Abstract
Rationale: Acute exposure to chlorine gas results in respiratory impairment, but few data are available on the pathobiology of the underlying lung damage.
Objectives: To assess lung function and potential lung damage pathways in the acute phase and longitudinally over a 15-mo follow-up after acute chlorine exposure.
Methods: Ten previously healthy children were accidentally exposed to chlorine gas at a swimming pool because of an erroneous servicing procedure. The fraction of nitric oxide in exhaled air (FeNO), exhaled breath condensate compounds, and serum Clara cell–specific protein CC16 were repeatedly measured.
Main results: In the acute phase, all patients had respiratory distress (one child required mechanical ventilation) and reduced lung function (median and interquartile range: FVC, 51 [43–60]% predicted; FEV1, 51 [46–60]% predicted). This was accompanied by low FeNO (4.7 [3.9–7.9] ppb), high exhaled breath condensate leukotriene B4 (LTB4) levels (24.4 [22.5–24.9] pg/ml), and increased serum CC16 levels (mean ± SEM, 23.4 ± 2.5 μg/L). Lung function returned to normal in 15 d (FVC, 97% predicted [82–108], and FEV1, 92% predicted [77–102]). FeNO reached normal values after 2 mo (12.6 [11.4–15] ppb), whereas LTB4 levels were still increased (12 [9.3–17.1] pg/ml).
Conclusion: Children acutely exposed to chlorine in a swimming pool presented a substantial lung function impairment associated with biochemical exhaled breath alterations, represented mainly by an increase in LTB4 and a reduction in FeNO. Although lung function and FeNO improved within a few weeks, the increased levels of exhaled LTB4 persisted for several months.
Keywords: chlorine inhalation, exhaled breath condensate, exhaled nitric oxide, pneumoproteinemia, pulmonary function
Acute chlorine inhalation results in a variety of dose-related lung effects ranging from respiratory mucous membrane irritation to pulmonary edema with acute respiratory failure, but few data are available on the pathobiology of lung damage underlying this intoxication (1–4). Although recovery is the most likely outcome, there is still concern as to the possibility of long-term sequelae (5–9).
There has been increasing interest in the application of noninvasive methods to assess the pathobiological mechanisms underlying respiratory disorders. In particular, the analysis of biomarkers in exhaled breath, considering exhaled gases and exhaled condensate, has been widely used in pulmonology research settings (10). Being completely noninvasive, the analysis of exhaled breath has the potential for addressing unmet medical needs because the respiratory tract can be repeatedly sampled, enabling longitudinal studies in a wide range of settings.
Among the broad spectrum of gaseous compounds detectable in exhaled air, the fraction of nitric oxide in exhaled air (FeNO) is the most extensively studied marker. In the lung, NO plays a key role in the physiological regulation of vessel and airway tone, and it can be altered in several heart–lung diseases (11).
Exhaled breath condensate (EBC) is a fluid obtained by freezing exhaled air under spontaneous breathing conditions and provides a noninvasive means for exploring several aspects of lung biology and pathobiology. A great variety of molecules originating from the surface of the airways can be measured in EBC, including proinflammatory cytokines, oxidative stress indicators, and other compounds involved in airway inflammation, such as arachidonic acid metabolites (12).
Another noninvasive diagnostic approach to assess lung injury is the so-called pneumoproteinemia concept, that is, assaying lung-specific proteins (e.g., Clara cell–specific protein CC16) in serum (13). In fact, because CC16 is secreted mainly within the respiratory tract, its occurrence in the vascular compartment suggests leakage from the lung into the bloodstream and it is thought to reflect both the rate of synthesis and the permeability of the lung epithelium.
Although noninvasive methods are being used for research purposes and are gradually being introduced in clinical settings (14), there have been no reports on their application in a real clinical scenario after acute exposure to and poisoning with pneumotoxic substances.
