Abstract
Objectives:
To identify methods used by athletic trainers to assess concussions and the use of that information to assist in return-to-play decisions and to determine athletic trainers' familiarity with new standardized methods of concussion assessment.
Design and Setting:
A 21-item questionnaire was distributed to attendees of a minicourse at the 1999 National Athletic Trainers' Association Annual Meeting and Clinical Symposia entitled “Use of Standardized Assessment of Concussion (SAC) in the Immediate Sideline Evaluation of Injured Athletes.”
Subjects:
A total of 339 valid surveys were returned by the attendees of the minicourse.
Measurements:
We used frequency analysis and descriptive statistics.
Results:
Clinical examination (33%) and a symptom checklist (15.3%) were the most common evaluative tools used to assess concussions. The Colorado Guidelines (28%) were used more than other concussion management guidelines. Athletic trainers (34%) and team physicians (40%) were primarily responsible for making decisions regarding return to play. A large number of respondents (83.5%) believed that the use of a standardized method of concussion assessment provided more information than routine clinical and physical examination alone.
Conclusions:
Athletic trainers are using a variety of clinical tools to evaluate concussions in athletes. Clinical evaluation and collaboration with physicians still appear to be the primary methods used for return-to-play decisions. However, athletic trainers are beginning to use standardized methods of concussion to evaluate these injuries and to assist them in assessing the severity of injury and deciding when it is safe to return to play.
Keywords: mild brain injury, grading scales, head injury, evaluation
Although cerebral concussion has historically been an injury common to most contact and collision sports, only recently has the topic garnered increased interest from clinicians, researchers, the media, and sport-governing bodies. This shift is perhaps most clearly illustrated by the volume of research publications, continuing education workshops, and features by the print and electronic media on concussion in athletes relative to 10 years ago. The public health concern about concussion in sports has also resulted in more research grant funding available to study the assessment and management of concussion in sports. Currently, researchers in several major, large-scale studies are exploring these issues at the high school, collegiate, and professional levels, both in the United States and internationally.
Numerous individuals and organizations have published recommendations or guidelines for the management of concussion in sports.1–3 Although investigators in several ongoing studies are attempting to identify factors that predict outcome and clarify the length of time necessary for adequate recovery after injury, current guidelines are based on consensus opinion of physicians and health care practitioners in the absence of empirical data. Some question exists about the level of consensus within the sports medicine community regarding certain aspects of different guidelines (eg, injury classification criteria, required time to withhold from competition after injury, etc). Past surveys4 suggest that most athletic trainers do not adhere to any specific concussion classification system or return-to-play guidelines in the clinical decision-making process.
In 1994, the National Athletic Trainers' Association (NATA) Research and Education Foundation sponsored a summit on mild brain injury in sports. Since the summit, several advancements have been made in the assessment of concussion in athletes. Published studies5,6 have highlighted the value of immediate, sideline, standardized mental status testing after concussion to clarify the acute neurocognitive effects of injury and to establish an index of severity for tracking recovery. Researchers7–11 have also discovered the importance of assessing subtle deficits in balance and postural stability that may indicate concussion. The aim of standardized cognitive status and postural stability testing on the sideline immediately after injury is to reduce the amount of guesswork often encountered by sports medicine clinicians in assessing concussion during the acute stage. Studies12–16 have also demonstrated the benefits of using more extensive neuropsychological testing to clarify the persistent effects of concussion, track recovery, and make more informed decisions regarding return to play after injury. Aside from the obvious advantages of more accurate assessment methods, some researchers have expressed concerns about the potential misuse of these methods to return a player to competition earlier than what is deemed to be “safe” according to current practice standards.
The impact of recent research developments, continuing education offerings, media coverage, and various injury management policies on the attitudes and practice standards held by athletic trainers with respect to sports concussion is not clear. The purpose of our study was to clarify the methods used to assess concussions and the use of that information for making return-to-play decisions by athletic health care providers. This survey was also designed to determine athletic trainers' familiarity with and use of standardized methods of concussion assessment, including the Balance Error Scoring System (BESS), Standardized Assessment of Concussion (SAC), and neuropsychological testing.
