External beam radiation therapy (EBRT) is a treatment modality being used increasingly to treat various cancers in companion animals. It involves passing one or more beams of radiation through a diseased region in the patient with the intent of effecting tumor cure, long-term control, or, in cases where cure is no longer achievable, the palliation of symptoms. The beams come from an external source, such as the capsule of Cobalt-60 housed within the head of the Theratron 780 machine (Theratron 780; MDS Nordion, Ottawa, Ontario) at the Veterinary Teaching Hospital of the Western College of Veterinary Medicine (WCVM). As with all forms of treating disease, there are potential side effects. The acute effects of radiation are those sequelae that appear within weeks of initiating treatment, as opposed to late effects that manifest months or years later. Typically, acute effects are temporary, whereas late effects tend to persist without improvement, or even worsen, over the long-term. As well, acute effects are more often seen with “full-course” or “curative intent” treatment, in which short-lived discomfort is considered a worthwhile trade-off for a probability of long-term tumor control or cure (1).
Side effects are limited to the tissues in the path of the treatment beams, such as the skin in beam entrance and exit zones. As radiation passes through the patient in the region designated for treatment, it deposits energy capable of producing cellular change. When the cell is malignant, the intent of therapy is to create damage that is irreversible and results in death of the cell or an equally lethal destruction of its ability to reproduce itself. When the cell is nonmalignant, or normal, damage is an outcome that is not desired. However, normal tissues are irradiated by necessity in external beam radiation therapy. This is due to a couple of factors. First, tumors are situated on or within normal tissues. In order for the radiation to reach the tumor cells and effect death, it must pass through surrounding tissues either before or after traversing the malignant region. Also, normal tissues around the tumor are intentionally included to account for possible microscopic extensions of malignant cells and slight daily variations in patient treatment position. Appropriate treatment planning and delivery techniques will ensure that as little normal tissue as possible is irradiated, while still achieving tumor destruction or control.
Radiation exerts its greatest impact upon rapidly proliferating cells, as found in hair follicles, sebaceous glands, and the basal layer of the epidermis, as well as in the targeted tumor (2–4). Radiation-related changes are usually not immediately evident in skin, as damage is incurred in the deeper basal layer cells and there is a time-lapse before the more superficial layers of the skin are affected (3,5). Effects do not begin to appear in most patients until the 3rd week of treatment. However, patients that are fair-skinned, or particularly sensitive due to medications or other reasons, can occasionally show skin damage earlier. Effects typically continue to progress through to the conclusion of treatment, and then reach their worst during the first 1 to 2 wk after treatment has finished.
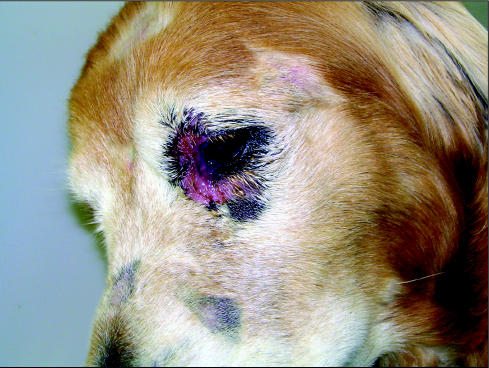
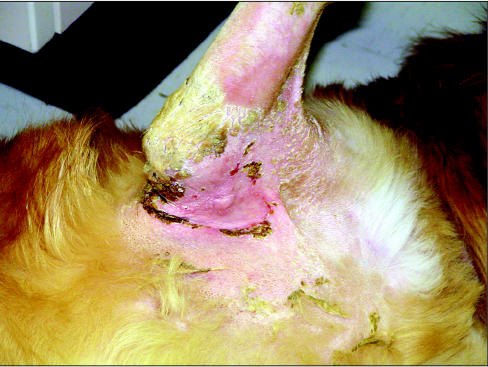
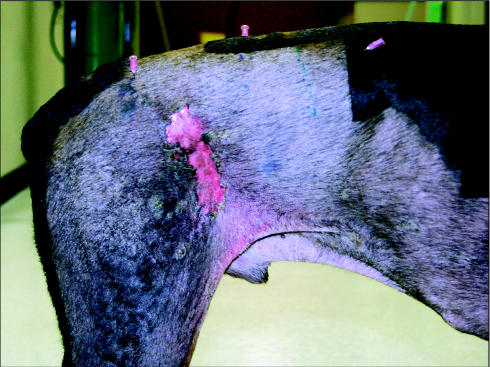
Acute effects in the skin usually manifest initially as a slight erythema. Epilation can also occur early in the course of treatment. As further radiation is given, reddening as well as inflammation of the skin tends to increase. Desquamation, which can be dry in nature and show little more than surface flaking of the stratum corneum, can also appear. In some cases, it can progress, such that a moist exudate begins to be released from portions of the irradiated skin. Moist desquamation is more probable if the treated site includes skin that is subject to friction, or has folds in its surface. Such regions include the axilla or groin, pads, and toes (Figures 1A, 2). Its occurrence is also more frequent in particularly sensitive areas, such as around the eyes, or when a bolus is placed on the skin surface during treatment delivery (Figures 3, 4A–C). In the latter case, use of the bolus is for the specific purpose of increasing the radiation dose to the skin; this is desirable in cases where tumor cells could be found near the skin surface, such as at tumor excision sites or in cancers involving the skin.
