Abstract
Yersinia pseudotuberculosis employs a type III secretion system for targeting of several virulence factors directly to the cytosol of eukaryotic cells. This protein translocation mechanism mediates the ability of Yersinia to resist phagocytosis and is required for sustained extracellular bacterial replication. In the present study, the Yersinia outer protein E (YopE) was used as a carrier molecule for type III-dependent secretion and translocation of listeriolysin O (LLO) from Listeria monocytogenes. In comparison to wild-type Yersinia, an attenuated Y. pseudotuberculosis yopK-null mutant strain hypertranslocates chimeric YopE/LLO into the cytosol of macrophages, resulting in enhanced major histocompatibility complex (MHC) class I-restricted antigen presentation of an LLO-derived CD8 T-cell epitope. Remarkably, T-cell activation assays also revealed a superior ability of translocated over secreted LLO to induce MHC class II-restricted antigen presentation. These in vitro observations were confirmed after immunization of mice with a single dose of the yopK-null mutant strain. Animals orally inoculated with recombinant Yersinia expressing translocated chimeric YopE/LLO revealed high numbers of gamma interferon-producing LLO-specific CD4 and CD8 T cells. For the first time, it is shown that cytosolic antigen display mediated by an extracellular bacterial carrier vaccine results in simultaneous CD4 and CD8 T-cell priming, conferring protection against an intracellular pathogen.
The genus Yersinia includes three pathogenic species. In humans, Y. pestis is the causative agent of bubonic plague. Y. pseudotuberculosis and Y. enterocolitica cause a systemic infection similar to plague in rodents, whereas in humans they cause a self-limiting gastrointestinal disease. A 70- to 75-kb virulence plasmid common to these pathogenic Yersinia species encodes a number of secreted proteins designated Yersinia outer proteins (Yops) that are part of a multicomponent secretion system (10). This secretion system, termed the type III secretion system (TTSS), is used by bacteria to establish a remarkable relationship to eukaryotic cells (24). When Yersinia species bind to the surface of macrophages, at least six Yops are delivered directly in a type III-dependent fashion into the cytosol of the host cell (32), mediating the ability to resist phagocytosis (3, 38) and to trigger apoptosis (42). The consequence of this translocation process is that pathogenic yersiniae survive and proliferate at extracellular sites in the infected host (49).
Recent progress in the development of bacterial live carrier vaccines has been made by the use of TTSS for heterologous antigen delivery (25, 44, 45, 46). In vitro studies have described and analyzed in detail the potential of YopE as a carrier molecule for heterologous antigen delivery by Y. enterocolitica (45). YopE is a translocated GTPase-activating molecule that can down-regulate Rho activity, leading to actin filament disruption and inhibition of phagocytosis by macrophages (4, 39, 40, 56). The N-terminal 18 amino acids of YopE fused to a large protein fragment of the p60 antigen from the intracellular pathogen Listeria monocytogenes were sufficient for type III-dependent secretion to the extracellular environment of Yersinia-infected target cells (45). In contrast, fusion of p60 to the N-terminal 138 amino acids of YopE resulted in translocation of the chimeric protein into the cytosol of host cells (45). T-cell activation assays revealed that the cytosolic delivery of the hybrid protein was a prerequisite to induce a p60-specific major histocompatibility complex (MHC) class I-restricted antigen presentation (45).
Y. enterocolitica has been already recognized as a potential bacterial live carrier for vaccination purposes. In the mouse model of infection, Sory et al. made use of Y. enterocolitica strains to induce serum antibody responses against the cytoplasmic CRA protein of Trypanosoma cruzi fused to YopE (52). However, currently there is no information available about the in vivo ability of the Yersinia TTSS to induce MHC class I- and II-restricted immune responses against heterologous antigens. Therefore, the aim of the present study was to investigate whether Yersinia is capable of efficient CD4 and CD8 T-cell priming in orally immunized mice. For this purpose, we used a Y. pseudotuberculosis yopK-null mutant strain as a bacterial carrier vaccine. Previously, this strain was found to be avirulent for orally infected mice (22). In addition, it has been shown elsewhere that the yopK-null mutant was able to colonize and persist in the Peyer's patches of these mice for up to 10 days, whereas it was unable to colonize the spleen (22). Further characterization of the yopK-null mutant revealed that this strain showed a dramatic increase in YopE translocation (23). This indicated that YopK is not a virulence protein per se but rather has a role in the control of translocation of antihost factors such as YopE (23). The inability of the yopK mutant strain to reach the bloodstream and to cause bacteremia on one hand and the ability to hypertranslocate YopE into eukaryotic cells on the other hand are desirable features of an attenuated bacterial carrier vaccine to be used for type III-mediated MHC class I-restricted heterologous antigen presentation.