This article reports on the application of noninvasive methods to assess the possible pathways of lung injury, in the acute phase and during a 15-mo follow-up, in a group of children accidentally exposed to chlorine gases in a swimming pool.
Some of the results of this study have been previously reported in the form of an abstract (15).
METHODS
On February 17, 2004, 18 children were accidentally exposed to chlorine gas during a swimming lesson. After an erroneous servicing procedure, an excessive quantity of chlorine was added to the pool; the water turned yellow and the children began to feel ill, with coughing, vomiting, dyspnea, and burning eyes and throat.
Ten children (5 males and 5 females; age range, 6 to 12 yr) were taken to the emergency department of Padova children's hospital (Padua, Italy); six were admitted to the pediatric ward and four to the pediatric intensive care unit.
After admission, the children were evaluated, using standard medical procedures. In addition, FeNO, spirometry, and EBC analyses were performed and serum was stored.
FeNO measurement, spirometry, and EBC collection were done in the first 24 h after exposure in nine children, and on Day 4 (after extubation) in one child needing mechanical ventilation.
The children were then reassessed periodically (on Days 1, 3, 8, and 15 and after 2, 4, 8, and 15 mo). At Month 8, the children also took an exercise challenge test.
The follow-up protocol was approved by the local ethics committee and both the parents and the children gave their informed consent to take part in the study.
FeNO was measured at a flow rate of 50 ml/s with the NIOX system (Aerocrine, Stockholm, Sweden), using a single-breath online method according to European Respiratory Society/American Thoracic Society recommendations (16). Lung function was analyzed by flow–volume spirometry according to international recommendations. In addition, a bronchodilation test was performed within 3 d of the intoxication. Exercise challenge was done on a treadmill as previously described (17).
EBC was collected with a condenser formed by five components: a mouthpiece set up to work also as a saliva trap, a nonrebreathing polypropylene valve, a 10-cm Tygon tube, a 50-ml polypropylene vial, and a Dewar flask refrigerated with ice. Children breathed tidally through the mouth for 15 min, without using a nose clip. They maintained a dry mouth during collection by periodically swallowing saliva. EBC samples were stored at −80°C in polypropylene tubes until analytical determinations.
EBC leukotriene B4 (LTB4) and EBC cysteinyl leukotrienes (Cys-LTs) were quantified by ELISA methods as previously described (17, 18).
Serum Clara cell–specific protein CC16 (collected 3–5 h after intoxication) was determined by latex immunoassay (19).
As a control group, we enrolled 10 healthy white children, relatives of doctors and nurses of our hospital, with no history of respiratory diseases or atopy, matched for age and sex with the intoxicated patients (5 males and 5 females; age range, 6 to 12 yr).
Statistical Analysis
Results are expressed as median and interquartile range, except for CC16 values, which are expressed as mean and SEM, being normally distributed. Data from intoxicated children were compared over time by repeated measures analysis of variance, followed by the Student-Newman-Keuls post hoc test. Correlations were tested by Spearman rank test. The Mann-Whitney U test was used to compare biomarker levels in exposed and control children. Statistical significance was assumed for p values of less than 0.05. Statistical analysis was performed with SigmaStat version 3.0 (SPSS, Chicago, IL).
See the online supplement for additional details on the methods.
RESULTS
The past medical history of the poisoned children was essentially negative and none of them had ever had respiratory problems, in particular a diagnosis of asthma. Five children were atopic but only one was suffering from mild recurrent allergic rhinitis. At the time of the accident, they were all healthy. Results of the standard medical procedures at admission are shown in Table 1. In the first hours after the poisoning, all of them were oxygen dependent, whereas four children needed more prolonged oxygen therapy (2–8 d after intoxication). A child needed mechanical ventilation for 4 d, during which time a bronchoscopy with bronchoalveolar lavage (BAL) was performed. Bronchoscopy revealed wide areas of deepithelialization, with yellow membranes along the trachea and main bronchi. BAL fluid analysis showed that 90% of cells were neutrophils.
