Abstract
Objective:
To identify subjects' changes in postural control during single-leg stance in the 4 weeks after acute lateral ankle sprain.
Design and Setting:
We used a 2 × 2 × 3 (side-by-plane-by-session) within-subjects design with repeated measures on all 3 factors. All tests were performed in a university laboratory.
Subjects:
Seventeen young adults (9 men, 8 women; age, 21.8 ± 5.9 years; mass, 74.9 ± 10.5 kg; height, 176.9 ± 7.1 cm) who had sustained unilateral acute mild or moderate lateral ankle sprains.
Measurements:
Measures of center-of-pressure excursion length, root mean square velocity of center-of-pressure excursions (VEL), and range of center-of-pressure excursions (RANGE) were calculated separately in the frontal and sagittal planes during 5-second trials of static single-leg stance.
Results:
We noted significant side-by-plane-by-session interactions for magnitude of center-of-pressure excursions in a given trial (PSL) (P = .004), VEL (P = .011), and RANGE (P = .009). Both PSL and VEL in the frontal plane were greater in the injured limbs compared with the uninjured limbs on day 1 and during week 2 but not during week 4, whereas sagittal-plane differences existed during all 3 testing sessions. Injured-limb, frontal-plane RANGE scores were greater than uninjured values at day 1 but not during weeks 2 or 4. No significant differences in sagittal-plane RANGE scores were seen.
Conclusions:
Postural control was significantly impaired in the injured limbs at day 1 and during week 2 after lateral ankle sprain but not during week 4. Consistent improvement in postural control measures on both injured and uninjured limbs was seen throughout the 4 weeks after ankle sprain.
Keywords: balance, stabilometry, functional testing
Lateral ankle sprains (LASs) remain one of the most frequent injuries in sports.1 The recurrence rate after LAS has been estimated to be as high as 80%.2,3 Functional instability of the ankle has been hypothesized to be a potential cause of recurrent ankle sprains, and deficits in postural control after LAS have been postulated as one manifestation of functional instability.4 Investigators have examined objective postural control measures in injured subjects after acute LAS,5–10 but routine follow-up testing to track changes in postural control after acute injury has been conducted in only a few studies.9,10
Leanderson et al9 performed a prospective study of 53 professional dancers, 6 of whom experienced moderate or severe LAS. Injured subjects had increased measures of center-of-pressure (COP) excursion amplitude and area from 0 to 12 weeks after injury compared with the uninjured dancers; however, testing was not performed at the same intervals in all subjects, and inferential statistics were not used to analyze the data. The postural control variables used were not calculated separately for the frontal and sagittal planes. Gradual improvements were seen with rehabilitation, and all injured subjects eventually returned to near preinjury levels.9
In a study of 92 subjects with ankle sprain, Holme et al10 demonstrated initial increases in COP excursion length (LEN) 6 weeks after acute injury, but a return to normal values was seen within 4 months regardless of whether or not subjects completed a supervised rehabilitation program. The postural control measure was not calculated separately for the frontal and sagittal planes. No measurements of postural control were assessed between the occurrence of injury and the ensuing 6-week assessment. Additionally, it is unclear if the structured rehabilitation sessions were begun immediately or 6 weeks after injury.10
The amplitude and velocity of frontal-plane COP excursions are significantly impaired in injured limbs compared with uninjured limbs within 8 days of acute LAS.5 To our knowledge, LEN, root mean square velocity of COP excursions (VEL), and range of COP excursions (RANGE) in both the frontal and sagittal planes at regular intervals within the first several weeks after acute LAS have not been quantified. An understanding of the typical pattern of changes in postural control in the first few weeks after LAS may serve as a useful guide to clinicians when making decisions to progress rehabilitation. Therefore, the purpose of our study was to serially assess these postural control variables between injured and uninjured ankles across the frontal and sagittal planes 1 day, 2 weeks, and 4 weeks after acute LAS.
