Abstract
Objective:
To determine the incidence of concussion in high school rugby players and compare the findings with the relevant published literature.
Design and Setting:
Prospective data collection in one US high school rugby program.
Subjects:
Two teams followed for 3 years.
Measurements:
Injury rate, injury severity, and time withheld from competition.
Results:
Seventeen concussions were recorded, accounting for 25% of all reported injuries. The incidence rate for concussion was 3.8 per 1000 athlete-exposures (95% confidence interval, 2.0–5.7) or 11.3 per 100 player-seasons (95% confidence interval, 5.9–16.7). Of the 17 concussions, 14 were Cantu grade 1, 2 were grade 2, and 1 was grade 3. Concussions accounted for 25% of all days lost from rugby participation due to injury.
Conclusions:
The incidence of concussion in this study was higher than previously reported in other studies. Methodologic limitations and administrative rules that required suspension for injured players may have suppressed reporting in previous epidemiologic studies. The incidence of concussion in rugby is probably much higher than previously suggested.
Keywords: injury, epidemiology
Rugby union is a ball-carrying game somewhat similar to North American football in that both are full-body contact sports in which 2 teams compete. In rugby, however, both offensive and defensive teams take the field at the same time, the ball cannot be thrown forward, and it is illegal to block a player who is not in possession of the football. Rugby is popular in many countries, including New Zealand, Australia, Fiji, Japan, South Africa, Argentina, England, Wales, Scotland, Ireland, and France. In the United States, the game is largely played at the high school and club levels; the total playing population is estimated to be about 50 000.1 Rugby has traditionally been a game for men, but recent years have seen an explosion in the numbers of women playing the game.
Concussion is of particular concern in rugby. Participants are largely unshielded from collision forces, and the cranium is subjected to violent acceleration-deceleration and rotational forces. Mouthguards and soft-shell head protection are used by some players, but their effectiveness in preventing concussion in rugby is open to question.2,3 To complicate matters, much of the world's rugby is played in situations in which medical personnel are frequently not present. Those medical personnel who are available are often not well trained in recognizing and managing concussions. An administrative barrier also affects concussion identification and management. Under the rules of the game, as promulgated by the International Rugby Board, any player who self-reports or is diagnosed as having a concussion is subject to an automatic 3-week suspension from all competitions and team practices. This mandatory 3-week “stand-down” period is supposed to apply even when a player sustains a very mild injury and returns to a normal level of functioning within minutes. As a result of these factors, we came to suspect that many rugby concussions go unreported.
As a first step toward determining the true incidence of concussion in rugby players, we analyzed data from a Utah high school rugby program that has applied standardized and current criteria for the diagnosis and management of concussion. This database is an important source of information on high school rugby injury because the primary data collector is a certified athletic trainer (ATC), and ATCs are not widely available in high school rugby programs. We then consider the published epidemiologic data on concussion in light of the Utah data and argue that previous studies have consistently underestimated the true incidence of concussion in rugby.
METHODS
One of us (R.J.S.) is the ATC for Highland Rugby in Utah, a well-organized rugby program that has competed successfully in the United States and abroad. The program maintains a first and second team in varsity competition and averages about 16 games per season per team. Injuries that result in time lost from games or team practices and all fractures and concussions are documented in a computer database. This database is maintained exclusively by one individual (R.J.S.). Exposure data on games and team practices are also recorded in the computer database. Data from the 1998, 1999, and 2000 seasons were analyzed.
