Abstract
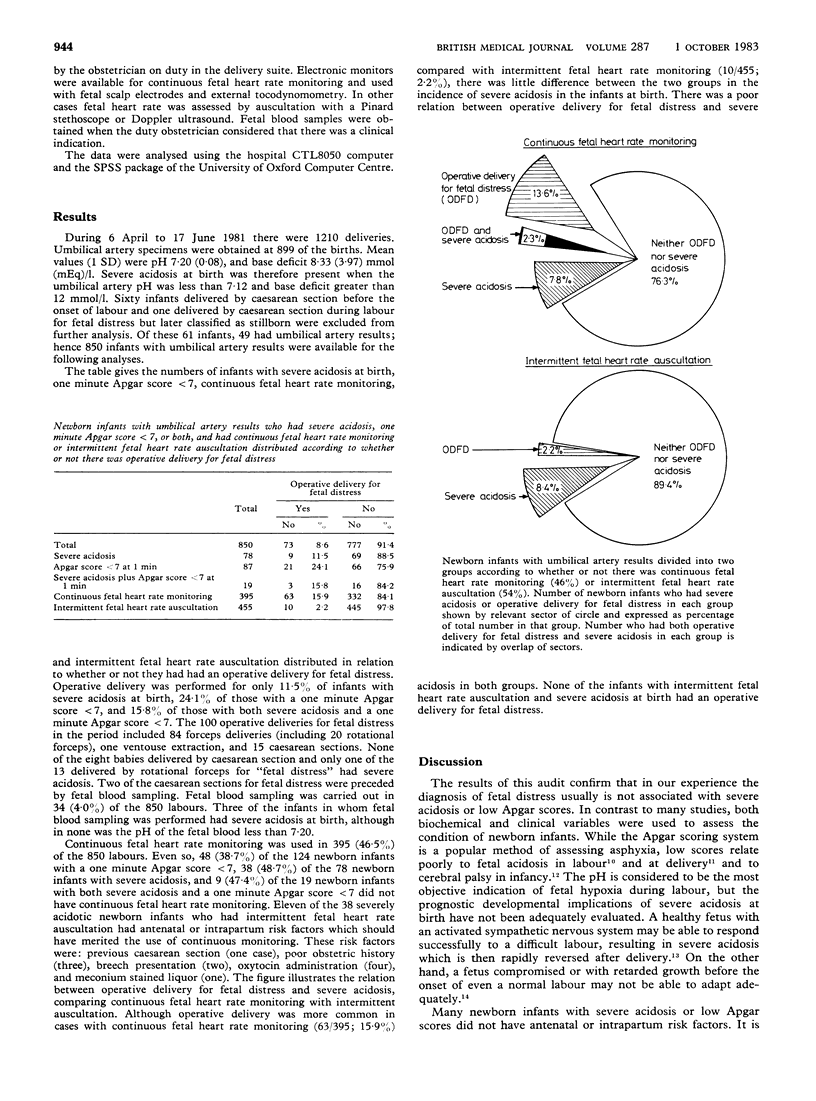
In a prospective audit of the obstetric management of 1210 consecutive deliveries the association was investigated between the need for operative delivery for fetal distress during labour and the condition of the newborn infant. Operative delivery was performed for only 11.5% of the newborn infants with severe acidosis at birth (umbilical artery pH less than 7.12, base deficit greater than 12 mmol (mEq)/1), 24.1% of those with an Apgar score less than 7 at one minute, and 15.8% of those with both severe acidosis and a one minute Apgar score less than 7. Most of the infants delivered operatively were in a vigorous condition at birth and did not have severe acidosis. Fetal blood sampling was done in 4.0% of labours. As none of the fetal blood values were less than 7.20 and only three of the infants sampled in utero suffered severe acidosis at birth, fetal blood sampling would have had to be performed much more often to provide a useful guide to metabolic state at birth. While the large majority of "at risk" fetuses had continuous fetal heart rate monitoring in labour, this had not been provided in 48.7% of the labours of infants with severe acidosis, 38.7% of infants with a one minute Apgar score less than 7, and 47.4% of infants with both severe acidosis and a one minute Apgar score less than 7. Continuous fetal heart rate monitoring was associated with a much higher incidence of operative delivery for fetal distress than was intermittent fetal heart rate auscultation. These results suggest an urgent need to review present methods for assessing the intrapartum condition of the fetus, making the diagnosis of fetal distress, and assessing the condition of the infant at birth.
