Abstract
Objective:
To examine the influences of clinician technique on performance and interpretation of the Lachman test.
Design and Setting:
Blinded, controlled, and randomized-block design clinical study conducted in an athletic training laboratory classroom.
Subjects:
Twenty-two certified athletic trainer clinicians and 12 model patients.
Measurements:
We used video analyses of 3-dimensional kinematics to identify variations in clinician technique. Each clinician's technique was classified according to the demonstrated grip configuration and test style.
Results:
Clinician grip configuration was found to relate to performance and interpretation of the Lachman test. Clinicians demonstrating proximal “tibia-hand” placement were more likely to correctly perform and interpret the Lachman test than clinicians demonstrating distal tibia-hand placement.
Conclusions:
Clinicians should use the correct techniques when attempting to evaluate and interpret athletic injuries.
Keywords: subset skills, test style, grip configuration, clinical evaluation
Traditional ideas regarding clinician technique for the examination of athletic injuries have been passed from teacher to student for generations of athletic trainers. Little empirical verification documents the effectiveness of many clinical techniques, and much of clinical practice is upheld as an “art.” Anecdotal evidence and observed clinical practice of customary and time-honored movement patterns demonstrated by mentors have been adopted as doctrines in the profession of athletic training.
The manual clinical-examination skills used by athletic trainers are no less than the culmination of art form and science and cannot be simplified to mere scientific theory. However, it could be argued that a fundamental component of an evolving didactic framework for athletic training clinical education is the identification of the correct clinical technique for evaluating and interpreting athletic injuries. As such, variations in clinician technique must be explored before instructional strategies aimed at guiding student skill development are introduced.1–3 Accordingly, perhaps athletic training clinical education could benefit from the use of more applied research theory regarding human motor behavior. This study represents a first attempt in the use of 3-dimensional kinematics for the purpose of identifying aspects of clinician technique for the Lachman test.
Despite advances in technology and specialized diagnostic tests, a careful history and thorough physical examination remain the cornerstone of knee-injury evaluation.4,5 Clinical tests for anterior cruciate ligament (ACL) deficiency have been given many names, and although the descriptions of these tests are not always consistent, the Lachman test6 is often considered the most sensitive clinical test for determining injury to the ACL.6–15 Pathologic motion during most knee-ligament tests is associated with injury to a specific ligament or ligamentous complex, and although it has been suggested that experienced physicians can accurately evaluate up to 90% of ligament disruptions by clinical examination alone,16 no data are available on the influences of variation in clinical technique on the evaluation and interpretation of the Lachman test as an isolated clinical-examination procedure.
Our purpose was to examine variations in clinician technique for performance and interpretation of the Lachman test. The standard for the correct technique of Lachman test performance and interpretation was the formal description of the Lachman test, as initially introduced in the literature.6 We set out to evaluate the influences of clinician technique on selected National Athletic Trainers' Association (NATA)-established sample subset skills for performing the Lachman test.17 The identification and use of subset skills as established by the NATA reflects the notion that when introducing didactic information about a specialized clinical-examination technique, such as the Lachman test, the individual parts of that skill (ie, subset skills) should be recognized so as to facilitate student learning. Subset skills can be explained as those parts of a clinical skill that are stand-alone, measurable competencies essential to the overall proficiency of the clinical skill in its entirety (ie, the Lachman test).
The NATA-established sample subset skills for the Lachman test17 have been identified as (1) patient positioning, (2) amount of knee flexion, (3) patient relaxation, (4) hand placement, (5) application of force, (6) translation determination, and (7) end-feel determination. We addressed the selected subsets of hand placement, application of force, translation determination, and end-feel determination. This protocol was followed to allow clinicians to perform the Lachman test in a manner consistent with their clinical practice. Patient positioning, amount of knee flexion, and patient relaxation were not assessed as part of this study in order to allow clinicians to perform natural (rather than constrained) movement patterns as they carried out the Lachman test. Subsequent research to address these subsets is currently in progress. For the purposes of this study, clinical judgments of tibial translation and end feel were combined operationally (ie, grade II translation, soft end feel) to reflect the complete evaluation and interpretation of the Lachman test.
METHODS
Clinicians
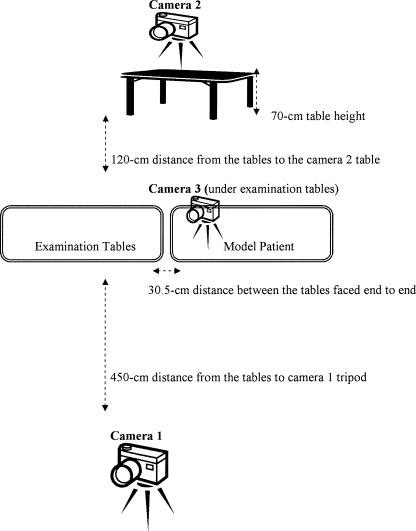
Twenty-two certified athletic trainer clinicians (14 men, 8 women; age = 33.86 ± 7.3 years; “tibia-hand” length = 18.50 ± 1.29 cm; tibia-hand width = 9.00 ± 0.59 cm; tibia-hand finger span = 20.00 ± 1.50 cm; 4 were left-hand dominant, 18 were right-hand dominant) volunteered to participate. Clinicians were trained professionals with diverse educational and experiential backgrounds. The clinicians had been certified by the NATA Board of Certification for 9.79 ± 6.53 years (range, 2 to 26 years).
The clinicians' anthropometric measurements ranged from the 50th to the 95th percentile for anthropometric estimates for adults (Table 1).18 Tibia-hand length measurements (18.50 ± 1.29 cm) and finger-span measurements (20.00 ± 1.50 cm) were in the 50th percentile, whereas hand-width measurements (9.00 ± 0.59 cm) were in the 95th percentile. The left hand is considered the tibia hand when performing the Lachman test on left knees in a manner consistent with the correct procedure.6 No significant differences were found between left- and right-hand anthropometric measurements.
Table 1.