The Highland rugby medical staff strives to ensure that all concussions are identified and that these injuries are managed in accordance with current clinical recommendations. Concussion injuries are closely monitored and are frequently reviewed by a team physician. Concussions are graded using the Cantu scale.4
To compare the Highland data with previously published estimates of the incidence of concussion in rugby, one of us (S.W.M.) searched for scientific articles reporting on the incidence of rugby injury. The MEDLINE and SPORTDiscus databases were searched for any article with the strings rugby and injur* in the title, abstract, or subject header. The search was limited to articles written in English (to avoid translation costs), published since 1980, and presenting population-based data on the incidence of rugby injury and concussion. Nine such articles were identified.5–13 The reference lists of these 9 articles were examined for additional publications that met our criteria but were not listed in MEDLINE or SPORTDiscus; one additional article was located.14
Each article was reviewed and the following data extracted: information on the study population, the number of injuries, the number of concussions, the definition of injury used in the study, the number of player-seasons of follow-up, and the methods used to collect injury data. The ways in which injury rates were reported in the literature varied widely. Some authors reported rates using player-hours as the denominator, whereas others used player-games or player-seasons. Player-seasons is the number of athletes per team multiplied by the number of seasons for which the team was followed; player-games is the number of athletes per team multiplied by the number of games for which each team was followed; and player-hours is the number of athletes per team multiplied by the number of competitions followed per team multiplied by the average length of the competition in hours. All of these exposure measures are variants on the underlying epidemiologic concept of person-time at risk of injury.
To compare the various studies, the concussion rate per 100 player-seasons was calculated using the data presented in each article. Player-seasons was used as the measure of exposure because this was the only measure that could be calculated for every study. For one study,9 the number of players at risk was an approximate number only; in another7 the approximate number of players at risk had to be estimated based on information in the article. One study14 presented exposure data for only a defined subset of subjects; the concussion incidence in this subgroup had to be estimated using other information in the article.
RESULTS
Incidence and Description of Concussion Injuries in Highland Rugby
Seventeen concussions were recorded during the 3 seasons of follow-up. For comparison, the total number of injuries (concussion and nonconcussion combined) was 69. Concussions, therefore, accounted for 24.6% of all reported injuries. The incidence rate for concussion was 3.8 per 1000 athlete-exposures (95% confidence interval [CI], 2.0–5.7). Twelve of the injuries occurred in games, for a rate of 11.1 per 1000 player-games (95% CI, 4.8–17.4), and 5 occurred in practices (1.5 per 1000 player-practices; 95% CI, 0.2–2.8). Eight of the concussion injuries were to backs, and 9 were to forwards. Concussions accounted for 25.3% of all days lost from rugby participation due to injury.
Fourteen observed concussions were Cantu grade 1, 2 were grade 2, and 1 was grade 3. The grade 3 event was characterized by a 5- to 6-minute loss of consciousness, accompanied by disorientation and mild convulsions. The athlete recovered relatively quickly and returned to competition within 2 weeks. A grade 2 concussion resulted in the greatest time lost from participation. The athlete experienced dizziness, amnesia, disorientation, and headache and was withheld from competition for 71 days.
The rate for all injuries overall (concussion and nonconcussion combined) was 1.5 per 1000 athlete-exposures (95% CI, 1.2–1.9). To facilitate comparison with other studies, we also calculated rates using player-seasons as the unit of exposure. Using this measure, the incidence rate for all injury was 46.0 per 100 player-seasons (95% CI, 35.1–56.9), and for all injuries excluding concussions, the incidence rate was 34.7 (95% CI, 25.2–44.1). The concussion rate was 11.3 per 100 player-seasons (95% CI, 5.9–16.7).
Comparison With Published Studies Reporting Concussion Incidence Rates
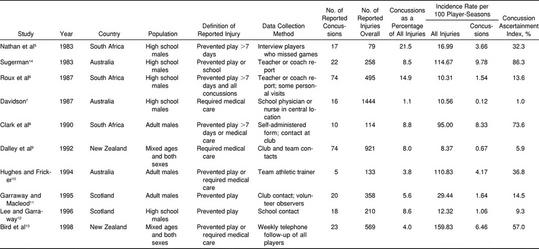
We compared our results with the published studies to determine the degree of underreporting of concussion, if any, in previously published data. Estimates of the incidence of concussion varied considerably among studies. The proportion of overall rugby injury that was classified as concussion ranged from 1% to 22%, and the incidence rate for concussion ranged from 0.1 to 8.3 per 100 player-seasons (Table).
Estimates of the Incidence of Concussion in Rugby
Under the assumption that the Highland data presented in this article are an estimate of the true incidence of concussion in these various playing populations, we constructed an index of concussion ascertainment in each study, defined as follows:
 |
Higher values of ɸi indicate greater success at identifying and collecting data on concussions; ɸi ranged from 1% (indicating that 99% of concussions were missed) to 86% (indicating that 14% were missed).
