Abstract
Objective:
The presence of posttraumatic amnesia (PTA) and loss of consciousness have been main factors used in a number of concussion guidelines. In this article, the focus is on using PTA (both retrograde and anterograde) as salient indicators of traumatic brain injury severity and the most reliable index of outcome prediction, even in mild cases.
Data Sources:
A MEDLINE search for the years 1990–2000 using the key words posttraumatic retrograde and anterograde amnesia, concussion and mild traumatic brain injury was done.
Data Synthesis:
On-the-field testing of PTA is a salient and integral component of the initial and follow-up neurologic assessments of the head-injured athlete.
Conclusions/Recommendations:
Initial and follow-up assessments of PTA, anterograde and retrograde, are an essential part of the neurologic evaluation of the head-injured athlete. Increasingly, neuropsychological testing, including computer models, is being employed in this assessment. The importance of not just PTA but all postconcussion signs and symptoms being absent at rest and exertion before allowing the athlete to return to play is emphasized.
Keywords: concussion, mild traumatic brain injury, athletic injury
Concussion is derived from the Latin word concussus, which means to shake violently. Initially, it was thought to produce only a temporary disturbance of brain function due to neuronal, chemical, or neuroelectrical changes without gross structural change. We now know that structural damage with loss of brain cells does occur with some concussions. In the last several years, the neurobiology of cerebral concussion has been advanced predominantly in animal studies but also in studies in man as well. It has become clear that, in the minutes to days after concussive brain injury, brain cells that are not irreversibly destroyed remain alive but in a vulnerable state. These cells are particularly vulnerable to minor changes in cerebral blood flow, increases in intracranial pressure, and especially anoxia. Animal studies have shown that, during this period of vulnerability, which may last as long as a week with a minor head injury such as a concussion, a minor reduction in cerebral blood flow that would normally be well tolerated now produces extensive neuronal cell loss.1–5 This vulnerability appears to be due to an uncoupling of the demand for glucose, which is increased after injury, with a relative reduction in cerebral blood flow. While the precise mechanisms of this dysfunction are still not fully understood, it is now clear that, although concussion in and of itself may not produce extensive neuronal damage, the surviving cells are in a state of vulnerability characterized by a metabolic dysfunction, which can be thought of as a breakdown between energy demand and production. Precisely how long this period of metabolic dysfunction lasts is not presently fully understood. Unfortunately, there are today no neuroanatomic or physiologic measurements that can be used to precisely determine the extent of injury in concussion or the severity of metabolic dysfunction or precisely when it has cleared. It is this fact that makes return-to-play decisions after a concussion a clinical judgment.
Team physicians, athletic trainers, and other medical personnel responsible for the medical care of athletes face no more challenging problem than the recognition and management of concussion. Indeed, such injuries have captured many headlines in recent years and have spurred studies within both the National Football League and the National Hockey League.
When discussing concussion, we must realize that there is no universal agreement on the definition and grading of concussion.1,6–8 Tables 1–8 present different attempts at grading concussion, all focusing on loss or nonloss of consciousness and posttraumatic amnesia (PTA) as hallmarks in the grading schemes. Furthermore, they may not give enough attention to the other signs and symptoms of concussion. As we all know, a patient with concussion may display any combination of the following signs and symptoms: a feeling of being stunned or seeing bright lights, brief loss of consciousness, lightheadedness, vertigo, loss of balance, headaches, cognitive and memory dysfunction, tinnitus, blurred vision, difficulty concentrating, lethargy, fatigue, personality changes, inability to perform daily activities, sleep disturbances, and motor or sensory symptoms.
Table 1.
Cantu Grading System for Concussion9*

Table 8.
Torg Grading System for Concussion13

Table 2.
Colorado Medical Society Grading System for Concussion10

Table 3.
AAN Practice Parameter (Kelly and Rosenberg) Grading System for Concussion6