METHODS
Subjects
Seventeen young adults (9 men, 8 women; age, 21.8 ± 5.9 years; mass, 74.9 ± 10.5 kg; height, 176.9 ± 7.1 cm) experienced acute mild or moderate LASs. All subjects were assessed by the same certified athletic trainer (J.H.). Mild sprains were classified as injury to 1 of the lateral ligaments, and moderate sprains were classified as injury to 2 of the lateral ligaments. Thirteen subjects sustained mild sprains, whereas 4 sustained moderate injuries. Nine sprains were to the right ankle, and 8 were to the left. All subjects were free of concomitant fractures or syndesmosis injuries. Subjects read and signed an informed consent form approved by the university's institutional review board (which also approved the study) before participating. We instructed all subjects in a graduated functional rehabilitation program that emphasized pain and swelling control; range-of-motion, strengthening, and balance exercises; and a gradual return to functional activities. Each subject progressed through the rehabilitation program under the guidance of either a certified athletic trainer or a licensed physical therapist.
Instrumentation
A 60 by 90-cm forceplate (Bertec Inc, Columbus, OH) measured translational forces (Fx, Fy, Fz) and moments of force (Mx, My, Mz), and COP trajectories were calculated using a custom computer program. Raw forceplate signals were amplified at 100 dB (model 4060S, Bertec), converted from analog to digital signals at 50 Hz, and filtered with a fourth-order, zero-lag, low-pass filter with a cutoff frequency of 8 Hz. We then calculated COP values using Labview software (National Instruments Inc, Austin, TX). The COP values could be resolved to an accuracy of 1 mm and were generated for both the frontal and sagittal planes.
Protocol
Subjects were asked to maintain a single-leg stance while standing barefoot on the forceplate and to stand as motionless as possible. The nonstance leg was held in approximately 30° of hip flexion and 45° of knee flexion and was not allowed to touch the stance leg during testing. Arms were folded across the chest, and testing was performed with eyes open to allow visual feedback during the maintenance of balance. If a touchdown (the nonstance leg touching the ground during data acquisition) occurred or the subject touched the nonstance leg to the stance leg, the trial was terminated and repeated. No trends were seen in terms of more repeated trials being necessary with the injured-limb stance versus the uninjured-limb stance.
The length of each trial was 5 seconds and was modeled after the methods previously reported by Goldie et al,11–13 which have been shown to be reliable and valid. Subjects performed 3 trials on each leg with a rest period of 30 seconds between trials. The order of leg testing was counterbalanced among all subjects to avoid a learning effect. Subject 1 performed all 3 left leg trials first, followed by all 3 right leg trials, whereas subject 2 had the right leg tested first and so on. All trials were conducted by the same investigator.
Subjects performed identical testing procedures on 3 occasions. Subjects were tested within 1 day of return to full weight bearing after the acute injury. All subjects performed day 1 testing within 5 days of the injury. Testing was repeated 2 weeks and 4 weeks after day 1 testing.
Dependent Measures
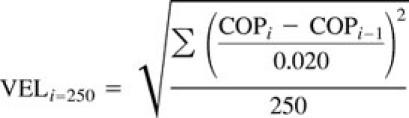
We calculated measures of LEN, VEL, and RANGE separately in the frontal and sagittal planes for each trial using Matlab 5.3 software (The MathWorks Inc, Natick, MA). We determined LEN by calculating the length of the path of the COP in the frontal and sagittal planes, respectively, throughout the entire 250-data point trial using the following equation:
The VEL of frontal and sagittal COP excursions was determined independently by dividing the length between adjacent measurements by 0.02 seconds for all 250 data points. Because the velocity could be expressed as either a positive or negative value, the VEL was calculated using the following formula: where VEL represents the magnitude of COP displacement over time and has been previously shown to be a highly reliable and valid measure of postural control.14
 |
Frontal-plane and sagittal-plane RANGE scores were calculated by subtracting the minimum COP value from the maximum COP value in both respective planes. The maximum and minimum values are the single highest and lowest COP values recorded in a given trial. The RANGE scores represent the distance in which COP excursions occur throughout a trial.
