Abstract
Objective:
The effects of concussion on mental status are often difficult to assess on routine clinical examination. I investigated the efficacy of standardized mental status testing on the sport sideline to detect abnormalities that result from concussion and provide an objective measure of postinjury cognitive recovery.
Design and Setting:
All subjects underwent a standardized preseason baseline mental status evaluation. Standardized testing of injured and uninjured control subjects was repeated on the sideline immediately after concussion and 48 hours after injury.
Subjects:
Sixty-three high school and collegiate football players with concussion and 55 uninjured control subjects were studied.
Measurements:
The Standardized Assessment of Concussion (SAC) was administered to evaluate neurocognitive functioning and neurologic status.
Results:
Immediately after concussion, injured subjects performed significantly below preinjury baseline and below uninjured controls on the SAC. Measurable deficits in orientation, concentration, and memory were evident immediately after concussion. A decline in SAC score at time of injury was 95% sensitive and 76% specific in accurately classifying injured and uninjured subjects on the sideline. Injured subjects demonstrated significant improvements in SAC score 48 hours after injury.
Conclusions:
Standardized mental status testing can be a valuable tool to assist the sports medicine clinician in detecting the immediate effects of concussion on mental status, tracking resolution of immediate postconcussive mental status abnormalities, and making more informed decisions on return to play after injury.
Keywords: athletic injuries, neuropsychological tests
The sports medicine clinician is faced with many challenges in providing care for young athletes, but perhaps none is more complex than the diagnosis and management of concussion.1 Detecting concussion is relatively clear-cut when the subject is rendered unconscious or obviously amnestic and disoriented, but more than 90% of sport-related head injuries result in no observable loss of consciousness (LOC) or amnesia and only slight disorientation.2,3 Milder deficits in neurocognitive functioning (eg, memory, concentration) are more common after an athlete experiences a concussion.4,5 Unfortunately, the effects of concussion on mental status are usually more subtle than obvious, often making them difficult to identify and fully characterize on routine clinical examination.
Recent efforts have focused on the development of brief, standardized methods of concussion assessment for use on the sport sideline, including measures to evaluate neurocognitive status,6–8 postural stability,9,10 and postconcussive symptoms.11,12 The aim of standardized screening instruments is to reduce the amount of “guesswork” often encountered by the sports medicine clinician in assessing concussion on the sideline. Researchers4,5 have emphasized the value of standardized mental status testing on the sideline after concussion to clarify the acute effects of injury and establish an index of severity against which to track recovery. More accurate injury assessment is also intended to reduce the risks of recurrent injury, cumulative neuropsychological impairment, and catastrophic outcome associated with sport-related concussion. Certified athletic trainers have made clear their impression that the addition of standardized concussion assessment methods results in a more clinically informative and accurate injury evaluation than a routine clinical examination alone.13
The Standardized Assessment of Concussion (SAC)6,8 was developed to provide clinicians with a more objective and standardized method of immediately assessing an injured athlete's mental status on the sport sideline within minutes of having sustained a concussion. The instrument is intended as a supplement to other methods of concussion assessment (eg, neuropsychological evaluation, postural stability testing) but not meant to be a stand-alone measure to determine the severity of injury or an athlete's readiness to resume participation after concussion. Previous investigators4,5,14 have documented the psychometric properties of the SAC and supported the sensitivity and clinical validity of the instrument in detecting sport-related concussion and providing a gross measure of postinjury cognitive recovery. The interpretation of validity and reliability data from earlier studies was limited, however, by the lack of a uninjured control group to undergo serial testing on the SAC under the same conditions as the injured subjects. The current study's design included a control group to assess the validity of the SAC in differentiating injured and uninjured subjects after sport-related concussion and provide an objective measure of postinjury neurocognitive recovery.
METHODS
Subjects and Design
A total of 1325 high school and collegiate football players were studied during the 1998 and 1999 football seasons. The sample consisted of 714 athletes from 16 high schools (mean age, 16.26 ± 0.83 years) and 611 players from 8 colleges and universities (mean age, 19.84 ± 1.30 years). All subjects underwent baseline testing on the SAC6,8 before the start of the football season. This study was approved by the institutional review board at the host institution. All subjects granted written, informed consent. Baseline testing was conducted by certified athletic trainers during preseason fitness and weight training or noncontact football drills and included conditions of exertion as prescribed in the SAC to control for fatigue and other factors often encountered after concussion during a sporting event.