Table 4.
Jordan Grading System for Concussion11

Table 5.
Ommaya Grading System for Concussion12

Table 6.
Nelson Grading System for Concussion7

Table 7.
Roberts Grading System for Concussion8

Presently, there is no universal agreement that PTA is a better or more sensitive predictor of outcome after traumatic brain injury than depth and duration of unconsciousness,14–16 but many consider the duration of PTA the best indicator of traumatic brain injury severity15,17 and the most dependable marker of outcome prediction,18–25 even in mild cases.16,26 While variously described by different investigators, PTA includes impaired orientation, that is, retrograde amnesia and anterograde amnesia.22,27–29 Recently, some investigators16,30–32 have suggested that PTA might better be called posttraumatic confusional state.
Posttraumatic amnesia may be divided into 2 types. The first type of PTA is retrograde, defined by Cartlidge and Shaw23 as a “partial or total loss of the ability to recall events that have occurred during the period immediately preceding brain injury.” The duration of retrograde amnesia usually progressively decreases. The second type of PTA is anterograde amnesia, a deficit in forming new memory after the accident, which may lead to decreased attention and inaccurate perception. Anterograde memory is frequently the last function to return after the recovery from loss of consciousness.33
Memory and new learning are believed to involve the cerebral cortex, subcortical projections, hippocampal formation (gyrus dentatus, hippocampus, and parahippocampal gyri), and the diencephalons, especially the medial portions of the dorsomedial and adjacent midline nuclei of the thalamus.34 In addition, frontal lobe lesions may cause alterations in behavior, including irritability, aggressiveness, and loss of inhibition and judgment. Recently, evidence has been presented that the right frontal lobe plays a prominent role in sustained attention.35
The lack of a universal definition or grading scheme for concussion renders the evaluation of epidemiologic data extremely difficult. As a neurosurgeon and team physician, I have evaluated many football players who suffered a concussion. Most of these injuries were mild, not involving loss of consciousness, and were associated with PTA, which was helpful in making the diagnosis, especially in mild cases.
I developed a practical scheme for grading concussion severity based on the duration of unconsciousness or PTA (or both), which has worked well on the field and sideline (see Table 1). The most mild concussion (grade 1) occurs without loss of consciousness, and the only neurologic deficit is a brief period of posttraumatic confusion or PTA, which, by definition, lasts less than 30 minutes. The moderate (grade 2) concussion is usually associated with a brief period of unconsciousness, by definition, not exceeding 5 minutes. Less commonly, consciousness is not lost; the athlete instead experiences a protracted period of PTA lasting more than 30 minutes but less than 24 hours. A severe (grade 3) concussion occurs with a more protracted period of unconsciousness lasting longer than 5 minutes. Rarely, it may occur without a loss of consciousness or with a shorter period of unconsciousness but with a very protracted period of PTA lasting more than 24 hours. In reality, prospective studies over the last several years have shown that virtually all concussions are grade 3 by this guideline because of PTA lasting longer than 24 hours (D. Erlanger, unpublished data, 2000). A protracted period of unconsciousness lasting more than 5 minutes is almost never seen on athletic fields; most periods of unconsciousness last seconds to a minute. Prospective studies over the last 10 years have demonstrated a correlation between the duration of postconcussive symptoms and PTA and abnormal results on neuropsychological tests. Therefore, I present an evidence-based modification of the original Cantu guidelines9 (Table 9).
Table 9.
Evidence-Based Cantu Grading System for Concussion

When checking for orientation and retrograde amnesia on the field, asking the athlete the current quarter, the score, what happened, and the names of the current and last week's opponents is useful. When checking for attention or anterograde amnesia deficits, useful tests are repeating 4 words immediately and 2 minutes later, repeating 5 numbers forward and especially backward, and repeating months of the year backward.
Recently, computer-administered minineuropsychological tests have been proposed as a more feasible way to conduct group baseline assessments,36,37 as well as a personal digital assistant version that can be connected to the Internet.38,39
Thus, while not yet the standard of care, neuropsychological tests (with a preseason baseline and serial postconcussion assessments) are assisting clinicians in concussion management, including return-to-play decisions.
Whether an athlete has been unconscious is, of course, important. It is generally believed that the degree of brain injury sustained is indicated by the depth and duration of coma.40–42 However, the coma referred to by these authors is not the seconds to minutes usually seen on the athletic field but rather hours' or days' duration. Thus, while not diminishing the importance of being rendered unconscious, I find it illogical to grade a concussion that produces postconcussion symptoms lasting months or years without loss of consciousness as less severe than a concussion resulting in brief unconsciousness and resolution of all postconcussion symptoms within a few minutes or hours. Brett Lindros, Al Toon, Jim Miller, Steve Young, and Merrill Hodge are professional athletes whose careers were ended by concussions without loss of consciousness that produced sustained postconcussion symptoms. We know these athletes consider their concussions very severe.
RETURN TO COMPETITION AFTER CONCUSSION
A sobering realization is that the ability to process information may be reduced after a concussion, and the severity and duration of functional impairment may be greater with repeated concussions.43–45 Studies clearly suggest that the damaging effects of the shearing injury to nerve fibers and neurons are proportional to the degree to which the head is accelerated and that these changes may be cumulative.46–48 Once a player has incurred an initial cerebral concussion, his or her chances of incurring a second one are 3 to 6 times greater than for an athlete who has never sustained a concussion.48–51
Table 10 presents guidelines for return to play after a concussion, including termination of a season. Before an athlete returns to play, he or she must not only be free of PTA symptoms but also of all postconcussion symptoms at rest and exertion. All the guidelines agree on this salient point. Table 11 is a postconcussion signs and symptoms checklist I have found useful. Thus, while it is a clinical decision as to when to return an athlete to play after a concussion, to return an athlete with postconcussion symptoms risks not only cumulative brain injury but the second-impact syndrome and would be against the recommendations of all current guidelines.
Table 10.
Guidelines for Return to Play After Concussion*
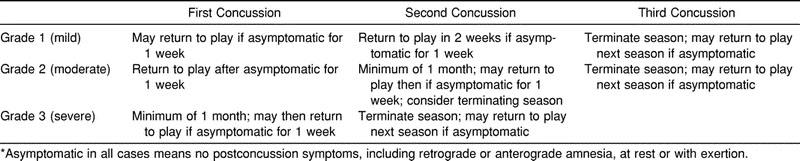
Table 11.
Postconcussion Signs and Symptoms Checklist

