Abstract
The incidence, clinical and investigative features, treatment, and course of severe oesophagitis in 200 patients seen and followed up in the Thoracic Surgical Department for north east Scotland from 1951 to 1967 are reviewed. The male/female ratio was 1/1·9. The incidence of severe oesophagitis (grades III and IV) approximated to 4·5 per 100,000; there was a dramatic increase from the age of 50 years onwards.
Reflux, with or without hiatal hernia, precedes oesophagitis and has an incidence in excess of 86 per 100,000. It is difficult to assess the extent to which reflux produces mild oesophagitis, but it is clear that it only infrequently leads to the severe grades.
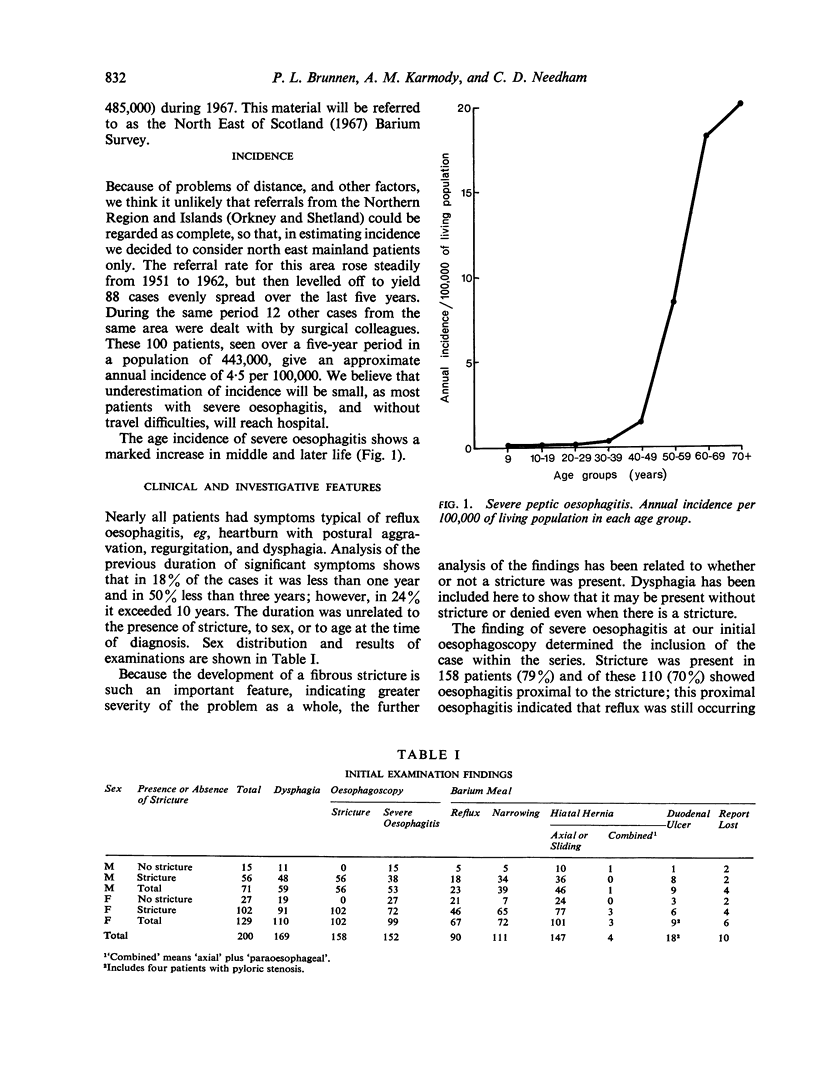
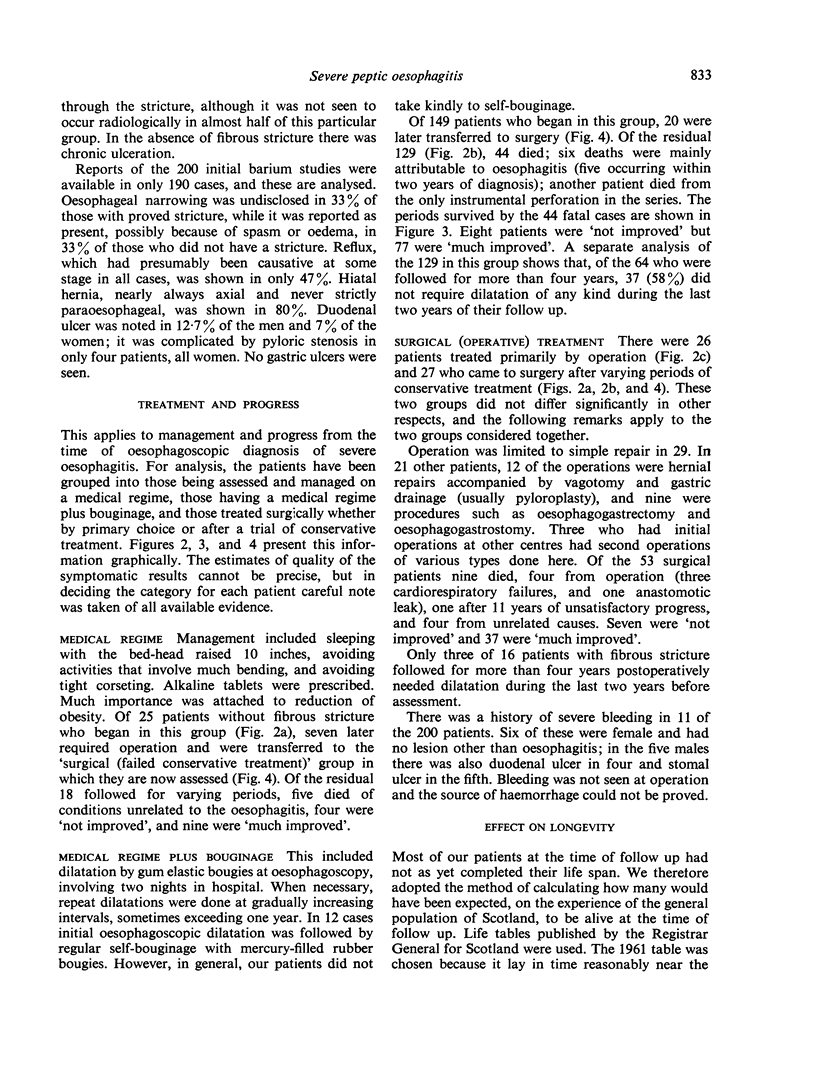
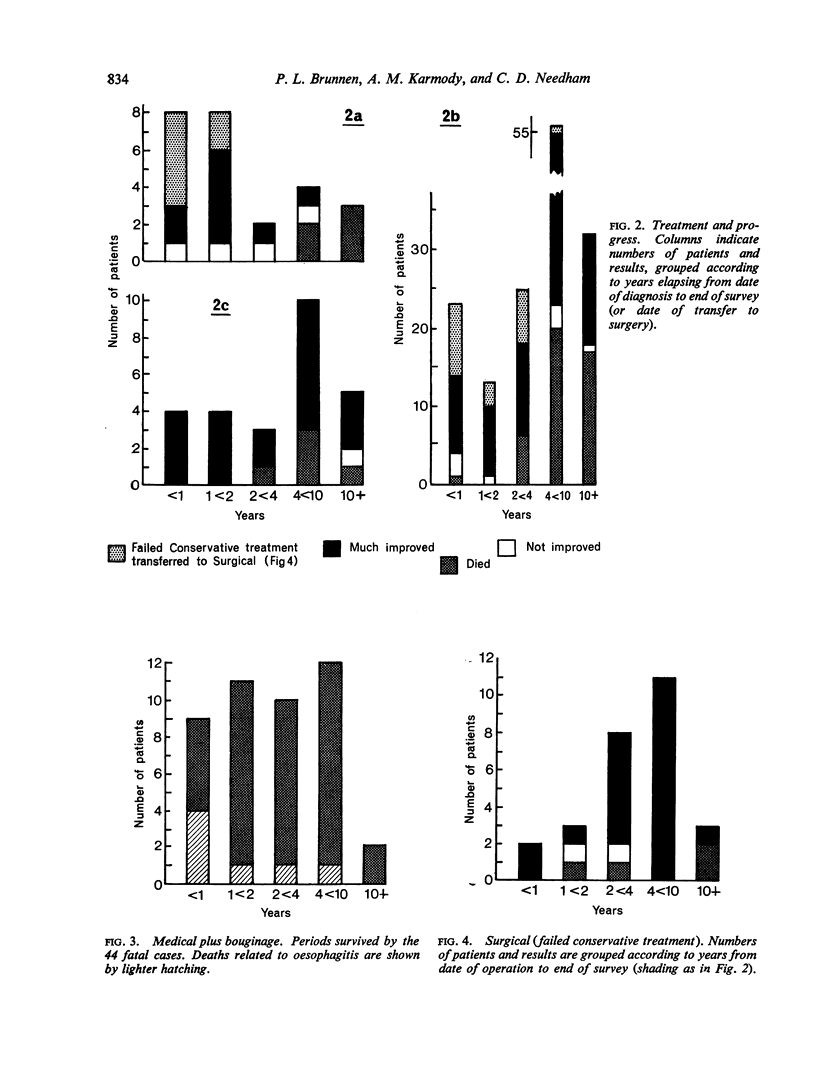
Severe oesophagitis does not always need operative treatment. A conservative regime, supplemented by bouginage as required, enables the poorer-risk older patient to live a near-normal life span, in very reasonable comfort. Fifty-three patients of the whole series were operated upon, half primarily and half after previous conservative treatment. The problems of operative treatment are discussed. Newer procedures designed to prevent reflux now allow operation to be more freely advised.