Statistical Analysis
We used a 2 × 2 × 3 (side-by-plane-by-session) within-subjects design with repeated measures on all 3 factors. Three separate, 3-factor repeated-measures analyses of variance were performed on LEN, VEL, and RANGE. For each of the 3 dependent measures, the means for the injured and uninjured limbs were calculated by averaging the 3 trials for each of the 3 testing sessions. Independent variables were side (injured, uninjured), plane (frontal, sagittal), and session (day 1, week 2, week 4). Post hoc testing was performed using univariate analyses of variance and the Tukey post hoc procedure to identify specific differences. The level of significance was set at .05 for all procedures. SPSS 8.0 for Windows (SPSS Inc, Chicago, IL) was used for the statistical calculations.
RESULTS
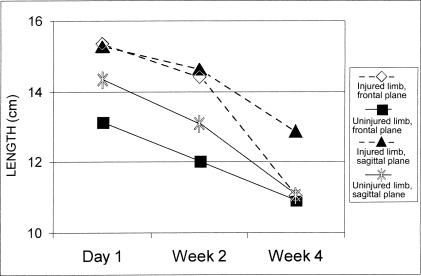
Significant side-by-plane-by-session interactions were identified for LEN (F2,32 = 6.56, P = .004), VEL (F2,32 = 5.21, P = .011), and RANGE (F2,32 = 5.50, P = .009) (Table). The interaction for LEN is explained by greater differences existing between injured and uninjured frontal-plane LEN scores at day 1 compared with sagittal-plane LEN scores (Figure 1). The LEN scores in both planes were significantly greater in injured limbs than uninjured limbs on day 1 and during week 2 (P < .05), but during week 4, only sagittal LEN was significantly different. The LEN measures gradually improved on both sides across the 3 testing sessions. The VEL scores responded very similarly to LEN scores (Figure 2). The explanation of the 3-way interaction for VEL is identical to that of LEN. The interaction for RANGE is explained by injured-limb, frontal-plane RANGE scores being significantly greater than uninjured values at day 1 (P < .05) but not during weeks 2 or 4 (P > .05) (Figure 3). Sagittal-plane RANGE scores were greater in the injured limbs compared with the uninjured limbs during all 3 sessions but not at statistically significant levels. Significant improvements were seen between sessions for VEL and LEN in both planes in the injured and uninjured limbs and for frontal-plane RANGE in the injured limbs.
Center-of-Pressure Excursion Length (LEN), Root Mean Square Velocity (VEL), and Excursion Range (RANGE) in the Frontal (X) and Sagittal (Y) Planes

Figure 1.
For center-of-pressure excursion length measures (LEN), the significant side-by-plane-by-session interaction was due to the gradual reduction in all measures except that of the injured limb in the sagittal plane.
Figure 2.
For center-of-pressure root mean square velocity measures (VEL), the significant side-by-plane-by-session interaction was due to the gradual reduction in all measures except that of the injured limb in the sagittal plane.
Figure 3.
For center-of-pressure excursion range measures (RANGE), the significant side-by-plane-by-session interaction was due to the lack of significant differences except for the frontal-plane measures on day 1.
DISCUSSION
Our results demonstrate a significant impairment in postural control within the first 2 weeks after LAS. Measurements of LEN and VEL were significantly elevated in injured limbs versus uninjured limbs at day 1 and during week 2 in the frontal plane and at day 1 and during weeks 2 and 4 in the sagittal plane. Measurements of RANGE were significantly increased in the frontal plane only at day 1 after injury. A close examination of our dependent variables may help to explain why the results were not identical for all of the measures.
