polio 1 | 13 | 13 | 13 |
| Polio 2 | 12 | 12 | 12 |
| Polio 3 | 2 | 2 | 2 |
| Total | 27 | 27 | 27 |
With the Coxprim primer set.
Subtyping of set B is reported in Table 2. IFA with the Pan-Enterovirus blend gave broadly specific signals for all specimens examined. More-specific typing was obtained for 25 out of 35 specimens. Twenty-nine out of 35 specimens gave the expected amplicon in the RT-PCR assay that preceded the RFLP step. This technique, however, allowed the identification of only 6 specimens out of 29. The VP1 assay was able to identify 27 out of 35 specimens. The assay was carried out in two stages, using first the 187-222 primer pair and then, for specimens where the first test failed to give results, the 011-012 pair. The remaining specimens were analyzed using the VP4-VP2 region. Only two specimens were successfully typed. The remaining four specimens remained unidentifiable, even when tested with the 5′NC assay.
TABLE 2.
Results obtained for the 35 samples in set B
| No. of samples positive by assay/total no. of samples tested | ||||||
|---|---|---|---|---|---|---|
| IFA |
RT-PCR (Coxprim primer set) | RT-PCR and RFLP analysis | RT-PCR and sequencing |
|||
| Pan- Enterovirus blend | Group blend | VP1 | VP4-VP2 | 5′NC | ||
| 35/35 | 25/35 | 29/35 | 6/29 | 27/35 | 4/8 | 0/4 |
Table 3 reports the results of investigations on set C. Though IFA with the broadly specific Pan-Enterovirus blend gave positive signals for all specimens, more-specific identification using monoclonal antibody group blends was possible only for 8 out of 17 specimens.
TABLE 3.
Results obtained for the 17 samples in set C
| No. of samples positive by assay/total no. of samples tested | ||||||
|---|---|---|---|---|---|---|
| IFA |
RT-PCR (Coxprim primer set) | RT-PCR and RFLP analysis | RT-PCR and sequencing |
|||
| Pan- Enterovirus blend | Group blend | VP1 | VP4-VP2 | 5′NC | ||
| 17/17 | 8/17 | 10/17 | 5/10 | 9/17 | 3/8 | 5/5 |
The RT-PCR step produced 10 amplicons from 17 specimens, but only 5 of these gave identifiable RFLP patterns. VP1 typing, using RT-PCR and sequence analysis, identified only nine specimens. The VP4-VP2 test made it possible to identify three out of the remaining eight specimens. The remaining five specimens were identified using 5′NC analysis.
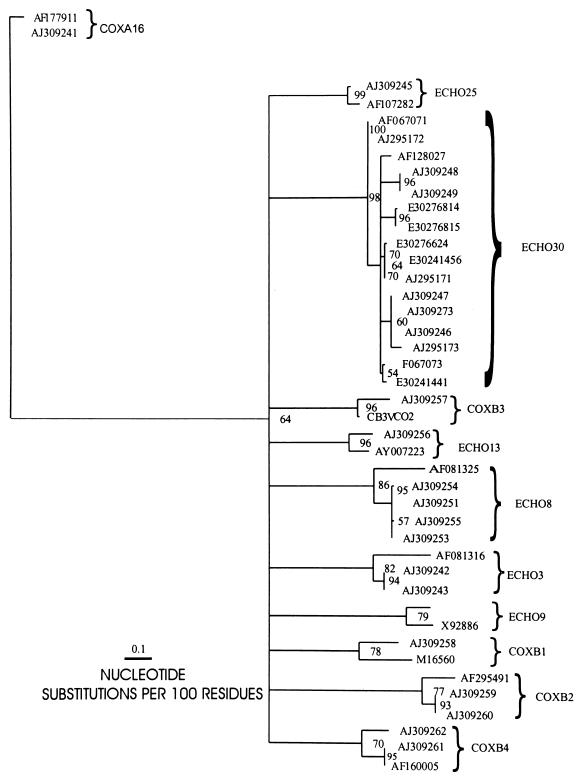
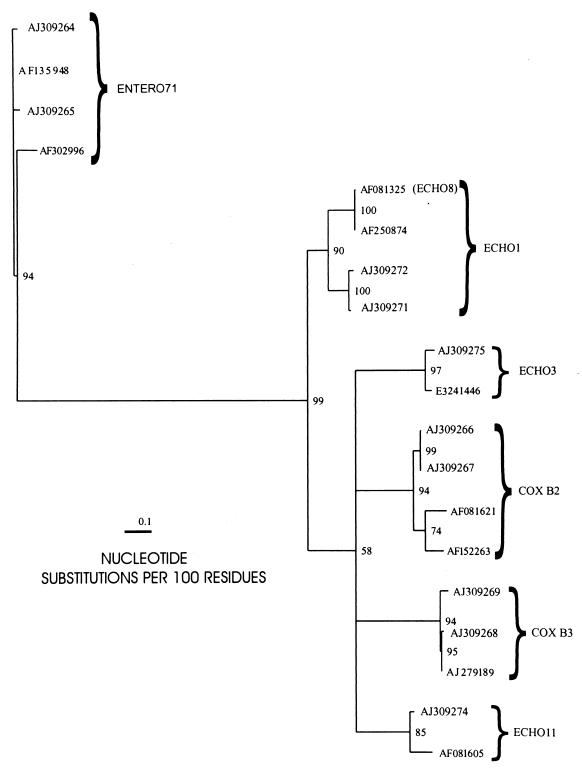
