Abstract
Objective:
To review models for the use of neuropsychological testing in the management of sport-related concussion at various levels of competition.
Background:
As we come to understand the natural history of sport-related concussive brain injury, it is increasingly evident that significant neurologic risks are associated with this type of injury. These risks include (1) acute intracranial pathology, (2) catastrophic brain swelling from second-impact syndrome, and (3) the potential risk for markedly prolonged recovery or permanent cognitive dysfunction associated with multiple concussions.
Description:
Neuropsychological testing has proved to be a useful tool in the medical management of sport-related concussion. In this paper, I describe a systematic model for the implementation of neuropsychological assessment of athletes at various levels of competition.
Clinical Advantages:
The systematic model was designed to incorporate state-of-the-art techniques for the detection and tracking of neurocognitive deficits associated with concussion into recently formulated guidelines for the medical management of sport-related concussion. Current applications of the model are discussed, as well as ongoing studies designed to elaborate the empirical underpinnings of the model and refine clinical decision making in this area.
Keywords: concussion, sports, brain injury
Mild traumatic brain injury (concussion) suffered by athletes engaged in organized sports has become the focus of increased attention by medical personnel engaged in the care of athletes, sport administrative bodies, the news media, and the players themselves. The growing number of medical reports and lay press articles devoted to the topic of sport-related concussion is a testament to the significance and complexity of this problem.
Concussion is typically the result of trauma to the head in contact sports, but it can occur in noncontact sports as well, usually as a result of falls. Concussion can also occur without a direct blow to the head if sufficient rotational forces are applied to the brain (eg, a whiplash injury).1 Kelly et al2 defined concussion as a “trauma-induced alteration in mental status that may or may not involve loss of consciousness.” This trauma-induced alteration in mental status can range in severity from a brief feeling of being dazed after the injury to an immediate loss of consciousness.
Traumatic brain injury has been recognized as a serious hazard for athletes since at least the turn of the century. President Theodore Roosevelt's concern over the 19 athletes who were killed or paralyzed by football injuries in 1904 led to the formation of the National Collegiate Athletic Association as a governing body to establish rules for safer competition.3 Although rules have been changed to improve player safety and protective equipment continues to evolve, concussive brain injury remains common in football. Approximately 63 000 incidents per year are estimated to occur in high school football alone in the United States.4
Football is not the only organized sport that carries a significant risk of concussion. Ice hockey has been reported to have even higher rates of concussion, and soccer has only slightly less risk.5 Even sports such as field hockey, wrestling, and lacrosse carry a substantial risk of concussive brain injury.4 Obviously, there is an inherent risk of physical injury (including concussion) associated with any sport, and changes in rules and improvements in equipment can only reduce these risks to a point. This is where the medical management of concussion becomes essential. A sophisticated medical management system for sport-related concussion is important for 3 main reasons:
Diagnosis and appropriate management of acute concussion. The appropriate management of the athlete at the time of the injury includes evaluating the severity of the concussion and identifying any potential neurosurgical emergencies (eg, epidural, subdural, or intracerebral hemorrhages) that would require immediate intervention. This initial evaluation and subsequent monitoring are of primary importance in cases of more severe injury, and the critical importance of appropriate medical intervention in such cases is obvious.
