Abstract
Internationally, stigma prohibits effective HIV/STD identification, prevention, and care. Interviews with 106 persons in an urban center in Eastern China, some know to have engaged in stigmatized risk acts (sex workers, STD clinic patients) and some vulnerable for stigmatization fears to influence health seeking behaviors (market employees, rural-to-urban migrants). Interviews focused on community norms, values, beliefs, and emotional and behavioral reactions to HIV/STD stigmatization related events. Attributions for infection were found to: mark individual's failure to adhere to sexuality norms; define a condition warranting the avoidance of infected persons and dismissal by medical professionals; and promote anticipation of negative emotions (i.e., shame, fear, and embarrassment) and devalued social roles and status. Strategies reported to avoid stigmatization include: avoiding HIV/STD knowledge; avoiding health care professionals, particularly in public settings; and conforming to community norms of shunning those suspected of risky behaviors. Results have direct implications for community marketing campaigns in China.
Keywords: Stigma, HIV/AIDS, STDs, China, Health Seeking
INTRODUCTION
“Stigma is a term that involves both deviance and prejudice but goes beyond both. Stigma involves perceptions of deviance but extends to more general attributions about character and identity. Stigma is more inclusive than prejudice because it involves individual-based responses to deviance, as well as group-based reactions as a function of category membership. Because stigma is socially defined, there is considerable variation across cultures...” (Dovidio, Major, and Crocker, 2000, p. 5).
Internationally, stigma is a major barrier to the prevention of HIV (World Health Organization, 2001; Lupton, 1999; Lamptey, 2002). China has 1 million Persons Living with HIV (PLH) and will have an anticipated 10 million PLH by the year 2010 (Rosenthal 2002; France-Presse 2002). With over 1/5 of the world's population (1.4 billion persons), the risk of a rampant epidemic is substantial. HIV-related stigma and discrimination impede every step in mounting an effective response for prevention, treatment, and care in China, similar to the way mental health problems (Tsang et al. 2000; Liu et al, 2003; Phillips, 2002) have been previously stigmatized. While systematic studies on HIV-related stigma in China are scarce, there are a substantial number of reports of PLH (people living with HIV) who have been stigmatized: vegetables grown by PLH cannot be sold in markets, children from families with a PLH have been barred from school, and persons suspected to have HIV have been denied health care services (Rosenthal, 8/25/2002; Ruwitch, 2002; Gu, 2002; Chu, 3/17/2002). Given the implications of HIV status on health seeking behavior, reducing HIV-related stigma is an urgent public health priority—having been listed as an important area for future international research collaboration during the Sino-US Conference on Research and Training in AIDS-related Areas (China CDC and US NIH 2002).
One key danger to HIV stigmatization is that associated fears can motivate secretiveness and denial that may allow risky sex behavior to continue (Citizens Commission on AIDS for New York City and Northern New Jersey, 1991; Coughlan, et al., 2001; Derlaga et al., 2002). For these individuals, fears of stigmatization may act as barriers to seeking care (Ward et al., 1997; Chesney and Smith, 1999; Brown et al., 2003). Stigmatization processes and fears must be understood in order to enhance the utilization of health care services through refining community marketing campaigns and service delivery strategies (Liu, et al., 2003).
This paper examines fears of HIV/STD stigmatization among persons who, by virtue of personal experience, may anticipate such stigma (i.e., sex workers and those treated for sexually transmitted diseases), and others able to provide insights into current community norms regarding such stigma (i.e., market workers and migrant workers). The primary focus of this study is to better understand how HIV/STD stigmatization fears may influence health seeking behavior in China. An attribution model is used to frame an understanding of how aspects participant provided reports of beliefs and values lead to particular patterns of behavior.
Socio-ecological perspectives argue that individuals' beliefs, values, and practices are determined by various aspects of the socio-cultural context (Bronfenbrenner, 1999, Super and Harkness, 2002; Markus and Kitayama, 1991). Stigma research points to context as a critical determinant of the psychological and behavioral affects of stigmatization (Crocker and Quinn, 2000). Thus, while stigmatization fears may emerge through interpersonal processes, the impacts on individuals are “determined by the broader cultural context (involving stereotypes, values, and ideologies), the meaning of the situation for participants, and the features of the situation that influence this meaning” (Dovidio et al., 2000, p. 3). An attribution perspective provides insight into the mechanisms through which health behavior decisions are formed as a function of the socio-cultural beliefs, values, and morals. This insight can then inform strategies for intervention and the evaluation of intervention effects. We explore how shared social beliefs, values, and morals may influence individuals, particularly the health seeking behavior of those who engage in acts that put them at risk for HIV/STD infection (Crandall and Moriarty, 1995; Weiner et al., 1988).
