Abstract
Eighty-two carbapenem-resistant isolates of Acinetobacter baumannii from a single hospital in Bilbao were typed into two major clusters and several subclusters. Disk synergy tests and PCR indicated the production of a zinc-independent OXA-class carbapenemase. Sequencing identified this enzyme, OXA-40, as a variant of the OXA-24-OXA-25-OXA-26 cluster.
Acinetobacter baumannii and its close relatives are important agents of nosocomial pneumonia in intensive care units (2, 20) and also cause a wide range of other nosocomial infections, especially in immunocompromised patients (2, 20). Many nosocomial acinetobacters are multiply resistant, meaning that such infections are difficult to treat, even with combination therapy. Moreover, acinetobacters often cause outbreaks and survive for long periods in the hospital environment, thereby posing a difficult challenge for infection control (20).
Carbapenems remain active against acinetobacter infections in many centers (2), but reports of carbapenem resistance have accumulated worldwide (1). Carbapenem-resistant strains of A. baumannii have been mostly sporadic in northern Europe but are endemic in some southern European countries, including parts of Spain (3, 7). Some reports have associated carbapenem resistance in Acinetobacter spp. with altered penicillin-binding or outer-membrane proteins (6, 12, 22), but Acinetobacter isolates producing carbapenem-hydrolyzing β-lactamases (carbapenemases) have been reported from at least 12 countries (1). Some of these carbapenemases are IMP- or VIM-class metallo-β-lactamases (5, 8, 18, 21, 25), but most acinetobacters produce zinc-independent members of molecular class D (1). Sequenced carbapenemases of this latter class from acinetobacters include OXA-23 (ARI-1) (9), OXA-24 (4), OXA-25, OXA-26, and OXA-27 (1).
Carbapenem resistance in Acinetobacter spp. has been endemic in Bilbao hospitals for several years (11). This study retrospectively investigated 82 isolates of Acinetobacter spp. isolated between June 1998 and April 1999 from 79 chronic bronchiectasis patients (three patients yielded two different isolates) attending the Hospital de Santa Marina, Bilbao, Spain. This is a 200-bed institution specializing in respiratory illness. The isolates were obtained from sputa (62 isolates), surgical wound swabs (4 isolates), skin ulcer swabs (4 isolates), urines (4 isolates), blood cultures (3 isolates), transtracheal aspirates (3 isolates), feces (1 isolate), and bronchoalveolar lavage specimens (1 isolate). Isolates were initially identified with the API 32 system (Biomerieux, Marcy l'Etoile, France) and stored at −80°C in nutrient broth containing 50% glycerol (vol/vol). As part of the present study, all isolates were reidentified as members of the A. baumannii complex (either A. baumannii or the closely related genomic species 13TU) by the technique of transfer DNA fingerprinting, in which PCR is used to amplify the species-specific spacer regions found between clusters of tRNA genes (10).
MICs for the isolates were determined by the National Committee for Clinical Laboratory Standards (NCCLS) broth microdilution method (16). Based on the NCCLS resistance breakpoint of ≥16 μg/ml for bacteria that grow aerobically, 49 (60%) and 45 (55%) of the 82 isolates were resistant to imipenem and meropenem, respectively. Isolates that were resistant to meropenem were also resistant to imipenem. Among the 49 imipenem-resistant isolates, resistance or intermediate resistance was also observed to ticarcillin (92%), piperacillin (100%), piperacillin plus tazobactam (61%), cefotaxime (94%), ceftazidime (90%), aztreonam (98%), gentamicin (90%), amikacin (69%), and ciprofloxacin (88%).
DNA was extracted from imipenem-resistant isolates and used with DAF-4, ERIC-2, and M13 core primers for the generation of randomly amplified polymorphic DNA (RAPD) fingerprints (11). RAPD fingerprints were also generated for 51 A. baumannii isolates associated with outbreaks of nosocomial infection in 18 different countries. Among these were carbapenem-resistant A. baumannii isolates from Madrid (strain RYC 52763/97) (3) and Barcelona (clones D and E; strains 228620 and 224220, respectively) (7). Fingerprint profiles were clustered with BioNumerics version 2.0 software (Applied Maths, Kortrijk, Belgium) by using the Dice coefficient and the UPGMA method. Isolates that clustered at a similarity coefficient (SAB) of >0.70 with a particular primer were considered to be related (13, 24).
