Abstract
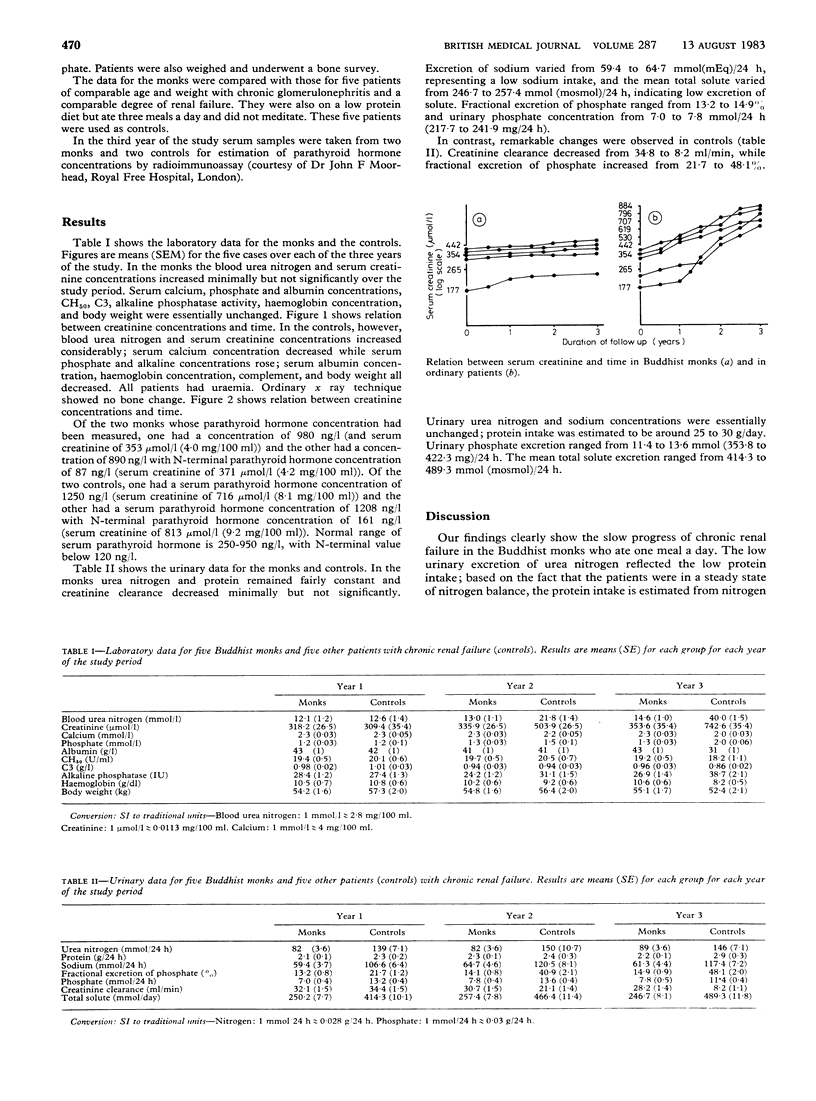
Clinical observations were made in five Buddhist monks with chronic renal failure on a low protein diet. These monks consumed only one meal and meditated three to four times a day. The estimated protein intake was from 15 to 19 g a day. Renal function remained stable over three years of observation. The general condition was satisfactory without any evidence of protein energy malnutrition. The data were compared with those of another group of patients who had a comparable degree of impairment of renal function but who consumed three meals a day of low protein diet. Protein intake was estimated to be from 25 to 30 g a day. These patients developed uraemia with severe renal failure and protein deficiency within three years. The findings support the role of protein restriction in maintenance of renal function in chronic renal failure and perhaps suggest a beneficial role for meditation.