Attributions are the results of social-cognitive processing in which individuals “interpret” social events toward determining their emotional and behavioral responses. Thus, appreciation of the internalized biases in typical attributions for HIV/STD risk behavior (acquired through normative socialization in a particular context) will inform an understanding of stigmatization fears. Attribution perspectives on stigmatization have focused on the dimensionality of stigmatization and how key dimensions contribute to understanding the stigma related experience. Empirical work has focused largely on the attribution dimensions of perceived danger, visibility, and controllability (Frable, 1993, Deaux et al., 1995; Crocker et al., 1998). Crocker et al. (1998) argued that the central dimensions to an optimal understanding of stigmatization are visibility and controllability—dimensions clearly relevant to attributions for HIV/STD risk behavior. “Visibility” impacts the selection of coping strategies individuals may take to manage the existence of a stigma and the amount of effort they may exert to conceal information about its presence. Thus, visibility concerns motivate both psychological and behavioral controls (Miller and Major, 2000; Smart and Wegner, 2000). The visibility dimension is defined here to include both characteristics apparent to the eye and any behavior that may indicate to others that one is a member of a potentially stigmatized group. “Controllability” of a stigma refers to the attributions one may form regarding an individual's responsibility for a stigma, as well as for maintaining or eliminating the mark (Weiner et al., 1988; Crandall, 2000, Cobb and DeChabert, 2002). Concerning HIV/STD infection, it is noteworthy that Weiner's (1995) theory and evidence suggest particular increases in the intensity of negative reactions to stigma that carries a negative moral judgment. Weiner argues that while emotional reactions and subsequent behavior vary as a function of responsibility attributions, “reactions to the stigmatized are, in part, based on moral evaluations. Stigmatized persons considered responsible for their marks are construed as moral failures...” (Weiner, 1995, pp. 64-65). Thus, controllability attributions map directly onto HIV/STD risk behavior and determine individuals' beliefs about responsibility, emotion, and socio-moral reaction.
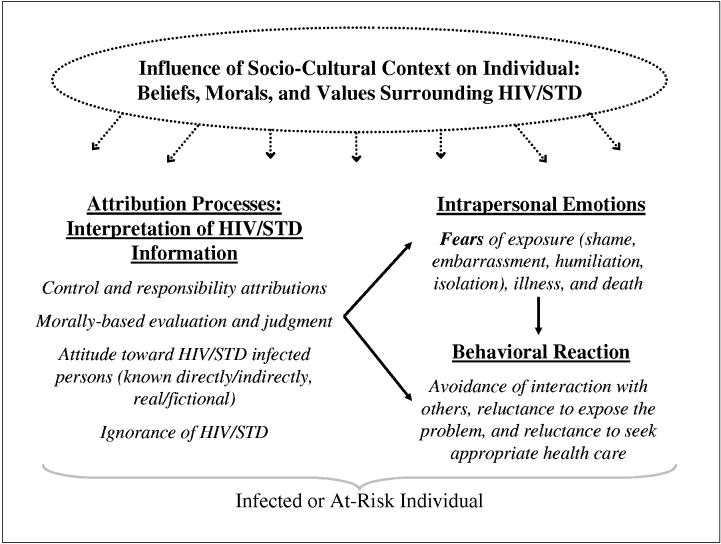
The attribution model presented here indicates that common socio-cultural beliefs and ideology surrounding HIV/STD exert a powerful influence on individuals through the arousal of stigmatization fears (Alonzo and Reynolds, 1995). Key features of this model are the broader socio-cultural beliefs, morals, and values held within the society, their influence on the content and nature of interpersonal interaction, and the cognitive processes through which relevant information is interpreted by individuals in determining emotional and behavioral responses (see Figure 1). The fear of social consequences associated with being exposed as sexually deviant increases the likelihood of activating the attribution process (Alubo et al., 2002; Chliaoutakis and Trakas, 1996; Leiker et al., 1995; Liu et al., 2002). Controllability beliefs and socio-moral judgments related to risky sex behavior determine perceptions of stigmatization and how they may impact the emotional and behavioral response of infected or at-risk individuals (Conrad, 1986; Fife and Wright, 2000; Pullium, 1993; Weitz, 1991). For example, Fife and Wright (2000) reported associations between the social and psychological impacts of HIV infection with experiences of social rejection, financial insecurity, internalized shame, and perceived social isolation. Moreover, the attribution dimension of peril or perceived danger is argued to intensify the process of evaluating HIV/STD stigmatization risk. Thus, fears of stigmatization will increase when HIV/STD infection is perceived as visible, controllable, and dangerous and such fears are associated with delays and avoidance of health seeking (Liu, et al., 2003).
Figure 1.
Foundations for HIV/STD Stigmatization Fears and Implications for Health Seeking Behavior: Attribution Model
Stigmatization can negatively impact any individual, and their close associates, who have been identified as participating in socially undesirable activities (Chesney and Smith, 1999; Fortenberry, et al., 2002; Liu, et al., 2003; Valdiserri, 2002). Identification of a target person as undesirable, deviant, or immoral can activate associated stigma beliefs and values and arouse feelings of disgust, anger, fear, sadness, and pity in others (Herek et al., 2002; Stokes and Peterson, 1998). Individuals aware of stigmatized characteristics or behaviors in others may seek to isolate or avoid the deviant person and extend these responses to target persons' associates (Herek et al., 2002). The nature and intensity of emotional and behavioral responses will be driven by the degree of fear and ignorance related to the risks of deviant characteristics or acts. Further, once individuals are “marked” or labeled as a member of a stigmatized group, they may have great difficulty re-establishing themselves in the minds of others as a desirable member of the mainstream society. This is particularly true where evidence of the stigma is easily identifiable (Lee et al., 2002; Frable et al., 1998). While HIV and STD related stigma is universal, the nature of any associated stigmatization will vary from one culture to another in terms of form and intensity depending on the relevant socio-cultural context—beliefs, values, morals.