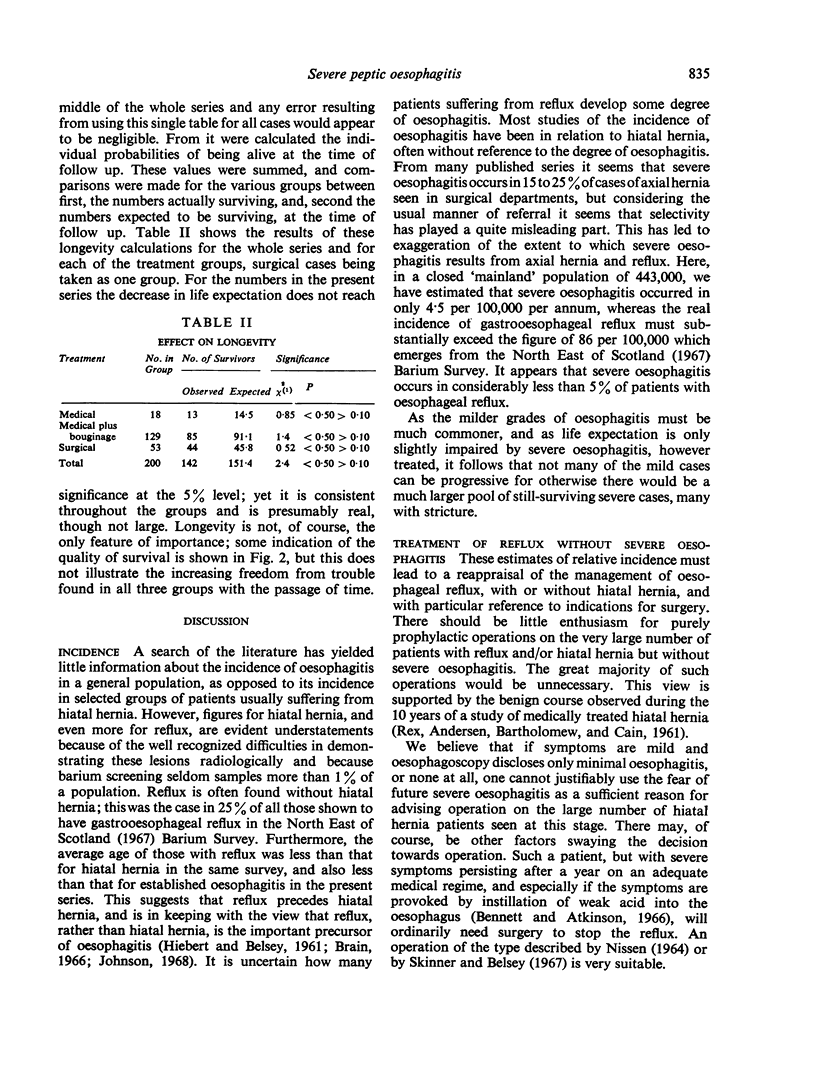
Perhaps, rather surprisingly, severe oesophagitis had very little effect on the expectation of life, whether treatment was conservative or operative.