The LEN results represent the sum of all COP excursions in each plane during a given trial. Individuals with impaired postural control are likely to have larger COP excursions and, thus, a larger sum of excursions throughout a trial. The VEL results represent the rate of COP excursions. Individuals with impaired balance are likely to have larger and faster COP excursions than those who are not impaired. As the velocity of COP excursions increases, it becomes more difficult, or even impossible, for the body to adequately compensate for the excursions and keep the COP within the base of support. The LEN and VEL results were very similar in our study because both reflect the magnitude of individual COP excursions during a trial. The RANGE results represent the limits of COP excursions during a trial and are constrained by the dimensions of an individual's foot. To maintain balance, COP must remain within the limits of the base of stability. If single-leg stance is maintained, measures of RANGE are limited within the finite breadth of the dimensions of the foot, whereas the measures of LEN and VEL are not constrained in a similar manner. The only significant difference in RANGE between limbs was in the frontal plane on day 1. This may be due to the limited variation possible in RANGE measures when single-leg stance is maintained throughout a trial.
Our results are consistent with previous findings5,7,9 of increases in various objective measures of postural control in injured limbs versus contralateral uninjured limbs after acute LAS. Friden et al5 reported increased frontal-plane COP excursion measures between the injured and uninjured limbs of 14 subjects between 3 and 8 days after an acute LAS. Significantly higher frontal-plane measures were also shown between the involved and uninvolved ankles of injured subjects and both limbs of healthy controls.5 Using a frontal-plane balance testing device, Golomer et al7 demonstrated significant impairments in injured limbs compared with uninjured limbs among 5 subjects between 4 and 15 days after acute LAS. Leanderson et al9 showed significant increases in COP excursion variables in injured limbs compared with uninjured limbs among 6 ballet dancers within 2 weeks of experiencing acute LAS. Each of these 6 injured dancers' postural control scores returned to preinjury levels with structured rehabilitation.9
Two studies have looked at postural control during single-leg stance in the injured limbs of subjects after acute LAS and compared them with healthy control subjects, but contralateral differences among injured subjects were not evaluated.6,8 Orteza et al6 demonstrated impaired balance on a testing device similar to that of Golomer et al7 among subjects within 6 weeks of an acute LAS compared with a group of healthy controls. Guskiewicz and Perrin8 demonstrated impaired postural control within 21 days of an acute ankle sprain among injured limbs compared with the limbs of healthy controls.
Deficits in postural control after ankle sprain may be due to several factors. Freeman et al4 originally hypothesized that balance impairments after ankle sprain were the result of impaired proprioception due to damage to joint mechanoreceptors and afferent nerve fibers, which occurs in conjunction with ligamentous damage during hyperinversion. Impaired proprioception may cause diminished or delayed response of the muscles that provide dynamic stability to the ankle joint and, thus, result in inadequate corrections to postural perturbations.15–18 Impaired postural control may also be due to altered proximal muscle activity in response to ankle injury. Subjects with ankle injuries have been shown to shift from the typical ankle strategy of balance maintenance during single-leg stance to the less efficient hip strategy of balance.19,20 Bullock-Saxton21 also demonstrated impaired ipsilateral gluteus maximus electromyographic activity in patients with a history of severe LAS, suggesting that distal injury may cause proximal changes in neuromuscular activity.
Another potential cause of impaired postural control after LAS is that lateral ligamentous injury may result in mechanical instability of the subtalar and talocrural joints and allow greater ranges of pronation and supination to occur during single-leg stance, thus resulting in greater magnitude and velocity of COP excursions.5,7–8 Interestingly, proprioceptive deficits have been reported as greatest near terminal ranges of motion.22 In the presence of excessive range of motion due to pathologic joint laxity, proprioceptive deficits may be accentuated, thus contributing to impaired postural control.