The nature of stigma associated with HIV/STD, and its socio-emotional impact, is argued to depend on attributions of responsibility for infection, possible consequences for others, outward manifestations of illness, and possible effects on competence (Conrad, 1986; Fife and Wright, 2000; Weitz, 1991). Given the broad socio-cultural beliefs surrounding sexually transmitted disease, it is plausible that perceptions of stigmatization for HIV/STD infected or at risk individuals would be high as control is commonly attributed to internal and controllable factors within the infected individual (Herek and Capitanio, 1999; Ladany et al., 1998; Clement and Schoennesson, 1998). Moreover, infected or those believed at risk for HIV/STD are typically associated with immoral and deviant behavior, such individuals frequently report concerns about exposing their status, and the social and health consequences for others, while real, are often exaggerated because of poor knowledge and social myth (Alubo et al., 2002; Chliaoutakis and Trakas, 1996; Leiker et al., 1995; Liu, et al. 2003). Figure 1 illustrates how socio-ecological circumstances influence the lives of infected and at-risk individuals. Individuals implicitly understand these circumstances as community members and through interpersonal interactions within the local community. Thus, where a society defines a behavior as objectionable, there is more likelihood that engagement of the behavior will arouse perceptions of stigmatization in the actor.
Despite increased effort to document prevalence rates and routes of HIV/AIDS in China since the first case was reported in 1985 (Gil 1994; Yu et al. 1996; Wu et al. 1997; Ministry of Health 2001), limited attention has been paid to HIV/STD related stigma and the contexts in which the perception of stigmatization impact health services utilization. In related work, fears of stigma and discrimination among persons with schizophrenia and their families in China have been found to damage self-esteem and, in turn, led to increased denial of the illness and poor treatment compliance (Phillips et al., 1994). Similarly, Kleinman and colleagues (1995), focused on such culturally meaningful issues as “face”, stigma, and social control in Chinese persons with epilepsy, noted that actively avoiding stigmatization was a strategy taken to maintain a family's place in the social network. They concluded that this strategy was commonly adopted because stigma and moral blame within the Chinese culture are frequently extended to an entire family, rather than being limited to the individual alone (Kleinman et al. 1995). Further, stigmatization fears and desire to protect families from shame have been found as salient obstacles to HIV status disclosure given the collectivist nature of Asian culture (Yep 1992-1993; Chin and Kroesen 1999; Yoshioka and Schustack 2001). Other research in China has reported beliefs that promiscuous people are despised, to be avoided, and should be punished (Lee, et al. 2003)—beliefs that have been found lead to discrimination that causes numerous distressing reactions in HIV carriers and AIDS patients (Gan and Liu 2000). Finally, Liu and colleagues have found that higher levels of perceived stigma were associated with increased delay in treatment seeking and disclosure of test results (Liu, et al. 2003; Liu, et al. 2001). Liu et al. (2003) reported that 80% of their sample, across all population demographics, experienced stigmatization that resulted in health seeking delay. The present study investigates the foundation of these stigmatization experiences and their devastating effects on health seeking. Through discovery and description of the socio-cultural context in China surrounding HIV/STDs, we explore “why” and “how” stigmatization fears impact health seeking behavior. We consider how characteristics of this context encourage particular patterns of attribution and fears of stigmatization related to these diseases and, in turn, influence the health seeking behavior of at-risk individuals.
METHOD
Participants
100 individuals in an urban center in Eastern China were recruited for participation. These individuals represent a sub-set of the population under study in an intervention project focused on the prevention of HIV/STD transmission and include recruitment of: 12 commercial sex workers (CSW), 58 rural-to-urban migrant and local market workers (MW), and 30 STD clinic patients (SCP). The participant sample is 45% female, 55% male, average age of 27.5 years (range 18 to 46 years), and average education through middle school (range primary school to college). While the commercial sex worker group was all female, younger (average age 23.6 years), and largely unmarried (only one reported being married—8%), there were no other significant differences between the groups in gender, age, marital status, or education.
Interview Design
Data were collected through semi-structured face-to-face interviews. Questions targeted participants' knowledge, attitudes, and beliefs about HIV/STD and the symptoms, causes, prognoses, prevention, and treatment of these diseases.
Procedures
Employing stratified random sampling strategies to assure representation of individuals from a range of sex, age, and marital status, research staff recruited individuals to participate in a study seeking to learn about and improve the health of the community. Potential participants were supplied with information documenting the details of participation according to US University standards for volunteer informed consent. Interviews took place in either a local health education institute (the base of study activities) or, if more convenient for the participant, in private rooms at the participant's workplace. Trained fieldworkers conducted the interviews, which took between 30 to 90 minutes to complete, and participants were compensated with an hourly wage in China. Interviews were audiotaped, the interviewer generated fieldnotes, and partial transcription of the audio recording was carried out when necessary to support the fieldnote content.
Data Processing/Management
Fieldnotes and transcriptions from the interviews were translated to English for processing and analysis. Of these translations, approximately 25% were examined by bilingual project staff to assure content fidelity. The UCLA EthnoNotes system (Lieber et al., 2002), a tool for the management, integration, and analysis of quantitative and qualitative data, was applied in organizing, interpreting, and analyzing the interview fieldnotes. Excerpts identified as relevant to the study were coded based on a coding scheme developed to provide a framework for understanding participant perspectives on perceptions of stigmatization and health seeking behavior. Excerpts coded as relevant to issues of fear, embarrassment, health seeking behavior, stigmatization, shame, isolation, and/or exposure were analyzed. Coding of data from approximately 20% of the cases was subjected to inter-rater reliability analyses. For these cases, codes applied by two independent coders were compared in order to validate the reliability of coding decisions among team members. Acceptable levels of inter-rater agreement were found, average Cohen's Kappa statistic for inter-rater reliability of .75 and ranging from .64 to .79 across the cases. The remaining cases were subsequently coded by at least one of the trained coders with occasional checks to assure that acceptable levels of coding reliability were maintained.
