Abstract
Objectives. The National Hemophilia Foundation and the Centers for Disease Control and Prevention conducted a national survey focusing on knowledge about, attitudes toward, and behaviors associated with key prevention activities among youths with hemophilia and used the data gathered to design a health promotion campaign.
Methods. A national, random sample of 459 patients was drawn from 20 hemophilia treatment centers and 8 hemophilia associations; 110 (24%) of the respondents were young people. A telephone questionnaire was used to measure knowledge, behaviors, and barriers to prevention.
Results. Thirty-six percent of the youth respondents believed that joint disease cannot be prevented; 60% managed hemophilia by avoiding physical activity. Only 31% of the respondents treated bleeding episodes within 1 hour. Although hepatitis was a clear threat to this hemophilic cohort, 78% did now know transmission routes for hepatitis C, and 67% did not know transmission routes for hepatitis B.
Conclusions. Young people with chronic disorders need help understanding that they can prevent complications. We identified key messages for a hemophilia prevention campaign, including exercising to ensure healthy joints and treating bleeding episodes early and adequately.
Hemophilia is a hereditary bleeding disorder that occurs primarily among males. It is characterized by bleeding into muscles and joints and can cause chronic pain and joint disease. Although people at all hemophilia severity levels can bleed as a result of an injury, those with severe forms of the disease often experience spontaneous bleeding. In rare cases, bleeding into vital organs can cause death. In the United States,1,2 approximately 18 000 people have the disease (1 of every 7500 males), and about 55% of these individuals are young people.3
More than 70% of patients in the United States are seen in one of 134 federally funded hemophilia treatment centers (HTCs).4 In addition to conducting research, teams of specialists at these HTCs use a patient-centered approach to provide state-of-the-art medical, psychosocial, and educational services. In tandem with HTCs, local chapters of the National Hemophilia Foundation (NHF) and nonaffiliated associations provide education and support services to families with hemophilia. Access to an HTC can be limited owing to location, insurance restrictions, and provider preferences, but many individuals not seen in HTCs seek services from NHF chapters and associations.
Treatment for hemophilia involves replacing the essential clotting factor at the time of a bleeding episode. If bleeding episodes are treated early and adequately, severe joint disease can be prevented.5 The majority of such episodes occur within joints: 80% in the knees, elbows, and ankles.6 In 1994, NHF’s Medical and Scientific Advisory Council recommended prophylaxis (routine clotting factor treatment several times per week) as the optimal therapy for children with severe hemophilia.7 Prophylaxis can be used to stabilize or improve function in a joint that has bled in the past (secondary prophylaxis) or to prevent bleeding (primary prophylaxis).
According to the Universal Data Collection Program of the Centers for Disease Control and Prevention (CDC),8 44% of people with severe hemophilia A (clotting factor VIII deficiency, the more prevalent form of hemophilia) and 33% of people with hemophilia B (clotting factor IX deficiency) are treated with some form of prophylaxis. (The Universal Data Collection Program collects a uniform set of clinical data and plasma specimens from bleeding disorder patients during their annual comprehensive visits to federally funded HTCs. The plasma is tested for hepatitis A, B, and C and for HIV, and a portion is stored for future blood safety investigations.8) Breakthrough bleeding can occur even when a patient is being treated via prophylaxis. Currently, most individuals with hemophilia treat bleeding episodes when they occur. With the development of safer factor replacement products, the effectiveness of prophylactic regimens versus such “on-demand” therapy is an area of current CDC research. The first randomized clinical trial of young children with hemophilia A on prophylaxis showed improved joint function.9
Until the past decade, treatment of hemophilia involved intravenous infusion of a human blood-derived clotting factor that was effective in stopping most bleeding episodes but transmitted blood-borne infections, including HIV and hepatitis A, B, and C. The toll of viral infections on the hemophilia community has been amply documented in the literature10–12 and in the CDC’s Universal Data Collection Program. According to the CDC’s Hemophilia Surveillance System, in 1998, 7.5% of youths with hemophilia were infected with HIV, and 53% contracted hepatitis C from tainted blood products (CDC, unpublished data, 1998). Newer manufacturing processes such as recombinant technology, implemented in the early 1990s, have since increased the safety of hemophilia blood products.