TABLE 1.
INDIVIDUAL CLINICAL PRESENTATION
| Patient
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1† | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| Sex, age (yr) | M, 12 | F, 6 | F, 8 | M, 9 | F, 7 | F, 10 | M, 9 | M, 9 | F, 8 | M, 8 |
| Chest wall in-drawing | Severe | Mild | Mild | Moderate | Mild | Mild | Absent | Moderate | Absent | Severe |
| Nasal flaring | Present | Absent | Absent | Present | Absent | Absent | Absent | Absent | Absent | Present |
| Sat.O2* at admission, % | < 92 | 92–95 | 92–95 | < 92 | 92–95 | 92–95 | 92–95 | < 92 | 92–95 | < 92 |
| Oxygen dependence, d | 8 | < 1 | < 1 | 3 | < 1 | < 1 | < 1 | 2 | < 1 | 4 |
| Chest X-ray at admission | Diffuse interstitial and alveolar infiltrates | Normal | Normal | Interstitial and alveolar infiltrates | Normal | Normal | Normal | Normal | Mild interstitial infiltrates | Interstitial infiltrate |
Definition of abbreviations: F = female; M = male.
Sat.O2 = oxygen saturation in room air, determined with a pulse oximeter.
Patient who needed mechanical ventilation.
All children were treated with oxygen therapy and inhaled steroids, and six were also given antibiotics and systemic steroids. The chest X-ray was pathologic in four children, with a picture of interstitial involvement accompanied in two cases by patchy and irregular areas of density.
FeNO
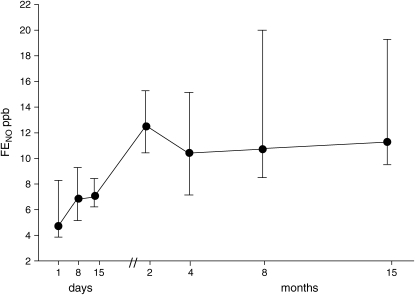
In the exposed children, the median FeNO levels in the acute phase (4.7 [3.9–7.9] ppb) were significantly lower than in healthy matched control subjects (10.8 [8.9–12.2] ppb) and gradually increased during follow-up, reaching normal values at 2 mo (12.6 [11.4–15] ppb; Figure 1).
Figure 1.
Time course of exhaled nitric oxide (FeNO) levels (median and interquartile range [IQR]). FeNO was measured on the day of admission in 9 out of 10 children and then in all 10 patients during the follow-up after acute chlorine inhalation. (Control values, 10.8 [8.9–12.2] ppb.)
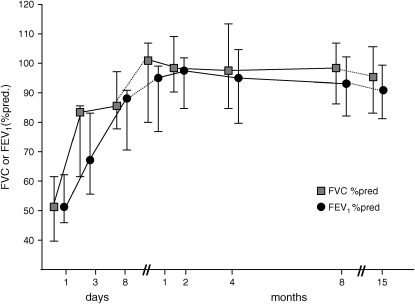
Pulmonary Function Test
Spirometric findings are shown in Figure 2. In the acute phase, there was evidence of an important reduction in FVC and FEV1 (median value of 51% predicted for both), with a normal ratio. There was a significant improvement in both parameters after 3 and 8 d; normal spirometric values were reached 15 d after the exposure to chlorine (median FVC, 97% predicted; median FEV1, 92% predicted). In the acute phase, four patients presented reversibility to β2-agonists, defined as a more than 12% increase in FEV1 after salbutamol inhalation.
Figure 2.
Time course of FVC% predicted and FEV1% predicted (median and IQR) after acute chlorine inhalation. Pulmonary function tests were performed on the day of admission and at several time points during the 15-mo follow-up (FEV1/FVC ratio values, range: 84–87). (Spirometry was performed in 9 children on Days 1 and 3 and then in all 10 patients during the follow-up.)