Figure 1A.
Moist desquamation in the right axilla.
Figure 2A.
Right metatarsus.
Figure 3.
Moist desquamation here is focused in the delicate tissue surrounding the eyes. Other skin on the face of this patient being treated for nasal adenocarcinoma received little impact beyond moderate erythema.
Figure 4A.
Note placement of bolus over a surgical scar on the right thigh of a patient being treated for soft tissue sarcoma.
Figure 4C.
The same patient 16 d later, with healing of the skin effects.
As acute changes are occurring within the skin, the patient will begin to feel discomfort if proper management is not exercised. This discomfort can range from mild irritation to considerable pain, and can potentially result in self-mutilation of affected tissues, if the patient attempts to gain relief through scratching, rubbing, or other actions.
As the damaged tissues start to heal, regions of moist desquamation will form crusts consisting of the dried exudate and sloughed off cells (Figure 1B). These crusts will alternately fall off and reform while the skin beneath them heals. Within a month following the conclusion of treatment, evidence of acute effects should have almost entirely disappeared. The skin could still show some erythema and hair loss; however, most of the discomfort associated with damage to the skin should be resolved.
Figure 1B.
Note how the skin, merely 3 d later, has shown further crusting with tender healed skin appearing beneath.
Numerous authors in the field of human oncology have noted a broad diversity in approaches to the management of skin effects, even among practitioners in a single hospital (5–9). A similar situation exists in veterinary oncology (2). Disparity has also been observed between techniques that are clinically practised and those that have been empirically proven (9). At the WCVM, we are attempting to adopt a protocol based upon approaches shown to offer significant benefit in the human field, with appropriate changes in application for our patients.
During the course of treatment, all aspects of the patient’s well-being are carefully monitored. This includes a daily visual inspection of the treated skin to monitor the appearance and progression of acute effects. Also, observation of the patient’s behavior, along with daily consultation with the patient’s care-giver, is critical to determining whether discomfort is being adequately controlled (10).
Care offered to companion animals for skin effects includes application of topical aloe vera-based lotions, and silver sulfa-diazine cream (Silvadene; Monarch Pharmaceuticals, Bristol, Tennessee, USA) (2). Use of an acemannan hydrogel wound dressing (Carrington Wound Gel; Carrington Laboratories, Irving, Texas, USA) has also been suggested (11). Along with these products, topical corticosteroids are a common tool in the management of skin effects in human radiation patients (12). The anti-inflammatory and antipruritic properties of these products make them especially suitable for patients who are prone to scratching themselves and thus causing physical trauma (6). At the WCVM, we use mometasone furoate lotion (Elocom; Schering Canada, Pointe-Claire, Quebec); a corticosteroid that has been shown to be effective in the management of acute radiation dermatitis in human patients (13). Gentle application of a thin layer to the treated skin is performed twice weekly during the first 2 wk of treatment. Thereafter, it is applied daily until treatment is concluded, except in regions of moist desquamation. Where moist desquamation occurs, the skin is left untouched, with no lotion or bandaging applied.
After the final radiation treatment, the application of mometasone furoate lotion is discontinued. Caregivers are advised that only an alcohol-free aloe vera gel should be put on skin that still shows signs of dry desquamation or erythema. Aloe vera gel is especially gentle on sensitive skin and can increase patient comfort during recovery without the potentially negative effects of longer-term corticosteroid use (14).
Maintaining cleanliness of the treated skin is important, as it decreases the risk of infection, which would complicate the healing of damaged tissue. If some form of dirt manages to get on the skin before healing has been completed, it should be removed by gently washing with warm, clean water. The skin can then be dried gently with a clean, soft towel or, even better, left to air-dry.
At the WCVM, we recommend that skin being treated with radiation not be bandaged or otherwise wrapped, either as a means of preventing the animal from getting at the irritated tissue or of attempting to limit infection. Bandaging can potentially cause mechanical trauma to delicate irradiated skin, and can therefore impede wound healing (15). However, protection against self-mutilation must be accomplished by using other methods (1). Once the skin becomes irritated, it is prudent to enforce continuous use of an Elizabethan collar or other device that prevents the patient from accessing the affected site (Figure 5).