Phylogenetic analyses of sequences from VP1 tests with the 187-222 primer are reported in Fig. 1. Three redundant echovirus 30 strains are omitted. To optimize alignment, the lengths of the sequences shown in Fig. 1 have been reduced to 123 nucleotides (nt) the length of the shortest sequence (average length, 339 nt). This segment spanned the VP1 region from position 2650 to 2773 (numbering based on the coxsackievirus B3 genome). Coxsackievirus A16 was the most divergent strain and was used as an outgroup. A total of 12 clusters was obtained. All 22 specimens clustered together with their respective prototypes. The complete set of specimens detected with the 011-012 primer pair is reported in Fig. 2. The length of each sequence has been reduced to that of the shortest sequence available, 303 nt. This segment spanned the region from position 2928 to 3231. As shown in Fig. 2, sequences representing the same serotype always grouped in distinct clusters. A total of six clusters was obtained. All 10 wild strains clustered together with their respective prototypes. The clustering of echovirus 1 with strains 1 and 8 of the echovirus prototype, which are 100% identical in this region, is consistent with a prior observation that echovirus 1 and 8 are isolates of the same serotype and that echovirus 8 should thus be reclassified as a variant of echovirus 1 (8). EV 71 was the most divergent strain and was therefore used as an outgroup. The two wild strains isolated clustered together with prototype strains isolated in Taiwan and in the United States. These strains have high bootstrap support. Sequences from the VP4-VP2 region had different lengths and spanned different parts of the region. The results reported in Tables 4, 5, and 6 are thus based on a deduced amino acid comparison and are expressed in terms of the percentage of identity computed by NETBLAST. The scores obtained ranged from 91 to 100%. It is reasonable to consider these results with a high degree of confidence. Table 6 also reports the results from the 5′NC analysis. Given the large number of sequences available in the data bank, it was possible to obtain high confidence values for all the examined sequences.
FIG. 1.
PUZZLE phylogenetic tree for the VP1 region from position 2650 to 2773 (coxsackie B1 virus numbering). Amplicons for sequencing were obtained using primer set 187-222. Sequences were adjusted as described in Materials and Methods.
FIG. 2.
PUZZLE phylogenetic tree for the VP1 region from position 2970 to 3291 (coxsackie B1 virus numbering). Amplicons for sequencing were obtained using primer set 011-012. Sequences were adjusted as described in Materials and Methods.
TABLE 4.