In this study, listeriolysin O (LLO) of L. monocytogenes fused to YopE was used as a model antigen. The murine Listeria infection is mainly characterized by the development of a protective CD8 T-cell response (28). CD4 T cells also respond to L. monocytogenes infection and can confer protective immunity (28). We demonstrate for the first time that translocation of chimeric YopE/LLO into the cytosol of antigen-presenting cells (APC) by a Y. pseudotuberculosis yopK-null mutant strain results in the induction of a codominant antigen-specific CD4 and CD8 T-cell response in orally vaccinated mice and animal protection against a virulent L. monocytogenes challenge.
(This research was conducted by U. Gerdemann in partial fulfillment of the requirements for a Ph.D. from the Max von Pettenkofer Institute for Hygiene and Medical Microbiology, Ludwig Maximilians University, Munich Germany.)
MATERIALS AND METHODS
Plasmids, bacterial strains, and growth conditions.
Escherichia coli χ6060 was used as an intermediate host for cloning procedures. Both chimeric proteins used in this study are tagged at their C terminus with an M45 epitope tag (MDRSRDRLPPFETETRIL) that is derived from the E4-6/7 protein of adenovirus (36). Previously described plasmid pHR231 (46) was digested with BamHI and SalI to retrieve a gene fragment encoding LLO51-363/M45. This fragment was cloned into the BamHI and SalI sites of plasmids pCJYE18-G3 and pCJYE138-G3 (26). The resulting plasmids pHR429 and pHR430 are pACYC184 derivatives (7). They bear the genetic information for the YopE chaperone SycE and for chimeric YopE1-18/LLO51-363/M45 or YopE1-138/LLO51-363/M45, respectively. Plasmid vectors constructed in this study were transformed into wild-type Y. pseudotuberculosis pIB102 (6), the attenuated Y. pseudotuberculosis yopK mutant strain pIB155 (23), and the attenuated Y. pseudotuberculosis ypkA mutant strain pIB44 (15) by electroporation. Overnight cultures of Y. pseudotuberculosis strains were grown in Luria-Bertani (LB) medium at 27°C. Next day, cultures were diluted and incubated at 37°C for 4 h to allow expression of components and targets of the TTSS encoded by the Yersinia virulence plasmid (45). When required, the antibiotics kanamycin (30 μg/ml) and chloramphenicol (20 μg/ml) were added. L. monocytogenes strain sv1/2a EGD (29) was used for challenge experiments in Yersinia-vaccinated mice.
Western blot analysis of secreted and translocated hybrid YopE/LLO proteins in Yersinia-infected P388D1 cells.
The detection of secreted and translocated chimeric YopE/LLO was carried out as described by Collazo and Galán (9) with the following modifications. Briefly, P388D1 macrophage-like cell monolayers were grown in 100-mm-diameter tissue culture plates in Dulbecco modified Eagle medium supplemented with 5% fetal bovine serum. Cells were infected with Y. pseudotuberculosis strains expressing different hybrid YopE/LLO proteins with a multiplicity of infection (MOI) of 10 in 2.5 ml of Hanks' balanced salt solution (HBSS) at 37°C. Prior to infection, bacterial overnight cultures (LB medium, 27°C) were diluted and incubated at 37°C for 4 h. After infection for 5 h, nonadherent bacteria were removed and cells were washed with HBSS. The infection supernatant was combined with the material from the washes and centrifuged at 8,000 × g for 20 min. The pellet containing nonadherent bacteria was resuspended in 200 μl of phosphate-buffered saline (fraction of non-cell-associated bacteria). The supernatant was filtered through a 0.45-μm-pore-size syringe filter, and proteins were precipitated by addition of 10% trichloroacetic acid (fraction of bacterium-free infection medium). Infected P388D1 cells were incubated for 30 min with Dulbecco modified Eagle medium containing 100 μg of gentamicin/ml to kill the cell-associated extracellular bacteria. Cells were then treated with 30 μg of proteinase K/ml in HBSS for 15 min at 37°C to eliminate cell surface-associated Yops. After proteinase K treatment, 3 ml of chilled HBSS containing 2 mM phenylmethylsulfonyl fluoride was added. Cells detached during the proteinase K treatment and were subsequently collected by low-speed centrifugation (600 × g for 10 min) and lysed in 1 ml of HBSS containing 0.1% Triton X-100 and 1 mM phenylmethylsulfonyl fluoride. Then the cell lysate was centrifuged at 15,000 × g for 10 min. The supernatant was filtered through a 0.45-μm-pore-size syringe filter, and proteins were precipitated in the presence of 10% trichloroacetic acid (fraction of Triton X-100-soluble P388D1 cell lysate containing translocated proteins). Samples were separated by sodium dodecyl sulfate-10% polyacrylamide gel electrophoresis and transferred to nitrocellulose membranes as described previously (9). Hybrid YopE/LLO proteins tagged at their C terminus with an M45 epitope were detected by immunoblot analysis. Western blots were treated with a monoclonal antibody (MAb) directed against M45 (kind gift of P. Hearing, State University of New York, Stony Brook) followed by horseradish peroxidase-labeled anti-mouse antibody. Blots were developed by using a chemiluminescence kit.