RESULTS
Among the many topics discernable in these data related to HIV/STD and health seeking, fear was the most frequently mentioned and most clearly linked to health seeking behaviors. Fear was reported as relevant to: (a) socio-cultural norms of anything associated with HIV/STD, (b) about one's own infection status or the possibility of becoming infected through contact with a known or suspected infected person, and (c) social sanctions associates with individuals identified with the diseases or risky sexual behavior. The attribution process model applied here suggests that the foundation of these fears is based upon individual interpretations of socio-cultural beliefs about control and responsibility. These interpretations are based on attributions of cause, moral evaluations of those whose behavior exposes them to HIV/STD infection, and attitudes and behaviors directed at those who are infected or believed to engage in risky behavior. This foundation establishes a social context in which perceptions of stigmatization are internalized and act as a barrier to appropriate health seeking behavior where it would be indicated.
The core dimensions of stigmatization described from an attributional perspective (Frable, 1993; Crocker et al., 1998) are well supported by the study evidence. It is noteworthy that the issues identified and discussed here were not subject to direct inquiry during the interviews. Thus, where the themes analyzed here were discussed by the participants, the relevant excerpts represent spontaneous discussion by the participants in the context of more general questioning. As such, 58% of the participants provided excerpts related to the themes analyzed here—no significant differences were found across participant gender, age, or sub-group (i.e., market employee, commercial sex worker, STD clinic patient) in the percentage of excerpts provided for each theme. Given only a subset of the full sample provided data relevant to the issues analyzed, percentages noted in the results discussion refer to this group. Key issues related to stigmatization are presented individually for clarity and to focus on the mechanisms of impact on health seeking. However, while they can be described out of context, it is important to consider that target individuals' actual experience must be understood as a holistic process. That is, the various issues are interrelated in complex ways toward a powerful generalized “fear” response and, thus, operate as a barrier to decisions about seeking appropriate health care. Finally, results illustrate how an attribution model can be applied to understand stigma as a barrier to health seeking behavior.
HIV/STD Stigmatization Fear in the Chinese Socio-Ecological Context
“Anyone who leads a decent life won't get this disease [AIDS]. Since it is hard to cure, people are very afraid of it. If an AIDS patient was identified within the community, they would be avoided because it is a serious and frightening disease, and it isn't clear how AIDS is spread. STD patients would be too embarrassed to have the disease treated and might give up; thinking it is hard to cure and they would have to tell the doctor how they got it. If they did get help, they would start at a private clinic where the doctors would probably not tell them if it is curable but just ask them to take their medicine. If one or two series of medication do not work, they might then go to a larger hospital. Finally, [in response to my question about where to get STD information] since I did not have an STD I have no intention to obtain any information about it” (MW30: a 29 year old female market worker with a primary school education).
This report is common among study participants and illustrates many beliefs about HIV/STD infected people, the quality and use of available health care, issues of disclosure, and perceived need for HIV/STD information. Across the sample, 43% of participants spontaneously provided such general statements about HIV/STD beliefs and values. From a socio-ecological perspective, the evidence regarding the attributional beliefs, morals, and values related to HIV/STD from this Chinese sample characterizes a context for fearfulness and stigmatization that would influence health seeking behavior. These circumstances are exacerbated by poor knowledge about HIV/STD transmission, symptoms, and treatment (apparent in reports from 36% of the sample) which has been shown associated with higher levels of discrimination and lower levels of empathy associated with HIV/STD stigma.
References to fearfulness and embarrassment about talking to others, even to medical personnel, about the possibility of infection are frequent—mentioned spontaneously by 64% of the interview participants. Further, expressed fears of discrimination and despise are salient—mentioned by 69% of the sample. For example, “I'm afraid they will look down on me [if I told friends/family I had this disease], they would definitely despise someone who got HIV because they will think it came from a promiscuous life and their treatment of this person would change... doctors cannot be friendly to HIV patients because they are afraid of being infected” (MW105). One sex worker says, “Patients will feel embarrassed when they see a doctor. We are afraid the doctors may have some discrimination against us, afraid of being looked down on. Other people would think that women with STDs must have had sex with someone, but they would think it is more common for men” (CSW106). And from another, “Doctors and health workers would be very fierce to the patient, even though the patient is shy, and they said ‘Oh, let me wash my hands, I don't want to get infected.’ One doctor asked me if I was a ‘service girl.’ You see, people of the service trade are hardly acceptable to society” (CSW110). These quotes also illustrate the moral judgments made toward those engaging in deviant and risky sexual behavior. Persons known to have put themselves at risk for HIV/STD infection are seen as shameless and likely to be socially isolated, experience discrimination, and perceived with disgust and despise. “STD's usually happen to men who had sex with sex workers, but can also be spread through cotton-padded quilts and clothes of hotels. Such things also appeared on TV and in books on family. The book ‘Happy Family Life’ tells of a man who got an STD in a hotel when he traveled on business and was misunderstood and even hated by his own family... STD patients are still looked down upon and discriminated against in the society” (MW21).
Key Attribution Dimensions of Stigmatization
Controllability- Thirty-nine percent of the sample provided excerpts indicating that attributions for infection are made to controllable causes, responsibility is assigned to the infected person, and moral judgments are imposed. The quotes above clearly illustrate the commonly held views which establish a context for fear regarding HIV/STD and, beyond the dangers of the diseases themselves, the potential social and psychological costs—perceived stigmatization—for anyone engaging in or suspected of behaviors that might expose them to the risk of infection. Simply, HIV and other STDs are commonly, albeit simiplistically, associated with sex workers and those who seek their services.