Experience and research have demonstrated the need to continue to enhance information and education programs aimed toward young people with bleeding disorders. Studies, notably the work of Kyngäs,13 have shown that approximately 50% of youths with chronic conditions do not comply with care recommendations. For example, young people are the least likely of any age group to keep medical appointments.13 Youth is a life stage fraught with questions and concerns about identity, self-esteem, and relationships. In the case of young people with a chronic condition, managing that condition affects nearly every aspect of living: school, work, career aspirations, sports, travel, disclosure, and dating.
Good management of a chronic condition, short of a cure, means full knowledge of the complications associated with the condition and the preventive behaviors that can ameliorate or eradicate these complications. Along with advising parents to consult an HTC when needed, HTC staff provide parents with extensive training in home treatment so that they can manage hemophilia and its complications. However, the process of educating and training young people as they assume the role of managing their own care has not been as formalized.
The NHF and CDC conducted a survey, completed in March 2000, aimed at ascertaining knowledge about, attitudes toward, and behaviors associated with key prevention activities among people with hemophilia. Three target populations were identified for the survey: men with hemophilia, parents of children younger than 10 years with hemophilia, and young people (13 through 21 years of age) with hemophilia. The study’s prime objective was to assess existing prevention knowledge and health practices in the hemophilia community so that an effective national prevention program could be developed. Our focus here was on information obtained from youths with hemophilia.
METHODS
A team composed of experts working directly in hemophilia care and people with hemophilia developed a telephone survey including both structured and open-ended questions. A combination of hemophilia-specific questions and questions researched and adapted from national health surveys was used in the instrument. Examples of the latter were 2 questions adapted from the International Physical Activity Questionnaire,14 one concerning strenuous activity (exercises designed to strengthen or tone muscles, such as push-ups or sit-ups) and the other focusing on 30 minutes of moderate physical activity (such as walking, skating, or pushing a lawn mower). Respondents were asked how many days of the past 7 they had engaged in strenuous or moderate activities. The hemophilia-specific questions were developed through conducting focus groups with patients and parents of young children with hemophilia from different parts of the country.
Once developed, the survey instrument was pilot tested to ensure that questions were understood and the sequencing was effective (e.g., list responses were not provided prematurely); the instrument was then refined. The survey’s objectives were to assess (1) compliance with recommended prevention behaviors (Figure 1 ▶); (2) self-management of hemophilia; (3) knowledge, beliefs, and practices related to dealing with joint disease and infections; and (4) the perceived value of HTC services. As a means of protecting participants’ identities and ensuring confidentiality of responses, the telephone survey was conducted by an independent professional survey firm (Macro/ORC International, New York, NY). An average of 45 minutes was required to complete each survey.
FIGURE 1—
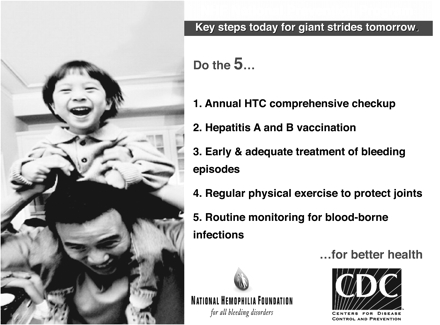
Five key prevention messages.
The sampling design was stratified (according to age and number of patients registered at the HTC) and systematic (a convenience sample of HTC and chapter patient/member lists was drawn for inclusion). Eighty percent of the sample was drawn from HTCs and 20% from NHF chapters and associations. Because the chapters and associations served both HTC and non-HTC patients, we assumed that there was a 60% to 70% patient list overlap (the survey firm checked across lists for duplicates). In addition, the HTC sample was purposefully drawn to ensure inclusion of a high percentage of Black/African American, Hispanic, and other minority patients. As a result, a total of 20 HTCs were used, 10 of which were classified as large (150 or more patients) and 10 of which were classified as small (fewer than 150 patients). In addition, 8 NHF chapters and associations were randomly selected from those identified.