Clinicians' Anthropometric Characteristics*
Model Patients
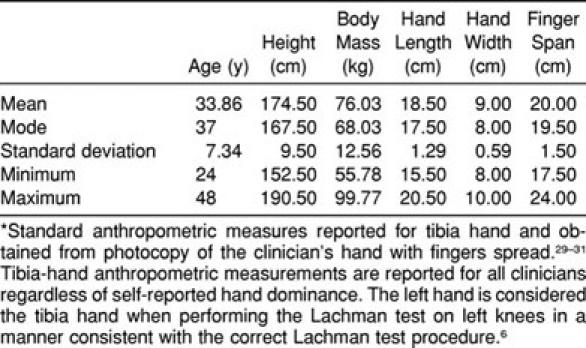
Twelve undergraduate students (5 male and 7 female subjects; age = 21.9 ± 4.5 years), medically cleared for participation in this study by an orthopaedic surgeon, served as model patients. The model patients' relevant anthropometric measurements ranged from the 50th to the 95th percentile for anthropometric estimates in adults (Table 2).18 Shank-length measurements (39.0 ± 3.0 cm) were within the 50th percentile for both male and female subjects, body mass (77.8 ± 21.9 kg) ranged from the 50th to the 95th percentile, and height (173.6 ± 9.8 cm) was comparable with the 50th percentile for male subjects and the 90th percentile for female subjects.18
Table 2.
Model Patients' Characteristics*
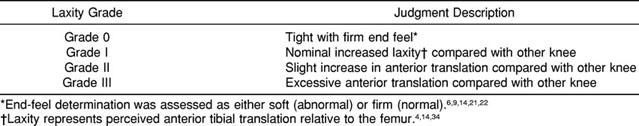
Orthopaedic diagnoses of knee-joint laxity provided criterion classification for end feel and grade of anterior instability.4,6,20–23 An illustration of orthopaedic diagnoses for involved-knee anterior laxity grade and end-feel determination for all model patients, along with a brief description of their medical histories with respect to knee injury, is provided in Table 3. The degree of pathologic laxity or instability was determined in accordance with the orthopaedic rating scale24–26 illustrated in Table 4. End-feel determination was assessed as either pathologic (soft) or normal (firm).6,9,14,22,23 The physicians' diagnoses of ACL integrity were based on a standardized history and manual physical examination documented for all model patients. Manual physical examination consisted of evaluation of range of motion and meniscal and ligamentous testing. Stability testing included valgus-varus stress testing performed at 0° and 30° of knee flexion, anterior and posterior drawer testing done at 90° of knee flexion with the foot in neutral position, and the stabilized Lachman test performed with a 15.24-cm (6-in) bolster placed under the distal thigh of the model patients to maintain knee flexion at 20° to 30°.
Table 3.
Orthopaedic Diagnoses* and Medical Histories for Model Patients
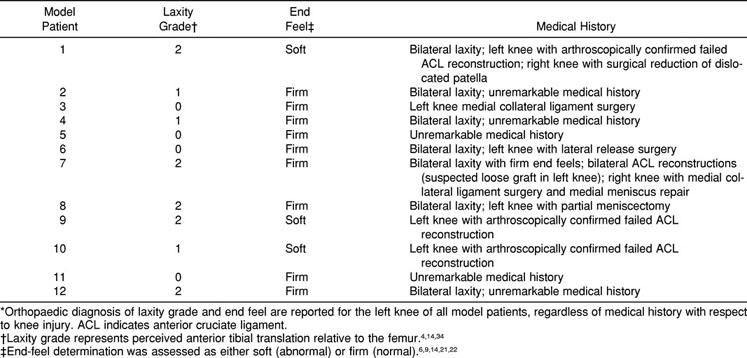
Table 4.
Anterior Instability Diagnostic Rating Scale
Model patients were asymptomatic by self-report with no physical complaints for a minimum of 3 months, regardless of their history with respect to knee injury. Six model patients had visible scars from past knee surgeries that included 1 meniscectomy, 1 meniscal repair, 1 surgical reduction of a dislocated patella, 1 lateral release surgery, 2 medial collateral ligament surgeries, and 3 arthroscopically confirmed failed ACL reconstructions (mean = 18 ± 4 months since diagnostic surgery). Four model patients had bilateral normal, healthy knees with tight, nonpathologic anterior laxity and firm end feels.
All participants in this study signed an informed consent form. All protocols were approved by the appropriate institutional review board for human subject research.
Preparatory Protocol
Reflective 3-dimensional joint markers were applied bilaterally to the participant clinicians' upper extremities to allow the recording of information about joint position and orientation of the limbs during performance of the Lachman test. The fifth metacarpophalangeal joint, the ulnar styloid process, the lateral humeral epicondyle, and the acromion process of the dominant upper limb served as bony landmarks for joint-marker attachment. A fifth joint marker was attached to the ipsilateral hip at the level of the iliac crest to serve as a reference marker.
Reflective pen markings were applied to the lateral femoral condyle of the left leg of all model patients. The tibial tuberosity and lateral malleolus provided bony landmark references to allow the recording of general information about knee-joint position and lower limb orientation, such as translation motion of the tibia with respect to the femur. An external X-Y reference structure was positioned in the background of the field of view for the main video camera (camera 1) used to record the interaction of the clinicians with the model patients in order to allow for more detailed evaluation of body-segment alignment. This arrangement was not disclosed to the clinicians and did not interfere with their technique or positioning during testing procedures.
Instrumentation
The KT1000 knee ligament arthrometer (MEDmetric, San Diego, CA) is a self-contained anterior-posterior tibiofemoral displacement-measuring instrument (Figure 1). The KT1000 is designed to quantitatively document objective clinical assessment of the sagittal-plane motions of the tibia relative to the femur. By pulling the force-sensing handle, electronic audible force levels are indicated at 6.80, 9.07, and 13.61 kg (15, 20, and 30 pounds) of anteriorly directed forces. Relative movement of the tibiofemoral joint is displayed on a dial and measured in millimeters as the relative motion between the patellar and tibial sensor pads. Intratester and intertester reliability for the KT1000 has been reported in the 90% confidence limit, with correlations between measurements as high as 0.97.21,27
Figure 1.