Immunofluorescence analysis of hybrid YopE protein translocation.
P388D1 cells were grown on glass coverslips to 60% confluency. One hour before the addition of bacteria, Dulbecco modified Eagle medium was replaced by 500 μl of HBSS. Bacteria were grown overnight for 12 h at 27°C in LB medium, diluted 1:20 in fresh medium, and grown for another 4 h under mild aeration to reach an optical density at 600 nm of 0.9. P388D1 cells were infected with Y. pseudotuberculosis at an MOI of ∼10 for 30 min or 2 or 5 h at 37°C and 5% CO2. Cells were washed three times with HBSS to remove non-cell-associated bacteria and fixed in phosphate-buffered saline-3.7% formaldehyde. Cell-associated extracellular bacteria were stained with an anti-Y. pseudotuberculosis lipopolysaccharide (LPS) polyclonal rabbit antiserum (kind gift of R. Rosqvist, Umeå University, Umeå, Sweden) and a secondary anti-rabbit tetramethylrhodamine isothiocyanate (TRITC) conjugate (1:100 in phosphate-buffered saline-3% bovine serum albumin; Sigma, Deisenhofen, Germany). After permeabilization of P388D1 cells (3 min in phosphate-buffered saline-0.1% Triton X-100), translocated hybrid YopE/LLO/M45 protein was detected with an anti-M45 MAb and an anti-mouse fluorescein isothiocyanate (FITC) conjugate (1:100 in phosphate-buffered saline-3% bovine serum albumin) (Sigma). Coverslips were mounted on glass slides and analyzed by fluorescence microscopy. Experiments were repeated at least three times.
Mice.
Female CB6F1 mice, 6 to 8 weeks old, were purchased from RCC (Füllinsdorf, Switzerland). All mice were kept under specific-pathogen-free conditions (positive-pressure cabinet) and were provided with food and water ad libitum.
Oral immunization of mice with recombinant Yersinia and in vivo protection assay.
Groups of 12 mice were immunized either orally with a single dose of 5 × 109 CFU of attenuated Y. pseudotuberculosis yopK-null mutant strain pIB155, pIB155(pHR429), or pIB155(pHR430) or intraperitoneally with 5 × 103 CFU of L. monocytogenes. Eight weeks after inoculation four mice per group were sacrificed, and spleens were used for further enzyme-linked immunospot (ELISPOT) analysis. The remaining eight mice per group were challenged intravenously with 103 CFU of log-phase L. monocytogenes strain sv1/2a EGD in 0.2 ml of phosphate-buffered saline. Three days after the challenge, CFU were determined by plating serial dilutions of spleen homogenates on PALCAM Listeria selective agar (Merck, Darmstadt, Germany). Colonies were enumerated after 48 h of incubation. Colony counts were corrected for dilution and averaged to yield CFU per organ. The level of protection was calculated as the log10 difference of the bacterial counts from immunized mice and naive control mice. Protection assays were repeated twice with similar results.
Bone marrow cultures.
Bone marrow-derived macrophages were obtained from bone marrow cultures of CB6F1 mice as described previously (50) and grown in Dulbecco modified Eagle medium supplemented with 10% fetal bovine serum and 10 ng of granulocyte-macrophage colony-stimulating factor/ml (R&D Systems, Wiesbaden, Germany). Macrophages were seeded at a density of 105 cells per well in 96-well flat-bottomed tissue culture plates and were fed with 100 μl of granulocyte-macrophage colony-stimulating factor-supplemented medium every 4 days. Macrophages were used for antigen presentation assays after 12 to 16 days of culture and were treated with 100 U of gamma interferon (IFN-γ; R&D Systems)/ml for 24 h before use.
T-cell lines and antigen presentation assay.