METHODS
Instrument
A 21-item questionnaire was developed for the purpose of identifying athletic trainers' use of various concussion evaluation tools and to determine if patterns of use vary across practice settings. A panel of athletic trainers and neuropsychologists, considered experts in the current trends of concussion assessment and management, constructed the questionnaire and reviewed it for completeness. The questionnaire consisted of 5 demographic questions to ascertain level of education, certification status, employment position and setting, and sports for which the athletic trainer provided clinical coverage. Concussion-related questions addressed the number of concussions evaluated per year, methods used to assess and grade concussions, and how these methods affect return-to-play decision making by the sports medicine staff.
Subjects
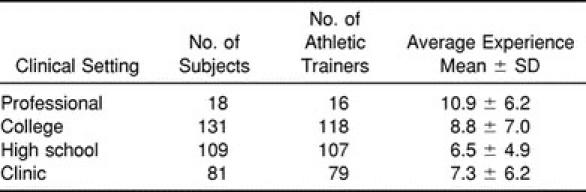
The questionnaire was distributed to approximately 900 attendees of a minicourse at the 1999 NATA Annual Meeting and Clinical Symposia entitled “Use of the Standardized Assessment of Concussion (SAC) in the Immediate Sideline Evaluation of Injured Athletes.” Attendees were given a questionnaire on arrival at the seminar and asked to complete the questionnaire before the lecture. A total of 403 completed surveys were voluntarily returned at the end of the session. For ease of comparison, completed surveys were then grouped according to setting of primary clinical responsibility. Surveys on which respondents failed to select a single answer to the question concerning setting of clinical responsibility were considered invalid, resulting in a final sample of 339 subjects. Table 1 describes this sample, grouped by clinical setting according to certification status and years of experience. Variations on sample size throughout the study occurred because not all respondents answered all questions on the survey. We used basic descriptive statistics to describe the population and clinical practice parameters. Analysis of variance was used to determine significant differences between number of concussions evaluated per year by clinical setting.
Table 1.
Athletic Trainer Distribution by Setting and Experience
RESULTS
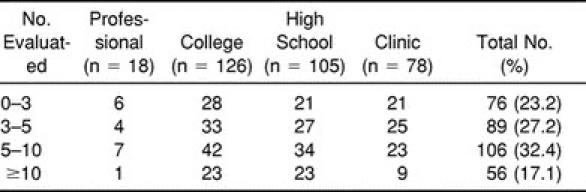
Table 2 presents a frequency distribution of the average number of concussions per year evaluated by athletic trainers in their respective employment settings. The mean (±SD) number of concussions evaluated per year was 7.04 (±5.0). Analysis of variance revealed no significant differences in the number of concussions evaluated per year by clinical setting (F3,323 = 1.374, P = .25).
Table 2.
Number of Concussion Evaluations per Year by Setting
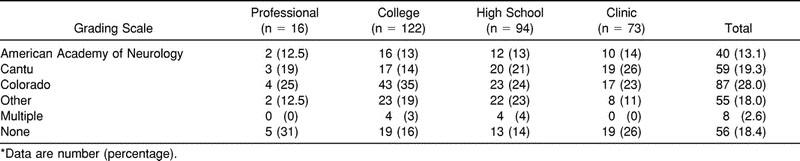
More respondents reported using the Colorado Guidelines (28%) than the American Academy of Neurology, Cantu, or other specific set of injury management guidelines (Table 3). More than 18% of the total respondents reported currently not using any type of concussion grading scale or return-to-play guidelines, whereas only a small percentage (2.6%) reported using more than a single set of guidelines. Further analysis by sport revealed that a relatively high percentage of athletic trainers did not report using grading scales in contact sports such as football (n = 44, or 16.4%), ice hockey (n = 10, or 17.2%), wrestling (n = 25, or 14.3%), lacrosse (n = 42, or 16.3%), and men's soccer (n = 39, or 17.0%).
Table 3.