Sixty-three injuries (4.75% of total sample) were documented during the study, including 30 high school (4.20% of high school participants) and 33 collegiate players (5.40% of college participants). Three injured subjects (4.76% of all injuries) were noted to have any observed or reported LOC, with a maximum duration of several seconds. Four injured athletes (6.35%) without LOC exhibited measurable retrograde amnesia (inability to recall events preceding injury) or posttraumatic amnesia (PTA) (inability to recall events after injury), ranging from several seconds to minutes surrounding the injury. No subjects experienced recurrent concussion, and there were no neurosurgical complications, cases of second-impact syndrome,15,16 or catastrophic outcomes encountered in this study.
Concussion was defined according to the American Academy of Neurology practice parameter17 (ie, trauma-induced alteration in mental status with or without LOC). Criteria contributing to the identification of an injured player included mechanism of injury (eg, acceleration or rotational forces applied to the head), symptoms reported or signs exhibited (eg, alteration in mental status, confusion, headache, dizziness, memory problems)17,18 by the player, and reports by teammates and other witnesses regarding the injured player's condition. The occurrence and duration of LOC and PTA were documented immediately after injury by the certified athletic trainer who examined the player.
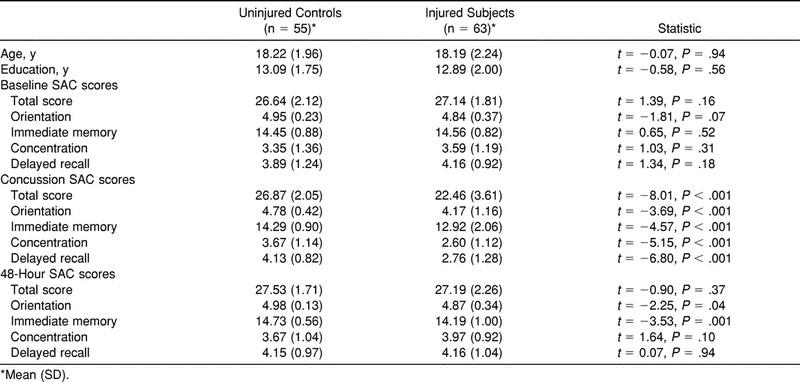
Injured subjects identified by the team's certified athletic trainer as having sustained a concussion were tested with the SAC on the sideline immediately following injury and again 48 hours after injury. This immediate assessment was conducted within 5 minutes of the injury in all cases. Fifty-five uninjured control subjects, including 24 high school (mean age, 16.42 ± 0.65 years) and 31 college players (mean age, 19.61 ± 1.41 years), were randomly selected from the pool of varsity players and reexamined on the SAC according to the same protocol as the injured subjects. All case-matched uninjured control subjects underwent SAC testing on the sideline after their respective matched subjects sustained a concussion and 48 hours after injury under the same conditions as injured athletes. In most cases, control subjects were platoon or special teams players tested immediately after exiting the field of play to control for fatigue and exertion. Table 1 provides a comparison of demographic variables and injury assessment data for control and injured subjects. No data were missing for the control or injured groups at the baseline, time of injury, or 48-hour assessment points.
Table 1.
Sample Characteristics and Standardized Assessment of Concussion (SAC) Scores for Injured and Control Subjects
Evaluation Measure
The SAC6,8 is a brief screening instrument designed for the neurocognitive assessment of concussion by a nonneuropsychologist with no prior expertise in psychometric testing. The SAC requires approximately 5 minutes to administer and includes measures of orientation, immediate memory, concentration, and delayed recall, summing to a total composite score of 30 points (Table 2). A standard neurologic screening is included in the SAC to assess deficits in strength, sensation, and coordination that result from concussion. The occurrence and duration of LOC, retrograde amnesia, and PTA also are recorded on the SAC. Three equivalent alternate forms of the test were used in this study to minimize practice effects from additional administration.4,5 The SAC is printed on pocket-sized cards for convenient use by athletic trainers and medical personnel who examine athletes on the sideline.
Table 2.