CD8 T cells against the H-2Kd-restricted epitope LLO91-99 were derived from spleens of L. monocytogenes-infected BALB/c mice and were propagated by repeated restimulation with P815 cells transfected with the human B7.1 gene (P815/B7) (2) in the presence of 10−9 M peptide as described previously (50). The CD4 T-cell line specific for the H-2Ab-restricted CD4 T-cell epitope LLO190-201 was established from spleens 14 days after intravenous infection of C57BL/6 mice with 103 CFU of L. monocytogenes and was repeatedly restimulated with syngeneic mitomycin C-inactivated splenocytes as APC in the presence of 10−6 M peptide (50). Both CD4 and CD8 T cells were grown in α-modified Eagle's medium (Invitrogen, Karlsruhe, Germany) supplemented with glutamine, penicillin, streptomycin, 10% fetal bovine serum, 100 U of recombinant murine interleukin 2 (R&D Systems)/ml, and 2 × 10−5 M mercaptoethanol. T-cell recognition of infected bone marrow-derived macrophages was measured by the detection of IFN-γ in culture supernatants as described previously (50). Briefly, macrophages were infected with Y. pseudotuberculosis in 96-well flat-bottomed microwell plates by 10 min of 200 × g centrifugation. After 2 h at 37°C infected APC were washed twice and culture medium supplemented with 50 μg of gentamicin/ml was added. After a further 18 h at 37°C, cells were fixed for 10 min with 1% paraformaldehyde in phosphate-buffered saline, and after thorough washing, 5 × 104 T cells were added to each well. The sensitivity of T-cell lines was monitored with APC loaded with graded amounts of the corresponding target peptides. After 12 to 18 h at 37°C, supernatants were harvested and the IFN-γ concentration was measured by means of an IFN-γ-specific enzyme-linked immunosorbent assay (ELISA) that binds and detects IFN-γ with a pair of specific MAbs. Results were corrected for dilution of the sample to yield the sample concentration in nanograms per milliliter.
ELISPOT assay.
The frequency of T lymphocytes in mice immunized with attenuated Y. pseudotuberculosis was determined with an IFN-γ-specific ELISPOT assay as described previously (46). Assays were performed in nitrocellulose-backed 96-well microtiter plates (Nunc, Wiesbaden, Germany) coated with rat anti-mouse IFN-γ MAb (RMMG-1; Biosource, Camarillo, Calif.). From each mouse, 6 × 105 unseparated splenocytes were set up in three different wells for triple determination of the respective T-cell frequency per animal. Splenocytes were stimulated for 6 h in round-bottomed microtiter plates in the presence of a 10−8 M concentration of the CD8 T-cell epitope LLO91-99 or a 10−6 M concentration of the CD4 T-cell epitope LLO190-201. Subsequently, activated cells (4 × 105 or 4 × 104/well) were transferred to ELISPOT plates and incubated overnight. ELISPOT plates were developed with biotin-labeled rat anti-mouse IFN-γ MAb (clone XMG1.2; Pharmingen, San Diego, Calif.), horseradish peroxidase-streptavidin conjugate (Dianova, Hamburg, Germany), and aminoethylcarbazole dye solution. The frequency of antigen-specific cells was calculated as the number of spots per splenocyte seeded. The specificity and sensitivity of the ELISPOT assay were controlled with T-cell lines specific for LLO91-99 or LLO190-201, respectively. Recovery of seeded T cells was higher than 90% for both cell lines.
Statistical analysis.
The statistical analysis of the results of in vitro experiments was performed with the Newman-Keuls multiple comparison test at the 0.05 significance level. The statistical significance of the results of in vivo experiments was checked with the nonparametric Tukey multiple comparison test at the 0.05 significance level. All tests were performed with WINKS statistical analysis software (Texasoft, Cedar Hill, Tex.).
RESULTS
Construction of chimeric YopE/LLO/M45 fusion proteins.
The delivery of YopE by extracellular Yersinia directly to the cytosol of eukaryotic cells has been visualized by confocal microscopy (41) and characterized by the YopE-adenylate cyclase reporter enzyme strategy (53). Analysis of the secretion and translocation of several chimeric YopE proteins revealed that the required information for YopE secretion and translocation is located in the N terminus of the 23-kDa molecule. The minimal sequence shown to be sufficient for secretion of YopE was found to comprise 11 to 15 residues (47, 54). The minimal domain required for translocation of YopE across the eukaryotic cell membrane was reduced to 50 amino acids comprising the binding site of the YopE-specific chaperone (SycE) which is required for YopE translocation (33). Recently, we have demonstrated with Salmonella enterica serovar Typhimurium that these well-defined N-terminal secretion and translocation domains of YopE fused to large portions of LLO from L. monocytogenes can be engaged to direct the heterologous antigen to the cytosol of APC (46). This vaccination strategy resulted in the induction of antigen-specific CD8 T-cell responses in orally vaccinated mice and animal protection against a virulent Listeria challenge (46).
