Abstract
Objective:
To describe the pathomechanics, diagnostic procedures, classification, and conservative management of the osteitis pubis syndrome in the elite soccer athlete.
Background:
Groin injuries can be the most difficult sport injuries to accurately diagnose and treat. Osteitis pubis is a painful, chronic syndrome that affects the symphysis pubis, adductor and abdominal muscles, and surrounding fascia. If misdiagnosed or mismanaged, osteitis pubis can run a prolonged and disabling course. The abdominal and adductor muscles have attachments to the symphysis pubis but act antagonistically to each other, predisposing the symphysis pubis to mechanical traction microtrauma and resulting in osteitis pubis. These antagonistic forces are most prevalent in kicking sports, such as soccer or football.
Description:
We provide a retrospective review of the demographics, diagnostic criteria and procedures, and conservative management of osteitis pubis in a professional soccer team. Osteitis pubis represented 3% to 5% of all injuries sustained by our professional soccer team between 1989 and 1997; 71.4% of those presenting with osteitis pubis were classified as having stage I disease, with a mean recovery time of 26.7 days. Midfielders were most affected by the syndrome (42.8%), whereas defenders and forwards exhibited equal incidences (25.7%) of osteitis pubis. Conservative management included nonsteroidal anti-inflammatory medication, electric stimulation, ultrasound, laser, cryomassage, and a progressive rehabilitation program.
Clinical Advantages:
Athletes who participated in this conservative management program appeared to return to full sport participation earlier and with fewer restrictions than the current literature seems to suggest. A 4-stage diagnostic criteria system was helpful in determining the course of treatment.
Keywords: groin pain, soccer injuries, pubic symphysis, rehabilitation, diagnosis
Osteitis pubis is a painful inflammatory condition of the symphysis pubis and surrounding muscle fascia caused by repeated traumatic or exertional stresses on the fascia and the joint, resulting in a traction microtrauma.1 First described by Beer in 1924,2 who presented 5 cases of osteitis pubis, and later by Spinelli in 19321 as a rectus abdominis adductoris syndrome, osteitis pubis has been recognized as one of the most chronic and debilitating syndromes to affect athletes. Although this condition has been reported as affecting basketball players and distance runners,3–5 most literature describes osteitis pubis as affecting athletes participating in kicking sports, such as soccer or football.3–5 Despite the low incidence of osteitis pubis (0.5% to 7%)5–7 in the general athletic population, it may run a prolonged and disabling course if misdiagnosed or mismanaged. Because groin injuries have been recognized as some of the most difficult sport injuries to diagnose and treat accurately, the practicing athletic trainer should understand the pathomechanics and clinical features of the osteitis pubis syndrome. The purpose of this article is to describe the diagnostic procedures, classification, and conservative management of osteitis pubis.
ANATOMY AND PATHOMECHANICS
The symphysis pubis is a fibrocartilaginous joint between the pubic rami. In addition, the abdominal muscles (rectus abdominis and external and internal oblique muscles) attach distally to the inguinal ligament, conjoined tendon, and pubic symphysis, whereas the adductor muscles (pectineus, adductor longus, adductor brevis, adductor magnus, gracilis) arise from the superior and inferior rami of the pubis. The obturator and femoral nerves with their cutaneous branches have been suggested as etiologic factors in groin pain.8 Thus, dysfunctions that affect the pubic symphysis can affect either joint mobility or the musculotendinous attachments of the abdominal or adductor muscles.