Prevention of second-impact syndrome. This potentially fatal syndrome is thought to result from the effects of a second concussion that occurs while the player is still symptomatic from an earlier concussion.2,6–9 In second-impact syndrome, cerebrovascular autoregulation is apparently disrupted, resulting in cerebrovascular congestion and malignant brain swelling with markedly elevated intracranial pressure. Reports of this syndrome have been limited thus far to adolescents and young adults, with a number of documented fatalities. Although controversy exists regarding the actual mechanism associated with this syndrome,10 the potential consequences are obviously catastrophic and argue for the development of sensitive techniques to ensure complete recovery from concussion before exposing a player to the risk of another injury.11
Monitoring of athletes to prevent prolonged recovery or permanent disability due to multiple concussions. The natural history of mild traumatic brain injury remains poorly understood. To date, virtually no prospective neuropsychological studies of an unselected (ie, non–self-referred) series of consecutive patients with concussion exist. As a result, no empirically determined parameters for the expected rate and degree of recovery from concussions of varying levels of severity have been established. It has been hypothesized for a number of years, however, that a previous history of concussion may result in the slowing of recovery or less complete recovery (or both) that is observed in individuals after a first concussion.12 It has been my experience that young adults typically recover rapidly and completely after a single concussion with brief or no associated loss of consciousness. This observation has also been made by others.13 The rate and ultimate degree of recovery in individuals who have suffered multiple concussions is less clear but may be slowed or reduced, particularly when the concussions are closely spaced.14
POTENTIAL MECHANISMS AND OUTCOMES OF PERMANENT DISABILITY FROM MULTIPLE CONCUSSIVE BRAIN INJURIES
Some evidence, primarily derived from animal studies, suggests that the rotational forces on the brain that appear to be responsible for producing concussion can result in scattered axonal injuries resulting from shearing forces.15 In milder cases, these pathologic changes are detectable only at the microscopic level. The rapid and apparently complete neuropsychological recovery that we typically observe in humans who have experienced injuries of comparable severity (in terms of momentum of impact) to these animal models is probably explicable by the concept of functional reserve; that is, we can compensate for mild, traumatically induced neuronal loss as a result of inherent redundancies in brain structures and systems. Although a certain degree of functional (ie, synaptic) reorganization may also take place after such injuries, this requires a longer period of time and, therefore, probably does not contribute to the rapid clinical recovery we typically observe.
Adhering to this theoretical model, each subsequent insult to the brain, however trivial, results in further depletion of this reserve capacity, eventually limiting the rate and perhaps the degree to which functional recovery can occur. This depletion could have 2 potential effects. The first is a direct, permanent loss of some neurocognitive functions as a result of repeated trauma. The second is a potentially increased sensitivity to the effects of normal aging or other disease states on the brain, for example, the premature expression of such age-related degenerative conditions as Parkinson disease or Alzheimer disease.
A prior history of head injury has been reported to be a risk factor for the diagnosis of Alzheimer disease16,17 and Parkinson disease.18 This may be due to prior neuronal loss from traumatic brain injury lowering the threshold for the clinical expression of these disorders. This model is based on the observation that the neuropathologic changes associated with each of these disorders are also observed in the brains of normal older individuals and that neither disease becomes clinically manifest until a certain degree of neuronal loss is reached. It is also well established that certain domains of cognitive functioning (eg, memory) decline with normal aging; it is conceivable that prior neuronal loss due to repeated head injury could accelerate this normal decline or make it clinically apparent at an earlier age.
Not only do all of these issues demand empirical investigation, they also underscore the need for a program to monitor the neurocognitive status of the athlete with a history of concussion, to minimize or avoid the possibility of permanent disability.
THE DEVELOPMENT OF A MODEL FOR THE MANAGEMENT OF CONCUSSION IN PROFESSIONAL SPORTS
Only recently have medical guidelines for the management of sport-related concussion been formulated and published. In 1986, Cantu19 published “Guidelines for return to contact sports after a cerebral concussion.” In 1991, the Colorado Medical Society20 published Guidelines for the Management of Concussion in Sports. Recently, the American Academy of Neurology21 adopted a revised version of these guidelines. Although these guidelines differ slightly in specifics, they each represent an attempt to develop a standardized approach to the assessment and clinical management of sport-related concussion. They are largely determined by clinical judgment rather than empirical evidence and are subject to revision as we learn more about the natural history of concussion.22
The goal of this paper is to describe the model that my colleagues and I have developed for the management of sport-related concussion, with a particular focus on the role of neuropsychological testing. The general model was designed primarily for implementation in contact sports, in which the incidence of concussion is sufficiently high for each player to be at a substantial level of risk. Neuropsychological testing is used within this model to provide us with a sensitive index of higher-level brain functioning, by measuring functions such as memory, attention, and speed and flexibility of cognitive processing. These specific functions have been demonstrated to be particularly sensitive to impairment as a result of mild traumatic brain injury. In contrast, a variety of other cognitive domains are much less sensitive to concussion (eg, language, simple motor functions, and visuospatial abilities), and we generally do not include these in brief test batteries designed for this purpose.