In this study, we constructed two plasmid vectors. Plasmid pHR429 encodes the N-terminal 18 amino acids of YopE fused to LLO51-363, resulting in a hybrid protein that contains the secretion domain but lacks the translocation domain of YopE (Fig. 1A). Plasmid pHR430 bears the genetic information for YopE1-138/LLO51-363. This hybrid protein contains both the secretion and translocation domains of YopE. To facilitate recognition, both chimeric molecules were tagged at their C terminus with an M45 epitope (Fig. 1A). Plasmids pHR429 and pHR430 carry also the sycE gene. It has been previously shown by our laboratory that concomitant expression of sycE and hybrid yopE gene fusions from the same plasmid significantly increases the translocation and antigen presentation efficiency of listerial proteins (45, 46). Transcription of plasmid-borne sycE and gene fusions is mediated by the wild-type yopE/sycE promoters that are both regulated by the Yersinia TTSS.
FIG. 1.
(A) Scheme of translational protein fusions of YopE with the L. monocytogenes-derived CD4 and CD8 target antigen LLO. C-terminal ends of these hybrid proteins were M45 epitope tagged, and they are encoded by the designated plasmids. Both plasmids bear the genetic information for the chaperone SycE. Transcription of vector-borne genes and gene fusions was achieved under the control of the wild-type yopE/sycE promoters. (B) Translocation of hybrid YopE/LLO proteins into macrophage-like cells. P388D1 cells were infected with wild-type Y. pseudotuberculosis pIB102 or the isogenic yopK-null mutant strain pIB155 carrying the indicated plasmid. The presence of chimeric YopE in different fractions was examined as described in Materials and Methods. Lanes 1, whole-cell lysate of non-cell-associated bacteria; lanes 2, bacterium-free infection medium; lanes 3, Triton X-100-soluble P388D1 cell lysate containing translocated proteins. The total protein amounts obtained from all three fractions were loaded. Hybrid YopE proteins were detected by protein immunoblotting with a MAb to M45.
Hypertranslocation of chimeric YopE/LLO into the cytosol of macrophages by a Y. pseudotuberculosis yopK-null mutant strain.
In a previous study, a yopK-null mutant strain of Y. pseudotuberculosis was found to induce a more rapid YopE-mediated cytotoxic response in HeLa cells as well in MDCK-1 cells than did the wild-type strain (23). It has been demonstrated that this effect was the result of an increase in translocation of YopE to the cytosol of eukaryotic host cells. In a first set of experiments, we were interested in whether this YopE-hypertranslocation phenotype of a yopK-null mutant could be used to efficiently deliver chimeric YopE/LLO to the cytosol of APC.
Infections of macrophage-like P388D1 cell monolayers with Y. pseudotuberculosis wild-type strain pIB102 or Y. pseudotuberculosis yopK-null mutant strain pIB155 bearing different plasmids as indicated in Fig. 1B were carried out with an MOI of 10. Five hours after infection, a biochemical fractionation of macrophages was conducted. Three different fractions were tested for the presence of hybrid YopE/LLO/M45 fusion proteins (Fig. 1B): (i) nonadherent yersiniae that were free from infection medium, (ii) Yersinia-free infection medium, and (iii) Triton X-100-soluble cell lysate containing cytosolic proteins. Figure 1B reveals that pIB155(pHR429) secreted the respective YopE hybrid protein into the infection medium at concentrations indistinguishable from those of pIB102(pHR429). As expected and demonstrated in recent publications (45, 46), YopE1-18/LLO/M45, which lacks the YopE translocation domain, was not found in the cytosol of macrophages infected with pIB102(pHR429) or pIB155(pHR429). In contrast, chimeric YopE1-138/LLO/M45 containing the secretion and translocation domains of YopE was readily detected in the cytosol of P388D1 cells infected with pIB102(pHR430) or pIB155(pHR430). Interestingly, the yopK-null mutant strain showed increased translocation of chimeric YopE compared to that of wild-type Y. pseudotuberculosis. In fact, enhanced chemiluminescence-Western blot analysis of serial dilutions of the different lysates revealed that P388D1 cells infected with pIB155(pHR430) contained about 20 to 25 times more hybrid YopE1-138/LLO/M45 protein than did lysates of cells infected with pIB102(pHR430) (data not shown).