KT1000 knee ligament arthrometer. (Photograph courtesy of MEDmetric Corp, San Diego, CA.)
As a check for the diagnoses of knee-joint laxity, the orthopaedic surgeon obtained instrumented clinical assessments of anterior tibial translation for each of the model patients with the KT1000 (Table 5). Measurements were conducted according to the manufacturer's protocol for ACL tests.28 This method of testing has been reported to allow each knee to act as its own control.24 The KT1000 has been shown to be both valid25–27 and reliable.29–33
Table 5.
Knee-Joint Anterior Laxity (mm) Using KT1000*
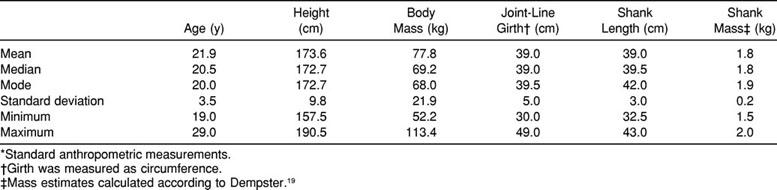
Three 60-Hz standard VHS video cameras (Panasonic, Secaucus, NJ) were used to record the events of the testing sessions: 1 camera to record the overall setup of the testing procedures and the general interaction of the clinicians with the model patients and 2 cameras to capture the clinicians' grip configurations from different angles (Figure 2). Camera 1 was secured on a tripod and positioned across the room from the examination table. Cameras 2 and 3 allowed a split-screen image for subsequent coding of the grip configurations used by the clinicians. Camera 2 was secured on a tripod situated atop a table, 70 cm in height. Camera 3 was positioned under the examination table. Rather than cutting a hole in a plinth, 2 standard-sized examination tables were placed end to end, with a 30.5-cm distance between them to allow camera 3 (positioned at a 30° angle, relative to the floor) to capture elements of the clinicians' grip configurations. This arrangement did not constrain clinician placement alongside the examination table during performance of the Lachman test.
Figure 2.
Video camera setup.
Procedures
Clinicians were tested individually in an athletic training laboratory classroom. The model patients' histories of knee injury were not revealed, and the clinicians were not permitted to ask the model patients any questions or to perform any additional manual stress tests other than the Lachman test in their examination of ACL integrity. Clinicians performed the Lachman test in a manner consistent with their clinical practice and without instructional feedback. They were asked to grade the amount of perceived tibial translation and the end-feel determination4,22,34 for the left knee of all model patients. A copy of the anterior instability rating scale used by the orthopaedic surgeon (see Table 4) was provided for all clinicians before the first model patient was presented. The injury rating scale was available throughout the testing session to accommodate clinicians who may have used a different scale in their usual practice. Clinicians were allowed to perform bilateral examinations and to repeat testing to their satisfaction before announcing their results. The number of trials was not standardized so as to allow clinicians to perform the Lachman test in a manner reflective of their usual clinical technique. Clinicians were not permitted to observe other clinicians conduct the Lachman test.
Neither the tibia nor the femur of the model patient's limb was in a fixed position during the physical examination, allowing clinicians to perform natural rather than constrained movement patterns as they performed the Lachman test. A 15.24-cm (6-in) bolster was available on request for placement under the distal thigh of the model patients. Model patients removed their shoes and socks before testing and were asked to wear shorts in order to permit the clinicians access to the midthigh region as necessary. Model patients were instructed to lie supine on the examination table and were assigned a random testing order for each clinician.
The presentation order of model patients followed a randomized-block design across clinicians and was determined using independent permutations of the list of model patients for each clinician. The clinicians performed the Lachman test and announced the results of the evaluation before being presented with another model patient. Each clinician was tested for only 1 session. Model patients were not restricted in their activities before or after the testing sessions. All testing sessions occurred between 7:00 and 9:00 PM.
A photocopy of each clinician's hands with fingers spread was made after the test trials to allow the collection of standard anthropometric measures of hand size. This method is consistent with conventional anthropometric data-collection and measurement procedures.35–37 Standardized instructions given to the clinicians were to fully spread their hands and firmly place them onto the glass without pressing hard on the glass. Although these procedures were closely monitored, we recognize that subject compliance is an assumption and not a guarantee. Photocopies of the clinicians' hands were placed on metric-scaled graph paper and measured using a metric ruler. The average of 3 measurements was recorded as the final measurement for each anthropometric reference site.
Statistical Analysis
The involved knee was operationally defined as the left knee for all model patients in this study. Side-to-side differences in KT1000 measurements refer to the mean tibial-translation test value (side-to-side difference expressed in mm) for 3 test trials and are calculated by subtracting the translation of the involved side (left knee in this study) from the uninvolved side (right knee). Positive KT1000 values indicate increased anterior tibial translation on the involved side. The analysis of KT1000 data was performed according to the manufacturer's specifications.28
The videotapes of the Lachman test trials were coded by classifying clinician technique according to 2 primary performance characteristics: grip configuration and test style. The clinicians' grip configurations were categorized according to thumb placement of the tibia hand and the number of digits along with the thumb in contact with each knee for each trial of the Lachman test. For this study, the hand used by the clinician to displace the patient's tibia relative to the femur was designated as the tibia hand. The tibia hand for examination of left knees is the left hand if the clinician follows the correct Lachman test procedure.6 Because not all clinicians demonstrated the correct Lachman technique, the hand used to translate the tibia relative to the femur was coded as the tibia hand when determining grip configuration.
In accordance with previous studies on human grip configurations,38–41 a grasp was defined as fixing the patient's knee relative to the hand(s) and relocating the patient's knee from its initial place of presentation to the final location in the act of realizing the goal of the task. Clinician grip configuration was categorized according to the clinician's thumb placement of the tibia hand with reference to the model patient's tibial tuberosity. Categories were operationally defined as condition A (Figure 3) and condition B (Figure 4). Clinicians demonstrating condition A grip used a more proximal grip configuration that placed the thumb of the tibia hand on the joint space of the model patient's knee. By comparison, clinicians demonstrating condition B grip exhibited a more distal grip configuration that placed the thumb of the tibia hand on or distal to the model patient's tibial tuberosity. Categories represent the predominant grip configuration demonstrated during at least 80% of the Lachman trials by an examiner. This type of coding system has been reported to have high interexperimenter reliability in classifying grip categories.40,41
Figure 3.
