The most common urological complaints that need referral to a primary care doctor or urological surgeon can be divided into those referable to the lower urinary tract and those referable to the upper urinary tract. Although a careful history may be diagnostic in patients with, for example, renal colic or testicular torsion, often non-specific features are more difficult to unravel.
Figure 1.
Recording frequency of micturition on a “time and volume” chart can be useful
Symptoms
The bladder has been described as an unreliable witness. Sensory innervation is mediated largely through parasympathetic nerves, with pain from overdistension mediated through the sympathetic nervous system. The precision with which the site and cause of symptoms in the lower and upper urinary tracts can be identified from this autonomic innervation is limited. Similar symptoms may occur as the result of different pathology. Urological evaluation on the basis of symptoms depends on understanding how much reliance can be placed on the patient's account of symptoms, and on the doctor phrasing questions so that the patient is clear about their meaning.
Table 1.
Urological symptoms
| • Obstructive symptoms |
| • Irritative symptoms |
| • Erectile dysfunction and sexual problems |
| • Urinary incontinence |
| • Pain |
| • Renal colic |
| • Fever |
| • Haematuria |
Obstructive symptoms
Hesitancy of micturition can be a reliable symptom. The patient can quantify accurately a delay in initiation of the urinary stream. Most men can describe whether their urinary stream is fast or slow—that is, strong or weak. Patients can confirm if their urinary stream is intermittent, and this is a good indicator of obstruction. A feeling of incomplete bladder emptying correlates poorly with objective findings on ultrasound examination.
Table 2.
Obstructive symptoms
| • Hesitancy |
| • Poor stream |
| • Intermittent stream |
| • Terminal dribbling |
Irritative symptoms
A burning sensation on micturition is common in patients with a lower urinary tract infection. A similar sensation can occur in the absence of infection, however, and infection can occur in the absence of any discomfort.
Table 3.
Irritative symptoms
| • Burning on micturition |
| • Urgency |
| • Daytime frequency |
| • Nocturia |
| • Urge incontinence |
The term “dysuria” is often applied to a burning sensation on micturition, but it means different things to people and is best avoided. Urgency of micturition may be sensory or motor in origin, but when a history is taken, it is hard to distinguish between the two—although the underlying pathologies are very different. Patients with urgency feel as if they may leak urine if they are not able to reach a lavatory imminently. The sensation of needing to pass urine again just after micturition—strangury—is the urological equivalent of tenesmus. In the urinary tract, the symptom is not diagnostic for any one pathology.
Frequency of micturition
When patients are asked to describe their urinary frequency, they have every opportunity for an unhelpful and lengthy reply. The number of times a patient wakes to pass urine at night is a value that most people can identify accurately. A single episode of nocturia is within normal limits. More than this number becomes increasingly important.
 This article is adapted from the second edition of the ABC of urology (Blackwell Publishing), available from all good medical bookshops, including www.hammicksbma.com
This article is adapted from the second edition of the ABC of urology (Blackwell Publishing), available from all good medical bookshops, including www.hammicksbma.com
Differentiation between urological and non-urological causes of non-specific symptoms can be made only after basic urological investigation
Daytime urinary frequency is subject to so many variables that it is almost unhelpful—except to know whether such frequency provokes an adverse effect on the patient's lifestyle.
Urinary incontinence
To establish the circumstances under which urine loss occurs is important. Neither men nor women are entirely continent. In men, a small urinary leakage at the end of the stream (also known as “post-micturition dribble”) is so common that it does not constitute an abnormality. Many women—young and old—leak a little urine on coughing.
Figure 2.
Male genitalia including scrotal contents. Reproduced from Adler M, et al. ABC of sexually transmitted infections. 5th edition. Oxford: Blackwell Publishing, 2004, and adapted from the Sexually transmitted infections: history taking and examination CD published by the Wellcome Trust, 2003.
The most important question to follow a complaint of urinary incontinence is “What protection do you need to cope with the leakage?” If the loss of urine needs no more than a change of underwear, further investigation is unlikely to be worthwhile, but referral for consideration of pelvic floor exercises may be beneficial to the patient.
Table 4.
Urinary leakage
| • Urinary leakage is more common in women than in men |
| • A severe degree of urge incontinence will probably cause a larger volume of urine loss than the most severe stress incontinence |
| • Some women are unable to identify how they leak |
| • Urinary leakage during sexual intercourse occurs in some women |
Renal and ureteric colic
The pain from a stone that is moving within the urinary tract is among the most severe pains that patients may experience. The site of the pain, however, is not a very reliable indicator of the site of the stone.