Results of various analyses of EV typing
| Accession no. | No. of samples | Resulta according to: |
Highest identity score (%) |
Geographical location of prototype (yr) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| LBM pool method | IFA | PCR with Coxprim primer set | RFLP analysis | PCR VP1 (187-222) | Nucleo- tide | Amino acid | Prototype | |||
| AJ309241 | 1 | Echovirus 15 | Echovirus 4 | − | − | + | 100 | 100 | Coxsackievirus A16 (Af177911) | Taiwan (1998) |
| AJ309245 | 1 | Echovirus 25 | + | + | NS | + | 96 | 97 | Echovirus 25 (Af107282) | Germany (1998) |
| AJ309248 | 1 | Echovirus 30 | Echovirus 30 | + | NS | + | 99 | 99 | Echovirus 30 (Af067071) | Germany (1997) |
| AJ309249 | 1 | Echovirus 30 | Echovirus 30 | − | − | + | 92 | 98 | Echovirus 30 (Af128027) | United States (1983) |
| AJ295171 | 5 | Echovirus 30 | Echovirus 30 | + | NS | + | 99 | 100 | Echovirus 30 (e30241456) | France (1998) |
| AJ309247 | 2 | Echovirus 30 | Echovirus 30 | + | NS | + | 99 | 100 | Echovirus 30 (e30241456) | France (1998) |
| AJ309273 | 1 | Echovirus 30 | + | + | NS | + | 94 | 100 | Echovirus 30 (e30241456) | France (1998) |
| AJ309246 | 1 | Echovirus 30 | Echovirus 30 | + | NS | + | 97 | 100 | Echovirus 30 (e30241456) | France (1998) |
| AJ309257b | 1 | − | Coxsackievirus B3 | + | Coxsackie- virus B4 | + | 100 | 100 | Coxsackievirus B3 (CB3VC02) | United States |
| AJ309256 | 1 | Coxsackie- virus A9 | Coxsackievirus A9 | + | NS | + | 99 | 98 | Echovirus 13 (AY007223) | Germany (2000) |
| AJ309254b | 1 | − | Echovirus | − | − | + | 83 | 83 | Echovirus 8 (Af081325) | United States |
| AJ309251 | 1 | Echovirus 9 | + | + | NS | + | 82 | 84 | Echovirus 8 (Af081325) | United States |
| AJ309255 | 1 | Echovirus 3 | + | + | NS | + | 83 | 95 | Echovirus 8 (Af081325) | United States |
| AJ309253 | 2 | Coxsackie- virus B4 | Echovirus | + | NS | + | 82 | 97 | Echovirus 8 (Af081325) | United States |
| AJ309242b | 1 | − | + | + | NS | + | 94 | 99 | Echovirus 3 (Af081316) | United States |
| AJ309243 | 2 | Echovirus 9 | Echovirus 9 | + | Echovirus 9 | + | 94 | 100 | Echovirus 3 (Af081316) | United States |
| AJ309263 | 1 | Echovirus 13 | + | + | NS | + | 95 | 98 | Echovirus 9 (X92886) | Germany |
| AJ309259b | 1 | − | Coxsackievirus B2 | − | − | + | 86 | 97 | Coxsackievirus B2 (Af295491) | Sweden (1984) |
| AJ309260b | 1 | − | + | − | − | + | 86 | 99 | Coxsackievirus B2 (Af295491) | Sweden (1984) |
| AJ309262 | 1 | Coxsackie- virus B4 | Coxsackievirus B4 | + | NS | + | 96 | 99 | Coxsackievirus B4 (Af160005) | France (1996) |
| AJ309261 | 1 | − | Coxsackievirus B4 | − | − | + | 99 | 98 | Coxsackievirus B4 (Af160005) | France (1996) |
| AJ309258 | 1 | Echovirus 30 | Coxsackievirus B1 | + | − | + | 84 | 91 | Coxsackievirus B1 (M16560) | United States (1949) |
+, positive result; −, negative result; NS, not significant.
This strain was also tested by primer set 011-012 of the VP1 region (see Table 5).
TABLE 5.