Two major clusters (I and II) were identified among the Bilbao isolates with primer DAF4. Cluster I could be divided into three subclusters using M13 primer and ten subclusters using ERIC-2 primer (Table 1). Isolates from each of these subclusters showed carbapenemase activity in the modified Hodge test (14), but there was no evidence for metallo-β-lactamase activity in EDTA-disk synergy tests (14). By using DAF-4 (the least discriminatory primer), representative isolates of M13 clusters 1 (isolate SM10; imipenem MIC, >128 μg/ml), 2 (isolate SM76; imipenem MIC, >128 μg/ml), 3 (isolate SM28; imipenem MIC, >128 μg/ml), and 4 (isolate SM80; imipenem MIC, >128 μg/ml) were directly compared with the collection of 51 A. baumannii isolates from other countries and regions. SM28 (M13 cluster 3) was related at an SAB of 88% to two carbapenem-susceptible isolates from Barcelona, Spain, and Trieste, Italy, respectively. SM28 was unrelated to a Madrid isolate known to produce OXA-24 (3) but was closely related to one of two epidemic clones (clone D; strain 228620) responsible for a large and sustained outbreak of A. baumannii infection in Barcelona (7). Isolates SM10, SM76, and SM80 were unrelated (SAB < 70%) to all isolates from other locations.
TABLE 1.
RAPD typing relationships amongst 49 imipenem-resistant isolates of A. baumannii from Bilbao
| DAF-4 cluster | M13 cluster | ERIC-2 cluster [no. of isolates] | Total no. of isolates | Representative isolate |
|---|---|---|---|---|
| I | 1 | A [2] | 2 | SM10 |
| 2 | B [1], E [1], L [1], T [1], M [3] | 7 | SM76 | |
| 3 | N [1], P [7], C [2], R [4] | 14 | SM28 | |
| II | 4 | Q [26] | 26 | SM80 |
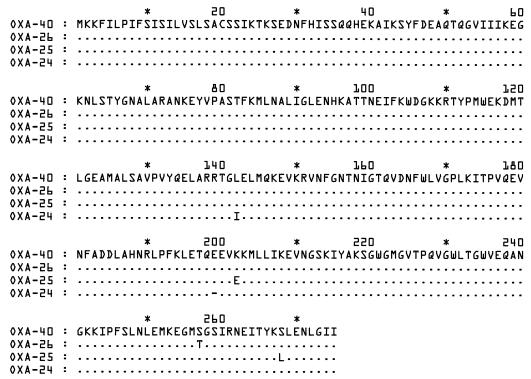
Isolates SM28 and SM80 (DAF-4 clusters I and II, respectively) were investigated by PCR for the presence of blaIMP (19), blaVIM (17), or OXA-type (1) carbapenemase genes. PCR with OXA-24 primers (1) amplified a ca. 1,030-bp fragment with both SM28 and SM80. No PCR evidence was obtained for the presence of blaIMP- or blaVIM-type genes. The ca. 1,030-bp fragment was sequenced on both strands by using a dye-labeled dideoxynucleoside triphosphate terminator cycle sequencing Quickstart kit (Beckman Coulter UK Ltd., High Wycombe, United Kingdom) and a CEQ 2000 automated sequencer (Beckman). Sequence data were analyzed with the GeneBuilder component of BioNumerics. The sequences obtained from SM28 and SM80 were identical and were 1,023 bp in size, including a reading frame of 825 bp. Figure 1 shows the relationship between the amino acid sequence coded by the gene from SM28 and SM80 and those of the OXA-24 (found in Madrid), OXA-25 (found in Murcia, Spain), and OXA-26 (found in Ghent, Belgium) enzymes, all of which share 98% similarity (1). The Bilbao enzyme had a closely related amino acid sequence, with two amino acids different from OXA-24 and OXA-25 and one amino acid different from OXA-26. The enzyme from Bilbao has been allocated the designation OXA-40 (K. Bush, personal communication).
FIG. 1.
Comparison of the amino acid sequence of OXA-40 from Bilbao (strains SM28 and SM80) with the sequences of OXA-24, OXA-25, and OXA-26. The sequences are identical except where differences are indicated.
The spread of specific acinetobacter clones has been demonstrated previously between hospitals in particular cities, such as Brooklyn, New York (15), or across whole countries, as seen with a single carbapenem-susceptible strain of A. baumannii that has been disseminated throughout Spain and the Canary Islands (23). Clonal outbreaks of infection caused by carbapenem-resistant strains of A. baumannii have been reported from Madrid (3) and Barcelona (7). The present study demonstrated that several different clusters of carbapenem-resistant A. baumannii isolates were endemic within a single hospital in Bilbao in 1998 and 1999 and produced a carbapenemase (designated OXA-40) that showed minor amino acid changes relative to OXA-24, OXA-25, and OXA-26.