Standardized Assessment of Concussion (SAC)

Data Analysis
Repeated-measures analyses of variance (ANOVAs) were conducted to analyze SAC scores, with group (injured versus control) as a between-subjects factor and assessment point (baseline, concussion, 48 hours) as a within-subjects factor. Level of competition (high school versus college) was included as a covariate in the repeated-measures ANOVAs. Statistical significance of P < .05 was set a priori for the ANOVAs. Post hoc comparisons of group differences at each assessment interval were evaluated using t tests. Paired t tests were used to analyze any significant differences in SAC scores within groups at baseline, time of injury, and 48 hours after injury. To minimize error rates associated with multiple comparisons, the .01 level of probability was used for post hoc comparisons.19 Bivariate (Pearson) correlational analyses were computed to examine the test-retest reliability of SAC scores for injured and control subjects across administrations.
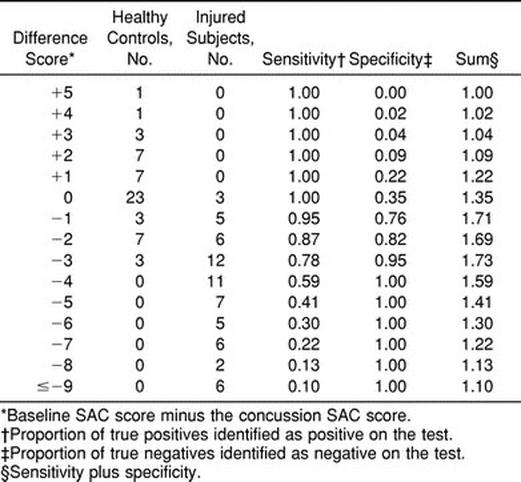
The SAC change scores were derived based on the difference between SAC total score at baseline and immediately after injury. A frequency distribution of observed change scores for injured and control subjects was generated to examine corresponding levels of sensitivity and specificity in accurately identifying injured and uninjured subjects. Documentation of concussion by the certified athletic trainer and inclusion of an injured subject in this research protocol, independent of performance on the SAC, was used as the standard on which to base sensitivity and specificity calculations. Sensitivity refers to the probability that a subject with a certain diagnosis (eg, concussion) will be correctly identified by a specific test result (eg, SAC change score). Specificity refers to the probability that an individual without the condition will be correctly classified as not having the condition. The sum of sensitivity and specificity calculations often provides the greatest overall classification value, but the relative importance of sensitivity and specificity varies, depending on the clinical issue under study. With respect to the diagnosis and management of concussion, one may argue that accurately detecting the greatest proportion of injured subjects (ie, sensitivity) is more critical than precisely identifying those subjects without an injury. Data were analyzed with SPSS 10.0 statistical software (SPSS Inc, Chicago, IL).20
Preliminary Analysis
The preseason baseline SAC total score mean for subjects who were eventually injured during the study was higher for college players than high school subjects (t1,61 = −2.51, P = .02), but there were no significant differences in SAC total scores for the 2 groups immediately after concussion (t1,61 = −0.403, P = .69) or 48 hours after injury (t1,61 = −1.55, P = .13). There was also no significant difference in the average change from preseason baseline SAC total score by high school and collegiate subjects immediately after injury (t1,61 = −0.86, P = .40). Additionally, the interaction (level × assessment point) (F2,230 = 0.47, P = .63) effect did not reach statistical significance for level of competition (high school versus college) as a covariate in the repeated-measures ANOVA that looked at the effects of group (injured versus controls) on SAC performance across time. Therefore, injury and control data for high school and collegiate subjects were combined for formal analysis of the study's main findings. There was no significant difference in SAC total score for injured and control subjects on preseason baseline testing (t1,116 = 1.39, P = .16). There were also no significant differences in SAC total score by those injured subjects administered different forms of the SAC (A, B, C) immediately after concussion (F2,60 = 0.45, P = .77).