Peril- Study participants frequently report fears related to the peril and visibility attribution dimensions, introduced earlier. First, fears about infection from contact with those believed to be infected are noted by 88% of all participants. The perceived danger of infection influences the level of fear and is linked to knowledge of and beliefs about disease transmission. Participants' reports that indicate relative ignorance and folk beliefs support higher levels of fearfulness and discriminative behavior, even from medical professionals. For example, “When friends or relatives know of a case [AIDS infection], they would not let him come back home and they will despise him because AIDS is infectious. It can spread through bowls or chopsticks when eating together... Doctors or health workers might also be afraid to treat him for fear of infection” (MW119). Reports of possible HIV infection through shared food containers, serving utensils, contact with clothes or water, and sharing of saliva are frequently mentioned. Concerns about the implications of infection are rational, but the lack of education and folk beliefs lead community members to take extreme precautions to avoid any contact with infected persons.
Visibility- Perhaps one of the most powerful fears impacting health seeking behavior in China are reflected in reports about social sanctions toward infected persons or those believe at risk for infection. Here the attribution dimension of visibility is relevant to the extent that individuals will resist exposing themselves to being identified with any behavior that involves infection risk. Sixty-nine percent of the sample make spontaneous reference to expectations of despise, shamefulness, and fear of condemnation for infected or at risk individuals. For example, “I caught trichomoniasis. First I paid 70 yuan for an exam from the No. 1 City Hospital and was diagnosed with gonorrhea, and had to pay another 300 or more yuan for medicine. Not believing I had gonorrhea, I saw a professor of the Provincial Institute of Chinese Traditional Medicine who sent me to the Provicial Hospital for an exam. He also asked if my husband did bad things outdoors and advised that I take care at home by not washing my clothes with my children's and not sitting on the same bench with them. At the Provincial Hospital I was diagnosed with vaginitis and received a prescription for some effective medicine that cost about 60 yuan. So I thought highly of the Provincial Hospital, but shocked by the No. 1 City Hospital in their suggesting I had done bad things outdoors. No education or advice was provided at either of these hospitals. As for AIDS, I fear being infected. Once anything bad happened [meaning immoral sexual conduct], my reputation would be affected and I would be condemned by society. So, usually AIDS patients would never tell others” (from interview with MW21: married female market worker with primary school education).
The nature of the Chinese socio-ecological context fosters fears related to the negative impacts on one's social status and relationships if identified with HIV/STD. Anticipated attitudes and behaviors toward the HIV/STD patients, and their close associates, exert a powerful and salient impact on associated health seeking behavior. As such, individuals will go to great lengths and accept serious risks and/or consequences to avoid exposing oneself to others as having engaged in risky sexual behavior.
Health Seeking Patterns
“There is certainly difficulties to seeking treatment from doctors for fear that people will say you have been promiscuous. Treatment is not easy either and depends on how much money you have. Girls are more embarrassed and afraid of being talked about and dare not tell others if they have contracted an STD. Men might be afraid of being laughed at” (MW102).
Fifty-two percent of participants provided explanations for treatment seeking in response to suspected STD infection. The sequence of treatment typically involves three stages with the first being an attempt to self-treat through a visit to the local pharmacy. This step is the most anonymous and involves self-diagnosis or accepting the advice of a friend or pharmacy worker. When this strategy is found to be ineffective, they next seek care at a private clinic for convenience and in order to protect one's privacy and anonymity. While care at private clinics is considered expensive and often ineffective, the majority of STD patients report having visited such a clinic before finally seeking care at a public hospital or STD clinic. “It is convenient to see doctors in private clinics, but I am afraid of the cost and quality of care. If my disease recurs I should go to a public hospital... I don't know if patients are looked down on, but I am afraid to tell other people” (SCP111). Often as the last resort, and despite being broadly acknowledged as the best quality and lower cost care, patients will seek diagnosis and treatment from doctors at public provincial hospitals and STD clinics. After finally seeking his care at an STD clinic, SCP113 reports, “I have spent a lot of money to cure this disease. I have no other choice. A lot of people will talk about you if they know you have it, so I fear others will know. When I come here I am afraid of encountering an acquaintance.”
DISCUSSION
This study's findings provide a number of insights into the impact of HIV/STD stigmatization fears on health seeking behavior. Evidence indicates that health seeking decisions are influenced by a complex set of factors that include suspicion about the quality and reliability of diagnosis and treatment, concerns about the monetary and time costs, and concerns about exposing oneself to social sanction. Participant reports clearly indicate that the strength of socio-moral values and beliefs are particularly salient and powerful determinants of behavior in Chinese society. One prominent implication of this social force is stigmatization and, in order to avoid social reprimand, individuals will take extraordinary measures to prevent exposure as having engaged in risky sex behavior. Consequently, stigmatization fears present a powerful obstacle to individuals' willingness to discuss risky behaviors with others, respond appropriately to the appearance of HIV/STD symptoms, and seek health care when necessary.