Results of various analyses of EV typing
| Accession no. | No. of samples | Resulta according to: |
Highest identity score (%) |
Geographical location of prototype (yr) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| LBM pool method | IFA | PCR with Coxprim primer set | RFLP analysis | PCR VP1 (011-012) | Nucleo- tide | Amino acid | Prototype | |||
| AJ309264 | 1 | − | + | + | NS | + | 99 | 100 | EV 71 (AJ135948) | United States (1985) |
| AJ309265 | 1 | − | + | + | NS | + | 97 | 100 | EV 71 (Af302996) | China (1998) |
| AJ309272b | − | Echovirus | − | − | + | 84 | 95 | Echovirus 8 (Af081325) | United States | |
| AJ309271c | 1 | Echovirus 15 | Echovirus | + | − | + | 95 | 95 | Echovirus 1 (AF250874) | United States |
| AJ309275b | − | + | + | NS | + | 94 | Echovirus 3 (E3241446) | France (1994) | ||
| AJ309266b | − | Coxsackievirus B2 | − | − | + | 87 | 98 | Coxsackievirus B2 (Af081621) | United States (1995) | |
| AJ309267b | − | + | − | − | + | 87 | 98 | Coxsackievirus B2 (Af152263) | United States (1994) | |
| AJ309269b | − | Coxsackievirus B3 | + | Coxsackie- virus B4 | + | 100 | 100 | Coxsackievirus B3 (CB3VC02) | United States | |
| AJ309268 | 1 | − | Coxsackievirus B3 | + | Coxsackie- virus B2 | + | 97 | 100 | Coxsackievirus B3 (AJ279189) | Romania (1995) |
| AJ309274 | 1 | Echovirus 5 | Echovirus 11 | + | Echovirus 5 | + | 91 | 98 | Echovirus 11 (Af081605) | United States (1993) |
TABLE 6.
Results of various analyses of EV typing
| Accession no. | No. of samples | Resulta according to: |
Highest identity score (%) |
Geographical location of prototype (yr) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| LBM pool method | IFA | PCR with Coxprim primer set | RFLP analysis | PCR | Nucleo- tide | Amino acid | Prototype | |||
| AJ309244 | 1 | Echovirus 5 | Echovirus 11 | + | Echovirus 5 | VP1 | 91 | 98 | Echovirus 11 (AF081605) | United States (1993) |
| AJ309250 | 1 | Echovirus 30 | + | + | − | VP1 | 91 | 97 | Echovirus 30 (AJ276624) | France (1998) |
| AJ314828 | 1 | − | Echovirus | − | − | VP2 | 84 | 95 | Echovirus 23 (A055846) | United States (1986) |
| AJ314829 | 1 | − | Echovirus | − | Echovirus 5 | VP2 | 82 | 95 | Coxsackievirus B3 (AF231765) | Germany |
| AJ314830b | Echovirus 15 | Echovirus | + | − | VP2 | 85 | 100 | Echovirus 1 (AF250874) | United States | |
| AJ314831 | 1 | Coxsackievirus B1 | Coxsackievirus B1 | + | NS | VP2 | 82 | 98 | Coxsackievirus B1 (AF295193) | United States (1958) |
| AJ314832 | 1 | Coxsackievirus B5 | Coxsackievirus B5 | + | NS | VP2 | 90 | 98 | Coxsackievirus B5 (JQ2021) | United Kingdom (1985) |
| AJ314833 | 1 | Coxsackievirus A9 | Coxsackievirus A9 | + | NS | VP2 | 97 | 97 | Coxsackievirus A9 (AF27732) | Finland (1983) |
| AJ309252 | 1 | Coxsackievirus B2 | Coxsackievirus B2 | + | Coxsackie- virus B2 | VP2 | 81 | 91 | Coxsackievirus B2 (AF085363) | Ohio (1947) |
| AJ312091 | 1 | − | + | + | NS | 5′NC | 100 | Coxsackievirus B2 (AJ295199) | Ohio (1947) | |
| AJ312089 | 1 | − | + | − | − | 5′NC | 99 | Coxsackievirus B2 (AJ295199) | Ohio (1947) | |
| AJ312090 | 1 | − | + | − | − | 5′NC | 100 | Coxsackievirus B2 (AJ295199) | Ohio (1947) | |
| AJ312088 | 1 | − | + | − | − | 5′NC | 98 | EV 71 (AF304499) | Taiwan (1988) | |
| 2 | Echovirus 22 | + | − | − | − | |||||
| 2 | Echovirus 22 | + | − | − | − | |||||
+, positive result; −, negative result; NS, not significant.
This strain was also tested by primer set 011-012 of the VP1 region (see Table 5).
DISCUSSION
We have observed remarkable differences between optimal identification strategies for the poliovirus and the nonpoliovirus group. In poliovirus typing and subtyping, LBM pool analysis, IFA, and RT-PCR, followed by RFLP typing, provided accurate and consistent results. Only one specimen was nontypeable by the LBM pool method, probably because of the low concentration of infectious particles; this specimen was typed as poliovirus 2 by the other two methods.