RESULTS
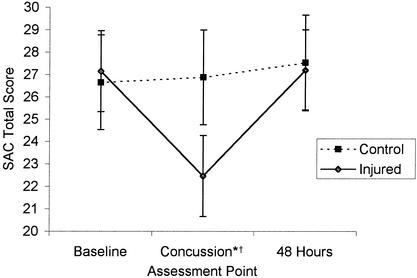
Repeated-measures ANOVA revealed a significant interaction effect (group × assessment point) for SAC total score (F2,232 = 64.38, P < .001). Main effects for group (F1,116 = 16.71, P < .001) and assessment point (F2,232 = 76.98, P < .001) on SAC total score were also significant. The pattern of mean SAC total scores for injured and control subjects at baseline, time of injury, and 48 hours after injury is illustrated in the Figure. Significant interaction effects were also revealed for the Orientation (F2,232 = 8.00, P < .001), Immediate Memory (F2,232 = 15.02, P < .001), Concentration (F2,232 = 26.52, P < .001), and Delayed Recall (F2,232 = 24.99, P < .001) subtests of the SAC. Main effects for group were demonstrated on Orientation (F1,116 = 18.85, P < .001), Immediate Memory (F1,116 = 16.79, P < .001), and Delayed Recall (F1,116 = 7.41, P = .007) subtests but not for the Concentration section (F1,116 = 1.10, P = .30). Main effects for assessment point were significant for the Orientation (F2,232 = 23.95, P < .001), Immediate Memory (F2,232 = 28.27, P < .001), Concentration (F2,232 = 20.68, P < .001), and Delayed Recall (F2,232 = 18.41, P < .001) subtests.
Standardized Assessment of Concussion (SAC) total scores for injured subjects (n = 63) and uninjured controls (n = 55) at baseline, immediately after concussion, and 48 hours after injury. *Injured group was significantly different from control group (P < .001). †Injured group was significantly different from baseline score (P < .001). Error bars indicate 1 SD above and below group mean.
Paired t tests indicated that injured subjects immediately after concussion performed significantly below their preseason baseline SAC total score (t1,62 = 11.03, P < .001), but uninjured control subjects did not (t1,54 = −1.03, P = .31). Injured subjects also scored significantly below preinjury baseline immediately after concussion on the Orientation (t1,62 = 4.25, P < .001), Immediate Memory (t1,62 = 6.43, P < .001), Concentration (t1,62 = 6.12, P < .001), and Delayed Recall (t1,62 = 7.74, P < .001) sections of the SAC. Control subjects performed slightly higher than their baseline performance on the SAC Concentration subtest (t1,54 = −2.10, P = .04) on the sideline, but there were no other significant differences between baseline and time of injury scores for controls on the other SAC subtests.
The SAC total score for injured subjects was significantly lower than uninjured controls immediately after injury (t1,116 = −8.01, P < .001). Scores for injured subjects immediately after concussion were also significantly lower than controls on the Orientation (t1,116 = −3.69, P < .001), Immediate Memory (t1,116 = −4.57, P < .001), Concentration (t1,116 = −5.15, P < .001), and Delayed Recall (t1,116 = −6.80, P < .001) sections of the SAC.
There was no significant difference between SAC total score for the injured group at baseline and 48 hours after injury (t1,62 = −0.23, P = .82). The only significant deficit relative to preseason baseline for injured subjects at the 48-hour assessment point was on the Immediate Memory section (t1,62 = 2.98, P = .004). A practice effect for injured subjects from baseline to 48 hours was detected on the Concentration section (t1,62 = −2.87, P = .006), and there were no significant differences on the Orientation (t1,62 = −0.50, P = .62) or Delayed Recall subtests (t1,62 = 0.00, P >.99).
Uninjured controls demonstrated a slight improvement from baseline to 48 hours that reached statistical significance for SAC total score (t1,54 = −3.32, P = .002) and the Immediate Memory (t1,54 = −2.76, P = .008) section. There were no significant differences in scores for uninjured controls at baseline and 48 hours on the Orientation (t1,54 = −1.00, P = .32) Concentration (t1,54 = −1.90, P = .06), and Delayed Recall (t1,54 = −1.31, P = .20) subtests. There was no significant difference in SAC total score for injured and uninjured subjects at the 48-hour assessment point (t1,116 = −0.90, P = .37). Injured subjects did, however, score significantly lower than uninjured control subjects on the Immediate Memory section of the SAC 48 hours after injury (t1,116 = −3.53, P = .001). There were no significant group differences on the other SAC subtests at the 48-hour assessment point.