Grip configuration A.
Figure 4.
Grip configuration B.
Following similar procedures, clinician test style was categorized according to the preferred method for achieving anterior translation of the tibia relative to the femur, demonstrated as the preferred test style during at least 80% of the Lachman trials. The fixed-femur test style (FFT) condition was operationally defined as displacing the patient's tibia relative to the stabilized femur such that the “femur hand” functions as a stabilizing counterforce hand against the forward pull on the tibia by the tibia hand. Clinicians demonstrating the FFT condition generated negligible or undetectable motion of the femur.
The shifting-femur test style (SFT) condition was operationally defined as displacing the patient's tibia relative to the repositioning femur such that the clinician pushes downward on the femur with the femur hand and simultaneously pulls forward on the tibia with the tibia hand while performing the anterior translation test. The SFT condition can most easily be described as a push-pull motion to the femur and tibia, respectively. Clinicians demonstrating the SFT condition generated clearly observable motion in both the tibia and the femur of the model patients.
Analyses were carried out using the SPSS statistical software program (version 10.0 for Windows, SPSS Inc, Chicago, IL). Clinician-assessment accuracy values were computed as the combined judgments for tibial-translation grade and end-feel determination to show the collective tendencies of these values. We calculated comparisons of the effects of clinician grip configuration on the number of accurate assessments using t tests for the differences among clinicians' grip configurations (P ≤ .001). The Fisher exact test was used to test the relationship between clinician grip configuration and style of anterior translation test (P ≤ .05), the relationship between clinician grip configuration and plane of motion in which the translation test was performed (P ≤ .05), and the relationship between test style and plane of motion in which the translation test was performed (P ≤ .01).
We attempted cluster analyses and discriminant analyses to gain statistical perspective on the contributions of model patient size and mass variables in predicting the grip configurations and upper extremity joint-movement patterns used by clinicians to perform the Lachman test. These statistics could not be calculated because clinicians used the same grip configuration and the upper extremity joint-movement pattern across model patients, regardless of variation among patient size and mass factors. When there are fewer than 2 cases, at least 1 of the variables has zero variance, or there is only 1 variable in the analysis, the software will not calculate additional statistics.
RESULTS
Anterior tibial translation values obtained from the KT1000 provide a quantitative assessment of the validity of the orthopaedic surgeon's diagnoses according to the displacement categories or grades used to classify knee-joint laxity in this study (see Table 5). Statistical calculations were not performed because the comparison of orthopaedic medical diagnoses and KT1000 results showed evident agreement in the degree of pathologic laxity or instability relative to the orthopaedic rating scale (eg, grade I laxity, 3 to 5 mm; grade II laxity, 6 to 9 mm).4,14,24–26,34 For those model patients with a history of knee injury, medical diagnoses were consistent with the involved-knee KT1000 measurements rather than with the side-to-side differences.
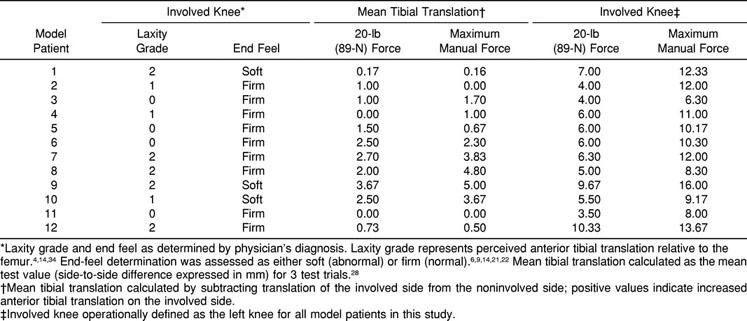
The mean number of accurate assessments with regard to category of clinician grip configuration was significant (Table 6). Clinicians demonstrating the condition A grip achieved a greater mean number of accurate assessments than those using the condition B grip. Of the certified athletic trainers sampled, 84.2% demonstrated condition B, although clinicians using condition A achieved a greater mean number of accurate assessments. Of the 4 clinicians using condition A, 75% were self-reported left-hand dominant. For this study, hand dominance was operationally defined as the hand used to sign one's name.
Table 6.
Effect of Clinician Grip Configuration on Number of Accurate Assessments*
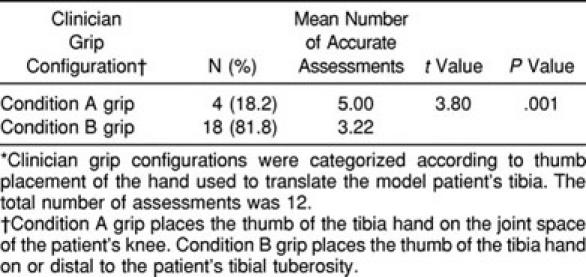
Clinician grip configuration and test style appeared to be related (Table 7). Clinicians using a grip configuration that places the thumb of the test hand on the patient's knee-joint space are more likely to use an FFT style. All clinicians using a grip configuration that placed the thumb of the tibia hand on the patient's knee-joint space used an FFT style. Fewer than half of the clinicians using a grip configuration that placed the thumb of the tibia hand on or distal to the tibial tuberosity of the patient's knee employed an FFT style.
Table 7.
The Relationship Between Clinician Grip Configuration and Test Style*
DISCUSSION
As in any area, research dealing with athletic training clinical education is in need of specific controlled definitions and research designs. Such foundational research could begin to establish the effect of a certain movement on a certain contingency of the skill-variability–performance relationship because it relates to the development of clinical skills. Insights into the influence of clinician grip configuration and technique variability during performance of the Lachman test can have important implications for the clinical instructor to improve teaching effectiveness and develop clinical skills.
