Abstract
Objective:
To provide historical background and current concepts regarding the importance of loss of consciousness (LOC) in the evaluation of concussion and athletes.
Data Sources:
A MEDLINE search identified scientific and clinical articles on sport concussion management published from 1966 to present. Discussions were held with authors of selected reports. Recent research findings reported at national meetings were reviewed.
Data Synthesis:
The relative importance of LOC in the evaluation of concussion was reviewed in light of scientific and clinical evidence in the literature. Comments made by authors of concussion grading scales were considered in the development of expert consensus statements.
Conclusions/Recommendations:
The observation of LOC at the time of concussion must be viewed as reflecting a potentially worrisome traumatic brain injury. LOC is followed by more severe acute mental status abnormalities and carries a greater risk of intracranial pathology than concussion without LOC. Prolonged LOC represents a neurologic emergency, which may require neurosurgical intervention. Lingering symptoms of concussion, even without LOC, should be monitored closely and managed according to established guidelines for safe return to play.
Keywords: concussion, mild traumatic brain injury, sport concussion guidelines
Does an athlete's loss of consciousness (LOC) affect the management of sport-related concussion? Increasing attention surrounds the issue of concussion in sports and recreation in the medical literature,1 as evidenced by the devotion of this entire issue of the Journal of Athletic Training to the topic. I will attempt to address the question, “In mild traumatic brain injury (MTBI), or more specifically, sport-related cerebral concussion, what is the importance of LOC?”
It is important to correct a common misconception that concussion only occurs if an individual is rendered unconscious. Health care professionals know that concussions often occur without LOC—especially in the world of athletics.2 Temporary confusion or even a permanent gap in memory (posttraumatic amnesia or PTA) can occur without LOC.3 This is true for concussion that occurs in any setting, not only in sports and recreation. While the focus of this article is concussion during athletic activity, any past medical history of concussion outside the sports arena must be considered when health care professionals make decisions regarding return to participation in sports.
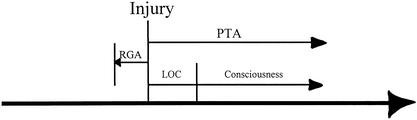
When an individual sustains a concussion with amnesia, he or she often later assumes that there was a LOC; however, it is important for the health care professional to determine whether LOC actually occurred. An individual who has amnesia associated with the injury cannot observe himself or herself and is, by definition, an unreliable historian regarding the event itself. Anyone rendered unconscious also has an associated amnesia, both for the period of time while unconscious and also for some span of time thereafter, before an awareness of the surroundings and events returns (Figure). A brief period of memory loss or retrograde amnesia is common following LOC and sometimes occurs even without LOC.4
Time course of concussion. RGA = retrograde amnesia, LOC = loss of consciousness, PTA = posttraumatic amnesia.
Concussion is diagnosed by determining what actually happened to the individual's brain function at the time of the injury.2 This diagnosis is not made by neuroimaging studies, such as computed tomography (CT) scanning or magnetic resonance imaging (MRI) scanning, nor is it made by neuropsychological testing performed days or weeks later. The examination of the athlete at the time of the injury or detailed accounts of the signs and symptoms at the time of the injury are much more valuable in formulating a diagnosis of concussion. In the sport setting, eyewitness reports or videotape evidence of the injury are often available and helpful in the neurologic assessment of the athlete.