Key dimensions of attributions for HIV/STD infection were explored and demonstrate the utility of an attributional model for understanding the impact of stigmatization fears in China. Findings indicate that reports of attribution for HIV/STD infection in this population are to controllable causes, concerns about exposure are high, sympathy is low, and there is considerable ignorance about and fear of infection. Under these conditions, Weiner (1995) suggests that there is a high likelihood of stigmatization and beliefs associated with HIV/STD and we find such stigmatization fears widespread in participant. Socio-moral judgments about infected persons in Chinese society perpetuate beliefs and cultural models about risky sex behavior, justify moral condemnation, and impact target persons via interpersonal engagement and their perceptions of stigma based on their interpretations of these socio-cultural beliefs. Findings here suggest that response to this impact is based primarily on “fear”—fear of shame, humiliation, embarrassment, and other social implications of exposure. Participant reports illustrate the nature by which their health seeking decisions are influenced by concerns about exposure based on the broader socio-cultural context. And, as such, stigmatization fears exert a strong negative influence on health seeking behavior related to HIV/STD infection.
This study contributes to a growing appreciation for the importance of addressing stigmatization issues in HIV/STD research and intervention (see Brown et al., 2003 for a review). Further, we recognize the need to incorporate culturally sensitive and responsive methods and interpretation that assure target populations can communicate local understandings of key issues associated with HIV/STD stigmatization. While the design of this study did not allow for a systematic within-subject investigation of stigmatization fears and associated outcomes, these are the data that allow researchers to understand the cultural context in which target populations live and negotiate. We find that an attributional perspective is well suited to understand the nature of HIV/STD stigmatization fears and their impact on health seeking behavior in China. This understanding supports the development of interventions and education to target the content and activities that are most likely to be effective in promoting the desired change. The larger intervention study from which the data used here were collected has benefited from this research and we hope other approaches will be similarly enhanced.
ACKNOWLEDGEMENTS
The study was funded by NIH/NIMH (grant #1U10MH61513) as a five-country Cooperative Agreement implementation of the Community Public Opinion Leader (C-POL) prevention program. The steering committee members for the study are: Carlos F. Caceres, M.D. (Peru); David D. Celentano, Sc.D. (U.S./India); Thomas Coates, Ph.D. (U.S./Peru); Tyler Hartwell, Ph.D. (U.S./RTI); Danuta Kasprzyk, Ph.D. (U.S./Zimbabwe); Jeffrey A. Kelly, Ph.D. (U.S./Russia); Andrei Kozlov, Ph.D. (Russia);Willo Pequegnat (NIHM); Mary Jane Rotheram, Ph.D. (U.S./China); Suniti Solomon, M.D. (India); Godfrey Woelk, Ph.D. (Zimbabwe); and Zunyou Wu, M.D. (China). Our appreciation to the research team in Fuzhou, China for their efforts in collecting and preparing the data for this study and to Michael Johnson, Ph.D. and Lai Ling Chau for their help developing and preparing this manuscript.
References
- Alonzo AA, Reynolds NR. Stigma, HIV and AIDS: An exploration and elaboration of a stigma trajectory. Social Science and Medicine. 1995;41(3):303–315. doi: 10.1016/0277-9536(94)00384-6. [DOI] [PubMed] [Google Scholar]
- Alubo O, Zwandor A, Jolayemi T, Omudu E. Acceptance and stigmatization of PLWA in Nigeria. AIDS Care. 2002;14(1):117–126. doi: 10.1080/09540120220097991. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. Environments in developmental perspective: Theoretical and operational models. In: Friedman SL, Wachs TD, editors. Measuring environment across the life span: Emerging methods and concepts. American Psychological Association; Washington, DC, US: 1999. pp. 3–28. [Google Scholar]
- Brown L, Macintyre K, Trujillo L. Interventions to reduce HIV/AIDS stigma: What have we learned? AIDS Education and Prevention. 2003;15(1):49–69. doi: 10.1521/aeap.15.1.49.23844. [DOI] [PubMed] [Google Scholar]
- China CDC Report from Chinese Center for Disease Control and Prevention 2002. November 1-3Paper presented at the The Sino-US Conference on Research and Training in AIDS-related Areas, Beijing, China [Google Scholar]
- Chesney MA, Smith AW. Critical delays in HIV testing and care: The potential role of stigma. American Behavioral Scientist. 1999;42(7):1162–1174. [Google Scholar]
- Chin D, Kroesen KW. Disclosure of HIV infection among Asian/Pacific Islander American women: Cultural stigma and support. Cultural Diversity and Ethnic Minority Psychology. 1999;5(3):222–235. [Google Scholar]
- Chliaoutakis J, Trakas DJ. Stigmatization, discrimination and fear of AIDS in Greece: Implications for health policy. Ethnicity and Health. 1996;1(4):359–371. doi: 10.1080/13557858.1996.9961805. [DOI] [PubMed] [Google Scholar]
- Choi K-H, Yep GA, Kumekawa E. HIV prevention among Asian and Pacific Islander American men who have sex with men: A critical review of theoretical models and directions for future research. AIDS Education and Prevention. 1998;10(3):19–30. [PubMed] [Google Scholar]