Muscle imbalances between the abdominal and hip adductor muscles have been suggested as an etiologic factor in osteitis pubis.3 Because of their attachments to the thoracic cage proximally and the pubis distally, the abdominal muscles act synergistically with the posterior paravertebral muscles to stabilize the symphysis, allowing single-leg stance while maintaining balance and contributing to the power and precision of the kicking leg.3 The adductors, because they stabilize the symphysis by bringing the lower extremity closer to the pelvis, are antagonists to the abdominal muscles. In addition, the adductor muscle group transmits mechanical traction forces toward the symphysis pubis during its activity as a prime mover in the soccer push pass, tackling, and directing the soccer ball. Imbalances between abdominal and adductor muscle groups disrupt the equilibrium of forces around the symphysis pubis, predisposing the athlete to a subacute periostitis caused by chronic microtrauma. This microtrauma exceeds the dynamic capacity of tissue for hypertrophic remodeling, resulting in tissue degeneration.9,10 Shear stress at the symphysis pubis can also cause sacroiliac dysfunction in osteitis pubis if hip internal rotation is limited in either flexion or extension. This shear stress is transmitted to the symphysis pubis, resulting in either anteroposterior movement of one half of the pelvis in relationship to the other in extension or proximal-distal movement in flexion.11
DEMOGRAPHICS
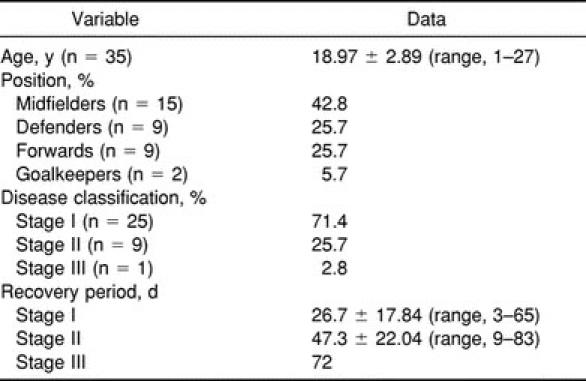
Jumping, twisting, or turning motions in sprinting, cutting, and kicking activities common to soccer and football have been implicated in the pathogenesis of osteitis pubis. The incidence of this syndrome in the general athletic population has been reported as 0.5% to 6.4%. Our demographic data collected between September 1989 and March 1997 reflect an incidence of 3% to 5% of all injuries affecting our soccer team,12 more consistent with the higher incidence of 2.5% to 7%6,7 found in the kicking sports compared with the general athletic population. Table 1 presents the demographic data for position, disease classification, and recovery period for 35 male elite soccer athletes who presented with osteitis pubis between 1989 and 1997. Although 44 athletes originally presented with osteitis pubis, 9 patients with stage IV osteitis pubis required surgical intervention, leaving 35 athletes (age, 18.97 ± 2.89 years) with stage I through III disease to undergo conservative management. Most athletes presented with stage I disease (71.4%). Not surprisingly, midfielders (42.8%) demonstrated the highest incidence, defenders and forwards were affected equally (25.7%), and goalkeepers had the lowest incidence (5.7%). These injury demographics are consistent with the pathomechanics of injury.
Table 1.
Demographic Data: Club Universidad Nacional, AC Soccer Players Presenting With Osteitis Pubis, 1989–1997
DIAGNOSIS
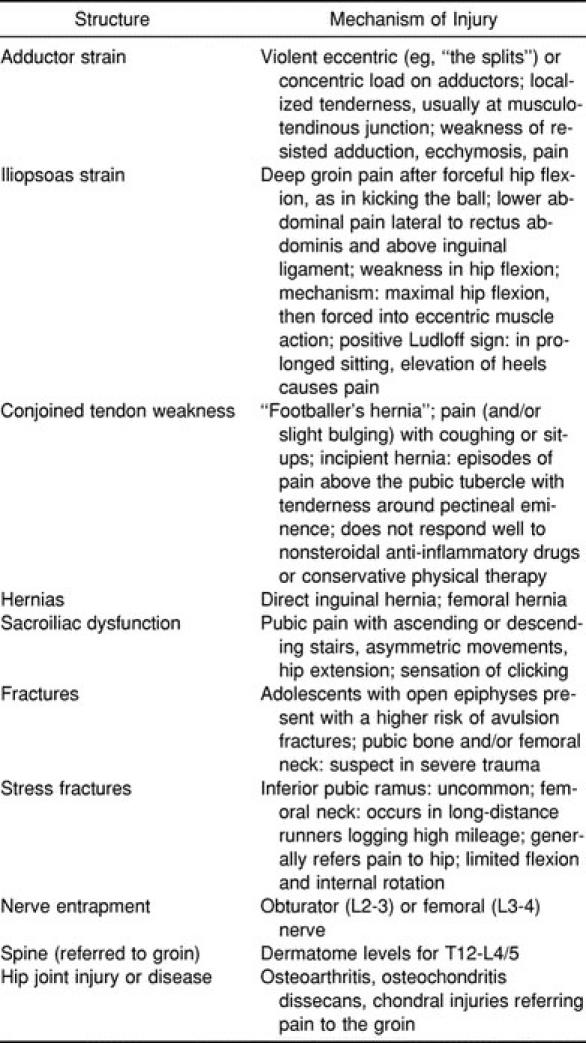
The clinical diagnosis of osteitis pubis was based on the history, physical examination, and radiographic (x-ray examination and bone scan) findings. Because the origin of groin pain is often difficult to elucidate, the sport medicine team must consider several differential diagnoses5,8,13–15 (Table 2); thus, the players were examined by the team's sports medicine specialist and orthopaedic surgeon and a general surgeon to eliminate inguinal hernia, urologic pathologic conditions, muscular injury, or other orthopaedic problems. Symptoms of osteitis pubis include pain when kicking or advancing the leg forward during the swing phase of gait, localized pain in the symphysis pubis, and pain in the lower portion of the abdominal muscle groups. The adductor muscles are evaluated bilaterally for pain and tenderness and increased muscle guarding in the muscle belly and at the musculotendinous attachments. Standard passive flexibility and resisted muscle tests of the adductor and abdominal muscle groups were performed to reproduce the painful symptoms.