In the nonpoliovirus group, nontypeable strains were encountered frequently. One of the specimens classed as nontypeable by LBM and IFA tests was shown by RFLP analysis and phylogenetic analysis to be rhinovirus 2. This supports the notion of specificity of these methods.
Several factors can affect the effectiveness and sensitivity of the viral isolation and neutralization test. These include the choice of cell lines and low initial viral titer. The lack of a complete panel of monoclonal antibodies means that the IFA can only be used for a limited range of serotypes. Its rapidity, sensitivity, and ease of application mean, however, that it can be useful in the clinical laboratory for rapid differentiation between polioviruses and nonpolio EVs.
Given that not all nonpolio EV sequences are available for comparison of restriction patterns, the results of RFLP analysis have to be considered as necessarily incomplete. In view of the tendency to make ever heavier use of molecular sequence data in virus classification, we believe that it would be useful to consider approaches using deoxyinosine degenerate primers. Considering their specificity and reliability, these techniques could well become the new gold standard for EV molecular typing. The results we obtained with these methods usually matched those of the VP1 test, especially in the presence of coxsackie B viruses. Some serotypes gave highly consistent results in all tests. One example is echovirus 30, for which 11 out of 12 specimens gave the same results on all tests. This suggests that the strain is almost stabilized and well adapted to replication in MRC-5 cell cultures.
In other cases where biological classification was available, this was rarely consistent with VP1 typing. Discordant results were especially common for serotypes belonging to the echovirus group. The results for echoviruses 22 and 23 show that, for these viruses, it is not possible to obtain amplification products using VP1 RT-PCR. This result confirms the results obtained by other authors (22) and is consistent with the reclassification of these viruses as a new Picornavirus genus (Paraechovirus) (6, 14). The failure to achieve amplification may be due to VP1 primers' reliance on conserved amino acid motifs specific to the EV genus.
Unexpectedly, the proposed VP4-VP2 analysis was able to detect a strain of echovirus 23 in viruses nontypeable by the LBM pool method. Even if molecular virologists have differing opinions concerning the validity of VP4-VP2 typing, our data show that in most cases the results are highly consistent with those obtained by other serological typing methods. It is worth pointing out that this test was applied only when VP1 typing had failed. We would thus argue that VP4-VP2 typing can complement the data obtained from VP1 typing, provided that amino acid sequence identity is not less than 90%. When we applied this practical criterion, VP4-VP2 typing proved to be extremely helpful.
For all remaining cases of nontypeable viruses, 5′NC analysis provided a reliable basis for phylogenetic investigations. A criterion of 98 to 99% nucleotide identity with published sequences produced reliable identifications.
The detection, in our Italian specimens, of strains such as EV 71, which cannot be typed with the LBM method, does not mean that these are new emergent viruses. It seems likely that this result was due to the absence of EV 71 antibodies in the standard LBM neutralization pool, which contains antibodies against only 42 of the 64 known human EV serotypes (EV 22 and EV 23 included).
In other cases the failure to detect viruses present in the standard pool may be due to low viral titer or to difficulties in in vitro propagation. These difficulties may be especially serious with liquor or myocardial specimens. In other cases, particularly with fecal specimens, mixes of different viruses may affect the success of the LBM pool test.
As sequence data become more widely available this will increase the efficiency and reliability of molecular techniques as a tool complementing serological techniques for EV identification. In this field, unfortunately, lack of confidence in available references reduces the reliability of phylogenetic classification. Many data bank submissions do not provide necessary information about the typing methods used. An uncertain classification by one author can thus be misrepresented as a reference by other authors, who are accustomed to using a phylogenetic approach for diagnostic purposes. In Italy, this situation is worsened by the fact that sequence data on common strains are often lacking or very limited. EV surveillance in Italy does not include EV typing, except where EV infectious diseases are suspected to be vaccine associated, in which case compliance with the World Health Organization schedule is mandatory. Where specific EV strains occur only sporadically, the importance of identifying them may be underestimated. An outbreak of echovirus 30 (AJ309273, AJ295171, and AJ295173), in October 1997 in Italy (associated with swimming pool use in Rome) and in other European countries led to increased interest in the identification of this specific strain. This experience helped us in identifying echovirus 30 (AJ309248 and AJ309249) in outbreaks of meningitis in 1998 and in 2000 (data not shown); these outbreaks—close to Rome—were again associated with swimming pool use. The identification of echovirus 30 is consistent with epidemiological data showing the widespread presence of the strain in France (accession no. e30241441) (4); in Germany in 1996 (28) and 1997 (e30/Frankfurt/M/97 strain; accession no. af067071); and in Romania, where it caused 5,000 nonfatal cases of disease between July and September 1999 (2).