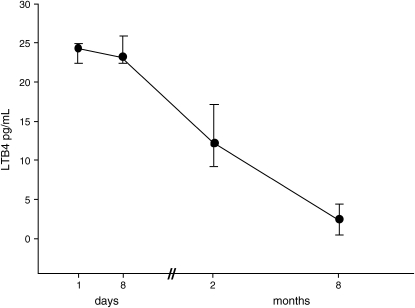
Exhaled Breath Biomarkers
At admission, LTB4 levels were significantly higher in the EBC of the exposed children than in those of the healthy control subjects (24.4 [22.5–24.9] vs. 4.7 [3–10.9] pg/ml); their concentration remained high after the first 8 d (23.3 [22.4–25.8] pg/ml) and then progressively declined over 8 mo, when they were not significantly different from control subjects (2.5 [0.5–4.4] pg/ml; Figure 3).
Figure 3.
Time course of leukotriene B4 (LTB4) levels (median and IQR). LTB4 was measured in exhaled breath condensate (EBC) collected on admission from 9 patients, and then from all 10 patients 1 wk, 2 mo, and 8 mo after acute chlorine inhalation. (Control values, 4.7 [3–10.9] pg/ml.)
Cys-LT levels were also higher in exposed children at admission than in control subjects (25.6 [13.1–38.3] vs. 7.2 [4–15.8] pg/ml) and then gradually dropped during the follow-up; at 8 mo they did not differ from control subjects (4.3 [2–5.9] pg/ml).
Serum CC16
Only one sampling time was available for CC16 (within 3–5 h of exposure); serum CC16 levels were significantly higher in the exposed children than in healthy children (23.4 ± 2.5 vs. 9.5 ± 0.5 μg/L).
Exercise Challenge Test
The exercise challenge, performed 8 mo after the accident, revealed no exercise-induced bronchoconstriction; none of the children had a drop in FEV1 greater than 12% and the mean FEV1 reduction was 5.5 ± 0.6%.
Correlations
There was a significant negative correlation between EBC LTB4 levels and FEV1% predicted (p = 0.01, r = −0.4) and between EBC LTB4 levels and FeNO values (p = 0.03, r = −0.04). FeNO and FVC% predicted were not correlated at any time point (p > 0.2 at all time points). FeNO values at admission were correlated with initial clinical severity (p = 0.03, r = −0.6) and with the length of oxygen dependence (p = 0.01, r = −0.7). Atopic and nonatopic children did not differ in any of the inflammatory markers studied, or in pulmonary function. See the online supplement for additional details on the results.
DISCUSSION
To our knowledge, this is the first study in humans to have applied noninvasive techniques (exhaled breath analysis) to assess lung injury in a real clinical scenario after acute chlorine exposure and poisoning.
Case reports of lung injuries after acute chlorine inhalation in occupational environments and also after community accidents have already been published (1, 3, 4), but they describe lung injuries in terms of lung function and imaging techniques, whereas little information is available on the underlying lung pathobiology after chlorine exposure in humans (9, 20).
Biological events in the lung can be evaluated by invasive methods, such as bronchoscopy and BAL, which have provided important insight on the biological processes occurring in lung diseases, and they still represent the “gold standard.” However, these methods have limited applicability, mainly because of the invasiveness of the sampling procedures, which makes them unsuitable for repeated measurements, particularly in children. As an alternative, several lung disease biomarkers can be analyzed from exhaled air and blood (10, 15, 21).
Previous studies reported respiratory symptoms in the acute phase after chlorine exposure, accompanied by restrictive or mixed deficits at pulmonary function tests, with symptoms fading over a few days and pulmonary function test findings returning to normal over a few months in most cases (5, 6). Nevertheless, some authors reported persistent airway hyperresponsiveness and obstruction in association with exposure to respiratory irritants and physical exertion even years after intoxication (7, 9).