An important point to be made prior to further discussion of this model is that neuropsychological test data are only one source of information regarding the effects of a concussion. Obtaining such data does not preclude the need to carefully screen for postconcussive symptoms (eg, headache, lightheadedness, nausea), directly evaluate neurologic status, and (in some cases) obtain neuroimaging studies. Abnormalities in any one of these domains can be taken as evidence of residual effects from a concussion. Performing normally on neuropsychological examination does not necessarily rule out the possibility that a player may be otherwise symptomatic or have neurologic abnormalities or exhibit direct evidence of brain trauma on magnetic resonance imaging.
Neuropsychological testing is, however, clearly one of the most sensitive techniques for detecting abnormal brain functioning after concussion, and as such, it plays an important role in the medical management of sport-related concussion. There are three basic types of neuropsychological test batteries used in the management of sport-related concussion. These include the sideline examination, the baseline neurocognitive examination, and the comprehensive neuropsychological examination.
LEVELS OF NEUROPSYCHOLOGICAL ASSESSMENT
The Sideline Examination
There is a role for brief neurocognitive testing in the sideline evaluation of athletes shortly postconcussion. All of the guidelines for the management of sport-related concussion rely on the assessment of cognitive status immediately postconcussion in distinguishing between grade 1 and grade 2 concussions, and this assessment determines whether an athlete returns to play in the ongoing game. The most widely used and best validated instrument for this purpose is the Standardized Assessment of Concussion (SAC).23,24 The SAC consists of a 30-point scale that measures orientation, attention, and anterograde memory. It was designed for use by athletic trainers, coaches, and sideline medical personnel and takes approximately 5 minutes to administer. The SAC is a very brief scale constructed for the sole purpose of detecting and quantifying the acute neurocognitive effects of concussion. The sideline examination consists of a brief neurologic screening with the SAC and exertional maneuvers designed to raise intracranial pressure in a controlled fashion.
The Baseline Neurocognitive Examination
The baseline examination consists of a somewhat more detailed and difficult set of neurocognitive tests, typically lasting 20 to 30 minutes. Tests are targeted at those neurocognitive functions most sensitive to impairment from concussion (memory, attention, and speed and flexibility of cognitive processing). This type of battery was originally developed to be administered to professional football and hockey players before the start of preseason training. This procedure, as the name implies, is done to obtain baseline neurocognitive data on all players, so that potentially subtle changes in neurocognitive status postconcussion can be detected. The need for individual baseline examinations arises from the recognition that substantial interindividual differences exist in preinjury cognitive functions such as memory and attention and that subtle deficits in a particular individual might be overlooked because of these differences. Baseline neurocognitive testing is also being conducted with greater frequency at the collegiate level, although the constituent subtests vary from site to site. A number of ongoing projects are designed to transfer baseline testing to a fully computerized test platform, but these are currently in a development phase and still lack sufficient clinical validity to support their implementation on a wide scale.
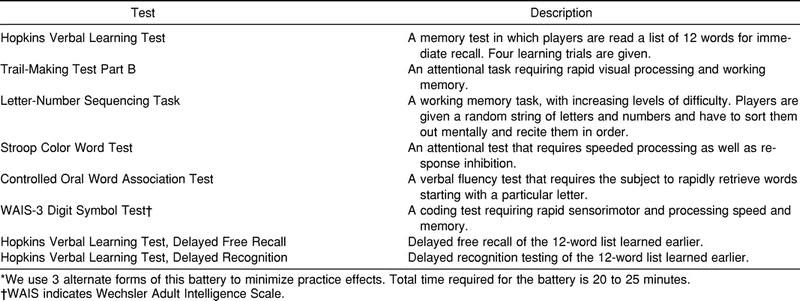
Our baseline battery of tests (Table 1) was modeled on a battery that was originally composed by Lovell and Collins25 for this purpose in their work with the Pittsburgh Steelers. We have refined this battery to take advantage of newer tests, as well as to eliminate constituent subtests that were found to lack sensitivity to concussion. We constructed 3 alternate forms of this battery (A, B, and C) to minimize practice effects on repeated testing. Our battery requires approximately 20 minutes to complete.
Table 1.
Baseline Neurocognitive Battery*
The Comprehensive Neuropsychological Examination
A standard clinical neuropsychological examination consists of comprehensive testing of multiple neurocognitive domains (eg, motor, attention, memory, language, visuospatial functions, executive and problem-solving functions) and assessment of psychological and emotional functioning. This typically requires 3 to 6 hours of testing for an adult. When the referring concern is traumatic brain injury, this type of examination is usually reserved for patients in whom there is some question of permanent impairment. In most cases of sport-related concussion, we expect complete recovery, and therefore, this type of examination is unnecessary. There are cases, however, in which an athlete has suffered multiple concussions or has had the baseline examination repeated to the point that the results are difficult to interpret. In those athletes, a comprehensive neuropsychological examination can be very informative with respect to quantifying impairment and informing decision making.