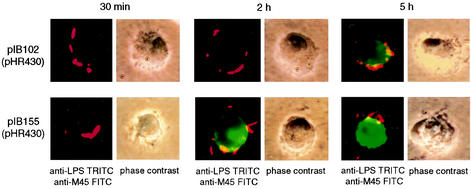
To further delineate the difference in the translocation efficiencies of Y. pseudotuberculosis wild type and the isogenic yopK-null mutant strain, P388D1 cells were infected with pIB102(pHR430) or pIB155(pHR430) for three different periods of time. Macrophages were fixed 30 min or 2 or 5 h after infection and processed for immunofluorescence staining with antibodies directed against M45 and Y. pseudotuberculosis LPS antigen. The left panels of Fig. 2 show typical images of extracellular Yersinia (TRITC signal, red color) and translocated chimeric YopE/LLO (FITC signal, green color) at these three different time points. No fluorescent anti-M45 FITC signal was detected in macrophages 30 min after infection. In contrast, 2 h postinfection hybrid YopE1-138/LLO/M45 protein translocated by the yopK-null mutant strain gave a prominent FITC signal whereas no such signal could be detected in samples infected with the wild-type strain pIB102(pHR430). Five hours after infection, translocation of hybrid YopE was visualized by immunofluorescence microscopy in P388D1 cells infected with either pIB102(pHR430) or pIB155(pHR430). However, macrophages infected with the yopK-null mutant strain gave a much stronger FITC signal than did cells infected with Y. pseudotuberculosis wild type.
FIG. 2.
Time-dependent translocation of hybrid YopE proteins into host cells visualized by immunofluorescence microscopy. P388D1 cells were infected with wild-type Y. pseudotuberculosis pIB102 or the isogenic yopK-null mutant strain pIB155 expressing translocated chimeric YopE/LLO/M45 for 30 min or 2 or 5 h at an MOI of 10. Left panels, extracellular bacteria were detected by using an anti-Yersinia LPS polyclonal antiserum conjugated with TRITC (red signal), and translocated chimeric YopE protein was visualized by using an anti-M45 MAb conjugated with FITC (green signal). Right panels, phase contrast of corresponding images.
Taken together, concordant results from the biochemical fractionation and immunofluorescence staining of Yersinia-infected P388D1 cells clearly demonstrate that the Y. pseudotuberculosis yopK mutant strain hypertranslocates chimeric YopE/LLO proteins into the cytosol of macrophage-like cells.
Hypertranslocation of chimeric YopE/LLO leads to enhanced antigen-specific MHC class I-restricted antigen presentation.
Efficient antigen display is an indispensable requirement for T-cell induction. The strength of antigen presentation generally depends on antigen access to the relative processing compartment, antigen processing efficacy, and antigen abundance (57). Hypertranslocation of antigen should improve antigen display and in principle also the induction of a T-cell response in vivo. To test the effect of hypertranslocation on MHC class I-restricted antigen presentation, the display of the Kd-restricted CD8 T-cell epitope LLO91-99 was monitored in vitro. LLO91-99 is the immunodominant CD8 T-cell epitope of LLO (55), and CD8 T cells specific for this epitope transfer protective immunity against L. monocytogenes to naive mice (21).
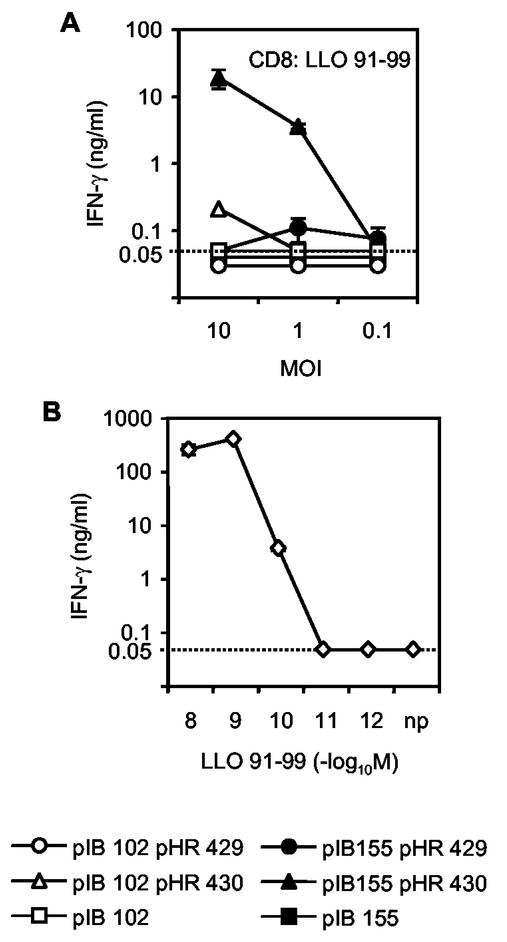
We directly compared the efficiencies of Y. pseudotuberculosis wild type and the Y. pseudotuberculosis yopK-null mutant strain expressing chimeric YopE/LLO/M45 in delivering LLO91-99 to the MHC class I-restricted antigen presentation pathway. Bone marrow macrophages derived from CB6F1 mice were infected with various Yersinia strains and used as APC. The ability of infected cells to present LLO91-99 to CD8 T cells was assessed in an in vitro antigen presentation assay by measuring secreted IFN-γ in the culture supernatant (Fig. 3). Macrophages infected with pIB155(pHR430) hypertranslocating YopE1-138/LLO were efficiently recognized by LLO91-99-specific T cells, whereas APC infected with wild-type strain pIB102(pHR430) stimulated a much weaker LLO91-99-specific T-cell response. As expected, bone marrow macrophages infected with pIB102(pHR429) or pIB155(pHR429) secreting but not translocating chimeric YopE1-18/LLO protein were less efficiently recognized by LLO91-99-specific T cells or did not induce any measurable level of IFN-γ secretion, respectively. Thus, efficient antigen presentation and CD8 T-cell stimulation were significantly enhanced in vitro by cytosolic delivery of the hypertranslocated chimeric YopE/LLO protein by the yopK-null mutant strain.