Primary Grading Systems Used for Concussion by Setting*
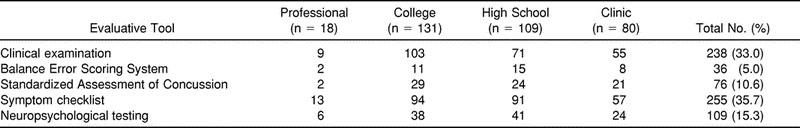
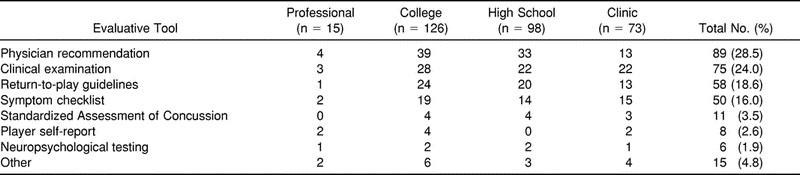
Clinical examination (n = 238, or 33%) and a symptom checklist (n = 255, or 15.3%) were the most common evaluative tools used to assess concussion (Table 4). A significant number of respondents also reported using various standardized assessment methods, including SAC (10.6%), BESS (5%), and neuropsychological testing (15.3%). Twenty-five percent of the athletic trainers surveyed had access to a neuropsychologist for consultation after concussion, and, of those who had access, 40% routinely referred their athletes to these professionals for further evaluation. A large number of respondents (86.2%) believed that athletic trainers should be trained to administer neuropsychological tests to assess concussion.
Table 4.
Evaluative Tools Used in the Assessment of Concussion
Athletic trainers (34%) and team physicians (40%) were primarily responsible for clinical decision making regarding return to play after concussion. In contrast, very few respondents indicated that decisions are primarily made by outside physicians (12%), coaches (2%), players (<1%), or parents (<1%). Respondents reported relying most frequently on physician recommendations (27.6%), clinical examination findings (23.3%), return-to-play guidelines (18%), and symptom checklists (15%) when making decisions about return to play after injury (Table 5). Fewer than 5% of the respondents reported using any single form of standardized assessment as the stand-alone method relied on most in making decisions regarding return to play after concussion.
Table 5.
Principal Evaluative Tools Used in the Return-to-Play Decision After Concussion
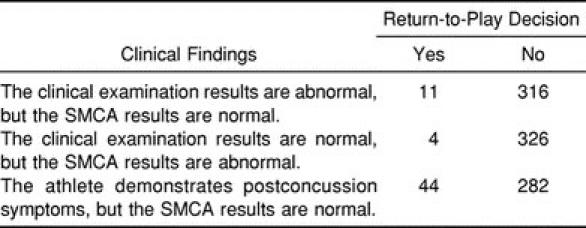
A large number of respondents (84%) believed that standardized methods of concussion assessment (SMCA) provide more information than a routine clinical or physical examination alone. Forty-seven percent of the sample believed that this information would likely result in a player's being withheld longer from competition after injury, whereas only 21% thought that a player might return to play sooner based on this information. Most respondents (97%) indicated that they would not return an athlete to play when results from an SMCA were normal, but the clinical examination results were abnormal. Nearly all respondents (99%) said they would not return an athlete still experiencing postconcussion symptoms (Table 6). Eighty-six percent of respondents indicated that they would not allow the athlete to return to play when the clinical examination results were normal, but the results of standardized assessment measures were abnormal. Twenty-four percent of the athletic trainers thought that the information from standardized methods of concussion assessment could potentially be misused to allow a player to return to competition earlier than what would be deemed “safe” after concussion.
Table 6.
Clinical Assessment and Standardized Methods of Concussion Assessment (SMCA) in Return-to-Play Decisions
Of the small percentage (17%) of athletic trainers who currently use the SMCA in the initial assessment of concussion, most (86%) believed the instrument provides a more accurate assessment than routine clinical examination alone. Sixty-three percent of this subsample indicated that they were more likely to withhold a player from return to competition as a function of using the SMCA information, whereas 30% said the results would have no effect on their return-to-play decision.
DISCUSSION
This survey was designed to clarify the current trends in clinical practice by athletic trainers in the assessment and management of sport-related concussion. The collective responses represent the opinions and practice patterns reported by a relatively large sample of certified athletic trainers and other health care providers responsible for coverage in a variety of male and female sports. These data certainly substantiate the notion that athletic trainers routinely encounter concussion in the care of their athletes during a sport season. On average, our sample reported being responsible for evaluating and managing more than 7 concussions per year across a wide range of sports with and without recognized risk of head injury.
Athletic trainers and team physicians were most often directly responsible for decisions regarding an athlete's readiness to return to play after concussion. Coaches, players, and parents are seldom primarily responsible for return-to-play decisions. Although routine clinical examination and input from an attending physician remain the primary sources of information used to make decisions about return to play after concussion, the specific criteria on which decisions are based remain less clear. More clinicians appear to be using a multidimensional approach to concussion assessment and management, which incorporates clinical examination findings, concussion grading scale criteria, symptom checklist information, return-to-play guidelines, standardized tests, and neuroimaging studies.