Table 2.
Differential Diagnosis of Groin Pain in Athletes
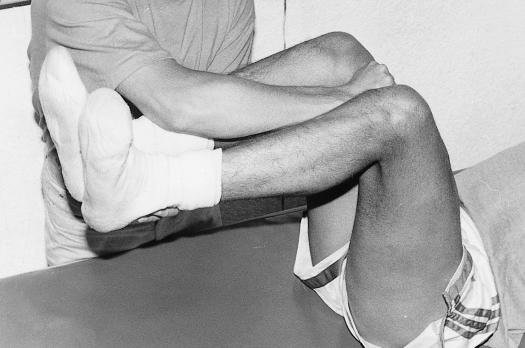
We determined tissue reactivity and stability of the pubic symphysis by the symphysis gap test (Figure 1). The athlete is in a 90°-90° hip- and knee-flexion position with the legs supported by the examiner. The athlete then performs an isometric adductor muscle contraction against the examiner's fist; painful isometric muscle action was considered a positive test result.
Figure 1.
Pubic symphysis gap test with isometric adductor contraction.
Magnified pubic radiographs (Figure 2) were taken, using a flamingo view in double- and single-leg stance positions on the right and left legs to detect pubic subluxation (>2 mm) with weight bearing and irregular borders over the symphysis and pubic rami. Technetium Tc 99m pubic bone scans were also taken to detect increased uptake in the area of the pubic symphysis (Figure 3).
Figure 2.
Radiograph of the symphysis pubis demonstrating increased space between the symphyses.
Figure 3.
Technetium Tc 99m bone scan image showing increased uptake in the pubic symphysis characteristic of osteitis pubis.
Athletes with osteitis pubis were classified into 4 stages based on their presenting clinical diagnostic features. Stage I includes unilateral symptoms involving the kicking leg and inguinal pain in the adductor muscles. The pain subsides after warm-up but recurs after the training session. Stage II consists of bilateral symptoms with inguinal pain involving the adductor muscles. The pain increases after the training session. Stage III comprises bilateral inguinal pain involving the adductor muscles and abdominal symptoms. The athlete complains of pain when kicking the ball, sprinting with rhythm or directional changes, changing positions from sitting to standing, and walking long distances. The athlete is unable to continue sport participation. Stage IV describes pain in the adductor and abdominal muscles referred to the pelvic girdle and lumbar spine with defecation, sneezing, and walking on uneven terrain. The athlete is unable to perform activities of daily living.