- Chu H.Doctor wages lonely battle against AIDS in China Los Angeles Times 2002. Issue Date
- Citizens Commission on AIDS for New York City and Northern New Jersey, N.Y., NY AIDS prevention and education: Reframing the message. AIDS Education and Prevention. 1991;3(2):147–163. [PubMed] [Google Scholar]
- Clement U, Schoennesson LN. Subjective HIV attribution theories, coping, and psychological functioning among homosexual men with HIV. AIDS Care. 1998;10(3):355–363. doi: 10.1080/713612416. [DOI] [PubMed] [Google Scholar]
- Cobb M, DeChabert JT. HIV/AIDS and care provider attributions: Who's to blame? AIDS Care. 2002;14(4):545–548. doi: 10.1080/09540120208629672. [DOI] [PubMed] [Google Scholar]
- Conrad P. The social meaning of AIDS. Social Policy. 1986;17(1):51–56. [Google Scholar]
- Coughlan E, Mindel A, Estcourt CS. Male clients of female commercial sex workers: HIV, STDs and risk behaviour. International Journal of STD and AIDS. 2001;12(10):665–669. doi: 10.1258/0956462011923895. [DOI] [PubMed] [Google Scholar]
- China State Council 2001. China's action plan for reducing and preventing the spread of HIV/AIDS (2001-2005): Unofficial translation of June 25 China AIDS action plan: Ministry of Health Communicable Disease Control Division [Google Scholar]
- Crandall CS. Ideology and lay theories of stigma: The justification of stigmatization. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The social psychology of stigma. Guilford Press; New York, NY: 2000. pp. 126–150. [Google Scholar]
- Crandall CS, Moriarty D. Physical illness stigma and social rejection. British Journal of Social Psychology. 1995;34(1):67–83. doi: 10.1111/j.2044-8309.1995.tb01049.x. [DOI] [PubMed] [Google Scholar]
- Crocker J, Major B, Steele C. Social stigma. In: Gilbert DT, Fiske ST, Lindzey G, editors. The handbook of social psychology. Vol. 2. Oxford University Press; New York, NY: 1998. pp. 504–553. [Google Scholar]
- Crocker J, Quinn DM. Social stigma and the self: Meanings, situations, and self-esteem. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The social psychology of stigma. Guilford Press; New York, NY: 2000. pp. 153–183. [Google Scholar]
- Deaux K, Reid A, Mizrahi K, Ethier KA. Parameters of social identity. Journal of Personality and Social Psychology. 1995;68(2):280–291. [Google Scholar]
- Derlaga VJ, Winstead BA, Greene K, Serovich J, Elwood WN. Perceived HIV-related stigma and HIV disclosure to relationship partners after finding out about the seropositive diagnosis. Journal of Health Psychology. 2002;7(4):415–432. doi: 10.1177/1359105302007004330. [DOI] [PubMed] [Google Scholar]
- Dovidio JF, Major B, Crocker J. Stigma: introduction and overview. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The social psychology of stigma. Guilford Press; New York, NY: 2000. pp. 1–28. [Google Scholar]
- Fife BL, Wright ER. The dimensionality of stigma: A comparison of its impact on the self of persons with HIV/AIDS and cancer. Journal of Health and Social Behavior. 2000;41(1):50–67. [PubMed] [Google Scholar]
- Fortenberry DJ, McFarlane M, Bleakley A, Bull S, Fishbein M, Grimley DM, Malotte CK, Stoner BP. Relationships of stigma and shame to gonorrhea and HIV screening. American Journal of Public Health. 2002;92(3):378–381. doi: 10.2105/ajph.92.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frable DES. Dimensions of marginality: Distinctions among those who are different. Personality and Social Psychology Bulletin. 1993;19(4):370–380. [Google Scholar]
- Frable DES, Platt L, Hoey S. Concealable stigmas and positive self-perceptions. Journal of Personality and Social Psychology. 1998;74(4):909–922. doi: 10.1037//0022-3514.74.4.909. [DOI] [PubMed] [Google Scholar]
- France-Presse China with one million HIV cases, warns of ten-fold increase 2002. September 6France-Presse. Available2002, November 12
- Gan Y-J, Liu S-H. Discussion on discrimination against HIV carriers and AIDS patients by villagers in China [In Chinese] Journal of China AIDS/STD Prevention. 2000;6(4):246–247. [Google Scholar]
- Gil VE. Sinic conundrum: A history of HIV/AIDS in the People's Republic of China. Journal of Sex Research. 1994;31(3):211–217. [Google Scholar]
- Gu L.Health-China: Youngster puts a face on HIV/AIDS 2002. January 29International Press Service. Available2002, April 8
- Herek G, Capitanio JP. AIDS stigma and sexual prejudice. American Behavioral Scientist. 1999;42(7):1130–1147. [Google Scholar]
- Herek GM, Capitanio JP, Widaman KF. HIV-related stigma and knowledge in the United States: prevalence and trends, 1991-1999. American Journal of Public Health. 2002;92(3):371–377. doi: 10.2105/ajph.92.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinman A, Wang W-Z, Li S-C, Cheng X-M. The social course of epilepsy: Chronic illness as social experience in interior China. Social Science and Medicine. 1995;40(10):1319–1330. doi: 10.1016/0277-9536(94)00254-q. [DOI] [PubMed] [Google Scholar]
- Ladany N, Stern M, Inman AG. Medical students' perceptions of and willingness to treat patients who are HIV infected. Journal of Applied Social Psychology. 1998;28(12):1031–1050. [Google Scholar]
- Lamptey PR. Reducing hererosexual transmission of HIV in poor countries. British Medical Journal. 2002;324(7331):207–211. doi: 10.1136/bmj.324.7331.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee M, Wu Z, Detels R, Guan J, Li L, Rotheram-Borus MJ, Group NCHPT.HIV-related stigma among market workers in China 2003University of California; Los Angeles: Manuscript submitted for publication [Google Scholar]