Our results show improvements in postural control measures during the first month after injury in both injured and uninjured limbs. Three plausible explanations are possible. Friden et al5 demonstrated bilateral impairments in several measures of frontal-plane postural control in subjects with acute LAS. Additionally, researchers23–27 have reported bilateral proprioceptive and neuromuscular deficits after injuries to the anterior cruciate ligament, supporting the hypothesis of a central mechanism for proprioception, neuromuscular control, and postural control. It is possible that in our sample, swelling and pain associated with the acute injury may have caused central impairments of postural control and resulted in elevated measures in both the injured and uninjured limbs. Because swelling and pain diminished in the weeks after injury, central impairments may also have diminished. These central impairments may be mediated through supraspinal or spinal levels of inhibition.28 Supraspinal inhibition could be the result of conscious perception of pain with full weight bearing during the initial sessions. Spinal-level inhibition through gamma motor neuron loop dysfunction has been previously hypothesized to cause impairment of postural control in those with ankle instability.29
A second possibility is that ankle joint effusion caused altered arthrokinematics of the ankle complex, leading to postural control impairments. Swelling after acute injury may have caused the subjects to adopt a different angle of the ankle during single-leg stance. For example, if the ankle was held in less dorsiflexion than normal, a subject's center of gravity would be held in a more posterior, and consequently more unstable, position and thus lead to elevated measures of COP excursions. Research is needed to validate this hypothesis.
The third possibility is that postural control improved bilaterally as a result of learning effects with repeated trials of balance exercises during rehabilitation and experimental testing. Several authors9,13,20,30–32 have demonstrated improved postural control after various balance and coordination training exercises in patients recovering from ankle sprain. Gauffin et al31 reported bilateral improvement in postural control after 8 weeks of ankle disk training in 10 male soccer players with a history of unilateral functional ankle instability, indicating that central impairments of postural control with pathologic ankle conditions may be reversible with adequate rehabilitation. Many, but not all, measures of postural control are estimates of variability during quiet standing.33,34 Because motor learning occurs after repetition of new motor tasks, variability tends to decrease as subjects become more efficient at the execution of the motor tasks.35 The bilateral improvements seen in our study may be due to decreased variability during single-leg stance with repetitive trials of balance exercises and tests.
It is not possible for us to unconditionally attribute the bilateral improvements seen in our study to reduction in central impairments of postural control, changes in ankle biomechanics, or motor learning in the 4 weeks after acute LAS. Most likely, a combination of all 3 contributed to improved postural control during recovery from ankle sprain. In future studies, the use of a control group may help to elucidate these issues.
Postural control measures have been used as an assessment modality to quantify functional improvement after rehabilitation of acute LAS9–10,13 and residual functional ankle instability.19,27–29,32 Significant reductions in measures of postural control have been identified in rehabilitation programs ranging from 6 to 16 weeks in length.9,20,30–32,36 Holme et al10 demonstrated reductions in COP excursion magnitude from 6 weeks to 4 months after ankle sprain in both a group of patients who completed a functional rehabilitation program and a group of patients who did not undergo supervised rehabilitation. However, subjects not undergoing supervised rehabilitation were 4 times more likely to experience a recurrent sprain within 1 year of initial injury than the group that undertook formal rehabilitation.10 Similarly, Wester et al37 reported a 2-fold reduction in recurrent ankle sprains in a group of ankle sprain–injured subjects undergoing a 12-week ankle disk–training program compared with a group not pursuing balance training.
Our results demonstrate that improvements in postural control may occur within 4 weeks of LAS when patients complete a rehabilitation program. Holme et al10 demonstrated that impairments of postural control may return to normal within 4 months after LAS, regardless of whether the subject participates in a structured rehabilitation program. Several researchers30,38–40 have demonstrated no significant deficits in objective postural control measures during single-leg stance in subjects with a history of functional ankle instability. These nonsignificant findings may be due to adaptive changes in the postural control system that occur during recovery from LAS. Although these adaptations may allow return to normal levels of instrumented postural control measures during static balance testing, these athletes may still be predisposed to recurrent episodes of ankle instability during dynamic activities. Once the initial pain and inflammation have been reduced after LAS, static balance testing in single-leg stance may not provide adequate challenge to the postural control and neuromuscular control systems to detect functional deficits. Hence, athletes who truly have functional ankle instability and may be at risk of recurrent sprain may not have significant differences in static postural-sway scores between their injured and uninjured limbs.