As would be expected, the level of test-retest (baseline to time of injury) correlation was higher for the uninjured control group (r = 0.66, P < .001) than the injured group (r = 0.38, P = .002). The mean difference in SAC total score from baseline to time of injury was −4.68 (3.37) for the injured group and +0.24 (1.71) for the control group. Test-retest reliability comparing SAC total score at baseline and 48 hours after injury was significant for both the injured (r = 0.69, P < .001) and control groups (r = 0.48, P < .001). Ninety-five percent of injured subjects demonstrated a drop in SAC total score by at least 1 point immediately after concussion, compared with 24% of uninjured controls on test-retest. The distribution of observed change in SAC scores, with sensitivity and specificity values, for the injured and control groups is shown in Table 3. A case-by-case qualitative review of SAC scores immediately after injury indicated that subjects who had sustained LOC or PTA were more severely impaired than those who did not, but sample sizes were not sufficient to support formal statistical analysis.
Table 3.
Differences Between Standardized Assessment of Concussion (SAC) Scores at Baseline and Immediately After Concussion for Injured and Control Subjects
DISCUSSION
The approach to mental status testing on the sport sideline after a suspected concussion has historically been qualitative and subjective, sometimes limited to the clinician's impression that “something's off” with respect to the injured athlete's presentation. It is now widely recognized that stereotypic questions such as “how many fingers am I holding up?” and “where are you?” are of little diagnostic value to the sports medicine clinician in determining whether an athlete has sustained a concussion and, if so, grading the severity of the injury. Most clinicians are now aware of the importance of systematically assessing the injured athlete's mental status and neurocognitive functioning to detect deficits in orientation, memory, and concentration after a concussion but simply lack an objective and systematic method for doing so.
The results of this study are consistent with earlier reports4,5,14 that support the value of standardized mental status assessment measures to aid the clinician in the diagnosis and management of concussion in athletes on the sport sideline. Standardized cognitive testing in this study was sensitive to subtle deficits in orientation, memory, and concentration in injured subjects who were otherwise not displaying signs of frank disorientation, amnesia in the classic sense, or gross neurologic dysfunction. Injured athletes who sustained a concussion as defined by the American Academy of Neurology guidelines17 exhibited, on average, a decrease of more than 4 points on the SAC immediately after concussion, whereas uninjured controls retested on the sideline showed an average increase of less than 1 point above their baseline. A drop of 1 point or more from preseason baseline score on the SAC was 95% sensitive and 76% specific in correctly classifying injured and uninjured subjects. These findings also suggest that the decline in SAC score by injured subjects immediately after concussion represents the direct effect of injury on cognitive functioning and is not due to other extraneous factors often encountered on the sport sideline (eg, fatigue, crowd noise, distractibility). Clinicians should, however, consider the potential impact of other postconcussive symptoms (eg, headache, nausea) on a player's performance on mental status testing.
The clinician's diagnosis is perhaps most difficult to make when subtle signs and symptoms raise the suspicion of concussion, but classic indicators of injury (eg, LOC, amnesia, focal neurologic abnormalities) are not manifested. Results from this study indicate that significant neurocognitive changes can be detected on standardized testing after concussion without LOC, PTA, or focal neurologic abnormalities. Approximately 90% of all injured subjects in this study experienced no LOC, PTA, or changes in gross neurologic status but exhibited measurable deficits in orientation, memory, or concentration function on standardized mental status testing immediately after injury. Although the infrequent occurrence of LOC and PTA in the current study did not allow formal statistical analysis of the effect of these phenomena on SAC scores, qualitative review suggests that LOC and PTA were accompanied by more severe cognitive impairment immediately after concussion. Further study is required to clarify the relative importance of LOC, PTA, and other factors in predicting recovery after sport-related concussion.
After determining that an athlete has indeed sustained a concussion, the clinician's next challenge is tracking recovery and determining whether an athlete is fit to return to action in the same contest. If not, the question remains as to when it is safe for a player to return to play after a period of recovery. The current findings suggest that standardized mental status testing may be helpful in establishing a quantifiable index against which to track resolution of acute, postconcussive, cognitive sequelae, and return to baseline cognitive functioning. Follow-up testing for residual deficits in new learning and memory appears to be especially critical, based on the current findings. These data can be used by the clinician in combination with information from other screening instruments, physical examination, more extensive neuropsychological testing, and the player's self-report on postconcussive symptoms to determine the level of recovery and the readiness to return to competition. Preseason baseline testing of all athletes is the recommended model for use of concussion screening instruments in sports, because comparison with an athlete's preinjury performance on a given measure provides the most accurate indicator of postinjury recovery.