Full text
PDF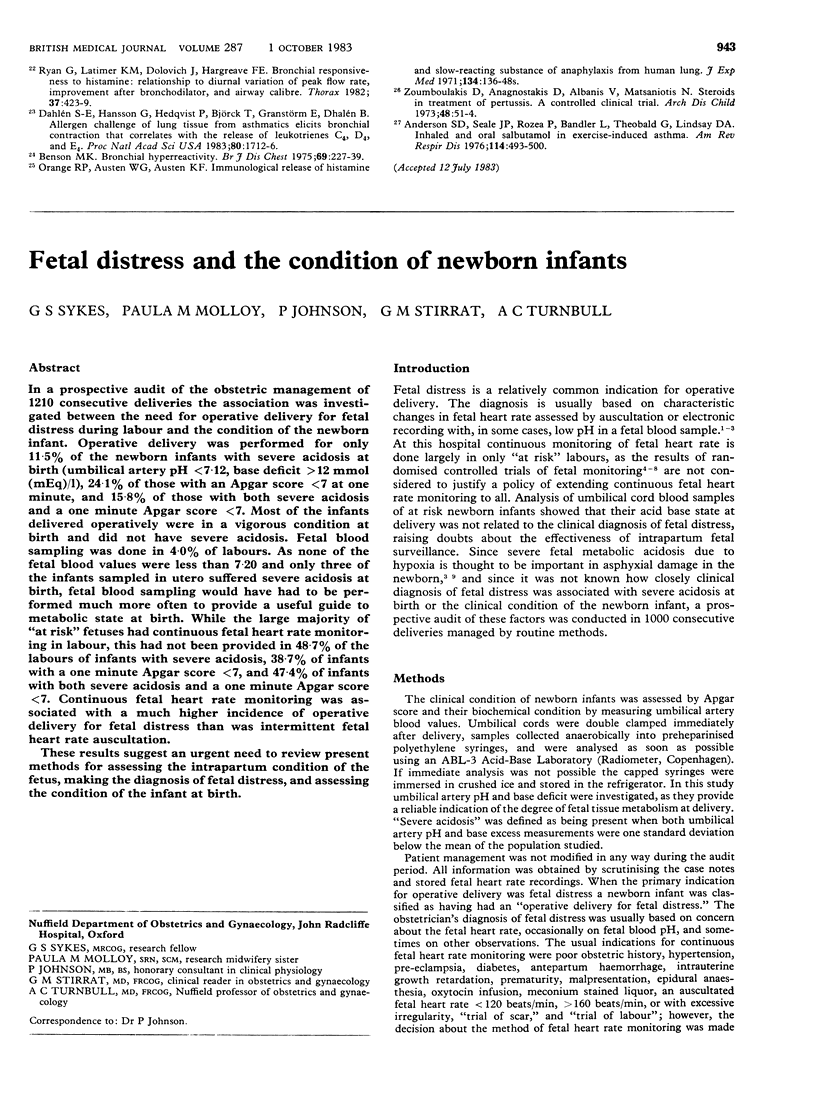

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beard R. W., Filshie G. M., Knight C. A., Roberts G. M. The significance of the changes in the continuous fetal heart rate in the first stage of labour. J Obstet Gynaecol Br Commonw. 1971 Oct;78(10):865–881. doi: 10.1111/j.1471-0528.1971.tb00198.x. [DOI] [PubMed] [Google Scholar]
- Gillmer M. D., Combe D. Intrapartum fetal monitoring practice in the United Kingdom. Br J Obstet Gynaecol. 1979 Oct;86(10):753–758. doi: 10.1111/j.1471-0528.1979.tb10689.x. [DOI] [PubMed] [Google Scholar]
- Haverkamp A. D., Orleans M., Langendoerfer S., McFee J., Murphy J., Thompson H. E. A controlled trial of the differential effects of intrapartum fetal monitoring. Am J Obstet Gynecol. 1979 Jun 15;134(4):399–412. doi: 10.1016/s0002-9378(16)33082-4. [DOI] [PubMed] [Google Scholar]
- Haverkamp A. D., Thompson H. E., McFee J. G., Cetrulo C. The evaluation of continuous fetal heart rate monitoring in high-risk pregnancy. Am J Obstet Gynecol. 1976 Jun 1;125(3):310–320. doi: 10.1016/0002-9378(76)90565-2. [DOI] [PubMed] [Google Scholar]
- Kelso I. M., Parsons R. J., Lawrence G. F., Arora S. S., Edmonds D. K., Cooke I. D. An assessment of continuous fetal heart rate monitoring in labor. A randomized trial. Am J Obstet Gynecol. 1978 Jul 1;131(5):526–532. doi: 10.1016/0002-9378(78)90114-x. [DOI] [PubMed] [Google Scholar]
- Kenny J. D., Garcia-Prats J. A., Hilliard J. L., Corbet A. J., Rudolph A. J. Hypercarbia at birth: a possible role in the pathogenesis of intraventricular hemorrhage. Pediatrics. 1978 Oct;62(4):465–467. [PubMed] [Google Scholar]
- Krebs H. B., Petres R. E., Dunn L. J., Jordaan H. V., Segreti A. Intrapartum fetal heart rate monitoring. III. Association of meconium with abnormal fetal heart rate patterns. Am J Obstet Gynecol. 1980 Aug 15;137(8):936–943. doi: 10.1016/s0002-9378(16)32835-6. [DOI] [PubMed] [Google Scholar]
- Low J. A., Cox M. J., Karchmar E. J., McGrath M. J., Pancham S. R., Piercy W. N. The prediction of intrapartum fetal metabolic acidosis by fetal heart rate monitoring. Am J Obstet Gynecol. 1981 Feb 1;139(3):299–305. doi: 10.1016/0002-9378(81)90014-4. [DOI] [PubMed] [Google Scholar]