Elevated measures of postural control during static single-leg stance have not been shown to predict recurrent ankle sprain in athletes with prolonged functional ankle instability.38 However, the lack of balance training after acute LAS appears to predispose ankle-injured subjects to recurrent sprain.10,37 Static postural control testing may not be sensitive enough to identify functional deficits in individuals with a history of ankle sprain.10 Perhaps clinicians and investigators would be better served by using dynamic balance tests, such as the Star Excursion Balance tests41,42 or the multiple single-leg hop stabilization test,43 when attempting to functionally assess athletes with a history of ankle sprain. These tests may be more sensitive in detecting functional deficits in the entire lower extremity during dynamic activities and may be more useful in predicting the risk of individual athletes for recurrent ankle sprains. Further research in this area is warranted.
In conclusion, we demonstrated initial impairment in postural control in the first 2 weeks after acute LAS. However, almost all measures of postural control returned to normal within 4 weeks of injury. We also identified bilateral improvements in postural control as athletes recovered from their ankle sprains. These bilateral improvements may be due to either training effects or the reduced central impairment of postural control after ankle injury. Future research is needed to identify quantifiable factors that may help to predict which athletes are predisposed to developing long-standing functional instability after acute LAS.
ACKNOWLEDGMENTS
This study was funded in part by a grant from the National Athletic Trainers' Association Research and Education Foundation.
REFERENCES
- 1.Garrick JG, Requa RK. The epidemiology of foot and ankle injuries in sports. Clin Sports Med. 1988;17:29–36. [PubMed] [Google Scholar]
- 2.Smith RW, Reischl SF. Treatment of ankle sprains in young athletes. Am J Sports Med. 1986;14:465–471. doi: 10.1177/036354658601400606. [DOI] [PubMed] [Google Scholar]
- 3.Yeung MS, Chan KM, So CH, Yuan WY. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28:112–116. doi: 10.1136/bjsm.28.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Freeman MAR, Dean MRE, Hanham IWF. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678–685. [PubMed] [Google Scholar]
- 5.Friden T, Zatterstrom R, Lindstrand A, Moritz U. A stabilometric technique for evaluation of lower limb instabilities. Am J Sports Med. 1989;17:118–122. doi: 10.1177/036354658901700120. [DOI] [PubMed] [Google Scholar]
- 6.Orteza LC, Vogelbach WD, Denegar CR. The effect of molded and unmolded orthotics on balance and pain while jogging following inversion ankle sprain. J Athl Train. 1992;27:80–84. [PMC free article] [PubMed] [Google Scholar]
- 7.Golomer E, Dupui P, Bessou P. Spectral frequency analysis of dynamic balance in healthy and injured athletes. Arch Int Physiol Biomech Biophys. 1994;102:225–229. doi: 10.3109/13813459409007543. [DOI] [PubMed] [Google Scholar]
- 8.Guskiewicz KM, Perrin DH. Effect of orthotics on postural sway following inversion ankle sprain. J Orthop Sports Phys Ther. 1996;23:326–331. doi: 10.2519/jospt.1996.23.5.326. [DOI] [PubMed] [Google Scholar]
- 9.Leanderson J, Eriksson E, Nilsson C, Wykman A. Proprioception in classical ballet dancers: a prospective study of the influence of an ankle sprain on proprioception in the ankle joint. Am J Sports Med. 1996;24:370–374. doi: 10.1177/036354659602400320. [DOI] [PubMed] [Google Scholar]