DISCUSSION
The Highland results demonstrate conclusively that it is possible, at the high school level, to collect high-quality data on rugby concussions. An ATC's involvement is the key to the success of the data collection system. Although ATCs receive instruction in the diagnosis and management of concussions, ATCs rarely work closely with a high school rugby program. The Highland data, therefore, afford us a unique insight into the incidence of concussion at this level of rugby.
Review of Previous Studies
The 10 studies reviewed herein were conducted in several different countries and covered both high school and adult playing populations. Nevertheless, the pattern is consistent, with all 10 studies producing estimates of concussion incidence well below those seen in Highland rugby. We present 2 explanations for this finding. First, the style of rugby played at Highland involves a greater risk of head impact or higher forces of the type needed to generate concussions, or both, resulting in a greater incidence of concussive injury. Second, previous researchers have underestimated the true incidence of concussion by varying degrees.
Specific characteristics of the Highland style of play are distinctive. More than half of the players have a background in North American football, which results in more emphasis on the “body-check” style of tackling. However, it seems implausible that differences in style of play could explain why rates of concussion in a Utah high school are 100 times greater than those reported in an Australian high school.7 Methodologic differences must account for most of the variation in concussion incidence among the various studies. Assuming that the Highland data represent a valid estimate of the true incidence of concussion in the playing populations detailed in the Table, the previous epidemiologic studies5–13 have probably underestimated the true incidence of concussion in rugby, in some cases by a substantial margin.
Possible Reasons for Underreporting in Previous Studies
A variety of methods were used in the 10 studies, ranging from weekly telephone contact with all players, both injured and uninjured (high-intensity follow-up), to recording all injuries reported to a central clinic (low-intensity follow-up). The definition of injury also varied among studies. We suggest that the observed concussion rate in each study is an artifact of 3 factors: (1) the actual rate of concussion in the population studied, (2) the definition of injury used in the study, and (3) the method used to collect injury data: in particular, the intensity of follow-up to ascertain injuries.
Variations in the true rate of concussion among these playing populations are probably minimal, since the basic characteristics of the game (running, tackling, passing) are similar for all populations. Intuitively, one would expect that variations in the definition of injury would influence the observed incidence rate. In fact, intensity of follow-up appears to be a stronger determinant of the observed incidence rate than the definition of injury, given that the investigators with the most restrictive injury definitions reported the highest rates for both concussion5,6,8 and overall injury.8
There is also empirical evidence of systematic underreporting of concussion injuries in rugby. In one study,6 the authors divided the participating high schools into 2 groups. The low-intensity follow-up group self-reported the injuries with little or no prompting, whereas the high-intensity follow-up group received regular personal visits as a prompt to reporting. Athletes at the high-intensity schools were 4 times more likely to report a concussion injury than those at the low-intensity schools, leading the authors to conclude that concussion in rugby is highly susceptible to underreporting.6
Providing well-trained medical professionals is essential to the identification and successful management of concussion. Unfortunately, much of the world's rugby is still played in situations in which medical personnel skilled in recognizing concussions are absent. Administrative barriers to the accurate reporting of concussion in rugby also exist. Any player diagnosed as having a concussion is subject to an automatic 3-week suspension from all competition. Originally designed to protect the player, this “stand-down” rule has probably put players at greater risk by discouraging athletes from seeking treatment and suppressing the reporting of symptoms associated with concussion. Sadly, some health care professionals have colluded in the process of discouraging the accurate reporting of concussions, as evidenced by the use of nonsensical diagnoses such as “traumatic migraine” or “loss of consciousness without concussion.” Mindful of the situation, the International Rugby Board recently modified its rules to permit an adult athlete to return to play if medically cleared for competition by a neurologist.
We believe that increasing the number of qualified health care professionals who serve rugby teams and who are trained in current techniques regarding concussion is an essential step toward improving the recognition and management of these injuries. As a first step toward improved recognition of concussions on the rugby field, we need better data on the incidence of concussion in rugby. Further epidemiologic studies that provide accurate data on concussion incidence are required.