A multidimensional approach to sideline assessment of concussion is strongly recommended. Assessment of one symptom domain is not sufficient, since the effects of concussion may manifest differently across individuals. Clinicians now have available several brief, standardized methods for assessment of mental status,6–8 postural stability,9,10 and postconcussive symptoms11,12 appropriate for use in a sport setting. Neuropsychological testing is also recognized as a valuable tool to objectively measure the effects of sports concussion and track postinjury recovery11,21–25 but is not very feasible for use on the sideline during sporting events. The combination of brief, standardized measures to quantify the immediate effects and follow-up neuropsychological testing of the injured athlete likely represents the best model for measuring the neurocognitive effects of injury, tracking recovery of function, and assisting the clinician in decision making on the athlete's return to competition.
The clinician should be aware of various limitations related to the use of brief concussion screening tools and have a full command of guidelines for the administration, scoring, and interpretation of a screening instrument before applying it in a clinical situation. These measures provide the clinician with objective information on the presence and severity of concussion but are not intended as a substitute for formal neurologic evaluation, neuropsychological testing, or medical follow-up of the injured subject. Brief assessment tools do not allow an exhaustive evaluation of all cognitive domains (eg, reaction time, information processing speed) sensitive to change after concussion. Screening instruments also do not represent a stand-alone method for declaring full recovery or clearing an athlete to return to play after concussion. All clinical information should be considered to ensure that a player is completely symptom free for a period before being released to return to competition after experiencing a head injury of any severity. More empirical data are required to address the debate on how long an athlete should be withheld from competition after concussion.
Current ongoing studies include SAC testing of injured subjects and matched controls at more points after injury to further clarify the course of early cognitive recovery after concussion. These studies will also correlate SAC findings with results from neuropsychological testing and other concussion assessment methods. A new line of research is under way that correlates objective clinical methods (eg, SAC, neuropsychological testing, postural stability testing, symptom reports) and findings on functional magnetic resonance imaging as a more direct measure of neurophysiological recovery after sport-related concussion. The specific aim of these studies is to elucidate the period of cerebral vulnerability after concussion, which may influence guidelines for the recommended period an athlete should be withheld from competition after injury.
CONCLUSION
The use of standardized measures can improve the accuracy of concussion assessment on the sport sideline. The ultimate goals of these methods are to provide the clinician with a more systematic framework for examining an injured athlete, to allow implementation of proper injury management strategies, and to permit more informed decisions on return to play. Early and accurate diagnosis of concussion is also critical to reducing the potential risks of recurrent injury, cumulative neuropsychological impairment, and catastrophic outcomes associated with second-impact syndrome. Screening instruments are valuable tools to assist the sports medicine clinician in the assessment and management of concussion but should not be used as a replacement for medical evaluation or as the sole determinant of an injured athlete's readiness to return to play after concussion.
ACKNOWLEDGMENTS
I thank all the certified athletic trainers who assisted in the data collection for this study and the players, coaching staff, and administration from each participating institution for their cooperation throughout the study.