The work reported in this paper suggests that the submission of sequences to public data banks should be encouraged. As sequence data become more widely available, this will facilitate the rapid molecular typing of clinical and environmental strains and the monitoring of potential sources for new recombinant EVs. In general terms the results of our work provide useful input for future studies of evolutionary relationships among EVs. More specifically, the methods described in this paper should be seen as a contribution to the development of references, guidelines, and computational techniques allowing an integrated, molecular, and immunological approach to the typing of microorganisms.
Acknowledgments
Thanks are due to Franca Pedone for excellent technical assistance and to Richard Walker for assistance with editing.
REFERENCES
- 1.Abzug, M. J., M. Loeffelholz, and H. A. Rotbart. 1995. Diagnosis of neonatal enterovirus infection by polymerase chain reaction. J. Pediatr. 126:447-450. [DOI] [PubMed] [Google Scholar]
- 2.Anonymous. 2000. Outbreak of aseptic meningitis associated with multiple enterovirus serotypes—Romania, 1999. Morb. Mortal. Wkly. Rep. 49:669-671. [PubMed] [Google Scholar]
- 3.Caro, V., S. Guillot, F. Delpeyroux, and R. Crainic. 2001. Molecular strategy for ′serotyping' of human enteroviruses. J. Gen. Virol. 82:79-91. [DOI] [PubMed] [Google Scholar]
- 4.Chambon, M., J. L. Bailly, A. Beguet, C. Henquell, C. Archimbaud, J. Gaulme, A. Labbe, G. Malpuech, and H. Peigue-Lafeuille. 1999. An outbreak due to echovirus type 30 in a neonatal unit in France in 1997: usefulness of PCR diagnosis. J. Hosp. Infect. 43:63-68. [DOI] [PubMed] [Google Scholar]
- 5.Chapman, N. M., S. Tracy, and C. J. Gauntt, and U. Fortmueller. 1990. Molecular detection and identification of enteroviruses using enzymatic amplification and nucleic acid hybridization. J. Clin. Microbiol. 28:843-850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coller, B. G., N. M. Chapman, M. A. Beck, M. A. Pallansch, C. G. Gauntt, and S. M. Tracy. 1990. Echovirus 22 is an atypical enterovirus. J. Virol. 64:2692-2701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grandien, M. M. Forsgren, and A. Ehrnst. 1995. Enterovirus, p. 279-297. In E. H. Lennette, D. A. Lennette, and E. T. Lennette (ed.), Diagnostic procedures for viral, rickettsial and chlamydial infections. American Public Health Association, Washington, D.C.
- 8.Harris, L. F., R. E. Haynes, H. G. Cramblett, R. M. Conant, and G. R. Jenkins. 1973. Antigenic analysis of echoviruses 1 and 8. J. Infect. Dis. 127:63-68. [DOI] [PubMed] [Google Scholar]
- 9.Johnston, S. L., G. Sanderson, P. K. Pattemore, S. Smith, P. G. Bardin, C. B. Bruce, P. R. Lambden, D. A. Tyrrell, and S. T. Holgate. 1993. Use of polymerase chain reaction for diagnosis of picornavirus infection in subjects with and without respiratory symptoms. J. Clin. Microbiol. 31:111-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kammerer, U., B. Kunkel, and K. Korn. 1994. Nested PCR for specific detection and rapid identification of human picornaviruses. J. Clin. Microbiol. 32:285-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kilpatrick, D. R., J. Quay, M. A. Pallansch, and M. S. Oberste. 2001. Type-specific detection of echovirus 30 isolates using degenerate reverse transcriptase PCR primers. J. Clin. Microbiol. 39:1299-1302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leland, D. S. 1992. Concepts of clinical diagnostic virology, p. 3-43. In E. H. Lennette (ed.). Laboratory diagnosis of viral infections, 2nd ed. Marcel Dekker, Inc., New York, N.Y.