The possible origins of class D carbapenemases have been considered previously and three hypotheses have been proposed, none of them mutually exclusive (1). One possibility is that an Acinetobacter strain (or strains) may have acquired a parental enzyme gene which has since diversified by mutation. In support of this hypothesis, it is notable that OXA-40 was closely related to the OXA-24 and OXA-25 enzymes reported from other parts of Spain but was more remote from the OXA-23-OXA-27 cluster, whose representatives have been found in the United Kingdom, Singapore, and Brazil (1). This suggests that minor diversification has occurred within the OXA-24-OXA-25-OXA-40 cluster in Spain rather than repeated de novo evolution.
While this study was being prepared, a preliminary report appeared describing the characterization of an OXA-type enzyme with a sequence identical to that of OXA-40 (L. Poirel, C. Héritier, and P. Nordmann, Abstr. 12th Eur. Congr. Clin. Microbiol. Infect. Dis., abstr. O384, 2002) found in a single recent isolate of A. baumannii from a patient transferred directly to France from a hospital in Portugal. While the precise relationship of this recent Portuguese isolate to the strains endemic in Bilbao in 1998 and 1999 has not yet been investigated, it appears that the OXA-40 gene has spread across the Iberian peninsula. The OXA-40 gene has been assigned GenBank accession number AF509241.
Acknowledgments
We are indebted to the staff of the Microbiology Department of the Hospital de Santa Marina, Bilbao, for their assistance with this project. We thank G. Bou and J. Vila for the gift of strains isolated in Madrid and Barcelona.
L.G. gratefully acknowledges the support of a project grant from the University of the Basque Country.
REFERENCES
- 1.Afzal-Shah, M., N. Woodford, and D. M. Livermore. 2001. Characterization of OXA-25, OXA-26, and OXA-27, molecular class D β-lactamases associated with carbapenem resistance in clinical isolates of Acinetobacter baumannii. Antimicrob. Agents Chemother. 45:583-588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bergogne-Bérézin, E., and K. J. Towner. 1996. Acinetobacter spp. as nosocomial pathogens: microbiological, clinical and epidemiological features. Clin. Microbiol. Rev. 9:148-165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bou, G., G. Cerveró, M. A. Domínguez, C. Quereda, and J. Martínez-Beltrán. 2000. Characterization of a nosocomial outbreak caused by a multiresistant Acinetobacter baumannii strain with a carbapenem-hydrolyzing enzyme: high-level carbapenem resistance in A. baumannii is not due solely to the presence of β-lactamases. J. Clin. Microbiol. 38:3299-3305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bou, G., A. Oliver, and J. Martínez-Beltrán. 2000. OXA-24, a novel class D β-lactamase with carbapenemase activity in an Acinetobacter baumannii clinical strain. Antimicrob. Agents Chemother. 44:1556-1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chu Y.-W., M. Afzal-Shah, E. T. S. Houang, M.-F. I. Palepou, D. J. Lyon, N. Woodford, and D. M. Livermore. 2001. IMP-4, a novel metallo-β-lactamase from nosocomial Acinetobacter spp. collected in Hong Kong between 1994 and 1998. Antimicrob. Agents Chemother. 45:710-714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clark, R. B. 1996. Imipenem resistance among Acinetobacter baumannii: association with reduced expression of a 33-36 kDa outer membrane protein. J. Antimicrob. Chemother. 38:245-251. [DOI] [PubMed] [Google Scholar]
- 7.Corbella, X., A. Montero, M. Pujol, M. A. Dominguez, J. Ayats, M. J. Agerich, F. Garrigosa, J. Ariza, and F. Gudiol. 2000. Emergence and rapid spread of carbapenem resistance during a large and sustained hospital outbreak of multiresistant Acinetobacter baumannii. J. Clin. Microbiol. 38:4086-4095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cornaglia, G., M. L. Riccio, A. Mazzariol, L. Lauretti, R. Fontana, and G. M. Rossolini. 1999. Appearance of IMP-1 metallo-β-lactamase in Europe. Lancet 353:899-900. [DOI] [PubMed] [Google Scholar]
- 9.Donald, H. M., W. Scaife, S. G. B. Amyes, and H. K. Young. 2000. Sequence analysis of ARI-1, a novel OXA β-lactamase, responsible for imipenem resistance in Acinetobacter baumannii 6B92. Antimicrob. Agents Chemother. 44:196-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ehrenstein, B., A. T. Bernards, L. Dijkshoorn, P. Gerner-Smidt, K. J. Towner, P. J. M. Bouvet, F. D. Daschner, and H. Grundmann. 1996. Acinetobacter species identification by using tRNA spacer fingerprinting. J. Clin. Microbiol. 34:2414-2420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gallego, L., and K. J. Towner. 2001. Carriage of class 1 integrons and antibiotic resistance in clinical isolates of Acinetobacter baumannii from Northern Spain. J. Med. Microbiol. 50:71-77. [DOI] [PubMed] [Google Scholar]