The selected organizations and HTCs created alphabetic patient or member lists for all people who fit the demographic categories delineated for the study. All eligible individuals were invited to participate in the survey by HTC, chapter, or association staff. Those who provided informed consent to take part were called at a prearranged time at their home and were administered the survey.
We weighted each participant’s responses to appropriately reflect the number of people sampled in the HTC or chapter/association, the primary sampling unit. We used a validated method to accommodate the lower than expected response rate in relation to the reported sizes of some of the HTC and chapter/ association lists. This strategy corrected for nonresponse within primary sampling units (i.e., HTCs and chapters/associations). SAS software (SAS Institute Inc, Cary, NC) was used in conducting all data analyses.
Once the data were analyzed, messages based on the findings were developed, including the importance of treating bleeding episodes early and adequately and the fact that hepatitis A and B are preventable through vaccination. Focus groups were used to test and refine these messages for use in the national hemophilia prevention campaign. Three focus groups were conducted in July 2000 in Columbus, Ohio, at an annual meeting of a cluster of midwestern NHF chapters hosting more than 600 people. Telephone focus groups and individual interviews were also conducted to gain a larger, national perspective on messages and potential materials that would be effective in reaching the target population (e.g., brochures or online newsletters).
RESULTS
The 110 youth survey respondents ranged in age from 13 through 21 years; 23% were 13 through 15 years of age, 49% were 16 through 18 years of age, and 28% were 19 years or older. The average age was 16.7 years. All of the youth respondents were male, and 32% were of Spanish or Hispanic origin. Among those not of Hispanic origin, 49% were White, 3% were African American, 5.5% were Asian, 0.5% were Native American, 5% were Pacific Islanders, and 5% were categorized as “other.”
Complications of Primary Concern
Participants were asked “What are the bleeding disorder complications you are most concerned about?” Joint disease (41%) and bleeding episodes (23%) were the primary concerns of most of the young people surveyed; only 10% reported hepatitis as a primary concern (Table 1 ▶). This concern with joint damage was corroborated in a related question that asked respondents to rate, on a scale of 1 to 10 (1 = not at all preventable, 10 = extremely preventable), the degree to which each complication is preventable. More than a third (36%) of the youth respondents believed that joint disease is not preventable; only 16% rated it as extremely preventable.
TABLE 1—
Hemophilia Complications of Primary Concern: Youths 13–21 Years of Age, United States, 2000
| Sample, % | |
| Joint damage | 41 |
| Bleeding episodes | 23 |
| HIV | 12 |
| Hepatitis | 10 |
| Agent or virusa | 1 |
| Head injuries | < 1 |
aAn as of yet unidentified agent or virus infiltrating the blood supply.
By contrast, 62% and 42% of young people, respectively, believed that HIV and hepatitis are extremely preventable. Relatively small percentages of young people believed that HIV and hepatitis are not preventable (16% in each case). A negligible percentage of the respondents (1%) expressed concern about some as yet unidentified agent or virus infiltrating the blood supply or factor treatment products.
Knowledge of Transmission of Blood-Borne Infections
The survey respondents were asked a series of questions designed to ascertain the extent of their knowledge of the various types of hepatitis. They were initially asked whether they had “ever received information about hepatitis.” Seventy-one percent reported that they had received such information. They were then asked to rate their general knowledge of hepatitis on a scale of 1 to 10, with 10 being a very high level of knowledge. Thirty-two percent rated their knowledge of hepatitis as high (rating of 8 or above); 46% rated their knowledge as moderate (ratings of 4–7); and 22% rated their knowledge as low (rating of 3 or below). In addition, respondents were asked specific questions about how hepatitis B and C are transmitted. Sixty-seven percent of the youths stated they did not know the transmission routes for hepatitis B, and 78% reported that they did not know how hepatitis C is transmitted.