Fever
Lower urinary tract infections do not cause a fever, which occurs only when a urinary infection is in a solid organ or if the patient has an obstructed and infected urinary tract.
Sexual dysfunction
Erectile dysfunction presents as an inability to initiate or sustain an erection sufficient to enable vaginal penetration and subsequent orgasm. The presence of nocturnal or early morning erections makes an organic cause of erectile dysfunction less likely.
Retrograde ejaculation occurs commonly in men after transurethral resection of the prostate and sometimes in those who have taken α adrenergic blockers. Failure of ejaculation may occur after sympathectomy or retroperitoneal surgery, as the sympathetic pathways to the prostate and seminal vesicles are interrupted. Premature ejaculation occurs most often as a functional problem.
Examination
Much of the genitourinary tract is hidden from view. This dictates that many decisions on management are usually possible only at a second outpatient visit, when the results of baseline investigations are available.
External genitalia
If a lax scrotum lies between the thighs, the scrotal contents can be delivered painlessly for examination by taking and pulling on a fold of scrotal skin. The testes appear without discomfort. The testes and epididymes can be identified separately.
If epididymal infection is present or testicular torsion is suspected, the examination must be gentle. Observation of the colour of the scrotal wall may reveal hyperaemia. The absence of a cremasteric reflex contraction when the scrotum, or the area close to the scrotum, is touched is also an important sign to elicit. The loss of this reflex is not diagnostic of one pathology, but its presence is strongly against a diagnosis of torsion.
Examination of the penis should include assessment of the degree to which the prepuce can be retracted. The external urethral meatus must be identified: in patients with hypospadias and epispadias, the meatus will be sited abnormally. If an attempt is made to pull the sides of the meatus apart, the presence of meatal stenosis can be identified. The shaft of the penis is palpated to identify fibrous plaques of Peyronie's disease, which usually are found dorsally.
When a stone enters the intramural ureter, patients often describe strangury, and, in men, discomfort may be felt at the tip of the penis
If a urinary tract infection is suspected the presence of nitrites and red cells on dipstick testing can be useful, although not unequivocal, confirmatory evidence
Ideally, antibiotics should not be prescribed until a urine culture has been taken
The patient's external genitalia should be examined with the patient in the supine and erect positions to identify pathologies such as hernia and varicocele
Rectal examination
Rectal examination is performed best with the patient in the left lateral position. The examiner's finger should be inserted while the patient exhales to encourage maximum relaxation of the anal sphincter. The tone of the anal sphincter is noted. Perianal sensation can be tested in the distribution of the S2, S3, and S4 segments—the spinal segments responsible for the main motor and sensory innervation of the bladder.
Figure 3.
S2, S3, and S4 segments are responsible for the main motor and sensory innervation of the bladder
Table 5.
Rectal examination
| • Anal sphincter tone |
| • Anal sphincter contractility |
| • Perianal sensation |
| • Prostate—size, surface, symmetry, and consistency |
Examination of the prostate per rectum provides only a rough estimate of the size: the prostate can be categorised as small, medium, or large. The consistency of the prostate can be described as soft, firm, or hard; the surface as smooth or irregular; and the lateral lobes as symmetrical or asymmetrical. No precise correlation exists between any of the features described and a specific pathology.
Figure 4.
Renal ultrasound scan showing pelvi-caliceal and upper ureteric dilatation
Table 6.
Initial investigations
| • Urine culture |
| • Urine cytology |
| • Biochemistry |
| • Ultrasonography |
| • Urodynamics |
| • Radiology |
| • Nuclear medicine |
Initial investigations
Dipstick urine testing
Although it is readily available and often used, dipstick testing of urine is an inaccurate investigation. The presence of white cells and nitrites is a rough guide to the presence of infection, although the absence of nitrites in the urine normally is enough to rule out an infection and the need for urine microscopy. Microscopic haematuria may be intermittent, but the presence of blood cells in the urine should normally prompt referral for further investigation, and it is considered unnecessary to confirm the presence of red cells by urine microscopy.
Urine culture
Many laboratories now use an automated method to identify red and white cells in the urine. The numbers of each that can be considered normal are considerably higher than the numbers regarded as normal when urine microscopy is used. These values must be recognised, particularly for red cells, to prevent inappropriate referrals.
Urine cytology
Although some automation is used for the analysis of urine cytology, the final arbiter is microscopy—the accuracy of which depends on the expertise of the cytopathologist.
Biochemistry
Renal function is measured better by serum creatinine than by blood urea, the latter being influenced by the degree of hydration and rate of metabolism. The extent of reserve renal function means there must be a loss of two thirds of overall renal function before levels of serum creatinine increase. Measurements of sodium, potassium, and chloride electrolytes are the other baseline biochemical tests of relevance.