In this longitudinal study, we found severe pulmonary function derangement in the first week after chlorine inhalation, with progressive improvement leading to normalization after 15 d (Figure 2). At the exercise challenge performed 8 mo after the accident, none of the children presented a significant drop in FEV1, suggesting normal bronchial hyperresponsiveness to an indirect stimulus. However, because direct and indirect challenges are weakly correlated and measure different mechanisms of bronchial hyperresponsiveness, we recognize that the choice of an exercise challenge instead of a methacholine test may be a limitation of our study.
FeNO values were lower at admission and in the first weeks by comparison with age-matched healthy control subjects and progressively increased to normal levels after 2 mo. The low FeNO levels observed after chlorine inhalation may be the consequence of massive epithelial destruction with subsequent damage of NO-producing cells of the airway wall—that is, epithelial, endothelial, and nervous cells (11, 22). This hypothesis is supported by the bronchoscopic findings of large areas of airway epithelial loss with proteinaceous exudates in the child who underwent endoscopy during mechanical ventilation.
Another possible cause of low FeNO values could be the reduction in lung volumes. However, this hypothesis seems unlikely because a nonsignificant relationship was found between vital capacity and FeNO values. Also, steroid therapy could have affected FeNO values; however, the lowest FeNO levels were registered at admission, when administration of steroids had been initiated a few hours previously. In addition, FeNO levels progressively increased in the first week, when all children were receiving inhaled steroids.
The hypothesis of diffuse epithelial damage is also supported by the increased values of serum CC16 we observed in the intoxicated children, which may be interpreted as a sign of injury to the lung epithelial permeability barrier. CC16 is secreted by polarized cells in the lumen of the respiratory tract, so its occurrence in the vascular compartment is suggestive of its passage from the lungs into the bloodstream via the bronchoalveolar–blood barrier (13). Moreover, increased CC16 levels, together with the alveolar infiltrates on chest X-rays in two patients, suggest peripheral lung involvement after chlorine inhalation, beside the bronchial damage shown by functional tests.
EBC LTB4 levels were clearly higher in our patients at admission than in control children. Leukotrienes are potent lipid mediators derived from arachidonic acid metabolism; LTB4 is involved in a number of events, including stimulation of leukocyte migration from the bloodstream, neutrophil recruitment and activation, and increased interleukin production (23). The high EBC LTB4 levels that we observed in the intoxicated children may indicate active neutrophilic inflammation in the airways of these patients, with the subsequent release of proteolytic enzymes, O2 radicals, and lipid mediators, resulting in tissue damage. This is consistent with the differential cell count we observed in the child needing mechanical ventilation, whose BAL fluid contained 90% neutrophils. The possible role of LTB4 in lung damage is further supported by its negative correlation with the lung function test results. Published data on in vitro tests also indicate a role for neutrophils in the lung response to acute chlorine exposure in mice and rats (24, 25).
The high LTB4 levels observed 2 mo after the exposure suggest persistent neutrophilic inflammation despite the lack of respiratory symptoms and the normalization of routine lung function test findings. Neutrophil recruitment is probably not the only factor involved in the pathogenesis of lung injury due to chlorine inhalation; in fact, chlorine exposure also induced an increase in EBC Cys-LT levels. These eicosanoids are produced by several cell types in the lung, including mast cells, basophils, eosinophils, and macrophages. It is known that Cys-LT production induces contraction of the airways and vascular smooth muscle, stimulates mucus secretion, and increases microvascular permeability (26).
Taken together, these latter findings led us to hypothesize a role for the arachidonic acid pathway in the lung damage seen in our children, and we speculate that, in addition to steroids, medication inhibiting the 5-lipoxygenase pathway and thus the production of LTB4 and Cys-LTs may be useful in such cases of acute lung injury.