A necessary and fundamental component of a developing theoretic framework for clinical-skill education is identifying clinician grip configurations and their relation to use of the appropriate technique when evaluating and interpreting an athlete's injuries. This study represents a first step toward developing a general framework in athletic training clinical education.
Orthopaedic Surgeons' Evaluations Versus KT1000 Measurements
Traditionally, the only means of evaluating ACL integrity was through manual clinical examination. The usual test for corroboration of athletic training clinical evaluations is orthopaedic diagnosis, also based on manual clinical-examination procedures. Although still considered the mainstay of knee-injury evaluation, findings from manual clinical-examination procedures such as the Lachman test are determined subjectively and are therefore open to bias and misinterpretation.
Accurate grading of tibial translation and determination of end-point character are achieved by combined proprioceptive and visual perception gained by the clinician through repetition and experience.4,6,9 If the clinician is unconvinced as to end-point distinctiveness, the test is graded positive, which can be a significant basis in interpreting the Lachman test.6,9,23 The characteristic firm end point is evidence of the check-reign effect of the primary stabilizer being tested, such as the ACL in the Lachman test.4,42–46 A “soft” or “mushy” end point occurs when restraint to translation is provided by the secondary stabilizers.6,45,47 Although both the manual clinical evaluation and the instrumented clinical assessment can provide information concerning tibial translation, only the manual clinical evaluation can detect end feel. This is an important consideration when interpreting situations involving side-to-side comparisons of nonpathologic yet noteworthy laxity combined with bilateral, firm end feels, as well as situations involving nonsignificant differences in side-to-side comparisons of minimal laxity combined with a unilateral, soft end feel. The general “rule of thumb” for interpretation of manual stress testing is that final determination is based on end-point distinctiveness rather than laxity.
Findings from manual clinical-examination procedures can be compared with values obtained from instrumented clinical-examination procedures such as the KT1000 tests. Although this comparison allows for corroboration of manual-examination findings, the results are influenced by the experience of the tester and are subject to interpretation by the reader.48,49 As with other special diagnostic techniques (such as arthrocentesis, radiography, arthrography, computed tomography, and magnetic resonance imaging) that are considered helpful procedures for evaluating acute knee injuries, the interpretation of the results is nonetheless limited in being both technology and reader dependent.50 Only arthroscopy, an invasive procedure, allows the surgeon to directly visualize all intra-articular structures in order to correctly identify and treat abnormalities.49 Each clinical test requires consistent subjective interpretation. Although perceived discrepancies between orthopaedic surgeons' evaluations and KT1000 measurements in this study should be thoughtfully considered, similar findings have been noted when investigating the association of KT1000 measurements with orthopaedic surgeons' interpretation of the Lachman test outcome for post-ACL reconstruction patients.51
Clinical Technique
Grip Configuration
Two categories of grip configuration were identified. Although our results show a relationship between grip configuration and Lachman test assessment accuracy, there is an absence of research literature addressing how the Lachman test has been used in actual practice. Proper clinician hand placement for the Lachman test was originally defined and shown by Torg et al.6 Many textbook descriptions of manual stress tests are inconsistent and occasionally contradict the figures used to illustrate testing procedures.
Test Style
The SFT condition can most easily be described as a push-pull motion. In the SFT condition, rather than using the femur hand as a stabilizing counterforce hand on the femur, the clinician pushes downward on the femur with the femur hand and simultaneously pulls forward on the tibia with the tibia hand. In the FFT condition, clinicians were able to anteriorly translate the patient's tibia on the stabilized femur with little or no motion of the femur by using the femur hand as a stabilizing counterforce hand on the femur. By contrast, clinicians demonstrating the SFT condition generated clearly observable motion in both the tibia and the femur of the patient being assessed.
As stated by Jordan,52 “to predict the effects of applying a torque around the knee joint, one must know the configuration and motion of the body.” Only then can the question(s) of how variation in clinical technique influences the evaluation and interpretation of athletic injuries be addressed. Observed, qualitative changes in clinician technique can only then be related to quantitative changes in relevant characteristics of the clinician-patient interaction associated with accurate translation and end-feel determination in manual stress testing such as the Lachman test.
CLINICAL CONSIDERATIONS
This study provides a first look at the influences of clinician technique on athletic training clinical evaluations using the Lachman test. When given the instruction to perform the Lachman test in a manner consistent with typical clinical practice, clinicians demonstrated test styles inconsistent with strict Lachman test protocol.6 On closer inspection, clinician performance variations were found to relate to NATA-established Lachman test subset skills17 and to influence the overall clinical examination.
Our findings suggest notable consequences to clinical instructors in their attempts to provide the best possible opportunities for successful learning to their students and to encourage the use of the appropriate technique during athletic training clinical evaluation. Although traditional athletic training clinical education is based on anecdotal evidence and objective evaluation of clinical-skill development, perhaps it is time to begin to provide the art of athletic training with a scientific foundation in order to advance the profession of athletic training.53–55
Adopting a theoretic framework for athletic training clinical-skill development offers possible insight for future development of theory-based, empirically tested clinical-instruction strategies with defensible support from ideology and theoretic underpinning in motor control and motor learning. Developing an understanding of the numerous variables and mechanisms that influence the appropriateness of clinician technique is essential for clinical instructors to successfully demonstrate and evaluate manual clinical-examination skills such as the Lachman test.
Because of these results, perhaps it would be prudent for clinicians to periodically review the Torg et al6 description of the Lachman test. Similarly, clinicians who experience difficulty in performing and interpreting the Lachman test may benefit from using one or more established Lachman-test modifications. Such modifications include the prone Lachman test,42 the stabilized Lachman test,43 and the drop-leg Lachman test.50 Each described test has certain advantages. For example, the stabilized Lachman test43 using a 10.16- to 15.24-cm (4- to 6-in) bolster under the distal thigh and the drop-leg Lachman test50 are useful when the patient's knee is disproportionately large in comparison with the examiner's hands.