Pathophysiology of Loss of Consciousness
It is important to distinguish between unconsciousness from a neurologic cause and other uses of the term “unconsciousness” in psychology or philosophy. Whereas psychological unconsciousness refers to a state of unawareness or repressed ideas,5 neurologic unconsciousness is paralytic coma.6 This neurologic state represents a form of brain dysfunction involving either the hemispheres or the deep structures of the brain (including the reticular activating system, which governs sleep and wake cycles7), or both. In the neurologic unconscious state, responses to the external world are primitive or reflexic and may be absent altogether. After severe traumatic brain injury, emergence from a coma into vegetative state does not change the fact that the individual is still unconscious, even though the eyes may be open. Only in the somewhat higher level of function known as the minimally conscious state do we see the beginning of neurologic consciousness and higher-level behaviors indicating an awareness of the external world.8
The Glasgow Coma Scale (GCS)9 was created to assess the depth of coma from traumatic causes of unconsciousness. Early in the establishment of this scale and the associated Glasgow Outcome Scale (GOS),10 it became clear that deeper levels of coma as measured by lower scores on the GCS typically carry a worse prognosis and poorer outcome on the GOS in adults11 and children.12 Lower GCS scores are associated with longer PTA,13 and several studies have shown PTA to be the best single predictor of outcome from all severities of traumatic brain injury.14,15
From decades of animal experiments and human experience with traumatic brain injury, we know that concussion commonly occurs without LOC.6,16,17 Periods of brief unconsciousness may be associated with concussion. Unconsciousness lasting longer than 30 minutes is thought to indicate a more serious form of brain injury than concussion.18
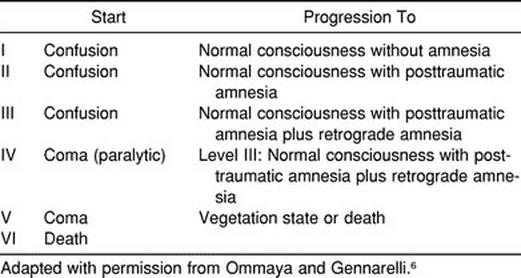
Important experimental animal work nearly 30 years ago by Ommaya and Gennarelli6 demonstrated that 3 of 6 grades of traumatic brain injury severity could be determined with milder forms of brain injury not involving LOC (Table 1). The mildest form was that of transient confusion without LOC or amnesia. The second grade included confusion plus PTA without unconsciousness. The third grade included confusion and PTA plus retrograde amnesia, again without LOC. Grades IV through VI involve LOC associated with progressively worse neurologic outcomes. Within each of these grades, shearing strains on brain tissue produced lesions that were detected near the cortical surface in milder cases, while deeper lesions within the brain were associated with more severe biomechanical forces.
Table 1.
Scale of Severity of Traumatic Brain Injury Not Involving Loss of Consciousness
Neuroimaging studies such as MRI19 and CT20 scans are known to detect traumatic lesions within the brain, MRI scans being more sensitive than CT scans.21,22 Individuals who are not rendered unconscious by head trauma are less likely to have subcortical contusions than those who are rendered unconscious.20 The longer the period of unconsciousness, the deeper the location of the lesions detected by CT23 and MRI scan.20 In cases of relatively mild traumatic brain injury, focal lesions on CT or MRI scans predict worse outcome.13,16 Brain lesions due to trauma have well-described neurobehavioral manifestations, some of which are seen during acute concussion as a result of diffuse damage primarily affecting frontal lobe functions, such as organization of thinking, information processing, decision making, planning, and carrying out complex tasks.24
External forces that affect head movement cause mechanical stress within the brain tissue, producing a sudden electric discharge or depolarization of nerve cells throughout the brain.25 LOC can occur from this effect alone. This electric depolarization leads to an outpouring of neurotransmitters in the brain, and a cascade of neurochemical changes results in excitatory and damaging effects on the nerve cells. The subsequent metabolic rearrangement can be measured by sophisticated functional neuroimaging techniques such as positron emission tomography (PET) scanning.26
High-powered electron microscopes have been used to analyze changes in brain tissue after mild traumatic forces have been applied.27 If these experimental animals are sacrificed immediately after the application of the traumatic force, the nerve cell projections known as axons appear normal; however, if the animal is allowed to survive the injury for several hours, axonal swelling and later degeneration occur. Neurochemical28 and structural changes,29,30 followed by the delayed effects of diffuse axonal injury,27 are known to occur with mild traumatic brain injury. Even so, it is not clear whether the mildest form of concussion, such as that producing transient confusion without amnesia, leads to these anatomical changes.
