The Case: A 7-year-old boy is brought to your office by his mother at the urging of his school. Although he reads extremely well and seems to understand material that is taught, he has great difficulty producing written work, initiating and finishing tasks and participating in gym class. He has trouble sitting still, often bumps into things and other people, and his behaviour is interfering with his academic progress. Socially he is isolated, especially on the school playground, where he avoids physical activity. After educational testing, the learning resource teacher concludes that there is no evidence of a learning disability. The patient appears to be a healthy, communicative boy who slouches noticeably in his chair. His mother is teary and anxious when describing his continuing difficulties.
What is your differential diagnosis? How would you assess this child?
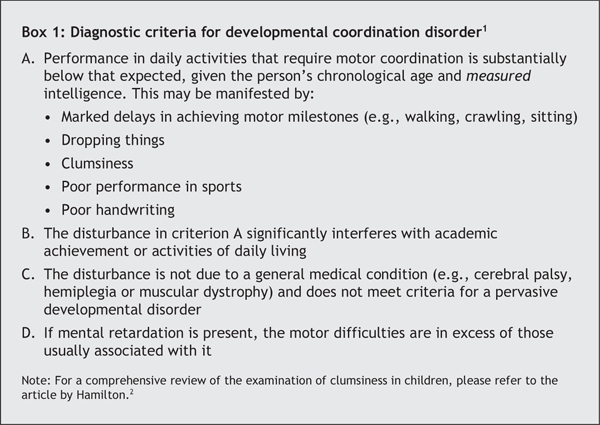
Motor coordination problems in otherwise healthy children of normal intelligence are common. Such children are often noted by parents, caregivers and teachers to have problems with daily tasks such as dressing themselves, to trip when they run, to spill things frequently and to have messy handwriting and drawing. They may be labelled as “clumsy,” “awkward” and “lazy.” Research has shown that children with these motor coordination problems often end up with serious academic and social impairments and problems with self-esteem. Developmental coordination disorder (DCD) is the term used when a child's delayed motor skill development affects his or her ability to perform age-appropriate daily activities (Box 1).
Box 1.
A total of 5%–6% of children meet the criteria for DCD.1 This means that, on average, at least 1 child in every primary school classroom is affected. Children with DCD are more likely than their peers to experience learning, emotional and behavioural problems (including learning disabilities, anxiety and attention-deficit hyperactivity disorder). Further, the deficits of DCD usually persist through adolescence and into adulthood. Early recognition of the condition by primary care providers may reduce its ultimate academic, emotional and behavioural impact.
Epidemiology and natural history
DCD is commonly diagnosed after age 5, when minor motor problems (often noted when the child was young) are highlighted by the structured demands of a school environment.2 The ratio of boys to girls varies from 2:1 to 5:1, depending on the group studied. The cause of DCD is poorly understood, since the results of genetic studies, imaging tests and other laboratory investigations are all inconclusive.
Children with DCD may appear to be inattentive because they have difficulty stabilizing their bodies and joints, so they look restless. They may also actively avoid tasks that require motor skills and become anxious in social situations. DCD and attention-deficit hyperactivity disorder frequently occur together, but the contribution of the motor difficulties to children's academic and social problems is often overlooked.
Although the pathophysiology is unknown, affected children appear to have underlying difficulties in motor planning (planning movements such as sitting down on a chair or figuring out how to jump), the timing and amount of force needed during movement (e.g., using too much or too little force to pick things up, being late reaching to catch a ball), and the integration of information from sensory and motor systems (e.g., relying heavily on visual information to climb stairs or fasten buttons).3 Children may also show poor balance, slow reaction and movement times, and difficulty executing fine motor skills needed for performing self-care activities, handwriting and drawing.2
The natural history of DCD is of concern, not because of the motor coordination problem itself but because of its impact on everyday activities and participation. Parents express concern about coordination difficulties when the child is young, but by early school age, these concerns are more evident as problems with self-care and academic activities. By the end of elementary school, social isolation, poor self-image and victimization are evident. Physical health concerns (childhood obesity and reduced physical fitness) and mental health problems (anxiety and depression) are commonly noted by early adolescence (Fig. 1).