The Lachman test is a specialized clinical test performed in a specific manner; therefore, any deviation from the exact technique should be referred to as an anterior translation test. During the physical examination, clinicians must consider that knee motion occurs simultaneously in 3 planes but is greatest in the sagittal plane.14,44,45 Tests for ACL instability require the knee to be put in positions that allow the secondary restraints to slacken.4,46,47,56 Evaluation of the ACL-deficient knee involves proper performance and interpretation of the Lachman manual-stress test.57 However, the accuracy and reliability of manual stress tests may vary according to the kinematics of the skill execution.58
LIMITATIONS
Reliability
We assumed that the clinicians' anthropometric measurements would represent a variety of clinicians' hand sizes and model patients' leg sizes typical to clinical practice. This assumption is limited to the extent that the clinicians and the model patients represented a lack of range for anthropometric measurements of hand and leg sizes. It is expected that with a greater range of hand and leg sizes, proportional relations among size-mass dimensions of the clinician-patient interaction will be uncovered to constrain clinician grip configurations during the Lachman test.
Skillfulness
We assumed that the measures of Lachman test performance and interpretation are valid measures that are typical of ordinary clinical practice. This assumption is limited in that clinical experience was measured as the number of years since certification by the NATA Board of Certification, regardless of the actual frequency or level of athletic training clinical experience. Trends in the data from these studies suggest that this is an open door for future development in the study of skillfulness and efficacy of athletic training clinical evaluations.
Clinical Diagnosis
We assumed that correct Lachman test performance and interpretation is central to accurate knee evaluation. This assumption is limited in that the results of the Lachman test as an isolated clinical-examination procedure are disputably incomplete and no single stress test is diagnostic.12
CONCLUSIONS
The NATA-established sample subset skills for the Lachman test17 are identified as (1) patient positioning, (2) amount of knee flexion, (3) patient relaxation, (4) hand placement, (5) application of force, (6) translation determination, and (7) end-feel determination. We assessed the selected subsets of hand placement, application of force, translation determination, and end-feel determination. This protocol was followed so that clinicians could perform the Lachman test in a manner consistent with their clinical practice. Patient positioning, amount of knee flexion, and patient relaxation were not assessed as part of this study in order to allow clinicians to perform natural rather than constrained movement patterns as they carried out the Lachman test. Subsequent research to address these subsets is currently in progress.
Our results indicate that even seasoned clinicians often improperly perform the Lachman test. Clinician grip configuration influenced performance and interpretation of the Lachman test. As with any clinical test for ligamentous instability, the reproducibility of the Lachman test is based on clinical knowledge and control of the variables that may affect the test.
It is important to identify the component roles of the NATA-established Lachman test sample subset skills17 in performing and interpreting the Lachman test. In this manner, clinicians are reminded of the subjective nature of this highly specialized clinical-examination procedure and encouraged to reevaluate the manner in which they perform and interpret the Lachman test.
The NATA-established Lachman test subset skills14 need to be quantified to ensure objective and consistent assessment and evaluation of Lachman test performance. Similarly, a minimum level of competence should be documented for each of the established subset skills. Clinical instructors and athletic training students must be able to easily recognize key components and important criteria of the Lachman test. To measure performance and level of clinical-skill development, document progress against a set of standards, and provide directives to improve future performance, the development of rating scales and scoring guides is necessary to outline standards for consistency in determining the level and quality of overall clinical-skill development.
These results provide strong evidence that clinician grip configurations play a major role in shaping the overall performance and interpretation of the Lachman test. There are, nonetheless, limitations to the present work that offer groundwork for future advances in the area of athletic training clinical-education research.
We assumed that the coding system we used in classifying grip categories would produce reliable results, as has been reported in research on human grip configuration.40,41 This assumption is limited to the extent that previous work using this coding technique38–41 did not encompass aspects of grip configuration in clinical practice. The coding system we used was in accordance with previous work on human grip configurations38–41 and is well known in the motor-control and motor-learning literature; however, in the future, authors studying skillfulness in athletic training clinical evaluations using this coding system may seek to reestablish the finding.
REFERENCES
- 1.Newell KM, Kugler PN, van Emmerik REA, McDonald PV. Search strategies and the acquisition of coordination. In: Wallace SA, editor. Perspectives on the Coordination of Movement. Amsterdam, Netherlands: Elsevier Science Publishers; 1989. pp. 85–122. [Google Scholar]