- Lee RS, Kochman A, Sikkema KJ. Internalized stigma among people living with HIV-AIDS. AIDS and Behavior. 2002;6(4):309–319. [Google Scholar]
- Leiker JJ, Taub DE, Gast J. The stigma of AIDS: Persons with AIDS and social distance. Deviant Behavior. 1995;16(4):333–351. [Google Scholar]
- Lieber E, Weisner TS, Presley M. EthnoNotes: An Internet-based fieldnote management tool. Manuscript in press, Field Methods. 2003:1–27. [Google Scholar]
- Liu H, Ma Z, Yu W, Xie J, Detels R. Acceptability of voluntary HIV testing and result disclosure among rural residents of China. Journal of Chinese Preventive Medicine. 2001;35:30–32. [PubMed] [Google Scholar]
- Liu H, Detels R, Li X, Ma E, Yin Y. Manuscript submitted for publication. University of California; Los Angeles: 2003. Stigma, delayed treatment, and spousal notification among male STD patients in China. [Google Scholar]
- Liu H, Xie J, Yu W, Song W, Gao Z, Ma Z, Detels R. A study of sexual behavior among rural residents of China. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1998;19(1):80–88. doi: 10.1097/00042560-199809010-00013. [DOI] [PubMed] [Google Scholar]
- Lupton D, McCarthy S, Chapman S. “Doing the right thing”: The symbolic meanings and experiences of having an HIV antibody test. Social Science and Medicine. 1995;41(2):173–180. doi: 10.1016/0277-9536(94)00317-m. [DOI] [PubMed] [Google Scholar]
- Markus HR, Kitayama S. Culture and the self: Implications for cognition, emotion, and motivation. Psychological Review. 1991;98(2):224–253. [Google Scholar]
- Miller CT, Major B. Coping with stigma and prejudice. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The social psychology of stigma. Guilford Press; New York, NY: 2000. pp. 243–272. [Google Scholar]
- Phillips M.The WPA programme - China 2002. Available2002, November 11
- Phillips MR, Pearson V, Li F, Xu M, Yang L. Stigma and expressed emotion: A study of people with schizophrenia and their family members in China. BritishJournal of Psychiatry. 2002;181(6):488–493. doi: 10.1192/bjp.181.6.488. [DOI] [PubMed] [Google Scholar]
- Rosenthal E.AIDS scourge in rural China leaves villages of orphans New York Times 2002a1Issue Date [Google Scholar]
- Rosenthal E.China raises estimates of HIV-AIDS cases to 1 million New York Times 2002b. Available2002, September 9
- Ruwitch J.China's gay activists cheer new openness on AIDS Reuters 2002. Available2002, November 10
- Smart L, Wegner DM. The hidden costs of hidden stigma. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The social psychology of stigma. Guilford Press; New York, NY: 2000. pp. 220–242. [Google Scholar]
- Stokes JP, Peterson JL. Homophobia, self-esteem, and risk for HIV among African American men who have sex with men. AIDS Education and Prevention. 1998;10(3):278–292. [PubMed] [Google Scholar]
- Super CM, Harkness S. Culture structures the environment for development. Human Development. 2002;45(4):270–274. [Google Scholar]
- Tsang WHH, Yongzhen W, Tam P. Needs and problems related to mental health services in Beijing. Psychiatric Rehabilitation Skills. 2000;4(1):1–21. [Google Scholar]
- Valdiserri RO. HIV/AIDS stigma: An impediment to public health. American Journal of Public Health. 2002;92(3):341–342. doi: 10.2105/ajph.92.3.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward H, Mertens TE, Thomas C. Health seeking behaviour and the control of sexually transmitted disease. Health Policy and Planning. 1997;12(1):19–28. doi: 10.1093/heapol/12.1.19. [DOI] [PubMed] [Google Scholar]
- Weiner B. Judgments of Responsibility: A Foundation for a Theory of Social Conduct. The Guilford Press; New York, NY: 1995. [Google Scholar]
- Weiner B, Perry RP, Magnusson J. An attributional analysis of reactions to stigma. Journal of Personality and Social Psychology. 1988;55(5):738–748. doi: 10.1037//0022-3514.55.5.738. [DOI] [PubMed] [Google Scholar]
- Weitz R. Uncertainty and the lives of persons with AIDS. In: Monat A, Lazuras RS, editors. Stress and coping: An anthology. 3rd Columbia University Press; New York, NY: 1991. pp. 352–369. [Google Scholar]
- WHO Live and let live - World AIDS campaign World Health Organization 2001. Available2002, November 11
- Wu Z, Zhang J, Detels R, Li VC, Cheng H, Duan S, Li Z, Dong L, Huang S, Jia M, Bi X. Characteristics of risk-taking behaviors, HIV and AIDS knowledge, and risk perception among young males in southwest China. AIDS Education and Prevention. 1997;9(2):147–160. [PubMed] [Google Scholar]
- Xiong W, Phillips MR, Hu X, Wang R. Family-based intervention for schizophrenic patients in China: A randomised controlled trial. British Journal of Psychiatry. 1994;165(2):239–247. doi: 10.1192/bjp.165.2.239. [DOI] [PubMed] [Google Scholar]
- Yep GA. HIV/AIDS in Asian and Pacific Islander communities in the U.S.: A review, analysis, and integration. International Quarterly of Community Health Education. 19921993;13(4):293–315. doi: 10.2190/QKJX-WD2T-C2YB-4WWE. [DOI] [PubMed] [Google Scholar]
- Yoshioka MR, Schustack A. Disclosure of HIV status: Cultural issues of Asian patients. AIDS Patient Care and STD's. 2001;15(2):77–82. doi: 10.1089/108729101300003672. [DOI] [PubMed] [Google Scholar]
- Yu ESH, Xie Q, Zhang K.-l. HIV infection and AIDS in China, 1985-1994. American Journal of Public Health. 1996;86(8):1116–1122. doi: 10.2105/ajph.86.8_pt_1.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]