CONSERVATIVE MANAGEMENT
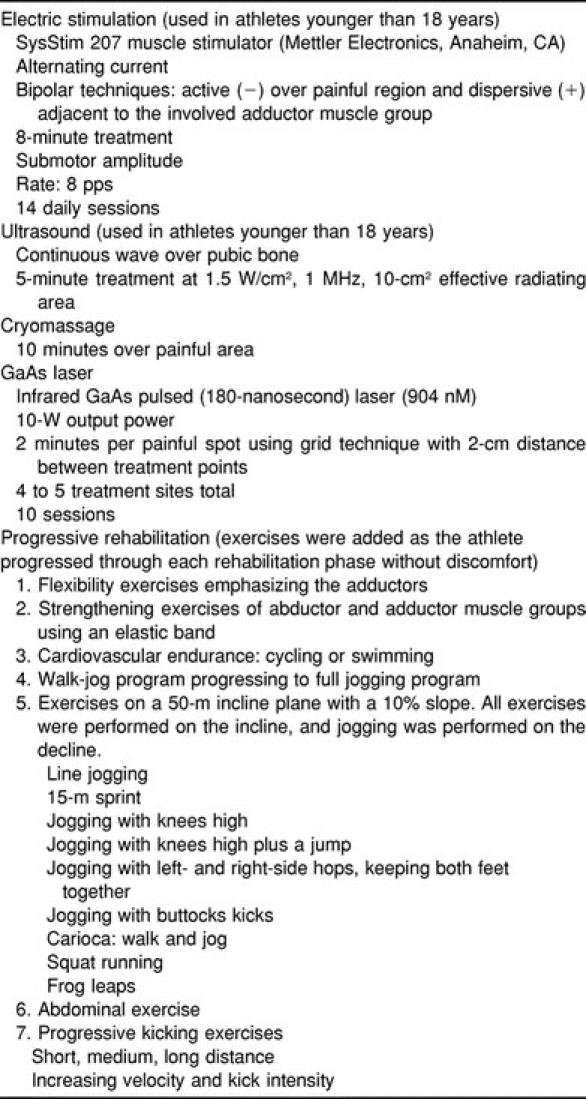
Conservative management of osteitis pubis for all athletes included pharmacologic management consisting of oral ibuprofen, 800 mg 3 times a day for 14 days; daily application of therapeutic modalities (cryomassage, laser, ultrasound, or electric stimulation) for 14 days; and a progressive rehabilitation program (Table 3). Ultrasound was not applied to athletes younger than 18 years because of concern for damage to the epiphyseal plates; alternatively, they received electric stimulation treatment.
Table 3.
Therapeutic Modalities and Rehabilitation Protocols for Osteitis Pubis
CONCLUSIONS
Our protocol has been used successfully to return athletes to a high level of sport performance. The mean time to symptom remission for the stage II group was nearly double that for the stage I group (6.7 weeks and 3.8 weeks, respectively). The sole athlete in the stage III group required 10 weeks for full recovery. These demographics suggest that early diagnosis and prompt treatment are of utmost importance to prevent this condition from becoming chronic. We have found our classification scheme helpful in improving our diagnostic accuracy and our ability to predict the course of recovery.
In addition to our approach to the conservative management of osteitis pubis, other authors1,16 have suggested nonsteroidal anti-inflammatory infiltration of the symphysis pubis. However, they do not mention the severity of the disease at the time of injection. This treatment plan, if initiated early in the syndrome, has demonstrated positive results in as little as 3 to 8 weeks in our population (compared with a range of 1 to 96 months17) without the need for invasive techniques or the athlete to modify or discontinue sport participation.
Because the symphysis pubis serves as the anterior axis for innominate rotation during normal walking18 and is also subjected to superior shear forces during single-leg stance, it seems reasonable to hypothesize this as the mechanism for osteitis pubis in the kicking athlete. Greenman18 further noted the importance of the abdominal muscles from above acting in a synergistic manner with the hip adductor muscles from below in maintaining joint integrity. Painful isometric hip adduction that occurs with the pubic symphysis gap maneuver19 is only one of a series of physical findings present in the clinical scenario of osteitis pubis. In severe cases, reflexogenic symptoms may extend to the thoracolumbar paraspinal muscles, the muscles of the pelvis and abdomen, and the anterior thigh muscles and tensor fascia latae.20
Osteitis pubis syndrome, because it is a chronic, painful syndrome that significantly impairs athletic performance, should be recognized and treated as early as possible to achieve optimal results. As with many sports injuries, prevention (in the form of adequate warm-up), flexibility exercises (particularly of the adductor muscles), conditioning exercises (especially of the abdominal muscles), correction of biomechanical problems (eg, agonist-antagonist muscle imbalances), and technique factors are of paramount importance, beginning with the preseason and extending through the playing season. Further investigation into the pathophysiology of each of the stages, causes, and triggering factors of this syndrome, as well as treatment outcomes, is warranted.