CONCLUSION
There is no universal agreement on concussion grading and return-to-play criteria after a concussion. There is, however, unanimous agreement that an athlete still suffering postconcussion symptoms at rest and exertion should not return to contact or collision sports. In this article, I present the logic for using the duration of posttraumatic amnesia (retrograde and especially anterograde) as a criterion to be employed in the grading of concussion severity.
REFERENCES
- 1.Jenkins LW, Marmarou A, Lewelt W, Becker DP. Increased vulnerability of the traumatized brain to early ischemia. In: Baethmann A, Go KG, Unterberg A, editors. Mechanisms of Secondary Brain Damage. New York, NY: Perseus Books; 1986. pp. 273–282. [Google Scholar]
- 2.Jenkins LW, Moszynski K, Lyeth BG, et al. Increased vulnerability of the mildly traumatized brain to cerebral ischemia: the use of controlled secondary ischemia as a research tool to identify common or different mechanisms contributing to mechanical and ischemic brain injury. Brain Res. 1989;477:211–224. doi: 10.1016/0006-8993(89)91409-1. [DOI] [PubMed] [Google Scholar]
- 3.Lee SM, Lifshitz J, Novda DA, Becker DP. Focal cortical-impact injury produces immediate and persistent deficits in metabolic autoregulation [abstract] J Cereb Blood Flow Metab. 1955;7:22. [Google Scholar]
- 4.Lifshitz J, Pinanong P, Le HM, et al. Regional uncoupling of cerebral blood flow and metabolism in degenerating cortical areas following a lateral cortical contusion [abstract] J Neurotrauma. 1955;12:129. [Google Scholar]
- 5.Sutton RL, Hovda DA, Adelson PD, Benzel BC, Becker DP. Metabolic changes following cortical contusion: relationships to edema and morphological changes. Acta Neurochir Suppl (Wien) 1994;60:446–448. doi: 10.1007/978-3-7091-9334-1_122. [DOI] [PubMed] [Google Scholar]
- 6.Kelly JP, Rosenberg JH. The diagnosis and management of concussion in sports. Neurology. 1997;48:575–580. doi: 10.1212/wnl.48.3.575. [DOI] [PubMed] [Google Scholar]
- 7.Nelson WE, Jane JA, Gieck JH. Minor head injury in sports: a new system of classification and management. Physician Sportsmed. 1984;12(3):103–107. [Google Scholar]
- 8.Roberts WO. Who plays? Who sits? Managing concussions on the sidelines. Physician Sportsmed. 1992;20(6):66–76. doi: 10.1080/00913847.1992.11710295. [DOI] [PubMed] [Google Scholar]
- 9.Cantu RC. Guidelines for return to contact sports after a cerebral concussion. Physician Sportsmed. 1986;14(10):75–83. doi: 10.1080/00913847.1986.11709197. [DOI] [PubMed] [Google Scholar]
- 10.Report of the Sports Medicine Committee. Guidelines for the Management of Concussion in Sports. Denver, CO: Colorado Medical Society; 1990. revised May 1991. [Google Scholar]
- 11.Jordan BJ, Tsairis PT, Warren RF, editors. Sports Neurology. Gaithersburg, MD: Aspen Publishers; 1989. p. 227. [Google Scholar]
- 12.Ommaya AK. Biomechanics of head injury: experimental aspects. In: Nahum AM, Melvin J, editors. Biomechanics of Trauma. Norwalk, CT: Appleton & Lange; 1985. pp. 245–269. [Google Scholar]
- 13.Torg JS. Athletic Injuries to the Head, Neck, and Face. St Louis, MO: Mosby-Year Book; 1991. p. 226. [Google Scholar]
- 14.Alexandre A, Colombo F, Nertempi P, Benedetti A. Cognitive outcome and early indices of severity of head injury. J Neurosurg. 1983;59:751–761. doi: 10.3171/jns.1983.59.5.0751. [DOI] [PubMed] [Google Scholar]
- 15.Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 16.Stuss DT, Binns MA, Carruth FG, et al. The acute period of recovery from traumatic brain injury: posttraumatic amnesia or posttraumatic confusional state? J Neurosurg. 1999;90:635–643. doi: 10.3171/jns.1999.90.4.0635. [DOI] [PubMed] [Google Scholar]