FIG. 3.
Effect of Yersinia-mediated hypertranslocation on MHC class I-restricted antigen display. Presentation of the MHC class I-restricted epitope LLO91-99 was measured in an in vitro antigen presentation assay with an epitope-specific CD8 T-cell line. (A) APC were infected with Y. pseudotuberculosis pIB102(pHR429) or pIB155(pHR429), each of which secretes the chimeric YopE/LLO protein, or with pIB102(pHR430) or pIB155(pHR430), which translocates or hypertranslocates the YopE/LLO fusion protein, respectively. Nontransformed pIB102 and pIB155 were used as controls. Cells were infected at an MOI of ∼10, ∼1, or ∼0.1. (B) The sensitivity of the CD8 T-cell line was monitored after loading of APC with graded amounts of LLO91-99 peptide. Activation of T cells was measured as the amount of IFN-γ secreted into the culture supernatant. The means and standard deviations of duplicate cultures are indicated. The dotted line at 0.05 ng/ml indicates the detection limit of the IFN-γ ELISA.
Superior ability of translocated over secreted chimeric YopE/LLO to induce antigen-specific MHC class II-restricted antigen presentation.
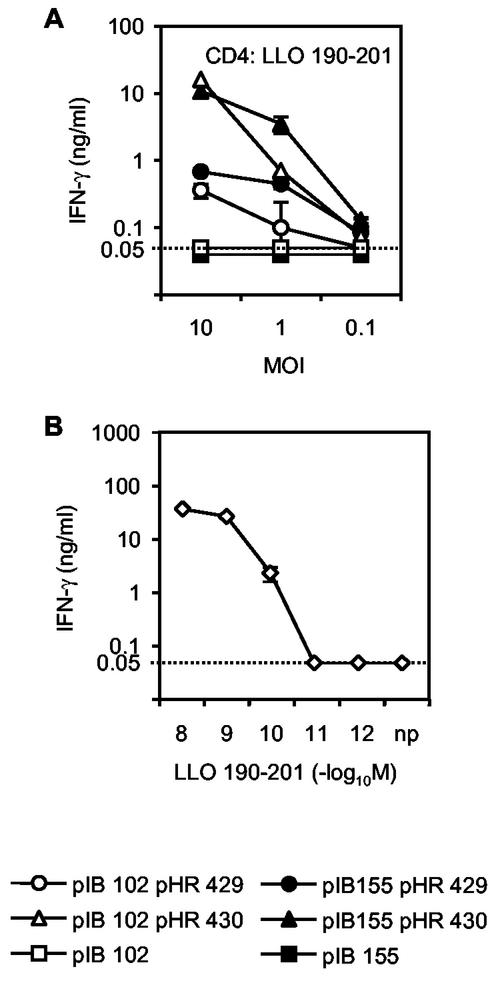
Currently, there is no information available about the efficacy of MHC class II-restricted antigen presentation of heterologous proteins delivered by the Yersinia TTSS. The effect of Yersinia-mediated secretion, regular translocation, and hypertranslocation of the YopE/LLO fusion protein on MHC class II-restricted antigen presentation was therefore studied with the immunodominant H-2Ab-restricted CD4 T-cell epitope LLO190-201 (17). Surprisingly, infection of bone marrow macrophages derived from CB6F1 mice with pIB102(pHR430) or pIB155(pHR430) translocating chimeric YopE/LLO into the host cell cytosol resulted in pronounced stimulation of LLO190-201-specific CD4 T cells (Fig. 4). In contrast, APC infected with pIB102(pHR429) or pIB155(pHR429) secreting YopE/LLO to the extracellular environment stimulated a significantly weaker antigen-specific CD4 T-cell response.
FIG. 4.