Full text
PDF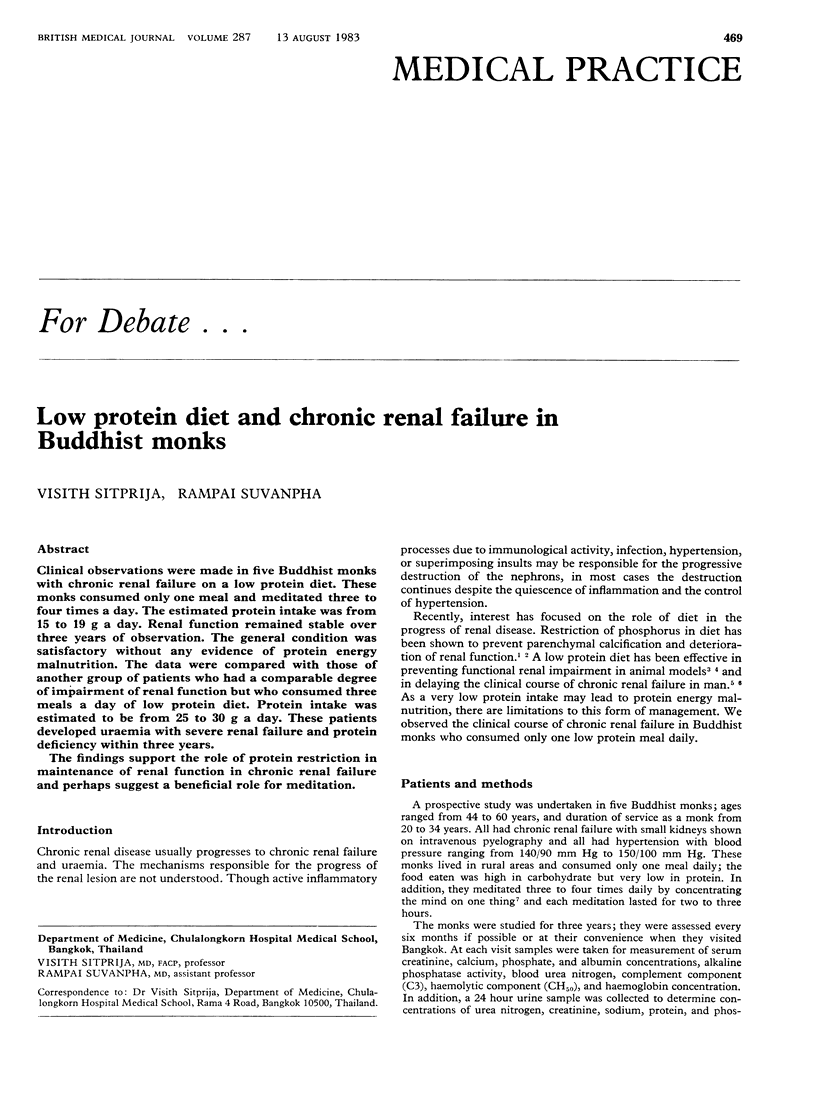

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brenner B. M., Meyer T. W., Hostetter T. H. Dietary protein intake and the progressive nature of kidney disease: the role of hemodynamically mediated glomerular injury in the pathogenesis of progressive glomerular sclerosis in aging, renal ablation, and intrinsic renal disease. N Engl J Med. 1982 Sep 9;307(11):652–659. doi: 10.1056/NEJM198209093071104. [DOI] [PubMed] [Google Scholar]
- Friend P. S., Fernandes G., Good R. A., Michael A. F., Yunis E. J. Dietary restrictions early and late: effects on the nephropathy of the NZB X NZW mouse. Lab Invest. 1978 Jun;38(6):629–632. [PubMed] [Google Scholar]
- Harvey K. B., Blumenkrantz M. J., Levine S. E., Blackburn G. L. Nutritional assessment and treatment of chronic renal failure. Am J Clin Nutr. 1980 Jul;33(7):1586–1597. doi: 10.1093/ajcn/33.7.1586. [DOI] [PubMed] [Google Scholar]
- Haut L. L., Alfrey A. C., Guggenheim S., Buddington B., Schrier N. Renal toxicity of phosphate in rats. Kidney Int. 1980 Jun;17(6):722–731. doi: 10.1038/ki.1980.85. [DOI] [PubMed] [Google Scholar]
- Ibels L. S., Alfrey A. C., Haut L., Huffer W. E. Preservation of function in experimental renal disease by dietary restriction of phosphate. N Engl J Med. 1978 Jan 19;298(3):122–126. doi: 10.1056/NEJM197801192980302. [DOI] [PubMed] [Google Scholar]
- Karambelkar P. V., Vinekar S. L., Bhole M. V. Studies on human subjects staying on an air-tight pit. Indian J Med Res. 1968 Aug;56(8):1282–1288. [PubMed] [Google Scholar]
- Lalich J. J., Faith G. C., Harding G. E. Protein overload nephropathy in rats subjected to unilateral nephrectomy. Arch Pathol. 1970 Jun;89(6):548–559. [PubMed] [Google Scholar]
- Maschio G., Oldrizzi L., Tessitore N., D'Angelo A., Valvo E., Lupo A., Loschiavo C., Fabris A., Gammaro L., Rugiu C. Effects of dietary protein and phosphorus restriction on the progression of early renal failure. Kidney Int. 1982 Oct;22(4):371–376. doi: 10.1038/ki.1982.184. [DOI] [PubMed] [Google Scholar]
- Walser M., Mitch W. E., Collier V. U. Calcium and phosphorus in chronic renal failure during nutritional therapy. Contrib Nephrol. 1980;20:92–102. doi: 10.1159/000384958. [DOI] [PubMed] [Google Scholar]