Studies of cerebral glucose metabolism in human traumatic brain injury have failed to show a relationship between LOC and metabolic perturbations that follow the injury. Glucose metabolism of patients who had sustained concussion but are fully alert at the time of PET scanning is not significantly different than those who are comatose at the time of the testing.26 However, we may be underestimating the amount of time the brain needs to recover from concussion because even after mild traumatic brain injury, metabolic derangements require about 10 days to resolve.31
Neuropsychological testing is our most sensitive measure of cognitive dysfunction after concussion, and it is the most useful method of determining readiness to return to play. Studies using neuropsychological tests after concussion have failed to show any difference between those who lost consciousness and those who did not.32,33 These tests are typically conducted days after the concussion and usually not in a sport setting but rather in a medical office setting as a follow-up evaluation. The most powerful way of using these instruments is to obtain preinjury testing on each athlete, so that postinjury scores can be compared against individual baseline performance. Some amateur sports teams are using this technique, and such tests have become standard parts of concussion evaluation protocols for some college football programs34 and the National Hockey League.35 The National Football League has put a similar program in place. I have been involved in coordinating the neuropsychological testing program for the Chicago Bears for the last 7 years. However, if cognitive functions are not evaluated within minutes of the injury, the distinction between grades of concussion is lost.
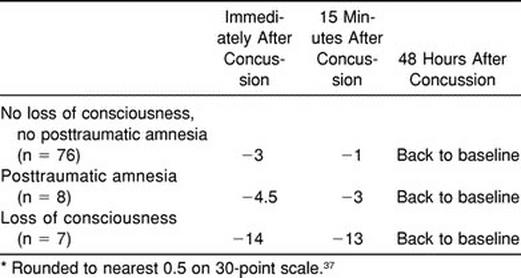
Sideline mental status testing can be valid and useful in documenting the effects of concussion. We recently reported that neurocognitive deficits can be detected immediately after even mild concussions in football players with the Standardized Assessment of Concussion (SAC).36 On the 30-point SAC scale, a drop of 3 points from preinjury baseline was seen in 76 athletes who experienced transient confusion without PTA or LOC. Eight players who had PTA without LOC dropped 4.5 points, and 7 players who had brief LOC dropped 14 points (Table 2). Only the mildest form of concussion was associated with rapid recovery of cognitive functions by retesting at 15 minutes after the injury. The group with PTA improved somewhat but did not regain the baseline level of performance. The LOC group demonstrated virtually no improvement in cognitive functions by 15 minutes postinjury.37 This study is the first to show that disturbances in mental function can be measured immediately after concussion in order to determine the severity of the injury. The findings of this study are most consistent with the grading scale published by the Colorado Medical Society.38,39
Table 2.
Changes in Standardized Assessment of Concussion Scores* After Concussion (n = 91)
Return to Play after LOC
Concussions with LOC are commonly associated with longer recovery time than concussions without LOC. That is the major reason why each of the most widely used sports concussion guidelines (Table 3) indicate that the appearance and length of LOC are associated with a more worrisome concussion.38–41
Table 3.
Sports Concussion Grading Scales*
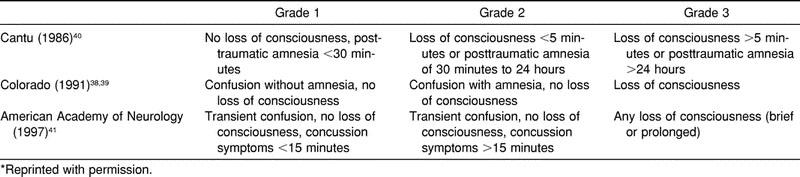
The consensus regarding return to play developed by the American Academy of Neurology41 is presented in Table 4. Any athlete rendered unconscious (grade 3) for even a few seconds must not be allowed to return to that practice or game and must undergo neurologic examination by a physician. In fact, only those without amnesia whose symptoms clear within 15 minutes are allowed to return to play that day.
Table 4.