It can safely be said that more athletic trainers are looking to standardized cognitive assessment, postural stability testing, and formal neuropsychological testing to guide their clinical decision making compared with several years ago. Our results indicate that a small but increasing number of athletic trainers currently use SMCA and that most (86%) believe these measures significantly improve the accuracy of their evaluation. A promising finding is that athletic trainers are receptive to the use of standardized assessment methods, despite also reporting that results from these measures may actually cause a player to be withheld longer from competition after concussion than if they were not used. Although athletic trainers are beginning to recognize the value of standardized methods of assessment, it is vital that they understand the importance of obtaining baseline measurements with which postinjury comparisons can be made. Although time consuming, the process can be made more manageable when it is incorporated into preseason physical examinations and screenings.
We found no current consensus for any single preferred concussion grading scale and set of return-to-play guidelines among athletic trainers. More respondents reported using the Colorado Guidelines than the Academy of Neurology guidelines, the Cantu guidelines, or any other system. Nearly 20% of respondents indicated that they are not currently using any specific concussion grading scale or return-to-play guidelines. Most agree that it is not critical that all clinicians adhere to the same specific set of classification criteria but rather that each sports medicine staff have a systematic means of concussion assessment and management to avoid making “on-the-fly” decisions that could result in undue risks. The current survey results are favorable in the sense that more athletic trainers appear to be using some form of systematic injury management recommendations than was the case several years ago. Clinicians should recognize that most concussion grading scales depend on amnesia and loss of consciousness, yet a very small percentage of concussions result in either of these 2 symptoms.4 Some of the grading scales have been criticized for placing too much emphasis on loss of consciousness while neglecting other symptoms. Future research is necessary to provide clinicians with an empirical basis on which to make the classification of injury severity and decisions regarding an athlete's readiness to safely return to competition after concussion. Thus, it is important to use a combination of overall symptom severity, a standardized assessment method, and an acceptable concussion grading scale when classifying injury.
A common theme in the recent literature on sports concussion is that any abnormalities reported or exhibited by the player after a suspected concussion require close attention by the responsible health care provider. All concussions are not created equal, and these injuries may manifest differently in individuals. Our results illustrate that athletic trainers recognize the importance of weighing all clinical information when assessing the injured athlete after concussion. Most would not return a player to competition if any findings from routine clinical examination, standardized assessment methods, or symptom screening were considered abnormal. The current data suggest that athletic trainers consider results from standardized sideline assessment methods (eg, SAC, BESS) and neuropsychological testing to be valuable but continue to place more emphasis on their own clinical examination and the symptoms reported by the player.
Our findings also suggest an increased frequency of collaboration between certified athletic trainers and neuropsychologists in the assessment of sport-related concussion. One in every 4 athletic trainers surveyed has access to a neuropsychologist for consultation, and 40% of those with access routinely refer injured players for testing and consultation after injury. Although athletic trainers incorporate neuropsychological test findings into their return-to-play decision making, seldom are these results the primary criteria considered.
Most respondents believe that standardized methods provide more information clinically than routine examination alone, yet a quarter of respondents expressed concern about the potential misuse of information from standardized assessment methods, including the danger of returning a player to competition too soon. A high percentage of athletic trainers already using these methods reported an improvement in the accuracy of their sideline assessment and indicated that they are now more likely to withhold a player even longer based on the information yielded by these measures.
Several issues related to neuropsychological testing in concussion assessment require attention in the near future, including the use of lengthy test batteries that are not practical in the sports medicine setting, the interest by athletic trainers in being trained to administer neuropsychological tests to assess concussion, and the acquisition of parental consent to perform neuropsychological assessments of high school athletes. Professionals from the fields of neuropsychology and athletic training need to jointly address these issues to develop solutions that meet the clinical demands of the sports medicine community and uphold the professional testing standards required of neuropsychologists.