Prevention Knowledge and Practice
A series of questions were developed to determine respondents’ knowledge about preventive and disease management behaviors that could reduce or avoid the complications of hemophilia and whether they engaged in these behaviors. Included in this series was the general question “What top three things do you do to manage your hemophilia and limit hemophilia complications?” Sixty percent of the respondents stated that they avoided or limited physical activity; 27% reported that they exercised as a preventive measure; and 24% indicated that they used clotting factor treatment preventively either on a regular schedule or before physical activity, sports, or strenuous exercise.
Twenty-four percent of the youth respondents reported that they were currently using long-term prophylaxis or undergoing routine treatment with blood products, and another 9% reported using short-term or problem-related prophylaxis. Roughly 22% indicated that they did not know whether or not they were being treated with some form of prophylaxis.
Respondents were asked specifically how quickly they usually treated a bleeding episode. They were asked to select the category that best described the timing of their self-treatment, ranging from within 1 hour to longer than 6 hours after the occurrence of a bleeding episode. Fewer than a third (31%) of the respondents reported treating a bleeding episode within 1 hour (Table 2 ▶).
TABLE 2—
Usual Timeliness of Self-Treatment of Bleeding Episodes: Youths 13–21 Years of Age, United States, 2000
| Sample, % | |
| 1 hour or less | 31 |
| 3 hours or less | 40 |
| 6 hours or less | 9 |
| Longer than 6 hours | 15 |
| Don’t know | 6 |
As a means of determining barriers to early treatment (i.e., treatment within 1–2 hours from the onset of the bleeding episode), participants were asked “When you cannot treat within an hour, what prevents you from doing so?” Twenty-nine percent of the youths stated they did not recognize such episodes and thus delayed treating them; 25% reported that they did not have clotting factor with them at the time of the episode. Another 11% indicated that they did not believe the episode was serious enough to require treatment. This last finding was related to the most prevalent response among the respondents: that they did not always recognize a bleeding episode when it occurred.
Exercise
In addition to early treatment of bleeding episodes, physical activity and exercise are important in preventing joint disease. Exercise strengthens muscle, and strong muscle protects joints. Youths were asked about their physical activity levels and participation in sports, particularly through the 2 earlier-described questions on strenuous and moderate activity adapted from the International Physical Activity Questionnaire.14 Respondents were asked how many days of the past 7 they had engaged in strenuous or moderate activities. More than a quarter (27%) responded that they did not engage in any strenuous or moderate physical activity on a regular basis.
DISCUSSION
Healthy Joints
Two important preventive measures against joint damage associated with hemophilia are physical activity/exercise and treatment timing, either early treatment of a bleeding episode (i.e., within 1 hour) or treatment with prophylaxis (a regimen of regular infusions). The present survey results provided the following specific information concerning the area of joint health: (1) joint damage was the top concern among the youth respondents; (2) 27% of these young people did not engage in any regular physical activity; (3) 60% believed that limiting physical activity is a way to manage their hemophilia; and (4) only 31% treated a bleeding episode in the recommended time period (i.e., within 1 hour).
Because episodes of bleeding into joints are the predominant types of bleeding episodes associated with hemophilia, there is a high risk of joint damage and disease, resulting in arthropathy, limits on range of motion, severe arthritis, and chronic pain. Building strong muscles and joints through physical activity decreases bleeding and its complications; however, if individuals experience joint damage, often from inadequate treatment or as a result of an injury, they are less likely to participate in activities and exercise that could maintain strong muscles and joints.
Rest, or refraining from physical activity, is in fact recommended once a bleeding episode has occurred; physical activity is urged as a preventive measure. Adults with hemophilia who did not have access to blood products and adequate treatment early in life almost always have visible joint deformities and experience chronic pain. Although prophylaxis is the optimal standard of care for children, it is only now being recognized that prophlaxis may need to be their lifelong treatment owing to the continued threat of joint destruction from bleeding.7
The factors just mentioned could have influenced young people’s response that joint disease was their most prevalent concern. The fact that one third of the respondents believed that joint disease was not preventable could explain why they reported low levels of participation in physical activity and why only one third reported that they treated a bleeding episode within 1 hour. Also, the primary reason they delayed treatment was that they did not recognize it as necessary.