- 12.Gehrlein, M., H. Leying, W. Cullman, S. Wendt, and W. Opferkuch. 1991. Imipenem resistance in Acinetobacter baumannii is due to altered penicillin binding protein. Chemotherapy 37:405-412. [DOI] [PubMed] [Google Scholar]
- 13.Grundmann, H. J., K. J. Towner, L. Dijkshoorn, P. Gerner-Smidt, M. Maher, H. Seifert, and M. Vaneechoutte. 1997. Multicenter study using standardized protocols and reagents for evaluation of reproducibility of PCR-based fingerprinting of Acinetobacter spp. J. Clin. Microbiol. 35:3071-3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee, K., Y. Chong, H. B. Shin, Y. A. Kim, D. Yong, and J. H. Yum. 2001. Modified Hodge and EDTA-disk synergy tests to screen metallo-β-lactamase-producing strains of Pseudomonas and Acinetobacter species. Clin. Microbiol. Infect. 7:88-91. [DOI] [PubMed] [Google Scholar]
- 15.Manikal, V. M., D. Landman, G. Saurina, E. Oydna, H. Lal, and J. Quale. 2000. Endemic carbapenem-resistant Acinetobacter species in Brooklyn, New York: citywide prevalence, interinstitutional spread, and relation to antibiotic usage. Clin. Infect. Dis. 31:101-106. [DOI] [PubMed] [Google Scholar]
- 16.National Committee for Clinical Laboratory Standards. 1999. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard M7-A2. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- 17.Poirel, L., T. Naas, D. Nicholas, L. Collet, S. Bellais, J.-D. Cavallo, and P. Nordmann. 2000. Characterization of VIM-2, a carbapenem-hydrolyzing metallo-β-lactamase and its plasmid- and integron-borne gene from a Pseudomonas aeruginosa clinical isolate in France. Antimicrob. Agents Chemother. 44:891-897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Riccio, M. L., N. Franceschini, L. Boschi, B. Caravelli, G. Cornaglia, R. Fontana, G. Amicosante, and G. M. Rossolini. 2000. Characterization of the metallo-β-lactamase determinant of Acinetobacter baumannii AC-54/97 reveals the existence of blaIMP allelic variants carried by gene cassettes of different phylogeny. Antimicrob. Agents Chemother. 44:1229-1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Senda, K., Y. Arakawa, S. Ichiyama, K. Nakashima, H. Ito, S. Ohsuka, K. Shimokata, N. Kato, and M. Ohta. 1996. PCR detection of metallo-β-lactamase gene (blaIMP) in gram-negative rods resistant to broad-spectrum β-lactams. J. Clin. Microbiol. 34:2909-2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Towner, K. J. 2001. Acinetobacter in intensive care units. CPD Infect. 3:99-102. [Google Scholar]
- 21.Tysall, L., M. W. Stockdale, P. R. Chadwick, M.-F. I. Palepou, K. J. Towner, D. M. Livermore, and N. Woodford. 2002. IMP-1 carbapenemase detected in an Acinetobacter clinical isolate from the UK. J. Antimicrob. Chemother. 49:217-218. [DOI] [PubMed] [Google Scholar]
- 22.Urban, C., E. Go, K. S. Meyer, N. Mariano, and J. J. Rahal. 1995. Interactions of sulbactam, clavulanic acid and tazobactam with penicillin binding proteins of imipenem-resistant and susceptible Acinetobacter baumannii. FEMS Microbiol. Lett. 125:193-197. [Google Scholar]
- 23.Vila, J., J. Ruiz, M. Navia, B. Becerril, I. Garcia, S. Perea, I. Lopez-Hernandez, I. Alamo, F. Ballester, A. M. Planes, J. Martinez-Beltran, and T. Jimenez De Anta. 1999. Spread of amikacin resistance in Acinetobacter baumannii strains isolated in Spain due to an epidemic strain. J. Clin. Microbiol. 37:758-761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Webster, C. A., K. J. Towner, H. Humphreys, B. Ehrenstein, D. Hartung, and H. Grundmann. 1996. Comparison of rapid automated laser fluorescence analysis of DNA fingerprints with four other computer-assisted approaches for studying relationships between Acinetobacter baumannii isolates. J. Med. Microbiol. 44:185-194. [DOI] [PubMed] [Google Scholar]
- 25.Yum, J. H., K. Yi, H. Lee, D. Yong, K. Lee, J. M. Kim, G. M. Rossolini, and Y. Chong. 2002. Molecular characterization of metallo-β-lactamase-producing Acinetobacter baumannii and Acinetobacter genomospecies 3 from Korea: identification of two new integrons carrying the blaVIM-2 gene cassettes. J. Antimicrob. Chemother. 49:837-840. [DOI] [PubMed] [Google Scholar]