- 2.Newell KM, McDonald PV. Searching for solutions to the coordination function: learning as exploratory behavior. In: Stelmach GE, Requin J, editors. Tutorials in Motor Behavior II. Amsterdam, Netherlands: North-Holland; 1982. pp. 517–532. [Google Scholar]
- 3.Newell KM, Valvano J. Therapeutic intervention as a constraint in learning and relearning movement skills. Scand J Occup Ther. 1998;5:23–35. [Google Scholar]
- 4.Bonnarens FO, Drez D., Jr . Clinical examination of the knee for anterior cruciate ligament laxity. In: Jackson DW, Drez D Jr, editors. The Anterior Cruciate Deficient Knee: New Concepts in Ligament Repair. Washington, DC: Mosby; 1987. pp. 72–88. [Google Scholar]
- 5.Irrgang JJ, Safran MR, Fu FH. The knee: ligamentous and meniscal injuries. In: Zachazewski JE, Magee DJ, Quillen WS, editors. Athletic Injuries and Rehabilitation. Philadelphia, PA: WB Saunders; 1996. pp. 623–692. [Google Scholar]
- 6.Torg JS, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976;4:84–93. doi: 10.1177/036354657600400206. [DOI] [PubMed] [Google Scholar]
- 7.DeHaven KE. Arthroscopy in the diagnosis and management of the anterior cruciate ligament deficient knee. Clin Orthop. 1983;172:52–56. [PubMed] [Google Scholar]
- 8.Donaldson WF, III, Warren RF, Wickiewicz T. A comparison of acute anterior cruciate ligament examinations: initial versus examination under anesthesia. Am J Sports Med. 1985;13:5–10. doi: 10.1177/036354658501300102. [DOI] [PubMed] [Google Scholar]
- 9.Frank C. Accurate interpretation of the Lachman test. Clin Orthop. 1986;213:163–166. [PubMed] [Google Scholar]
- 10.Jackson RW. The torn ACL: natural history of untreated lesions and rationale for selective treatment. In: Feagin JA, editor. The Crucial Ligament: Diagnosis and Treatment of Ligamentous Injuries About the Knee. New York, NY: Churchill Livingstone; 1988. pp. 341–348. [Google Scholar]
- 11.Jonsson T, Althoff B, Peterson L, Renstrom P. Clinical diagnosis of ruptures of the anterior cruciate ligament: a comparative study of the Lachman test and the anterior drawer sign. Am J Sports Med. 1982;10:100–102. doi: 10.1177/036354658201000207. [DOI] [PubMed] [Google Scholar]
- 12.Katz JW, Fingeroth RJ. The diagnostic accuracy of ruptures of the anterior cruciate ligament comparing the Lachman test, the anterior drawer sign, and the pivot shift test in acute and chronic knee injuries. Am J Sports Med. 1986;14:88–91. doi: 10.1177/036354658601400115. [DOI] [PubMed] [Google Scholar]
- 13.King S, Butterwick DJ, Cuerrier J-P. The anterior cruciate ligament: a review of recent concepts. J Orthop Sports Phys Ther. 1986;8:110–122. doi: 10.2519/jospt.1986.8.3.110. [DOI] [PubMed] [Google Scholar]
- 14.Larson RL. Clinical evaluation. In: Larson RL, Grana WA, editors. The Knee: Form, Function, Pathology, and Treatment. Philadelphia, PA: WB Saunders; 1993. pp. 73–102. [Google Scholar]
- 15.Paessler HH, Michel D. How new is the Lachman test? Am J Sports Med. 1992;20:95–98. doi: 10.1177/036354659202000122. [DOI] [PubMed] [Google Scholar]
- 16.Oberlander MA, Shalvoy RM, Hughston JC. The accuracy of the clinical knee examination documented by arthroscopy: a prospective study. Am J Sports Med. 1993;21:773–778. doi: 10.1177/036354659302100603. [DOI] [PubMed] [Google Scholar]
- 17.National Athletic Trainers' Association. Clinical Instructor Educator Seminar. Providence, RI: National Athletic Trainers' Association; 2001. Jan 7, [Google Scholar]
- 18.Pheasant ST. Bodyspace: Anthropometry, Ergonomics and the Design of Work. 2nd ed. Bristol, PA: Taylor & Francis Inc; 1990. [Google Scholar]
- 19.Dempster WT. Space Requirements of the Seated Operator. Dayton, OH: Wright-Patterson Air Force Base; 1955. Wright Air Development Center Technical Report 55-159. [Google Scholar]
- 20.Daniel DM, Fritschy D. Anterior cruciate ligament injuries. In: DeLee JC, Drez D Jr, editors. Orthopaedic Sports Medicine: Principles and Practice. Philadelphia, PA: WB Saunders; 1994. pp. 1313–1361. [Google Scholar]
- 21.Daniel DM, Malcom LL, Losse G, Stone ML, Sachs R, Burks R. Instrumented evaluation of knee laxity: a comparison of five arthrometers. J Bone Joint Surg Am. 1985;67:720–726. [PubMed] [Google Scholar]
- 22.Larson RL, Grana WA. The Knee: Form, Function, Pathology, and Treatment. Philadelphia, PA: WB Saunders; 1993. [Google Scholar]
- 23.Gurtler RA, Stine R, Torg JS. Lachman test evaluated: quantification of a clinical observation. Clin Orthop. 1987;216:141–150. [PubMed] [Google Scholar]
- 24.Lintner DM, Kamaric E, Moseley JB, Noble PC. Partial tears of the anterior cruciate ligament: are they clinically detectable? Am J Sports Med. 1995;23:111–118. doi: 10.1177/036354659502300119. [DOI] [PubMed] [Google Scholar]
- 25.Anderson AF, Lipscomb AB. Preoperative instrumented testing of anterior and posterior knee laxity. Am J Sports Med. 1989;17:387–392. doi: 10.1177/036354658901700313. [DOI] [PubMed] [Google Scholar]
- 26.Bach BR, Jr, Warren RF, Flynn WM, Kroll M, Wickiewicz TL. Arthrometric evaluation of knees that have a torn anterior cruciate ligament. J Bone Joint Surg Am. 1990;72:1299–1306. [PubMed] [Google Scholar]
- 27.Daniel DM, Stone ML, Sachs R, Malcom LL. Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med. 1985;13:401–407. doi: 10.1177/036354658501300607. [DOI] [PubMed] [Google Scholar]
- 28.MEDmetric Corporation. KT1000 Knee Ligament Arthrometer User's Guide. San Diego, CA: MEDmetric Corp; 1994. [Google Scholar]
- 29.Sherman OH, Markolf KL, Ferkel RD. Measurements of anterior laxity in normal and anterior cruciate absent knees with two instrumented test devices. Clin Orthop. 1987;215:156–161. [PubMed] [Google Scholar]