ACKNOWLEDGMENTS
We thank Soledad Echegoyen, MD, for her comments.
REFERENCES
- 1.Fanton SF. Osteitis pubis etiology and treatment. Paper presented at: Sports Medicine 1997: An NFL Perspective; May 9–11, 1997; San Francisco, CA. [Google Scholar]
- 2.Schnute WJ. Osteitis pubis. Clin Orthop. 1961;20:187–192. [PubMed] [Google Scholar]
- 3.Volpi P, Melegati G. La pubalgia del calciatore: aspetti eziopatogenetici e classificativi. Ital J Sports Traumatol. 1985;8:271–274. [Google Scholar]
- 4.McMurtry CT, Avioli LV. Osteitis pubis in an athlete. Calcif Tissue Int. 1986;38:76–77. doi: 10.1007/BF02556833. [DOI] [PubMed] [Google Scholar]
- 5.Lovell G. The diagnosis of chronic groin pain in athletes: a review of 189 cases. Aust J Sci Med Sport. 1995;1:76–79. [PubMed] [Google Scholar]
- 6.Dahan R. Rehabilitation of muscle-tendon injuries to the hip, pelvis and groin areas. Sports Med Arthrosc Rev. 1997;5:326–333. [Google Scholar]
- 7.Westlin N. Groin pain in athletes from southern Sweden. Sports Med Arthrosc Rev. 1997;5:280–284. [Google Scholar]
- 8.Hannan C, Hall T, Pyne L. Groin pain from a manipulative therapy perspective. Aust Physiother Assoc Sport Physiother Group. 1994;3:10–16. [Google Scholar]
- 9.Cabot J, Marin M, Cisa J. Pubialgia del deportista. Rev Ortop Trauma. 1985;29IB:255–258. [Google Scholar]
- 10.Hanson PG, Angevine M, Juhl J. Osteitis pubis in sports activities. Physician Sportsmed. 1978;7(10):111–114. doi: 10.1080/00913847.1978.11710782. [DOI] [PubMed] [Google Scholar]
- 11.Williams JGP. Limitation of hip joint movement as a factor in traumatic osteitis pubis. Br J Sports Med. 1978;12:129–133. doi: 10.1136/bjsm.12.3.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rodriguez C, Echegoyen S, Miguel A, Lima H. Soccer injuries: study in three seasons. J Athl Train. 1998;33:S21. [Google Scholar]
- 13.Sullivan D. Groin pain from a manipulative therapy perspective. Aust Physiother Assoc Sport Physiol Group. 1994;3:18–19. [Google Scholar]
- 14.Peterson L. Groin injuries. In: Garrett WE Jr, Kirkendall DT, Contiguglia SR, editors. The US Soccer Sports Medicine Book. Baltimore, MD: Williams & Wilkins; 1996. pp. 244–245. [Google Scholar]
- 15.Mozes M, Papa MZ, Zweig A, Horozowski H, Adar R. Iliopsoas injury in soccer players. Br J Sports Med. 1985;19:168–170. doi: 10.1136/bjsm.19.3.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holt MA, Keene JS, Graft BK, Helwig DC. Treatment of osteitis pubis in athletes: results of corticosteroid injections. Am J Sports Med. 1995;23:601–606. doi: 10.1177/036354659502300515. [DOI] [PubMed] [Google Scholar]
- 17.Fricker PA, Taunton JE, Ammann W. Osteitis pubis in athletes: infection, inflammation or injury? Sports Med. 1991;12:266–279. doi: 10.2165/00007256-199112040-00005. [DOI] [PubMed] [Google Scholar]
- 18.Greenman PE. Principles of Manual Medicine. Baltimore, MD: Williams & Wilkins; 1989. Principles of diagnosis and treatment of pelvic girdle dysfunction. [Google Scholar]
- 19.Po F, Vannucci C, Bianco M, Calvosa G. La pubalgia da sport. Int J Sports Traumatol. 1989;11:47–55. [Google Scholar]
- 20.Dvorak J, Dvorak V. In: Manual Medicine: Diagnostics. 2nd ed. Gilliar WG, Greenman PE, translators. New York, NY: Thieme Medical Publishers Inc; 1999. [Google Scholar]