MANAGEMENT MODELS FOR HIGH SCHOOL, COLLEGIATE, AND PROFESSIONAL COMPETITION
The resources available to athletic trainers at various levels of competition are obviously markedly different, as are the consequences for withholding a player from return to play. At the National Football League or National Hockey League level, a decision to keep a key player from returning to play for one or more games could potentially result in tremendous financial losses for the team. Conversely, sending a player back too quickly could result in a second concussion, which might require a much more protracted recovery and potential loss of the player for the entire season. At the high school level, the consequences of this decision-making process are not as momentous, and it may be somewhat easier to adopt a conservative management approach. In terms of resources, professional teams also have the resources to retain experienced neurologists and neuropsychologists to manage athletes with concussive brain injuries in consultation with team physicians and athletic trainers. Collegiate teams are typically less well equipped for such purposes (although there are some exceptions), and high schools cannot be expected to adopt such a model. As a result, it is appropriate to design different models for high school, collegiate, and professional sport settings.
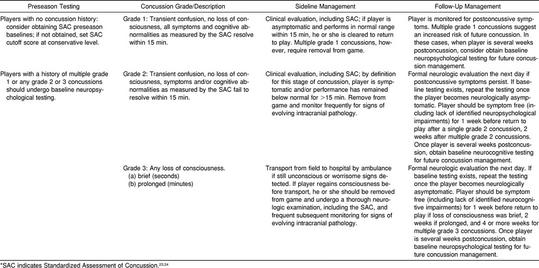
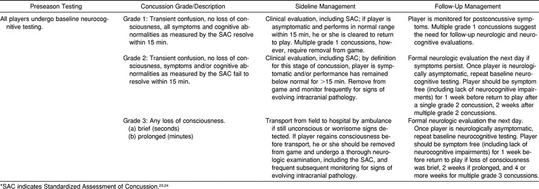
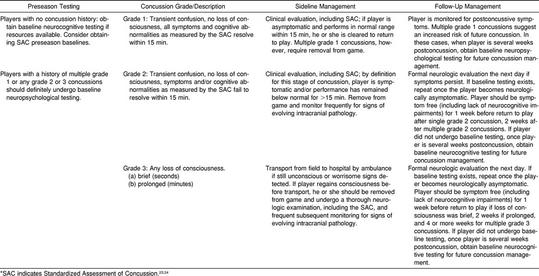
In the models detailed (Tables 2 through 4), the American Academy of Neurology guidelines21 for the management of concussion in sports are used to grade concussion level and determine return to play. Although no data suggest that one set of guidelines is inherently superior to another for this purpose, the American Academy of Neurology guidelines have the most objective criteria for differentiating between a grade 1 and grade 2 concussion (provided that a formal sideline evaluation, such as the SAC, is conducted). Differentiating a grade 1 from a grade 2 concussion is important because this provides an objective and standardized measure of the appropriateness of allowing a player to return to an ongoing game. With the use of the SAC, this differentiation can be made objectively. The models below are suggested as guidelines for implementing the various levels of neuropsychological testing (sideline, baseline, and comprehensive evaluations).
Table 2.
Algorithm for Implementation of High School–Level Model*
Table 4.
Algorithm for Implementation of Professional-Level Model*
The Model for High School–Level Concussion Management
At the high school level, obtaining baseline neuropsychological testing is probably unrealistic from a practical standpoint, at least until well-validated computerized batteries are available. The need to obtain baseline scores on the SAC is also debatable. While this practice may slightly improve the sensitivity and specificity of the SAC,26 a reasonable alternative would be to set a fairly conservative cut-off level for impairment. For example, in our total sample of 91 concussed and 1189 normal high school and collegiate athletes, an SAC score of 25 or less as a cut-off for impairment correctly identified 80% of the injured players and misidentified fewer than 30% of the normal players. This is a reasonably conservative approach that would seem to be appropriate for the high school level (Table 2). A concussion symptom checklist25 can also be useful to monitor postconcussive symptoms in a standardized way over time.