Time to Return to Play After Removal From Contest*
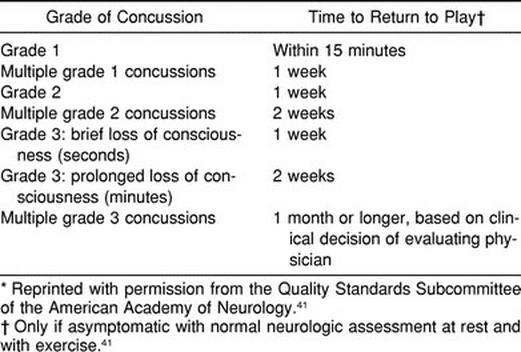
LOC lasting several minutes should be viewed as a potential neurosurgical emergency requiring urgent medical evaluation. A brief LOC is followed by 1 week off. Longer periods of LOC extend the time of recovery by an additional week or more. Two grade 3 concussions in the same season result in 1 month off. Other contributory factors, such as persistent headache, head pain from associated soft tissue injury, neck pain, and sleep disturbance adversely affect mental functions and can prolong recovery time. The athlete's physician may determine that a longer recovery time is required.
More than one member of a panel of sports medicine specialists31 reported routinely returning players to the same practice or game in which they had been rendered unconscious. Such a practice is unsupported by neuroscience or expert consensus and puts the athlete in danger of permanent and possibly catastrophic neurologic harm.
Summary
It is rewarding to have the opportunity to present this information to the readership of the Journal of Athletic Training because the athletic trainer is the health care professional most likely to witness a concussion during a sport event and is most often in a position to initiate the evaluation and management of the injured player. A growing body of scientific knowledge supports the notion that concussion should be considered a serious medical condition that can have a long-lasting and even catastrophic outcome if misunderstood and mismanaged. I have reviewed the evidence regarding the role of LOC in the diagnosis and management of sport concussion. The evidence generally supports the contention that concussion with LOC represents a worse form of brain injury than concussion without LOC but that rates of recovery vary from individual to individual. Detailed neurologic evaluation, neuroimaging, neuropsychological assessment, and honest reporting of symptoms by the athlete each have very important roles in the safe management of concussion.
All return-to-play guidelines published in recent times emphasize the need for monitoring an athlete with mental status testing of some kind and insisting that he or she be symptom free for some prescribed period of time before returning to activity. Neuropsychological evaluation of the athlete who had been rendered unconscious should be done whenever possible before clearance to return to play. Again, these guidelines are based on the consensus of specialists selected for their expertise in the diagnosis and management of sport concussion. Recent evidence in medical science seems to support the observation that we have been underestimating the amount of time it takes to recover from concussion. The careful clinician errs on the side of caution in making return-to-play decisions after concussion in sports.
REFERENCES
- 1.Kelly JP. Traumatic brain injury and concussion in sports. JAMA. 1999;282:989–991. doi: 10.1001/jama.282.10.989. [DOI] [PubMed] [Google Scholar]
- 2.Kelly JP, Rosenberg JH. Diagnosis and management of concussion in sports. Neurology. 1997;48:575–580. doi: 10.1212/wnl.48.3.575. [DOI] [PubMed] [Google Scholar]
- 3.Fisher CM. Concussion amnesia. Neurology. 1966;16:826–830. [Google Scholar]
- 4.Yarnell PR, Lynch S. Retrograde memory immediately after concussion. Lancet. 1970;1:863–864. doi: 10.1016/s0140-6736(70)91691-0. [DOI] [PubMed] [Google Scholar]
- 5.The New Lexicon Webster's Dictionary of the English Language. New York, NY: Lexicon Publications Inc; 1987. p. 1072. [Google Scholar]
- 6.Ommaya AK, Gennarelli TA. Cerebral concussion and traumatic unconsciousness: correlation of experimental and clinical observations of blunt head injuries. Brain. 1974;97:633–654. doi: 10.1093/brain/97.1.633. [DOI] [PubMed] [Google Scholar]