REFERENCES
- 1.Guskiewicz KM, Riemann BL, Perrin DH, Nashner LM. Alternative approaches to the assessment of mild head injury in athletes. Med Sci Sports Exerc. 1997;29:213–221. doi: 10.1097/00005768-199707001-00003. [DOI] [PubMed] [Google Scholar]
- 2.Cantu RC. Head injuries in sport. Br J Sports Med. 1996;30:289–296. doi: 10.1136/bjsm.30.4.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guskiewicz KM, Weaver NL, Padua DA, Garrett WE., Jr Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28:643–650. doi: 10.1177/03635465000280050401. [DOI] [PubMed] [Google Scholar]
- 4.McCrea M, Kelly JP, Kluge J, Ackley B, Randolph C. Standardized assessment of concussion in football players. Neurology. 1997;48:586–588. doi: 10.1212/wnl.48.3.586. [DOI] [PubMed] [Google Scholar]
- 5.McCrea M, Kelly JP, Randolph C, et al. Standardized assessment of concussion (SAC): on-site mental status evaluation of the athlete. J Head Trauma Rehabil. 1998;13:27–35. doi: 10.1097/00001199-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 6.McCrea M, Kelly JP, Randolph C. Standardized Assessment of Concussion (SAC): Manual for Administration, Scoring and Interpretation. Waukesha, WI: CNS Inc; 1996. [Google Scholar]
- 7.Kutner KC, Barth JT. Sports related concussion. Natl Acad Neuropsychol Bull. 1998;5:19–23. [Google Scholar]
- 8.McCrea M, Kelly JP, Randolph C. Standardized Assessment of Concussion (SAC): Manual for Administration, Scoring and Interpretation. 2nd ed. Waukesha, WI: CNS Inc; 2000. [Google Scholar]
- 9.Riemann BL, Guskiewicz KM, Shields EW. Relationship between clinical and forceplate measures of postural stability. J Sport Rehabil. 1999;8:1–7. [Google Scholar]
- 10.Riemann BL, Guskiewicz KM. Effects of mild head injury on postural stability as measured through clinical balance testing. J Athl Train. 2000;35:19–25. [PMC free article] [PubMed] [Google Scholar]
- 11.Lovell MR, Collins MW. Neuropsychological assessment of the college football player. J Head Trauma Rehabil. 1998;13:9–26. doi: 10.1097/00001199-199804000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Ferguson RJ, Mittenberg W, Barone DF, Schneider B. Postconcussion syndrome following sports-related head injury: expectation as etiology. Neuropsychology. 1999;13:582–589. doi: 10.1037//0894-4105.13.4.582. [DOI] [PubMed] [Google Scholar]
- 13.Ferrara MS, McCrea M, Peterson CL, Guskiewicz KM. A survey of practice patterns in concussion assessment and management. J Athl Train. 2001;36:145–149. [PMC free article] [PubMed] [Google Scholar]
- 14.Pottinger L, Cullum M, Stallings RL. Cognitive recovery following concussion in high school athletes. Arch Clin Neuropsychol. 1999;14:39–40. [Google Scholar]
- 15.Saunders RL, Harbaugh RE. The second-impact in catastrophic contact-sports head trauma. JAMA. 1984;252:538–539. [PubMed] [Google Scholar]
- 16.Cantu RC. Second-impact syndrome. Clin Sports Med. 1998;17:37–44. doi: 10.1016/s0278-5919(05)70059-4. [DOI] [PubMed] [Google Scholar]
- 17.Practice parameter: the management of concussion in sports [summary statement]. Report of the Quality Standards Committee. Neurology. 1997;48:581–585. doi: 10.1212/wnl.48.3.581. [DOI] [PubMed] [Google Scholar]
- 18.Kelly JP, Rosenberg JH. Diagnosis and management of concussion in sports. Neurology. 1997;48:575–580. doi: 10.1212/wnl.48.3.575. [DOI] [PubMed] [Google Scholar]
- 19.Huck SW, Cormier W. Reading Statistics and Research. New York, NY: HarperCollins; 1996. [Google Scholar]
- 20.SPSS Advanced Models 10.0. Chicago, IL: SPSS Inc; 1999. [Google Scholar]
- 21.Barth J, Alves W, Ryan T, et al. Mild head injury in sports: neuropsychological sequelae and recovery of function. In: Levin H, Eisenberg H, Benton A, editors. Mild Head Injury. New York, NY: Oxford University Press; 1989. pp. 257–275. [Google Scholar]
- 22.Macciocchi SN, Barth JT, Alves W, Rimel RW, Jane JA. Neuropsychological functioning and recovery after mild head injury in collegiate athletes. Neurosurgery. 1996;39:510–514. [PubMed] [Google Scholar]
- 23.Maddocks D, Saling M. Neuropsychological deficits following concussion. Brain Inj. 1996;10:99–103. doi: 10.1080/026990596124584. [DOI] [PubMed] [Google Scholar]
- 24.Hinton-Bayre AD, Geffen G, McFarland K. Mild head injury and speed of information processing: a prospective study of professional rugby league players. J Clin Exp Neuropsychol. 1997;19:275–289. doi: 10.1080/01688639708403857. [DOI] [PubMed] [Google Scholar]
- 25.Collins MW, Grindel SH, Lovell MR, et al. Relationship between concussion and neuropsychological performance in college football players. JAMA. 1999;282:964–970. doi: 10.1001/jama.282.10.964. [DOI] [PubMed] [Google Scholar]