The Model for Collegiate-Level Concussion Management
Many collegiate athletic programs use a brief neurocognitive battery such as the one detailed in Table 1 to obtain baseline measures of participants in sports with a high risk for concussion. The consequences of removing key players from competition are more significant at the collegiate level than at the high school level, which also argues for a somewhat more sophisticated approach to concussion management. Most larger schools have graduate-level psychology training programs with faculty and students who can serve as a resource for facilitating baseline testing. The suggested collegiate-level model is detailed in Table 3.
Table 3.
Algorithm for Implementation of Collegiate-Level Model*
The Model for Professional-Level Concussion Management
Currently, all National Hockey League and most National Football League players undergo baseline neurocognitive testing as part of concussion management programs. All of these teams can easily obtain quality neurologic and neuropsychological consultation to help athletic trainers and team physicians with decision making regarding return-to-play status for players who have experienced concussions. Our program with the Chicago Bears was the first (to our knowledge) to involve baseline testing of an entire professional sports team, and this program has been ongoing for several years. The suggested professional-level model is detailed in Table 4.
Overall, the 3 models differ only with respect to the extent to which baseline testing is implemented in the preseason period and during the follow-up management. Obviously, these are guidelines and not practice standards. Individual athletic trainers, team physicians, and consulting neurologists and neuropsychologists may elect to deviate from these guidelines based on the circumstances of a particular case and their clinical judgment. Athletic trainers are likely to be the individuals who are responsible for coordinating the preseason, sideline, and postconcussion management protocols, and they should use these models as a starting point to determine the most appropriate protocol for their teams.
CURRENT LIMITATIONS TO THE USE OF NEUROPSYCHOLOGICAL TESTING
Although neurocognitive testing clearly has a role in the management of sport-related concussion, some factors limit the utility of this approach in detecting subtle impairments of brain function after concussion. These factors primarily involve the baseline examination, rather than the sideline examination or full-scale neuropsychological assessment. Sideline examinations have limitations due to time constraints and availability of personnel for administration of the examination; however, the SAC has proven utility in identifying neurocognitive impairments in players who are otherwise asymptomatic. Full-scale neuropsychological assessments are detailed clinical tools that should be used only for situations in which a player exhibits long-standing symptoms.
The baseline battery is arguably the most important tool in the decision-making process in managing sport-related concussion. The consulting neuropsychologist is usually called on to make a recommendation based solely on the results of this battery. In a typical scenario, the data from a postconcussive examination are compared with the data from a player's preseason (or earlier) baseline testing and reviewed for evidence of significant decline that would indicate that the player is still experiencing the effects of the concussion. This comparison is complicated by the following facts:
A certain degree of measurement error is associated with all psychological tests, such that scores may fluctuate somewhat on retesting.
The degree of this error term varies in magnitude depending on the nature of the specific test.
Practice effects associated with most cognitive tasks result in some improvement in performance from one test session to the next.
The magnitude of the practice effect can vary as a function of the individual test and as a function of the interval between testings.
The neuropsychologists involved in this interpretive process must weigh all of these factors in clinical decision making. Unfortunately, adequate empirical evidence to guide this decision making is currently lacking. Although we are usually aware of short-term (ie, days or weeks) retest reliability and practice effects for individual tests, longer-term data (months or years) are usually lacking, as are data on the effects of administering the battery multiple times over a series of weeks (which is not uncommon). As a result, a neuropsychologist is often forced to rely more heavily on clinical judgment than would be ideal in such settings.27 One approach to minimize this problem is to routinely postpone neurocognitive testing after a concussion until a player is otherwise completely asymptomatic. The rationale for this is basic: if a player is symptomatic, no further documentation of the fact that he or she has not yet recovered from a concussion is necessary. As a matter of practice, however, players at the professional level are routinely tested while still symptomatic. This almost invariably leads to one more testing session after the symptoms have resolved and obviously complicates the interpretation of the additional test session, which may be requested only a few days after the first postconcussive examination. Reserving the neurocognitive testing until players are otherwise asymptomatic is an important measure that can be taken to minimize uncontrolled variance in the test data. Studies establishing the parameters of test-retest stability and practice effects over time with baseline25 are another.