Hepatitis Prevention
Hepatitis is another area of heightened salience for people with hemophilia and bleeding disorders (the liver processes clotting factors). Yet, our data revealed that although approximately 53% of the respondents had hepatitis C infection, 78% of the overall sample did not know how hepatitis C is transmitted, and 67% did not know how hepatitis B is transmitted.
The youths in the study cohort were born between 1978 and 1986. Heat-treated factor became available in 1985 for FVIII products (to treat hemophilia A or factor VIII deficiency) and in 1987 for FIX products (to treat hemophilia B or factor IX deficiency).15 In this study, 70% of the participants had the severe form of hemophilia, and 3% had the moderate form (the remainder had mild hemophilia). Therefore, 73% of these young people were likely to have been in the high-risk pool for viral infection through blood products.
Although not everyone at risk had contracted the viruses, it is important that all youths with hemophilia understand the infection routes and risks for hepatitis A, B, and C and for HIV. HTC providers consider such knowledge important in managing this chronic disease. As is the case in the general population, young people with hemophilia need to understand the risks associated with sexual activity and behaviors such as experimenting with illegal drugs, particularly during this period of evolving maturity that Green characterized as a virtual “mind, body and soul construction site.”16(p370)
Although most of the youths (71%) had been provided with information about hepatitis, the survey revealed a low level of actual knowledge of hepatitis and a highly prevalent belief that the disease is preventable. Despite the importance of understanding the various types of hepatitis, and despite the estimated incidence of hepatitis C infection in our cohort, 78% of these young people did not know how hepatitis C is transmitted. This finding points to the crucial need to educate young people with hemophilia about blood transmission of hepatitis B and C and the risk of sexual transmission of hepatitis B.
A limitation of the survey was that it was difficult to ascertain whether the 16% of respondents who believed that the different types of hepatitis are not preventable held this belief because there is no vaccine for hepatitis C or because of their lack of knowledge about the safety of blood products and the effectiveness of hepatitis A and B vaccination in preventing transmission. Our results indicate that prevention campaign messages aimed toward young people need to emphasize hepatitis education.
Developing a National Prevention Campaign
Working from the key findings of the national survey described here and extant knowledge in the field, the NHF and CDC distilled 5 key messages (Figure 1 ▶) that they believed would be necessary in an effective campaign to prevent complications of bleeding disorders. Focus group testing with young people yielded a slogan—“Do the 5!”—that has become rather ubiquitous throughout the hemophilia and bleeding disorders community.
These campaign messages are currently being delivered to patients participating in NHF chapter, association, and HTC activities. Prevention teams, each composed of a young person with a bleeding disorder, a chapter or local association representative, and an HTC staffperson, have been formed in local communities. National and regional training sessions have been conducted to assist chapters, associations, HTCs, and their prevention teams in developing strategies to deliver these messages. In addition, trained youth peer educators are integral to message delivery. Finally, an evaluation strategy is being developed to ensure the effectiveness of the campaign.
Conclusions
Effective prevention message campaigns must be evidence-based and tailored toward specific target populations within the campaign audience. Delivery of messages to specific populations requires assessment and input from a sample of the target audience, ensuring a patient-centered approach.
When designing a campaign aimed at individuals with a chronic condition, it is important to take into account the sensitivities, feelings, fears, and other issues associated with the condition. Equally important is consideration of normative developmental or life stage issues for the target population, particularly when interventions are being targeted toward young people with chronic conditions.
Acknowledgments
This study was funded through a cooperative agreement between the Centers for Disease Control and Prevention and the National Hemophilia Foundation (U50/CCU214593).