- 7.Plum F, Posner JB. States of acutely altered consciousness. In: Plum F, Posner JB, editors. The Diagnosis of Stupor and Coma. 3rd ed. Philadelphia, PA: FA Davis; 1982. pp. 3–5. [Google Scholar]
- 8.Giacino JT, Zasler ND, Katz DI, Kelly JP, Rosenberg JH, Filley CM. Development of practice guidelines for assessment and management of the vegetative and minimally conscious states. J Head Trauma Rehabil. 1997;12:79–89. [Google Scholar]
- 9.Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 10.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–484. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 11.Narayan RK, Greenberg RP, Miller JD, et al. Improved confidence of outcome prediction in severe head injury. J Neurosurg. 1981;54:751–762. doi: 10.3171/jns.1981.54.6.0751. [DOI] [PubMed] [Google Scholar]
- 12.Wagstyl J, Sutcliffe AJ, Alpar EK. Early prediction of outcome following head injury in children. J Pediatric Surg. 1987;22:127–129. doi: 10.1016/s0022-3468(87)80427-x. [DOI] [PubMed] [Google Scholar]
- 13.Williams DH, Levin HS, Eisenberg HM. Mild head injury classification. Neurosurgery. 1990;27:422–428. doi: 10.1097/00006123-199009000-00014. [DOI] [PubMed] [Google Scholar]
- 14.van der Naalt J, van Zomeron AH, Sluiter WJ, Minderhoud JM. One year outcome in mild to moderate head injury: the predictive value of acute injury characteristics related to complaints and return to work. J Neurol Neurosurg Psychiatry. 1999;66:207–213. doi: 10.1136/jnnp.66.2.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brooks DN, Aughton ME, Bond MR, Jones P, Rizvi S. Cognitive sequelae in relationship to early indices of severity of brain damage after severe blunt head injury. J Neurol Neurosurg Psychiatry. 1980;43:529–534. doi: 10.1136/jnnp.43.6.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Denny-Brown D, Ritchie Russell W. Experimental cerebral concussion and the mechanism of experimental concussion. Brain. 1941;64:94–164. [Google Scholar]
- 17.Gennarelli TA. Cerebral concussion and diffuse brain injuries. In: Cooper PR, editor. Head Injury. 3rd ed. Baltimore, MD: Williams & Wilkins; 1993. pp. 137–158. [Google Scholar]
- 18.Mild Traumatic Brain Injury Committee of the Head Injury Interdisciplinary Special Interest Group of the American Congress of Rehabilitation Medicine. J Head Trauma Rehabil. 1993;8:86–87. [Google Scholar]
- 19.Jenkins A, Teasdale G, Hadley MD, Macpherson P, Rowan JO. Brain lesions detected by magnetic resonance imaging in mild and severe head injuries. Lancet. 1986;2:445–446. doi: 10.1016/s0140-6736(86)92145-8. [DOI] [PubMed] [Google Scholar]
- 20.Levin HS, Williams DH, Eisenberg HM, High WM, Jr, Guinto FC., Jr Serial MRI and neurobehavioral findings after mild to moderate closed head injury. J Neurol Neurosurg Psychiatr. 1992;55:255–262. doi: 10.1136/jnnp.55.4.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Levi L, Giulburd JN, Lemberger A, Soustiel JF, Feinsod M. Diffuse axonal injury: analysis of 100 patients with radiological signs. Neurosurgery. 1990;27:429–432. [PubMed] [Google Scholar]
- 22.Gentry LR, Godersky JC, Thompson B, Dunn VD. Prospective comparative study of intermediate-field MR and CT in the evaluation of closed head trauma. AJR Am J Roentgenol. 1988;150:673–682. doi: 10.2214/ajr.150.3.673. [DOI] [PubMed] [Google Scholar]
- 23.Levin HS, Williams DH, Crofford MJ, et al. Relationship of depth of brain lesions to consciousness and outcome after closed head injury. J Neurosurg. 1988;69:861–866. doi: 10.3171/jns.1988.69.6.0861. [DOI] [PubMed] [Google Scholar]
- 24.Levin HS, Handel SF, Goldman AM, Eisenberg HM, Guinto FC., Jr Magnetic resonance imaging after ‘diffuse’ nonmissile head injury: a neurobehavioral study. Arch Neurol. 1985;42:963–968. doi: 10.1001/archneur.1985.04060090045012. [DOI] [PubMed] [Google Scholar]