Full text
PDF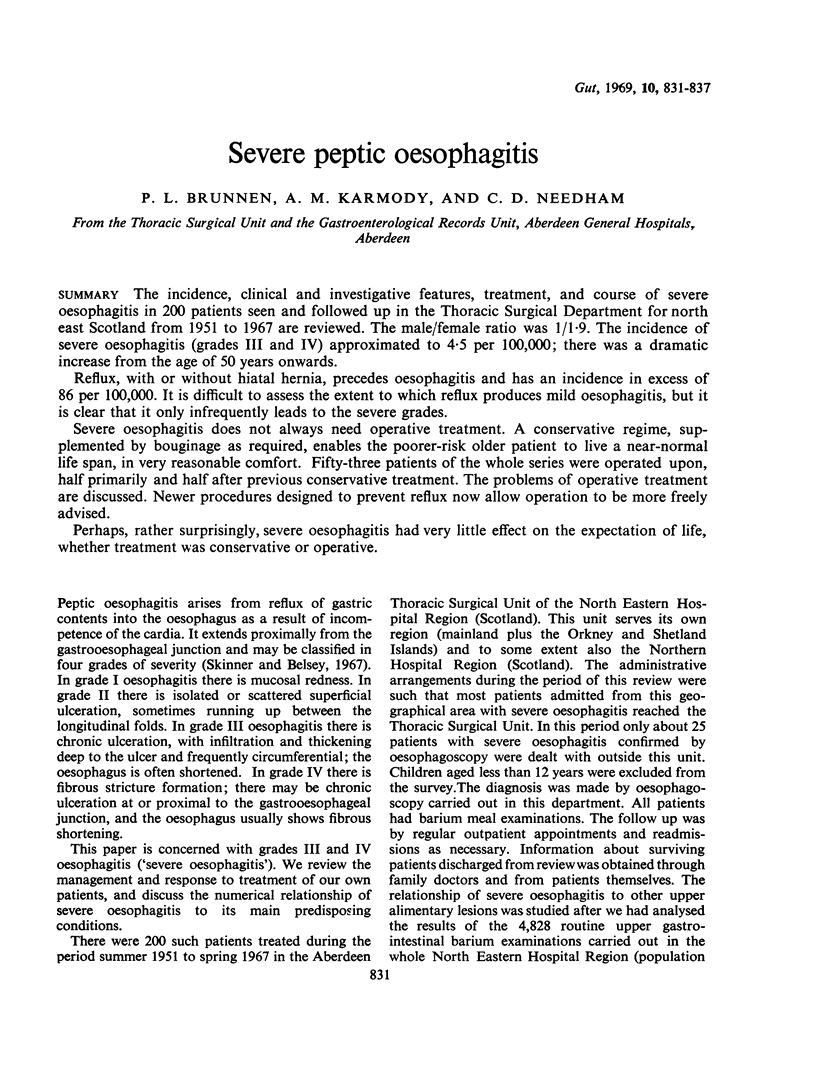

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ALLISON P. R. Reflux esophagitis, sliding hiatal hernia, and the anatomy of repair. Surg Gynecol Obstet. 1951 Apr;92(4):419–431. [PubMed] [Google Scholar]
- BARRETT N. R. Benign stricture in the lower esophagus. J Thorac Cardiovasc Surg. 1962 Jun;43:703–715. [PubMed] [Google Scholar]
- Belsey R. Benign strictures of the oesophagus. Proc R Soc Med. 1966 Oct;59(10):932–933. [PMC free article] [PubMed] [Google Scholar]
- Bennett J. R., Atkinson M. Oesophageal acid-perfusion in the diagnosis of precordial pain. Lancet. 1966 Nov 26;2(7474):1150–1152. doi: 10.1016/s0140-6736(66)90472-7. [DOI] [PubMed] [Google Scholar]
- Brain R. Peptic strictures of the oesophagus associated with duodenal ulcer and operations for its relief. Proc R Soc Med. 1966 Oct;59(10):929–931. [PMC free article] [PubMed] [Google Scholar]
- Burge H. W., Gill A. M., MacLean C. D., Lewis R. H. Symptomatic hiatus hernia: a study of the pyloro-duodenal region and the rationale of vagotomy in its treatment. Thorax. 1966 Jan;21(1):67–74. doi: 10.1136/thx.21.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson J. S. Hiatal hernia. Postgrad Med J. 1968 Aug;44(514):579–585. doi: 10.1136/pgmj.44.514.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HIEBERT C. A., BELSEY R. Incompetency of the gastric cardia without radiologic evidence of hiatal hernia. The diagnosis and management of 71 cases. J Thorac Cardiovasc Surg. 1961 Sep;42:352–362. [PubMed] [Google Scholar]
- REX J. C., ANDERSEN H. A., BARTHOLOMEW L. G., CAIN J. C. Esophageal hiatal hernia: a 10-year study of medically treated cases. JAMA. 1961 Oct 21;178:271–274. doi: 10.1001/jama.1961.03040420011003. [DOI] [PubMed] [Google Scholar]
- Skinner D. B., Belsey R. H. Surgical management of esophageal reflux and hiatus hernia. Long-term results with 1,030 patients. J Thorac Cardiovasc Surg. 1967 Jan;53(1):33–54. [PubMed] [Google Scholar]
- THAL A. P., HATAFUKU T., KURTZMAN R. NEW OPERATION FOR DISTAL ESOPHAGEAL STRICTURE. Arch Surg. 1965 Apr;90:464–472. doi: 10.1001/archsurg.1965.01320100008003. [DOI] [PubMed] [Google Scholar]
- Tanner N. C. Stricture of the lower œsophagus. Proc R Soc Med. 1966 Oct;59(10):933–933. [PMC free article] [PubMed] [Google Scholar]
- Weir R. D., Backett E. M. Studies of the epidemiology of peptic ulcer in a rural community: prevalence and natural history of dyspepsia and peptic ulcer. Gut. 1968 Feb;9(1):75–83. doi: 10.1136/gut.9.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]