FUTURE DIRECTIONS IN THE REFINEMENT OF THESE MODELS
As indicated previously, the empirical underpinnings of the SAC examination are sufficiently firm to support its implementation as a standard tool for the sideline evaluation of concussion in a variety of settings. The management guidelines of our models follow a strategy for which we have moderate clinical certainty. The use of this type of standardized approach with objective neurocognitive measurement will enable the accumulation of evidence for evaluation of needed modifications over time. Our ultimate goal is to obtain sufficient empirical evidence to establish an accepted standard of practice.
One important route to that goal will be the refinement of our interpretation of the baseline neurocognitive test battery. A number of groups are currently researching this issue. Many investigators agree that a fully computerized battery may be the most workable approach. This approach will have the effect of making test administration and scoring fully objective, simplifying interpretation, and facilitating the exchange of baseline data for players as they move through different levels of competition or from one team to another. It will also simplify the practical aspects of obtaining baseline and follow-up testing, as a neuropsychologist will not need to be on site for the testing. Some preliminary data suggest that such an approach is feasible,28 but the clinical validity studies necessary to support the implementation of a specific battery are still lacking. Investigations of test-retest data for different time intervals, clinical validity with injured players, and criterion validity data for comparison with existing individually administered batteries will be needed to establish the sensitivity and validity of any computerized approach.
CONCLUSIONS
A number of publications over the last several years have focused on the consequences and management of sport-related concussion. In many ways, the development of various scales, guidelines, and management models have far outpaced our scientific progress in this area, and we continue to lack an empirical basis for most of our interventions. It is clear, however, that sport-related concussion has specific, short-term consequences and potential long-term effects and that neuropsychological testing has a role in the evaluation and management of players who suffer such injuries. The management models presented above are predicated on our current understanding of the short-term consequences and recovery from sport-related concussion and incorporate the most well-validated neuropsychological tools for detecting residual effects of concussion. The data that continue to accumulate across centers using these models should advance our understanding of the natural history of mild traumatic brain injury and thereby more clearly elucidate the risks involved and the most appropriate interventions for athletes who sustain concussions at all ages and levels of competition.
REFERENCES
- 1.Lindenberg R, Freytag E. Brainstem lesion characteristic of traumatic hyperextension of the head. Arch Pathol. 1970;90:509–515. [PubMed] [Google Scholar]
- 2.Kelly JP, Nichols JS, Filley CM, Lillehei KO, Rubenstein D, Kleinschmidt-DeMasters BK. Concussion in sports: guidelines for the prevention of catastrophic outcome. JAMA. 1991;226:2867–2869. doi: 10.1001/jama.266.20.2867. [DOI] [PubMed] [Google Scholar]
- 3.Albright JP, McCauley E, Martin RK, et al. Head and neck injuries in college football: an eight year analysis. Am J Sports Med. 1985;13:147–152. doi: 10.1177/036354658501300301. [DOI] [PubMed] [Google Scholar]
- 4.Powell J, Barber-Foss KD. Traumatic brain injury in high school athletes. JAMA. 1999;282:958–963. doi: 10.1001/jama.282.10.958. [DOI] [PubMed] [Google Scholar]
- 5.Dick RW. A summary of head and neck injuries in collegiate athletics using the NCAA Injury Surveillance System. In: Hoerner EF, editor. Head and Neck Injuries in Sports. Philadelphia, PA: American Society for Testing and Materials; 1994. [Google Scholar]