CONCLUSIONS
Published estimates of the incidence of concussion in rugby vary widely. Using data from a large, high school–based rugby program in the United States, we have demonstrated that the incidence of concussion in rugby is probably much higher than previously suggested.
Much of the world's rugby is played in countries where there is a shortage of medical personnel well trained in recognizing and managing concussion. In addition, until recently, the International Rugby Board ruled that any player with a concussion must be suspended from active competition for 3 weeks (even for a grade 1 injury that resolved within minutes), and the effect of this rule has probably been to dampen reporting of symptoms by concussed players.
As a result of these 2 factors, previous epidemiologic studies of rugby injury have probably underestimated the incidence of concussion in rugby, in some cases by a wide margin. Efforts to better prevent, recognize, and manage these injuries need to be implemented in the game of rugby. Developing accurate incidence data will assist us in raising awareness of the problem of concussion in rugby.
ACKNOWLEDGMENTS
We thank Kristen Kucera, ATC, for assistance with literature review and manuscript preparation.
REFERENCES
- 1.Wetzler MJ, Akpata T, Albert T, Foster TE, Levy AS. A retrospective study of cervical spine injuries in American rugby, 1970 to 1994. Am J Sports Med. 1996;24:454–458. doi: 10.1177/036354659602400408. [DOI] [PubMed] [Google Scholar]
- 2.Chalmers DJ. Mouthguards: protection for the mouth in rugby union. Sports Med. 1998;25:339–349. doi: 10.2165/00007256-199825050-00006. [DOI] [PubMed] [Google Scholar]
- 3.Wilson BD. Protective headgear in rugby union. Sports Med. 1998;25:333–337. doi: 10.2165/00007256-199825050-00005. [DOI] [PubMed] [Google Scholar]
- 4.Cantu RC. Guidelines for return to contact sports after a cerebral concussion. Physician Sportsmed. 1986;14(10):75–83. doi: 10.1080/00913847.1986.11709197. [DOI] [PubMed] [Google Scholar]
- 5.Nathan M, Goedeke R, Noakes TD. The incidence and nature of rugby injuries experienced at one school during the 1982 rugby season. S Afr Med J. 1983;64:132–137. [PubMed] [Google Scholar]
- 6.Roux CE, Goedeke R, Visser GR, van Zyl WA, Noakes TD. The epidemiology of schoolboy rugby injuries. S Afr Med J. 1987;71:307–313. [PubMed] [Google Scholar]
- 7.Davidson RM. Schoolboy rugby injuries, 1969–1986. Med J Aust. 1987;147:119–120. doi: 10.5694/j.1326-5377.1987.tb133299.x. [DOI] [PubMed] [Google Scholar]
- 8.Clark DR, Roux C, Noakes TD. A prospective study of the incidence and nature of injuries to adult rugby players. S Afr Med J. 1990;77:559–562. [PubMed] [Google Scholar]
- 9.Dalley DR, Laing DR, McCartin PJ. Injuries in rugby football, Christchurch 1989. N Z J Sports Med. 1992;20:2–5. [Google Scholar]
- 10.Hughes DC, Fricker PA. A prospective survey of injuries to first-grade rugby union players. Clin J Sport Med. 1994;4:249–256. [Google Scholar]
- 11.Garraway M, Macleod D. Epidemiology of rugby football injuries. Lancet. 1995;345:1485–1487. doi: 10.1016/s0140-6736(95)91040-9. [DOI] [PubMed] [Google Scholar]
- 12.Lee AJ, Garraway WM. Epidemiological comparison of injuries in school and senior rugby. Br J Sports Med. 1996;30:213–217. doi: 10.1136/bjsm.30.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bird YN, Waller AE, Marshall SW, Alsop JC, Chalmers DJ, Gerrard DF. The New Zealand Rugby Injury and Performance Project, V: epidemiology of a season of rugby injury. Br J Sports Med. 1998;32:319–325. doi: 10.1136/bjsm.32.4.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sugerman S. Injuries in an Australian school's rugby union season. Aust J Sports Med Exerc Sci. 1983;15:5–14. [Google Scholar]