- 10.Holme E, Magnusson SP, Becher K, Bieler T, Aagaard P, Kjaer M. The effect of supervised rehabilitation of strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9:104–109. doi: 10.1111/j.1600-0838.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- 11.Goldie PA, Bach TM, Evans OM. Force platform measures for evaluating postural control: reliability and validity. Arch Phys Med Rehabil. 1989;70:510–517. [PubMed] [Google Scholar]
- 12.Goldie PA, Evans OM, Bach TM. Steadiness in one-legged stance: development of a reliable force-platform testing procedure. Arch Phys Med Rehabil. 1992;73:348–354. doi: 10.1016/0003-9993(92)90008-k. [DOI] [PubMed] [Google Scholar]
- 13.Goldie PA, Evans OM, Bach TM. Postural control following inversion injuries of the ankle. Arch Phys Med Rehabil. 1994;75:969–975. [PubMed] [Google Scholar]
- 14.Geurts AC, Nienhuis B, Mulder TW. Intrasubject variability of selected force-platform parameters in the quantification of postural control. Arch Phys Med Rehabil. 1993;74:1144–1150. [PubMed] [Google Scholar]
- 15.Konradsen L, Ravn JB. Ankle instability caused by prolonged peroneal reaction time. Acta Orthop Scand. 1990;61:388–390. doi: 10.3109/17453679008993546. [DOI] [PubMed] [Google Scholar]
- 16.Karlsson J, Andreasson GO. The effect of external ankle support in chronic lateral ankle joint instability: an electromyographic study. Am J Sports Med. 1992;20:257–261. doi: 10.1177/036354659202000304. [DOI] [PubMed] [Google Scholar]
- 17.Lofvenberg R, Karrholm J, Sundelin G, Ahlgren O. Prolonged reaction time in patients with chronic lateral instability of the ankle. Am J Sports Med. 1995;23:414–417. doi: 10.1177/036354659502300407. [DOI] [PubMed] [Google Scholar]
- 18.Konradsen L, Voigt M, Hojsgaard C. Ankle inversion injuries: the role of the dynamic defense mechanism. Am J Sports Med. 1997;25:54–58. doi: 10.1177/036354659702500110. [DOI] [PubMed] [Google Scholar]
- 19.Tropp H, Odenrick P. Postural control in single-limb stance. J Orthop Res. 1988;6:833–839. doi: 10.1002/jor.1100060607. [DOI] [PubMed] [Google Scholar]
- 20.Pintsaar A, Brynhildsen J, Tropp H. Postural corrections after standardized perturbations of single limb stance: effect of training and orthotic devices in patients with ankle instability. Br J Sports Med. 1996;30:151–155. doi: 10.1136/bjsm.30.2.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bullock-Saxton JE. Local sensation changes and altered hip muscle function following severe ankle sprain. Phys Ther. 1994;74:17–31. doi: 10.1093/ptj/74.1.17. [DOI] [PubMed] [Google Scholar]
- 22.Glencross D, Thornton E. Position sense following joint injury. J Sports Med Phys Fitness. 1981;21:23–27. [PubMed] [Google Scholar]
- 23.Friden T, Zatterstrom R, Lindstrand A, Moritz U. Disability in anterior cruciate ligament insufficiency: an analysis of 19 untreated patients. Acta Orthop Scand. 1990;61:131–135. doi: 10.3109/17453679009006504. [DOI] [PubMed] [Google Scholar]
- 24.Co FH, Skinner HB, Cannon WD. Effect of reconstruction of the anterior cruciate ligament on proprioception of the knee and heel strike transient. J Orthop Res. 1993;11:696–704. doi: 10.1002/jor.1100110512. [DOI] [PubMed] [Google Scholar]
- 25.Zatterstrom R, Friden T, Lindstrand A, Moritz U. The effect of physiotherapy on standing balance in chronic anterior cruciate ligament insufficiency. Am J Sports Med. 1994;22:531–536. doi: 10.1177/036354659402200416. [DOI] [PubMed] [Google Scholar]
- 26.Jerosch J, Prymka M. Knee joint proprioception in normal volunteers and patients with anterior cruciate ligament tears, taking special account of the effect of a knee bandage. Arch Orthop Trauma Surg. 1996;115:162–166. doi: 10.1007/BF00434546. [DOI] [PubMed] [Google Scholar]