- 30.Steiner ME, Brown C, Zarins B, Brownstein B, Koval PS, Stone P. Measurement of anterior-posterior displacement of the knee: a comparison of the results with instrumented devices and with clinical examination. J Bone Joint Surg Am. 1990;72:1307–1315. [PubMed] [Google Scholar]
- 31.Wroble RR, van Ginkel LA, Grood ES, Noyes FR, Shaffer BL. Repeatability of the KT100 arthrometer in a normal population. Am J Sports Med. 1990;18:396–399. doi: 10.1177/036354659001800411. [DOI] [PubMed] [Google Scholar]
- 32.Forster IW, Warren-Smith CD, Tew M. Is the KT1000 ligament arthrometer reliable? J Bone Joint Surg Br. 1989;71:843–847. doi: 10.1302/0301-620X.71B5.2584257. [DOI] [PubMed] [Google Scholar]
- 33.Highgenboten CL, Jackson A, Meske NB. Genucom, KT1000, and Stryker knee laxity measuring device comparisons: device reproducibility and interdevice comparison in asymptomatic subjects. Am J Sports Med. 1989;17:743–746. doi: 10.1177/036354658901700602. [DOI] [PubMed] [Google Scholar]
- 34.Bach BR, Jr, Warren RF, Wickiewicz TL. The pivot shift phenomenon: results and description of a modified clinical test for anterior cruciate ligament insufficiency. Am J Sports Med. 1988;16:571–576. doi: 10.1177/036354658801600603. [DOI] [PubMed] [Google Scholar]
- 35.Garrett JW. The adult human hand: some anthropometric and biomechanical considerations. Hum Factors. 1971;13:117–131. doi: 10.1177/001872087101300204. [DOI] [PubMed] [Google Scholar]
- 36.Pheasant ST. Anthropomentric estimates for British civilian adults. Ergonomics. 1982;25:993–1001. doi: 10.1080/00140138208925060. [DOI] [PubMed] [Google Scholar]
- 37.Snyder RG, Schneider LW, Owings CL, Reynolds HM, Golomb DH, Schork MA. Anthropometry in Infants, Children and Youths To Age 18 for Product Safety Designs. Warrendale, PA: Society for Automotive Engineers; 1977. [Google Scholar]
- 38.Cesari P, Newell KM. The scaling of human grip configurations. J Exp Psychol Hum Percept Perform. 1999;25:927–935. doi: 10.1037//0096-1523.25.4.927. [DOI] [PubMed] [Google Scholar]
- 39.Newell KM, Cesari P. On taking the grasping out of prehension. Motor Control. 1999;3:285–288. doi: 10.1123/mcj.3.3.285. [DOI] [PubMed] [Google Scholar]
- 40.Newell KM, Scully DM, McDonald PV, Baillargeon R. Task constraints and infant grip configurations. Dev Psychobiol. 1989;22:817–831. doi: 10.1002/dev.420220806. [DOI] [PubMed] [Google Scholar]
- 41.Newell KM, Scully DM, Tenenbaum F, Hardiman S. Body scale and the development of prehension. Dev Psychobiol. 1989;22:1–13. doi: 10.1002/dev.420220102. [DOI] [PubMed] [Google Scholar]
- 42.Feagin JA. The Crucial Ligaments: Diagnosis and Treatment of Ligamentous Injuries About the Knee. New York, NY: Churchill Livingstone; 1988. Principles of diagnosis and treatment; pp. 3–14. [Google Scholar]
- 43.Wroble RR, Lindenfeld TN. The stabilized Lachman test. Clin Orthop. 1988;237:209–212. [PubMed] [Google Scholar]
- 44.Daniel DM, Stone ML. Diagnosis of knee ligament injury: tests and measurements of joint laxity. In: Feagin JA, editor. The Crucial Ligaments: Diagnosis and Treatment of Ligamentous Injuries About the Knee. New York, NY: Churchill Livingstone; 1988. pp. 287–293. [Google Scholar]
- 45.Nordin M, Frankel VH. Basic Biomechanics of the Musculoskeletal System. Philadelphia, PA: Lea & Febiger; 1989. [Google Scholar]
- 46.Butler DL, Noyes FR, Grood ES. Ligamentous restraints to anterior-posterior drawer in the human knee: a biomechanical study. J Bone Joint Surg Am. 1980;62:259–270. [PubMed] [Google Scholar]
- 47.Grood ES, Suntay WJ, Noyes FR, Butler DL. Biomechanics of knee-extension exercise: effect of cutting the anterior cruciate ligament. J Bone Joint Surg Am. 1984;66:25–34. [PubMed] [Google Scholar]
- 48.Torzilli PA, Greenberg RL, Insall JN. An in vivo biomechanical evaluation of anterior-posterior motion of the knee: roentgenographic measurement technique, stress machine, and stable population. J Bone Joint Surg Am. 1981;63:960–968. [PubMed] [Google Scholar]
- 49.Hughston JC, Andrews JR, Cross MJ, Moschi A. Classification of knee ligament instabilities, part I: the medial compartment and cruciate ligaments. J Bone Joint Surg Am. 1976;58:159–172. [PubMed] [Google Scholar]
- 50.Adler GG, Hoekman RA, Beach DM. Drop leg Lachman test: a new test of anterior knee laxity. Am J Sports Med. 1995;23:320–323. doi: 10.1177/036354659502300312. [DOI] [PubMed] [Google Scholar]
- 51.Tyler TF, McHugh MP, Gleim GW, Nicholas SJ. Association of KT-1000 measurements with clinical tests of knee stability 1 year following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1999;29:540–545. doi: 10.2519/jospt.1999.29.9.540. [DOI] [PubMed] [Google Scholar]
- 52.Jordan MI. Handbook of Perception and Action. Vol 2. Academic Press Ltd; 1996. Computational aspects of motor control and motor learning; pp. 71–120. [Google Scholar]
- 53.Davies GJ. The need for critical thinking in rehabilitation. J Sport Rehabil. 1995;4:1–22. [Google Scholar]
- 54.Omohundro J. John Omohundro: in his own words: advice for a dynamic profession. Pro Football Athl Train. 2000;18(1):1–6. [Google Scholar]
- 55.Rothstein JM. Disciplines, demigods, and data. Phys Ther. 1988;78:1044–1045. [Google Scholar]
- 56.Noyes FR, Grood ES, Torzilli PA. Current concepts review: the definitions of terms for motion and position of the knee and injuries of the ligaments. J Bone Joint Surg Am. 1989;71:465–472. [PubMed] [Google Scholar]
- 57.Malone T, Kegerreis ST. Physical Therapy of the Knee. New York, NY: Churchill Livingstone; 1988. [Google Scholar]
- 58.Hurley WL, Newell KM, Buckley WE. Intervention strategies in athletic training clinical education: the influence of grip configurations and compensatory movement patterns in clinical skill development. Paper presented at: National Athletic Trainers' Association 2001 Educators' Conference; January 19–21, 2001; Fort Worth, TX. [Google Scholar]