- 17.Jennett B, MacMillan R. Epidemiology of head injury. Br Med J (Clin Res Ed) 1981;282:101–104. doi: 10.1136/bmj.282.6258.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bishara SN, Partridge FM, Godfrey HPD, Knight PG. Post-traumatic amnesia and Glasgow Coma Scale related to outcome in survivors in a consecutive series of patients with severe closed-head injury. Brain Inj. 1992;6:373–380. doi: 10.3109/02699059209034952. [DOI] [PubMed] [Google Scholar]
- 19.Brooks DN, Aughton ME, Bond MR, Jones P, Rizvi S. Cognitive sequelae in relationship to early indices of severity of brain damage after severe blunt head injury. J Neurol Neurosurg Psychiatry. 1980;43:529–534. doi: 10.1136/jnnp.43.6.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brooks DN, Hosie J, Bond MR, Jennett B, Aughton ME. Cognitive sequelae of severe head injury in relation to the Glasgow Outcome Scale. J Neurol Neurosurg Psychiatry. 1986;49:549–533. doi: 10.1136/jnnp.49.5.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haslam C, Batchelor J, Fearnside MR, Haslam SA, Hawkins S, Kenway E. Post-coma disturbance and post-traumatic amnesia as nonlinear predictors of cognitive outcome following severe closed head injury: findings from the Westmead Head Injury Project. Brain Inj. 1994;8:519–528. doi: 10.3109/02699059409151004. [DOI] [PubMed] [Google Scholar]
- 22.Shores EA. Comparison of the Westmead PTA Scale and Glasgow Coma Scale as predictors of neuropsychological outcome following extremely severe closed head injury. J Neurol Neurosurg Psychiatry. 1989;52:126–127. doi: 10.1136/jnnp.52.1.126-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cartlidge NEF, Shaw DA. Head Injury. London, England: WB Saunders; 1981. [Google Scholar]
- 24.Evans CD. Assessment of disability after head injury. Rheumatol Rehabil. 1976;15:168–169. doi: 10.1093/rheumatology/15.3.168. [DOI] [PubMed] [Google Scholar]
- 25.Gillingham FJ. The importance of rehabilitation. Injury. 1969;1:142. [Google Scholar]
- 26.Crovitz HF, Horn RW, Daniel WF. Inter-relationships among retrograde amnesia, post-traumatic amnesia, and time since head injury: a retrospective study. Cortex. 1983;19:407–412. doi: 10.1016/s0010-9452(83)80009-4. [DOI] [PubMed] [Google Scholar]
- 27.Daniel WF, Crovitz HF, Weiner RD. Neuropsychological aspects of disorientation. Cortex. 1987;23:169–187. doi: 10.1016/s0010-9452(87)80030-8. [DOI] [PubMed] [Google Scholar]
- 28.Geffen GM, Encel JS, Forrester GM. Stages of recovery during post-traumatic amnesia and subsequent everyday memory deficits. Neuroreport. 1991;2:105–108. doi: 10.1097/00001756-199102000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Levin HS, O'Donnell VM, Grossman RG. The Galveston Orientation and Amnesia Test: a practical scale to assess cognition after head injury. J Nerv Ment Dis. 1979;167:675–684. doi: 10.1097/00005053-197911000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Alexander MP. Traumatic brain injury. In: Benson DF, Blumer D, editors. Psychiatric Aspects of Neurologic Disease. New York, NY: Grune & Stratton; 1982. pp. 219–248. [Google Scholar]
- 31.Katz DI. Neuropathology and neurobehavioral recovery from closed head injury. J Head Trauma Rehabil. 1992;7:1–15. [Google Scholar]
- 32.Benson DF, Gardner H, Meadows JC. Reduplicative paramnesia. Neurology. 1976;26:147–151. doi: 10.1212/wnl.26.2.147. [DOI] [PubMed] [Google Scholar]
- 33.Russell WR. Cerebral involvement in head injury: a study based on the examination of two hundred cases. Brain. 1932;55:549. [Google Scholar]