- 27.Hoffman M, Schrader J, Koceja D. An investigation of postural control in postoperative anterior cruciate ligament reconstruction patients. J Athl Train. 1999;34:130–136. [PMC free article] [PubMed] [Google Scholar]
- 28.Lephart SM, Pincivero DM, Giraldo JL, Fu FH. The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med. 1997;25:130–137. doi: 10.1177/036354659702500126. [DOI] [PubMed] [Google Scholar]
- 29.Myo-Hla K, Ishii T, Sakane M, Hayashi K. Effect of anesthesia of the sinus tarsi on peroneal reaction time in patients with functional instability of the ankle. Foot Ankle Int. 1999;20:554–559. doi: 10.1177/107110079902000903. [DOI] [PubMed] [Google Scholar]
- 30.Tropp H, Ekstrand J, Gillquist J. Factors affecting stabilometry recordings of single limb stance. Am J Sports Med. 1984;12:185–188. doi: 10.1177/036354658401200302. [DOI] [PubMed] [Google Scholar]
- 31.Gauffin H, Tropp H, Odenrick P. Effect of ankle disk training on postural control in patients with functional instability of the ankle joint. Int J Sports Med. 1988;9:141–144. doi: 10.1055/s-2007-1024996. [DOI] [PubMed] [Google Scholar]
- 32.Bernier JN, Perrin DH. Effect of coordination training on proprioception of the functionally unstable ankle. J Orthop Sports Phys Ther. 1998;27:264–275. doi: 10.2519/jospt.1998.27.4.264. [DOI] [PubMed] [Google Scholar]
- 33.Guskiewicz KM, Perrin DH. Research and clinical applications of assessing balance. J Sport Rehabil. 1996;5:45–63. [Google Scholar]
- 34.Slobounov SM, Moss SA, Slobounova ES, Newell KM. Aging and time to instability in posture. J Gerontol A Biol Sci Med Sci. 1998;53:B71–B78. doi: 10.1093/gerona/53a.1.b71. [DOI] [PubMed] [Google Scholar]
- 35.Sparrow WA, Irizarry-Lopez VM. Mechanical efficiency and metabolic cost as measures of learning a novel gross motor task. J Motor Behav. 1987;19:240–264. doi: 10.1080/00222895.1987.10735410. [DOI] [PubMed] [Google Scholar]
- 36.Mattacola CG, Lloyd JW. Effects of a 6-week strength and proprioception training program on measures of dynamic balance: a single-case design. J Athl Train. 1997;32:127–135. [PMC free article] [PubMed] [Google Scholar]
- 37.Wester JU, Jespersen SM, Nielsen KD, Neumann L. Wobble board training after partial sprains of the lateral ligament of the ankle: a prospective randomized study. J Orthop Sports Phys Ther. 1996;23:332–336. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- 38.Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sports Exerc. 1984;16:64–66. [PubMed] [Google Scholar]
- 39.Bernier JN, Perrin DH, Rijke A. Effect of unilateral functional instability of the ankle on postural sway and inversion and eversion strength. J Athl Train. 1997;32:226–232. [PMC free article] [PubMed] [Google Scholar]
- 40.Isakov E, Mizrahi J. Is balance impaired by recurrent sprained ankle? Br J Sports Med. 1997;31:65–67. doi: 10.1136/bjsm.31.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kinzey SJ, Armstrong CW. The reliability of the star-excursion test in assessing dynamic balance. J Orthop Sports Phys Ther. 1998;27:356–360. doi: 10.2519/jospt.1998.27.5.356. [DOI] [PubMed] [Google Scholar]
- 42.Hertel J, Miller SJ, Denegar CR. Intratester and intertester reliability during the Star Excursion Balance Tests. J Sport Rehabil. 2000;9:104–116. [Google Scholar]
- 43.Riemann BL, Caggiano NA, Lephart SM. Examination of a clinical method of assessing postural control during a functional performance task. J Sport Rehabil. 1999;8:171–183. [Google Scholar]