In conclusion, children acutely exposed to chlorine in a swimming pool had substantial lung function impairment associated with biochemical exhaled breath alterations, represented mainly by an increase in leukotrienes and a reduction in FeNO. Although lung function and exhaled NO improved within a few weeks, the increased levels of exhaled LTB4 persisted for several months. These findings shed new light on the pathobiology of chlorine-induced lung damage and may suggest new therapeutic implications for these patients.
Supplementary Material
Acknowledgments
The authors thank Prof. A. Bernard and staff (University of Louvain) for CC16 analysis of serum samples. The authors also thank Dr. F. L. M. Ricciardolo (University of Genoa) for useful suggestions, and the children and parents for their enthusiastic participation in the follow-up study.
Supported in part by grant 1R01 HL72323-01 from the National Heart, Blood, and Lung Institute (NHLBI; Bethesda, MD). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NHLBI or National Institutes of Health.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.200509-1392OC on June 8, 2006
Conflict of Interest Statement: G.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. M.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. S.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. S.Z. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. R.A. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. G.F. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. L.D.D. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. A.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. E.B. has served on the scientific advisory board for Aerocrine (Sweden).
References
- 1.Sexton JD, Pronchik DJ. Chlorine inhalation: the big picture. Clin Toxicol 1998;36:87–93. [DOI] [PubMed] [Google Scholar]
- 2.Mrvos R, Dean BS, Krenzelok EP. Home exposures to chlorine/chloramine gas: review of 216 cases. South Med J 1993;86:654–657. [DOI] [PubMed] [Google Scholar]
- 3.Agabiti N, Ancona C, Forastiere F, Di Napoli A, Lo Presti E, Corbo GM, D'Orsi F, Perucci CA. Short term respiratory effects of acute exposure to chlorine due to a swimming pool accident. Occup Environ Med 2001;58:399–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parimon T, Kanne JP, Pierson DJ. Acute inhalation injury with evidence of diffuse bronchiolitis following chlorine gas exposure at a swimming pool. Respir Care 2004;49:291–294. [PubMed] [Google Scholar]
- 5.Jones RN, Hughes JM, Glindmeyer H. Lung function after acute chlorine exposure. Am Rev Respir Dis 1986;134:1190–1195. [DOI] [PubMed] [Google Scholar]
- 6.Abhyankar A, Bhambure N, Kamath NN, Pajankar SP, Nabar ST, Shrenivas A, Shah AC, Deshmukh SN. Six month follow-up of fourteen victims with short-term exposure to chlorine gas. J Soc Occup Med 1989;39:131–132. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz DA, Smith DD, Lakshminarayan S. The pulmonary sequelae associated with accidental inhalation of chlorine gas. Chest 1990;97: 820–825. [DOI] [PubMed] [Google Scholar]
- 8.Brooks SM, Weiss MA, Bernstein I. Reactive airway dysfunction syndrome (RADS): persistent asthma syndrome after high level irritant exposures. Chest 1985;88:376–384. [DOI] [PubMed] [Google Scholar]
- 9.Schonhofer B, Voshaar T, Kohler D. Long-term lung sequelae following accidental chlorine gas exposure. Respiration (Herrlisheim) 1996;63: 155–159. [DOI] [PubMed] [Google Scholar]
- 10.Kharitonov SA, Barnes PJ. Exhaled markers of pulmonary disease. Am J Respir Crit Care Med 2001;163:1693–1722. [DOI] [PubMed] [Google Scholar]