- 13.Lim, K. A., and M. Benyesh-Melnick. 1960. Typing of viruses by combination of antiserum pools. Application to typing of enteroviruses (Coxsackie and Echo). J. Immunol. 84:309-317. [PubMed] [Google Scholar]
- 14.Mayo, M. A., and C. R. Pringle. 1998. Virus taxonomy—1997. J. Gen. Virol. 79:649-657. [DOI] [PubMed] [Google Scholar]
- 15.Melnick, J. L., V. Rennick, B. Hampil, N. J. Schmidt, and H. H. Ho. 1973. Lyophilized combination pools of enterovirus equine antisera: preparation and test procedures for identification of field strains of 42 enterovirus. Bull. W. H. O. 48:263-268. [PMC free article] [PubMed] [Google Scholar]
- 16.Melnick, J. L., and I. L. Wimberly. 1985. Lyophilized combination pools of enterovirus equine antisera: new LBM pools prepared from reserves of antisera stored frozen for two decades. Bull. W. H. O. 63:543-550. [PMC free article] [PubMed] [Google Scholar]
- 17.Morens, D. M., M. A. Pallansch, and M. Moore. 1991. Poliovirus and other enteroviruses, p. 427-497. In R. B. Belshe (ed.), Textbook of human virology. Mosby Year Book, St. Louis, Mo.
- 18.Muir, P., U. Kammerer, K. Korn, M. N. Mulders, T. Poyry, B. Weissbrich, R. Kandolf, G. M. Cleator, A. M. van Loon, et al. 1998. Molecular typing of enteroviruses: current status and future requirements. Clin. Microbiol. Rev. 11:202-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muscillo, M., G. La Rosa, A. Carducci, L. Cantiani, and C. Marianelli. 1999. Molecular and biological characterization of poliovirus 3 strains isolated in Adriatic seawater samples. Water Res. 33:3204-3212. [Google Scholar]
- 20.Oberste, M. S., K. Maher, and M. A. Pallansch. 1998. Molecular phylogeny of all human enterovirus serotypes based on comparison of sequences at the 5′ end of the region encoding VP2. Virus Res. 58:35-43. [DOI] [PubMed] [Google Scholar]
- 21.Oberste, M. S., K. Maher, D. R. Kilpatrick, M. R. Flemister, B. A. Brown, and M. A. Pallansch. 1999. Typing of human enteroviruses by partial sequencing of VP1. J. Clin. Microbiol. 37:1288-1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oberste, M. S., K. Maher, D. R. Kilpatrick, and M. A. Pallansch. 1999. Molecular evolution of the human enteroviruses: Correlation of serotype with VP1 sequence and application to picornavirus classification. J. Virol. 73:1941-1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oberste, M. S., K. Maher, M. R. Flemister, G. Marchetti, D. R. Kilpatrick, and M. A. Pallansch. 2000. Comparison of classic and molecular approaches for the identification of untypeable enteroviruses. J. Clin. Microbiol. 38:1170-1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oberste, M., D. Schnurr, K. Maher, S. al Busaidy, and M. Pallansch. 2001. Molecular identification of new picornaviruses and characterization of a proposed enterovirus 73 serotype. J. Gen. Virol. 82:409-416. [DOI] [PubMed] [Google Scholar]
- 25.Page, R. D. 1996. TreeView: an application to display phylogenetic trees on personal computers. Comput. Applic. Biosci. 23:357-358. [DOI] [PubMed] [Google Scholar]
- 26.Rigonan, A. S., L. Mann, and T. Chonmaitree. 1998. Use of monoclonal antibodies to identify serotypes of enterovirus isolates. J. Clin. Microbiol. 36:1877-1881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strimmer, K., and A. von Haeseler. 1996. Quartet puzzling: a quartet maximum-likelihood method for reconstructing tree topologies. Mol. Biol. Evol. 13:964-969. [Google Scholar]
- 28.Vieth, U. C., M. Kunzelmann, S. Diedrich, H. Timm, A. Ammon, O. Lyytikainen, and L. R. Petersen. 1999. An echovirus 30 outbreak with a high meningitis attack rate among children and household members at four day-care centers. Eur. J. Epidemiol. 15:655-658. [DOI] [PubMed] [Google Scholar]