Figure 5.
Preventing self-trauma of the radiation treatment site is critical.
Effective pain management may also serve to reduce the patient’s desire to disturb the treated skin. Multimodal approaches to achieving pain control have been recommended (16). At the WCVM, we utilize a number of medications in various combinations, depending on the particular needs and coexisting conditions of the patient. These drugs currently include nonsteroidal anti-inflammatories, various narcotic analgesics, and local anesthetic blocks. While we have not yet formally studied its effectiveness, we have also, on occasion, incorporated the complementary therapy of acupuncture into a patient’s care.
Thus far at the WCVM, we have not encountered a significant number of cases in which a patient’s skin becomes infected prior to the resolution of acute effects. As a result, we do not routinely recommend the use of antibiotics, nor have we often found them necessary when guidelines concerning cleanliness and protection against physical trauma are followed.
Figure 2B.
Note how skin effects are more severe between the toes on this treated limb.
Figure 4B.
Skin beneath the bolus showed a more severe skin reaction.
References
- 1.Gillette EL, LaRue SM, Gillette SM. Normal tissue tolerance and management of radiation injury. Semin Vet Med Surg (Small Anim) 1995;10:209–213. [PubMed] [Google Scholar]
- 2.McEntee MC. Veterinary radiation therapy: Review and current state of the art. J Am Anim Hosp Assoc. 2006;42:94–109. doi: 10.5326/0420094. [DOI] [PubMed] [Google Scholar]
- 3.Sitton E. Early and late radiation-induced skin alterations. Part I: Mechanisms of skin changes. Oncol Nurs Forum. 1992;19:801–807. [PubMed] [Google Scholar]
- 4.Stone HB, Coleman CN, Anscher MS, McBride WH. Effects of radiation on normal tissue: Consequences and mechanisms. Lancet Oncol. 2003;4:529–536. doi: 10.1016/s1470-2045(03)01191-4. [DOI] [PubMed] [Google Scholar]
- 5.Porock D, Nikoletti S, Kristjanson L. Management of radiation skin reactions: Literature review and clinical application. Plast Surg Nurs. 1999;19:185–92. [PubMed] [Google Scholar]
- 6.Wood G, Casey L, Trotti A. Skin changes. Cancer Treat Res. 2006;128:171–181. doi: 10.1007/0-387-25354-8_9. [DOI] [PubMed] [Google Scholar]
- 7.Boot-Vickers M, Eaton K. Skin care for patients receiving radiotherapy. Prof Nurse. 1999;14:706–708. [PubMed] [Google Scholar]
- 8.Seegenschmiedt H. Management of skin and related reactions to radiotherapy. Front Radiat Ther Oncol. 2006;39:102–119. doi: 10.1159/000090855. [DOI] [PubMed] [Google Scholar]
- 9.D’haese S, Bate T, Claes S, Boone A, Vanvoorden V, Efficace F. Management of skin reactions during radiotherapy: A study of nursing practice. Eur J Cancer Care (Engl) 2005;14:28–42. doi: 10.1111/j.1365-2354.2005.00510.x. [DOI] [PubMed] [Google Scholar]
- 10.de Lorimier L, Fan TM. Understanding and recognizing cancer pain in dogs and cats. Vet Med. 2005;100:352–362. [Google Scholar]
- 11.Harris D, King GK, Bergman PJ. Radiation therapy toxicities. Vet Clin North Am Small Anim Pract. 1997;1997;27:37–46. doi: 10.1016/s0195-5616(97)50004-0. [DOI] [PubMed] [Google Scholar]
- 12.Sitton E. Early and late radiation-induced skin alterations. Part II: Nursing care of irradiated skin. Oncol Nurs Forum. 1992;19:907–912. [PubMed] [Google Scholar]
- 13.Bostrom A, Lindman H, Swartling C, Berne B, Bergh J. Potent corticosteroid cream (mometasone furoate) significantly reduces acute radiation dermatitis: Results from a double-blind, randomized study. Radiother Oncol. 2001;59:257–265. doi: 10.1016/s0167-8140(01)00327-9. [DOI] [PubMed] [Google Scholar]
- 14.Maddocks-Jennings W, Wilkinson JM, Shillington D. Novel approaches to radiotherapy-induced skin reactions: A literature review. Complement Ther Clin Pract. 2005;11:224–231. doi: 10.1016/j.ctcp.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 15.Park RD, O’Brien TR, Baker BB, Morgan JP. Acute radiodermatitis in the beagle dog: Gross observation after single-dose exposure with x-irradiation. J Am Vet Radiol Soc. 1973;14:49–56. [Google Scholar]
- 16.de Lorimier L, Fan TM. Treating cancer pain in dogs and cats. Vet Med. 2005;100:364–379. [Google Scholar]