- 34.Adams RD, Victor M, Ropper AJ. Principles of Neurology. 6th ed. New York, NY: McGraw-Hill; 1997. p. 427. [Google Scholar]
- 35.Stuss DT, Shallice T, Alexander MP, Picton TW. A multidisciplinary approach to anterior attentional functions. Ann NY Acad Sci. 1995;769:191–211. doi: 10.1111/j.1749-6632.1995.tb38140.x. [DOI] [PubMed] [Google Scholar]
- 36.Maroon JC, Lovell MR, Norwig J, Podell K, Powell JW, Hartl R. Cerebral concussion in athletes: evaluation and neuropsychological testing. Neurosurgery. 2000;47:659–672. doi: 10.1097/00006123-200009000-00027. [DOI] [PubMed] [Google Scholar]
- 37.Bleiberg J, Halpern EL, Reeves D, Daniel JC. Future directions for the neuropsychological assessment of sports concussion. J Head Trauma Rehabil. 1998;13:36–44. doi: 10.1097/00001199-199804000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Erlangler DM, Feldman DJ, Theodoracopilus FL, et al. Development and validation of a Web-based protocol for management of sports related concussion. Paper presented at: National Academy of Neuropsychology; November 16, 2000; Orlando, FL. [Google Scholar]
- 39.Bleiberg J, Reeves D, Kane RL, Garmoe W. The National Rehabilitation Hospital Mild Brain Dysfunction Automated Neuropsychological Assessment Metrics (NRHMBD-ANAM) Washington, DC: National Rehabilitation Hospital; 2000. [Google Scholar]
- 40.Carlsson CA, Von Essen C, Lofgren J. Factors affecting the clinical course of patients with severe head injuries, Part I, Influence of biological factors; Part II, Significance of post-traumatic coma. J Neurosurg. 1968;29:242–251. doi: 10.3171/jns.1968.29.3.0242. [DOI] [PubMed] [Google Scholar]
- 41.Gilchrist E, Wilkinson M. Some factors determining prognosis in young people with severe head injuries. Arch Neurol. 1979;36:355–359. doi: 10.1001/archneur.1979.00500420065008. [DOI] [PubMed] [Google Scholar]
- 42.Stover SL, Zeiger HE., Jr Head injury in children and teenagers; functional recovery correlated with the duration of coma. Arch Phys Med Rehabil. 1976;57:201–205. [PubMed] [Google Scholar]
- 43.Gronwall D, Wrightson P. Delayed recovery of intellectual function after minor head injury. Lancet. 1974;2:605–609. doi: 10.1016/s0140-6736(74)91939-4. [DOI] [PubMed] [Google Scholar]
- 44.Gronwall D, Wrightson P. Cumulative effect of concussion. Lancet. 1975;2:995–997. doi: 10.1016/s0140-6736(75)90288-3. [DOI] [PubMed] [Google Scholar]
- 45.Symonds C. Concussion and its sequelae. Lancet. 1962;1:1–5. [Google Scholar]
- 46.Gennarelli TA, Seggawa H, Wald U, et al. Physiological response to angular acceleration of the head. In: Grossman RG, Gildenberg PL, editors. Head Injury: Basic and Clinical Aspects. New York, NY: Raven Press; 1982. pp. 129–140. [Google Scholar]
- 47.Peerless SJ, Rewcastle NB. Shear injuries of the brain. Can Med Assoc J. 1967;96:577–582. [PMC free article] [PubMed] [Google Scholar]
- 48.Schneider RC, Kennedy JC, Plant ML. Sports Injuries. Baltimore, MD: Williams & Wilkins; 1985. [Google Scholar]
- 49.Guskiewicz KM, Weaver NL, Padua DA, Garrett WE., Jr Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28:643–650. doi: 10.1177/03635465000280050401. [DOI] [PubMed] [Google Scholar]
- 50.Zemper E. Analysis of cerebral concussion frequency with the most commonly used models of football helmets. J Athl Train. 1994;29:44–50. [PMC free article] [PubMed] [Google Scholar]
- 51.Gerberich SG, Priest JD, Boen JR, Straub CP, Maxwell RE. Concussion incidences and severity in secondary school varsity football players. Am J Public Health. 1983;73:1370–1375. doi: 10.2105/ajph.73.12.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]