- 6.McQuillen JB, McQuillen EN, Morrow P. Trauma, sport, and malignant cerebral edema. Am J Forensic Med Pathol. 1988;9:12–15. doi: 10.1097/00000433-198803000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Fekete JF. Severe brain injury and death following minor hockey accidents: the effectiveness of the “safety helmets” of amateur hockey players. Can Med Assoc J. 1968;99:1234–1239. [PMC free article] [PubMed] [Google Scholar]
- 8.Cantu RC, Voy R. Second impact syndrome: a risk in any contact sport. Physician Sportsmed. 1995;23(6):27–34. doi: 10.1080/00913847.1995.11947799. [DOI] [PubMed] [Google Scholar]
- 9.Cantu RC. Second-impact syndrome. Clin Sports Med. 1988;17:37–44. doi: 10.1016/s0278-5919(05)70059-4. [DOI] [PubMed] [Google Scholar]
- 10.McCrory PR, Berkovic SF. Second impact syndrome. Neurology. 1998;50:677–683. doi: 10.1212/wnl.50.3.677. [DOI] [PubMed] [Google Scholar]
- 11.Mueller FO. Catastrophic head injuries in high school and college sports. J Athl Train. 2001;36:312–315. [PMC free article] [PubMed] [Google Scholar]
- 12.Gronwall D, Wrightson P. Cumulative effect of concussion. Lancet. 1975;2:995–997. doi: 10.1016/s0140-6736(75)90288-3. [DOI] [PubMed] [Google Scholar]
- 13.Alexander MP. Mild traumatic brain injury: pathophysiology, natural history, and clinical management. Neurology. 1995;45:1253–1260. doi: 10.1212/wnl.45.7.1253. [DOI] [PubMed] [Google Scholar]
- 14.Bream HT. Post concussion syndrome: a case study. Athl Ther Today. 1996;1:7–10. [Google Scholar]
- 15.Povlishok JT. Pathophysiology of traumatically induced axonal injury in animals and man. Ann Emerg Med. 1993;22:980–986. doi: 10.1016/s0196-0644(05)82738-6. [DOI] [PubMed] [Google Scholar]
- 16.Mayeux R, Ottman R, Tang MX, et al. Genetic susceptibility and head injury as risk factors for Alzheimer's disease among community-dwelling elderly persons and their first-degree relatives. Ann Neurol. 1993;33:494–501. doi: 10.1002/ana.410330513. [DOI] [PubMed] [Google Scholar]
- 17.Lye TC, Shores EA. Traumatic brain injury as a risk factor for Alzheimer's disease: a review. Neuropsychol Rev. 2000;10:115–129. doi: 10.1023/a:1009068804787. [DOI] [PubMed] [Google Scholar]
- 18.Stern M, Dulaney E, Gruber SB, et al. The epidemiology of Parkinson's disease: a case-control study of young-onset and old-onset patients. Arch Neurol. 1991;48:903–907. doi: 10.1001/archneur.1991.00530210029018. [DOI] [PubMed] [Google Scholar]
- 19.Cantu RC. Guidelines for return to contact sports after a cerebral concussion. Physician Sportsmed. 1986;14(10):75–83. doi: 10.1080/00913847.1986.11709197. [DOI] [PubMed] [Google Scholar]
- 20.Report of the Sports Medicine Committee. Guidelines for the Management of Concussion in Sports (revised) Denver, CO: Colorado Medical Society; 1991. [Google Scholar]
- 21.Practice parameter: the management of concussion in sport (summary statement). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 1997;48:581–585. doi: 10.1212/wnl.48.3.581. [DOI] [PubMed] [Google Scholar]
- 22.Bailes JE, Hudson V. Classification of sport-related head trauma: a spectrum of mild to severe injury. J Athl Train. 2001;36:236–243. [PMC free article] [PubMed] [Google Scholar]
- 23.McCrea M, Kelly JP, Kluge J, Ackley B, Randolph C. Standardized assessment of concussion in football players. Neurology. 1997;48:586–588. doi: 10.1212/wnl.48.3.586. [DOI] [PubMed] [Google Scholar]
- 24.McCrea M, Kelly JP, Randolph C, et al. Standardized assessment of concussion (SAC): on-site mental status evaluation of the athlete. J Head Trauma Rehabil. 1998;13:27–35. doi: 10.1097/00001199-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Lovell MR, Collins MW. Neuropsychological assessment of the college football player. J Head Trauma Rehabil. 1998;13:9–26. doi: 10.1097/00001199-199804000-00004. [DOI] [PubMed] [Google Scholar]
- 26.McCrea M. Standardized mental status testing on the sideline after sport-related concussion. J Athl Train. 2001;36:274–279. [PMC free article] [PubMed] [Google Scholar]
- 27.Barr WB. Methodologic issues in neuropsychological testing. J Athl Train. 2001;36:297–302. [PMC free article] [PubMed] [Google Scholar]
- 28.Daniel JC, Olesniewicz MH, Reeves DL, et al. Repeated measures of cognitive processing efficiency in adolescent athletes: implications for monitoring recovery from concussion. Neuropsychiatry Neuropsychol Behav Neurol. 1999;12:167–169. [PubMed] [Google Scholar]