- 25.Giza CC, Hovda DA. Ionic and metabolic consequences of concussion. In: Cantu RC, Cantu RI, editors. Neurologic Athletic Head and Spine Injuries. Philadelphia, PA: WB Saunders; 2000. pp. 80–100. [Google Scholar]
- 26.Bergsneider M, Hovda DA, Lee SM, et al. Dissociation of cerebral glucose metabolism and level of consciousness during the period of metabolic depression following human traumatic brain injury. J Neurotrauma. 2000;17:389–401. doi: 10.1089/neu.2000.17.389. [DOI] [PubMed] [Google Scholar]
- 27.Povlishock JT, Kontos HA. Continuing axonal and vascular change following experimental brain trauma. J Cent Nerv Sys Trauma. 1985;2:285–298. doi: 10.1089/cns.1985.2.285. [DOI] [PubMed] [Google Scholar]
- 28.Lee SM, Wong MD, Samii A, Hovda DA. Evidence for energy failure following irreversible traumatic brain injury. Ann N Y Acad Sci. 1999;893:337–340. doi: 10.1111/j.1749-6632.1999.tb07849.x. [DOI] [PubMed] [Google Scholar]
- 29.McIntosh TK, Smith DH, Meaney DF, Kotapka MJ, Gennarelli TA, Graham DI. Neuropathological sequelae of traumatic brain injury: relationship to neurochemical and biomechanical mechanisms. Lab Invest. 1996;74:315–342. [PubMed] [Google Scholar]
- 30.Saatman KE, Graham DI, McIntosh TK. The neuronal cytoskeleton is at risk after mild and moderate brain injury. J Neurotrauma. 1998;15:1047–1058. doi: 10.1089/neu.1998.15.1047. [DOI] [PubMed] [Google Scholar]
- 31.Woljtys EM, Hovda D, Landry G, et al. Current concepts: concussion in sports. Am J Sports Med. 1999;27:676–687. doi: 10.1177/03635465990270052401. [DOI] [PubMed] [Google Scholar]
- 32.Leininger BE, Gramling SE, Farrell AD, Kreutzer JS, Peck EA., III Neuropsychological deficits in symptomatic minor head injury patients after concussion and mild concussion. J Neurol Neurosurg Psychiatry. 1990;53:293–296. doi: 10.1136/jnnp.53.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lovell MR, Iverson GL, Collins MW, McKeag D, Maroon JC. Does loss of consciousness predict neuropsychological decrements after concussion? Clin J Sport Med. 1999;9:193–198. doi: 10.1097/00042752-199910000-00002. [DOI] [PubMed] [Google Scholar]
- 34.Lovell MR, Collins MW. Neuropsychological assessment of the college football player. J Head Trauma Rehabil. 1998;13:9–26. doi: 10.1097/00001199-199804000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Lovell MR, Burke CJ., III . Concussions in ice hockey: The National Hockey League Program. In: Cantu RC, Cantu RI, editors. Neurologic Athletic Head and Spine Injuries. Philadelphia, PA: WB Saunders; 2000. pp. 109–116. [Google Scholar]
- 36.McCrea M, Kelly JP, Kluge J, Ackley B, Randolph C. Standardized assessment of concussion in football players. Neurology. 1997;48:586–588. doi: 10.1212/wnl.48.3.586. [DOI] [PubMed] [Google Scholar]
- 37.Kelly JP, McCrea M, Randolph C. The detection of neurocognitive deficits at the threshold of concussion. Neurology. 2000;54:243–244. [Google Scholar]
- 38.Kelly JP, Nichols JS, Filley CM, Lillehei KO, Rubinstein D, Kleinschmidt-DeMasters BK. Concussion in sports: guidelines for the prevention of catastrophic outcome. JAMA. 1991;266:2867–2869. doi: 10.1001/jama.266.20.2867. [DOI] [PubMed] [Google Scholar]
- 39.Report of the Sports Medicine Committee. Guidelines for the Management of Concussion in Sports (revised) Denver, CO: Colorado Medical Society; 1991. [Google Scholar]
- 40.Cantu RC. Guidelines for return to contact sports after a cerebral concussion. Physician Sportsmed. 1986;14(10):75–83. doi: 10.1080/00913847.1986.11709197. [DOI] [PubMed] [Google Scholar]
- 41.Practice parameter: the management of concussion in sports (summary statement). Report of the Quality Standards Subcommittee. Neurology. 1997;48:581–585. doi: 10.1212/wnl.48.3.581. [DOI] [PubMed] [Google Scholar]