- 11.Ricciardolo FL, Sterk PJ, Gaston B, Folkerts G. Nitric oxide in health and disease of the respiratory system. Physiol Rev 2004;84:731–765. [DOI] [PubMed] [Google Scholar]
- 12.Hunt J. Exhaled breath condensate: an evolving tool for noninvasive evaluation of lung disease. J Allergy Clin Immunol 2002;110:28–34. [DOI] [PubMed] [Google Scholar]
- 13.Hermans C, Bernard A. Lung epithelium–specific proteins: characteristics and potential applications as markers. Am J Respir Crit Care Med 1999;159:646–678. [DOI] [PubMed] [Google Scholar]
- 14.Smith AD, Cowan JO, Brassett KP, Herbison GP, Taylor DR. Use of exhaled nitric oxide measurements to guide treatment in chronic asthma. N Engl J Med 2005;352:2163–2173. [DOI] [PubMed] [Google Scholar]
- 15.Bonetto G, Corradi M, Carraro S, Zanconato S, Bastardo C, Mutti A, Bernard A, Baraldi E. Swimming pool acute chlorine inhalation in children: pulmonary function and markers of lung damage over a 8 month follow-up [abstract]. Eur Respir J 2005;26:395. [Google Scholar]
- 16.Baraldi E, de Jongste JC. Measurement of exhaled nitric oxide in children, 2001 [ERS/ATS statement]. Eur Respir J 2002;20:223–237. [DOI] [PubMed] [Google Scholar]
- 17.Carraro S, Corradi M, Zanconato S, Alinovi R, Pasquale MF, Zacchello F, Baraldi E. Exhaled breath condensate cysteinyl leukotrienes are increased in children with exercise-induced bronchoconstriction. J Allergy Clin Immunol 2005;115:764–770. [DOI] [PubMed] [Google Scholar]
- 18.Bodini A, Peroni D, Vicentini L, Loiacono A, Baraldi E, Ghiro L, Corradi M, Alinovi R, Boner AL, Piacentini GL. Exhaled breath condensate eicosanoids and sputum eosinophils in asthmatic children: a pilot study. Pediatr Allergy Immunol 2004;15:26–31. [DOI] [PubMed] [Google Scholar]
- 19.Lagerkvist BJ, Bernard A, Blomberg A, Bergstrom E, Forsberg B, Holmstrom K, Karp K, Lundstrom NG, Segerstedt B, Svensson M, et al. Pulmonary epithelial integrity in children: relationship to ambient ozone exposure and swimming pool attendance. Environ Health Perspect 2004;112:1768–1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leroyer C, Malo JL, Infante-Rivard C, Dufour JG, Gautrin D. Changes in airway function and bronchial responsiveness after acute occupational exposure to chlorine leading to treatment in a first aid unit. Occup Environ Med 1998;55:356–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Watson WP, Mutti A. Role of biomarkers in monitoring exposures to chemicals: present position, future prospects. Biomarkers 2004;9:211–242. [DOI] [PubMed] [Google Scholar]
- 22.de Gouw HW, Grunberg K, Schot R, Kroes AC, Dick EC, Sterk PJ. Relationship between exhaled nitric oxide and airway hyperresponsiveness following experimental rhinovirus infection in asthmatic subjects. Eur Respir J 1998;11:126–132. [DOI] [PubMed] [Google Scholar]
- 23.Freeland HS, Schleimer RP, Schulman ES, Lichtenstein LM, Peters SP. Generation of leukotriene B4 by human lung fragments and purified human lung mast cells. Am Rev Respir Dis 1988;138:389–394. [DOI] [PubMed] [Google Scholar]
- 24.Martin JG, Campbell HR, Iijima H, Gautrin D, Malo JL, Eidelman DH, Hamid Q, Maghni K. Chlorine-induced injury to the airways in mice. Am J Respir Crit Care Med 2003;168:568–574. [DOI] [PubMed] [Google Scholar]
- 25.Demnati R, Fraser R, Ghezzo A, Martin JG, Plaa G, Malo JL. Time-course of functional and pathological changes after a single high acute inhalation of chlorine in rats. Eur Respir J 1998;11:922–928. [DOI] [PubMed] [Google Scholar]
- 26.Drazen JM, Israel E, O'Byrne PM. Treatment of asthma with drugs modifying the leukotriene pathway. N Engl J Med 1999;340:197–206. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.