- Nelson K. B., Ellenberg J. H. Apgar scores as predictors of chronic neurologic disability. Pediatrics. 1981 Jul;68(1):36–44. [PubMed] [Google Scholar]
- Renou P., Chang A., Anderson I., Wood C. Controlled trial of fetal intensive care. Am J Obstet Gynecol. 1976 Oct 15;126(4):470–476. doi: 10.1016/0002-9378(76)90641-4. [DOI] [PubMed] [Google Scholar]
- Saling E., Schneider D. Biochemical supervision of the foetus during labour. J Obstet Gynaecol Br Commonw. 1967 Dec;74(6):799–811. doi: 10.1111/j.1471-0528.1967.tb15561.x. [DOI] [PubMed] [Google Scholar]
- Savage M. O., Mirakian R., Harries J. T., Bottazzo G. F. Could protracted diarrhoea of infancy have an autoimmune pathogenesis? Lancet. 1982 Apr 24;1(8278):966–967. doi: 10.1016/s0140-6736(82)91965-1. [DOI] [PubMed] [Google Scholar]
- Sykes G. S., Molloy P. M., Johnson P., Gu W., Ashworth F., Stirrat G. M., Turnbull A. C. Do Apgar scores indicate asphyxia? Lancet. 1982 Feb 27;1(8270):494–496. doi: 10.1016/s0140-6736(82)91462-3. [DOI] [PubMed] [Google Scholar]
- Weber T. The validity of discontinuous pH-measurements on fetal blood and of cardiotocography in predicting neonatal Apgar score. Dan Med Bull. 1979 Jul;26(4):186–191. [PubMed] [Google Scholar]
- Wilson R. W., Schifrin B. S. Is any pregnancy low risk? Obstet Gynecol. 1980 May;55(5):653–656. [PubMed] [Google Scholar]
- Wood C., Renou P., Oats J., Farrell E., Beischer N., Anderson I. A controlled trial of fetal heart rate monitoring in a low-risk obstetric population. Am J Obstet Gynecol. 1981 Nov 1;141(5):527–534. doi: 10.1016/s0002-9378(15)33273-7. [DOI] [PubMed] [Google Scholar]
- Zalar R. W., Jr, Quilligan E. J. The influence of scalp sampling on the cesarean section rate for fetal distress. Am J Obstet Gynecol. 1979 Sep 15;135(2):239–246. doi: 10.1016/0002-9378(79)90352-1. [DOI] [PubMed] [Google Scholar]
- Zuspan F. P., Quilligan E. J., Iams J. D., van Geijn H. P. Predictors of intrapartum fetal distress: the role of electronic fetal monitoring. Report of the National Institute of Child Health and Human Development Consensus Development Task Force. Am J Obstet Gynecol. 1979 Oct 1;135(3):287–291. doi: 10.1016/0002-9378(79)90691-4. [DOI] [PubMed] [Google Scholar]