We thank Michael Soucie for his contributions to the sampling design, data analyses, and discussion of the study methods; Lauren Daitch and Neil Frick of the National Hemophilia Foundation for assistance with the literature review; and William Milczarski of the City University of New York for copyediting. Also, we wish to particularly acknowledge the contributions of the 20 hemophilia treatment centers, the 8 NHF chapters and local associations, and their patients and members.
Human Participant Protection This study was approved by the institutional review boards of the university medical centers affiliated with the 20 hemophilia treatment centers, the National Institutes of Health, and Macro International. All participants provided informed consent.
Peer Reviewed
Note. The findings and conclusions presented are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Contributors A. M. Nazzaro, S. Owens, and W. K. Hoots originated and developed the project, from questionnaire construction through sample design, data analysis, and implementation. K. L. Larson assisted with questionnaire development, data collection, and program implementation. A. Nazzaro wrote the original draft and S. Owens wrote the revised version, with each editing the other’s work.
References
- 1.Soucie JM, Evatt B, Jackson D. Hemophilia Surveillance System Project Investigators. Occurrence of hemophilia in the United States. Am J Hematol. 1998; 59:288–294. [DOI] [PubMed] [Google Scholar]
- 2.DiPaola J, Nugent D, Young G. Current therapy for rare factor deficiencies. Haemophilia. 2001;7(suppl): 16–22. [DOI] [PubMed] [Google Scholar]
- 3.Hemophilia Data Set, Calendar Year 2000. Atlanta, Ga: Centers for Disease Control and Prevention; 2000.
- 4.Soucie JM, Nuss R, Evatt B, et al. Mortality among males with hemophilia: relationship with source of medical care. Blood. 2000;96:437–442. [PubMed] [Google Scholar]
- 5.Battistella LR. Maintenance of musculoskeletal function in people with haemophilia. Haemophilia. 1998;4(suppl 2):26–32. [DOI] [PubMed] [Google Scholar]
- 6.Rodriguez-Merchan EC. Effects of hemophilia on articulations of children and adults. Clin Orthop. 1996; 328:7–13. [PubMed] [Google Scholar]
- 7.Recommendation Concerning Prophylaxis. New York, NY: National Hemophilia Foundation, Medical and Scientific Advisory Council; 2001. MASAC document 117, updated June 2006, document 170.
- 8.Report on the Universal Data Collection Program. Atlanta, Ga: Centers for Disease Control and Prevention; 2005.
- 9.Manco-Johnson MJ, Abshire TC, Brown D, et al. Initial results of a randomized, prospective trial of prophylaxis to prevent joint disease in young children with factor VIII (FVIII) deficiency. Paper presented at Annual Meeting of the American Society of Hematology, December 2005, Atlanta, Ga.
- 10.Chorba T, Holman R, Clarke M, Evatt B. Effects of HIV infection on age and cause of death for persons with hemophilia A in the United States. Am J Hematol. 2001;66:229–240. [DOI] [PubMed] [Google Scholar]
- 11.Eyster E, Sherman KE, Goedert JJ, et al. Prevalence and changes in hepatitis C virus genotypes among multi-transfused persons with hemophilia. J Infect Dis. 1999;179:1062–1069. [DOI] [PubMed] [Google Scholar]
- 12.Ragni MV. Hepatitis A vaccine trial in individuals with hemophilia. HemAware. January/February 1997: 14–16.
- 13.Kyngäs H, Kroll T, Duffy M. Compliance in adolescents with chronic diseases: a review. J Adolesc Health. 2000;26:379–388. [DOI] [PubMed] [Google Scholar]
- 14.International Physical Activity Questionnaire. Available at: http://www.ipaq.ki.se. Accessed June 15, 2006. (originally accessed Spring 1998).
- 15.Soucie JM, Richardson LC, Evatt B, et al. Risk factors for infection with hepatitis B and hepatitis C viruses in a large cohort of hemophilic males. Transfusion. 2001;41:338–343. [DOI] [PubMed] [Google Scholar]
- 16.Green K. Treatment strategies for adolescents with hemophilia: opportunities to enhance development. Adolesc Med. 1999;10:369–376. [PubMed] [Google Scholar]