Ultrasonography
Ultrasound examinations are used in the investigation of renal, ureteric, bladder, prostatic, and scrotal pathology. They may be regarded as an extension of examination. The person who undertakes the examination has the advantage of seeing the images in real time, whereas the doctor has only a few still images. The report thus is of prime importance. Limitations of ultrasonography vary in different situations.
Kidney
In the kidney, ultrasound is better than computed tomography at identifying renal cysts, but it may fail to distinguish between parapelvic cysts and hydronephrosis. Ultrasound is a poor way of screening for renal stones. Assessment of the size of a stone using ultrasound is not very accurate.
Culture of a midstream specimen of urine is the only way to identify patients whose symptoms truly result from infection
Ureter
Ureteric dilatation can be identified, but the cause is much more difficult to define. A stone at the lower end of the ureter may be identified by using the full bladder as an acoustic window.
Figure 5.
Ultrasound scan showing dilated ureter
Bladder
The bladder is seen easily on transabdominal ultrasound, and volume measurements are simple and accurate. Intravesical pathology, such as tumours and stones, can be seen best when the bladder is full.
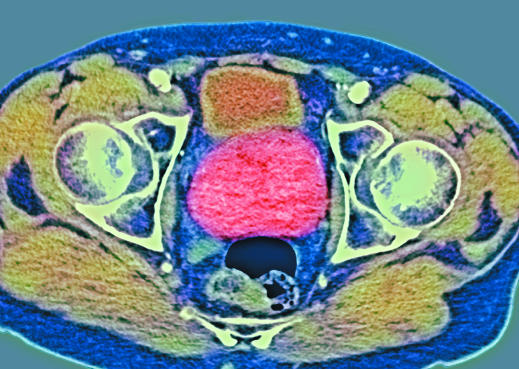
Figure 6.
Axial coloured magnetic resonance image scan of a patient with prostate cancer. With permission from Du Cane Medical Imaging Ltd/Science Photo Library
Prostate
Transrectal ultrasonography of the prostate has transformed the understanding of prostatic anatomy and pathology. Biopsies of the prostate and placement of radioactive seeds in brachytherapy are always undertaken with ultrasound imaging.
Table 7.
Radiological investigations
| • Plain abdominal x ray |
| • Intravenous urogram |
| • Urethrogram |
| • Retrograde ureterogram |
| • Antegrade ureterogram |
| • Computed tomography |
| • Magnetic resonance imaging |
| • Isotope renogram |
| • Isotopic glomerular filtration rate |
| • Isotope bone scan |
Scrotum
The scrotal contents are one of the few sites in urological practice where examination is easy. Differentiation between the normal epididymis and testis is accurate, and the vas can be palpated. In the presence of a tense hydrocele or inflammation, examination becomes more difficult and ultrasound may be worthwhile.
Urodynamics
Urodynamic investigations of the upper urinary tract are not often performed. Assessment of the function of the lower urinary tract can be made by a number of investigations:
Urinary flow rate
Assessment of bladder capacity and the size of the residual urine volume
Measurement of bladder pressures with a urethral catheter during bladder filling and emptying
Pressure or flow assessment under fluoroscopic imaging.
Radiological investigation
The methods of radiological investigation include those listed in the box above and each are used in different situations.
Intravenous urography (combined with renal ultrasonography) is the investigation of choice for patients with painless haematuria. New low osmolarity contrast media causes severe allergic reactions in < 0.02% of patients.
Computed tomography is the investigation of choice for identifying renal masses. The speed of the investigation has advantages, but interpreting the images needs a considerable investment in time at a sophisticated workstation that can format the images.
Magnetic resonance imaging has been adopted as the investigation of choice in the staging of prostate cancer. The same investigation can be helpful if used on bone settings to interpret areas of increased isotope uptake on a bones scan.
Dynamic isotope renography that uses mercaptoacetylglycine (MAG3) as the radiopharmaceutical is the most accurate method of identifying upper urinary tract obstruction and also shows differential renal function.
Static renography with dimercaptosuccinic acid (DMSA) will identify renal scarring and differential renal function.
The most accurate measurement of glomerular filtration rate is obtained by using an ethylenediamine tetra-acetic acid (EDTA) clearance technique.
Isotope bone scans are used in uro-oncology to identify bony metastatic disease.
The ABC of urology is edited by Hugh N Whitfield, consultant urological surgeon, Royal Berkshire Hospital, Reading, and Chris Dawson, consultant urologist, Edith Cavell Hospital, Peterborough. The book will be published in September 2006.
Competing interests: None declared.