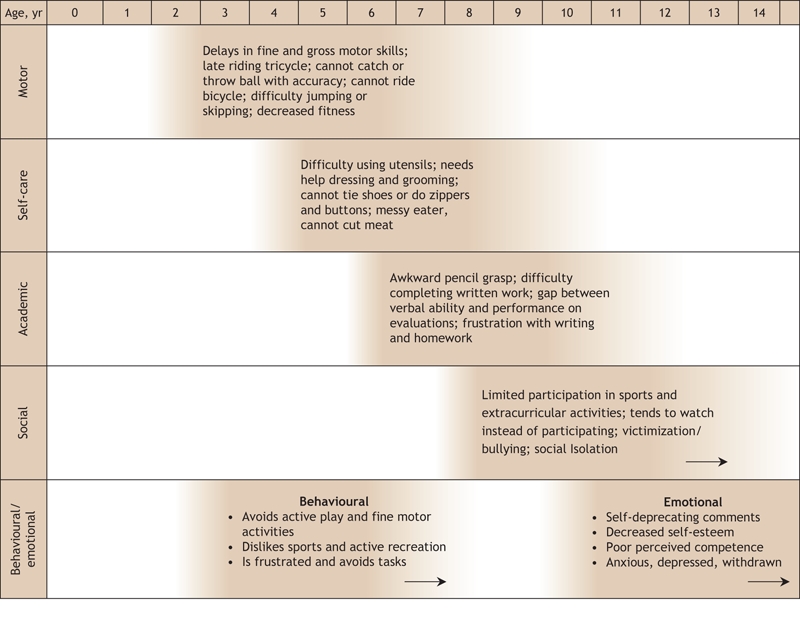
Fig. 1: Concerns typically noted by parents of children with developmental coordination disorder at different ages.
Screening
Annual health examinations are ideal times to screen for DCD. Parents can be asked to complete a self-administered questionnaire (see example in Appendix 1, available at www.cmaj.ca/cgi/content/full/175/5/471/DC1), or the physician can conduct a structured interview, listening for difficulties commonly associated with DCD. In addition, the physician can assess the child using simple screening activities administered in his or her office (see Appendix 2, available at www.cmaj.ca/cgi/content/full/175/5/471/DC1). Children with symptoms or signs of a motor coordination disorder require further evaluation.
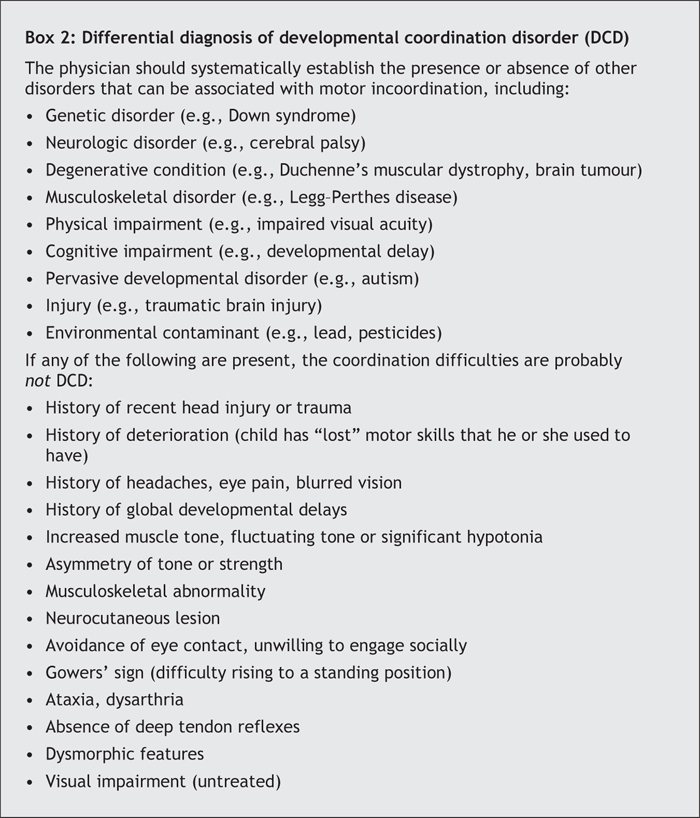
An assessment that takes into account the differential diagnosis of DCD (Box 2) is necessary, since DCD is a diagnosis of exclusion. Elements of the child's history, physical examination and laboratory test profile that would make alternate diagnoses more likely are indicated.