In summary, recent research publications, continuing education efforts, and increased attention to sports-related concussion appear to have had a small but significant impact on the clinical practice of athletic trainers in the assessment and management of concussion. Clinical judgment and collaboration with an attending physician continue to drive clinical decision making on return to play after injury, but the inclusion of standardized assessment methods appears to be making increasing contributions to these decisions. Also, no consensus yet exists on specific guidelines for injury classification and return-to-play recommendations. Some time is likely to pass before clinical research findings are galvanized into standards of clinical practice and embraced by the larger sports medicine community. Further research and education are necessary to demonstrate the potential value of innovative methods in improving the accuracy of concussion assessment, tracking postinjury recovery, and making more informed decisions regarding safe return to play.
ACKNOWLEDGMENTS
We thank Eric Claas, ATC, for his assistance with data entry.
REFERENCES
- 1.Warren WL, Jr, Bailes JE. On the field evaluation of athletic head injuries. Clin Sports Med. 1998;17:13–26. doi: 10.1016/s0278-5919(05)70057-0. [DOI] [PubMed] [Google Scholar]
- 2.Cantu RC. Return to play guidelines after a head injury. Clin Sports Med. 1998;17:45–60. doi: 10.1016/s0278-5919(05)70060-0. [DOI] [PubMed] [Google Scholar]
- 3.Cantu RC. Cerebral concussion in sport: management and prevention. Sports Med. 1992;14:64–74. doi: 10.2165/00007256-199214010-00005. [DOI] [PubMed] [Google Scholar]
- 4.Guskiewicz KM, Weaver NL, Padua DP, Garrett WE., Jr Epidemiology of concussion in high school and collegiate football players. Am J Sports Med. 2000;28:643–650. doi: 10.1177/03635465000280050401. [DOI] [PubMed] [Google Scholar]
- 5.McCrea M, Kelly JP, Kluge J, Ackley B, Randolph C. Standardized assessment of concussion in football players. Neurology. 1997;48:586–588. doi: 10.1212/wnl.48.3.586. [DOI] [PubMed] [Google Scholar]
- 6.McCrea M, Kelly JP, Randolph C, et al. Standardized Assessment of Concussion (SAC): on-site mental status evaluation of the athlete. J Head Trauma Rehabil. 1998;13:27–35. doi: 10.1097/00001199-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Guskiewicz K, Riemann B, Perrin D. Alternative approaches to the assessment of mild head injury in athletes. Med Sci Sports Exerc. 1997;29:S213–S221. doi: 10.1097/00005768-199707001-00003. [DOI] [PubMed] [Google Scholar]
- 8.Riemann BL, Guskiewicz KM. Objective mild head injury evaluation through a battery of clinical postural stability tests. J Athl Train. 1998;33:S18. [Google Scholar]
- 9.Ingersoll CD, Armstrong CW. The effects of closed-head injury on postural sway. Med Sci Sports Exerc. 1992;24:739–743. [PubMed] [Google Scholar]
- 10.Riemann BL, Guskiewicz KM. Assessment of mild head injury using measures of balance and cognition: a case study. J Sport Rehabil. 1997;6:283–289. [Google Scholar]
- 11.Rubin AM, Woolley SM, Dailey VM, Goebel JA. Postural stability following mild head or whiplash injuries. Am J Otol. 1995;16:216–221. [PubMed] [Google Scholar]
- 12.Macciocchi SN, Barth JT, Alves W, Rimel RW, Jane JA. Neuropsychological functioning and recovery after mild head injury in collegiate athletes. Neurosurgery. 1996;39:510–514. [PubMed] [Google Scholar]
- 13.Collins MW, Grindel SH, Lovell MR, et al. Relationship between concussion and neuropsychological performance in college football players. JAMA. 1999;282:964–970. doi: 10.1001/jama.282.10.964. [DOI] [PubMed] [Google Scholar]
- 14.Hinton-Bayre AD, Geffen G, McFarland K. Mild head injury and speed of information processing: a prospective study of professional rugby league players. Clin Exp Neuropsychol. 1997;19:275–289. doi: 10.1080/01688639708403857. [DOI] [PubMed] [Google Scholar]
- 15.Maddocks D, Saling M. Neuropsychological deficits following concussion. Brain Inj. 1996;10:99–103. doi: 10.1080/026990596124584. [DOI] [PubMed] [Google Scholar]
- 16.Lovell MR, Collins MW. Neuropsychological assessment of the college football player. J Head Trauma Rehabil. 1998;13:9–26. doi: 10.1097/00001199-199804000-00004. [DOI] [PubMed] [Google Scholar]