Box 2.
Referral and treatment
Early referral to an occupational therapist or pediatric multidisciplinary team can help confirm the diagnosis and rule out comorbid conditions such as speech or language difficulties, attentional problems, learning difficulties and mental health problems. This type of team can also help devise early management plans that may improve the child's developmental outcomes. Successful treatment approaches involve various allied health professionals, and the child's parents, physician and teachers.2,3
Armed with a diagnosis of DCD, parents are in a position to advocate for their child and to adapt their child's environment to encourage independence and self-esteem. Children with DCD lack confidence in situations where motor skills are required. Simple changes such as Velcro fasteners instead of buttons and laces can speed up dressing. Physical activities that naturally incorporate repetition and a constant environment, such as swimming, can be encouraged rather than team games. Teachers can reduce a child's stress and encourage academic progress by “matching” the child's abilities to the task. For example, reducing writing requirements, giving more time to complete tasks and encouraging different roles in physical education class can be helpful.4 Resources containing teaching tips and strategies for parents and educators can be found at the CanChild Centre for Childhood Disability Research (www.canchild.ca).
The case revisited
Physical examination reveals that the patient has normal hearing and vision, is slightly overweight and has low muscle tone (slouches and has unstable posture in sitting and standing positions). Administration of the screening activities shows that the boy's one-legged balance is poor. His pencil grasp is awkward, he uses excessive pressure, and his printing is slow. His sitting posture at the desk is “floppy” and he props his head upright by leaning on his other hand. The patient is unable to bounce and catch a tennis ball (see video clip, available at www.cmaj.ca/cgi/content/full/175/5/471/DC2).
In the parent questionnaire, the mother indicates that her son has great difficulty with many motor-based activities, is slow to learn new motor skills and becomes easily frustrated. Further questions about his disruptive behaviour in the classroom reveal that he misbehaves only when written work is required; he is not otherwise inattentive.
DCD is diagnosed. The physician provides the boy's parents with a variety of educational materials and suggests a referral to an occupational therapist and a review in 3 months.
Cheryl Missiuna Associate Professor School of Rehabilitation Science Co-Director, CanChild Centre for Childhood Disability Research McMaster University Hamilton, Ont. Robin Gaines Clinical Researcher Children's Hospital of Eastern Ontario Associate Member, CanChild Centre for Childhood Disability Research Adjunct Professor School of Rehabilitation Sciences University of Ottawa Helen Soucie Medical Writer Children's Hospital of Eastern Ontario Research Institute Ottawa, Ont.
Supplementary Material
Acknowledgments
Many of the materials presented in this report were developed for physician education as part of a Primary Health Care Transition Fund grant provided by the Ontario Ministry of Health and Long-term Care.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
REFERENCES
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington: The Association; 2000.
- 2.Hamilton SS. Evaluating clumsiness in children. Am Fam Physician 2002;66:1435-40. [PubMed]
- 3.Wilson PH. Practitioner review: approaches to assessment and treatment of children with DCD: an evaluative review. J Child Psychol Psychiatry 2005;46: 806-23. [DOI] [PubMed]
- 4.Missiuna C, Rivard L, Pollock N. They're bright but can't write: developmental coordination disorder in school aged children. Teach Exceptional Children Plus 2004;1(1):article 3. Available: http://escholarship.bc.edu/education/tecplus/vol1/iss1/art3/ (accessed 2006 July 13).
ADDITIONAL RESOURCES
- ·.CanChild Centre for Childhood Disability Research (www.canchild.ca): educational material for parents, teachers, service providers and members of the community available free
- ·.DCD PACK — Physician Allied Health Collaboration Kit (www.dcdpack.ca [enter “dcdpack” as username and “dcdchild” as password]): educational material for primary care physicians
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