Effect of Yersinia-mediated hypertranslocation on MHC class II-restricted antigen display. Presentation of the CD4 T-cell epitope LLO190-201 was monitored in an in vitro antigen presentation assay. (A) APC were infected with Y. pseudotuberculosis pIB102 or pIB155 bearing the indicated plasmids which encode the secreted or translocated form of hybrid YopE/LLO. (B) The sensitivity of the LLO190-201-specific CD4 T-cell line was monitored after loading of APC with graded amounts of peptide. Activation of T cells was measured as the amount of IFN-γ secreted into the culture supernatant. The means and standard deviations of duplicate cultures are indicated. The dotted line at 0.05 ng/ml indicates the detection limit of the IFN-γ ELISA.
At an MOI of 10, the amount of YopE1-138/LLO/M45 hypertranslocated by pIB155(pHR430) did not result in superior MHC class II-restricted antigen presentation (Fig. 4) compared to the lower amount of chimeric protein delivered by pIB102(pHR430) (Fig. 1B and 2). It is conceivable that at this particular MOI the amount of hybrid protein translocated by both recombinant Yersinia strains already reached the level of saturation for sufficient MHC class II antigen presentation. However, at an MOI of 1 the effect of enhanced cytosolic delivery of hybrid YopE/LLO correlated with a more efficient antigen presentation of LLO190-201 by APC.
In summary, results from in vitro MHC class I and II antigen presentation assays indicate that cytosolic translocation of LLO leads to MHC class I-restricted and, remarkably, to efficient MHC class II-restricted antigen display. In particular MHC class I antigen presentation can be further enhanced by hypertranslocation of chimeric YopE/LLO.
Transloctated but not secreted YopE/LLO induces antigen-specific CD4 and CD8 T-cell responses in vivo.
The potential of the attenuated Y. pseudotuberculosis yopK-null mutant strain pIB155 expressing chimeric YopE/LLO/M45 protein to induce CD4 and CD8 T cells in vivo was investigated. For this purpose, CB6F1 mice were orally inoculated with a single dose of 5 × 109 CFU of pIB155 harboring the indicated plasmid. Control groups received a sublethal intraperitoneal dose of 5 × 103 CFU of L. monocytogenes. To exclude differences in bacterial colonization between pIB155(pHR429) and pIB155(pHR430) as a possible reason for different T-cell responses, CFU of these two strains in Peyer's patches were determined on days 2, 5, and 9 (data not shown). The two strains colonized the Peyer's patches of orally immunized CB6F1 mice to the same extent.
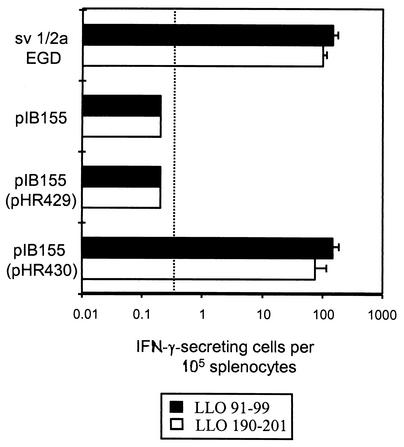
Eight weeks after inoculation, ELISPOT assays were performed to determine the frequency of LLO-specific CD4 and CD8 T cells in vivo. The frequency of LLO190-201-specific CD4 and LLO91-99-specific CD8 T cells was calculated as the number of IFN-γ spots generated per 105 spleen cells in the presence of the corresponding synthetic peptides. Mice immunized with pIB155(pHR430) hypertranslocating YopE1-138/LLO revealed similar numbers of IFN-γ-producing cells reactive with LLO190-201 and LLO91-99 as did mice infected with L. monocytogenes (Fig. 5). In contrast, in the group of animals immunized with the vaccine strain pIB155 or pIB155(pHR429) secreting YopE1-18/LLO the frequency of IFN-γ-producing cells reactive with LLO190-201 and LLO91-99 was below the detection limit of the ELISPOT assay. These experiments verify the results obtained from the antigen presentation assays. In accordance with the in vitro observations and as expected, cytosolic delivery of translocated but not of secreted YopE/LLO led to prominent MHC class I-restricted antigen presentation and antigen-specific CD8 T-cell priming. Strikingly, translocation but not secretion of chimeric YopE resulted in efficient LLO-specific CD4 T-cell induction after oral immunization of mice. To increase the available amount of secreted YopE/LLO for exogenous antigen presentation by APC in vivo, we orally applied 5 × 109 CFU of pIB155(pHR429) to mice on three consecutive days (data not shown). Even with this immunization strategy, the frequency of LLO190-201-specific CD4 T cells was below the detection limit of the ELISPOT assay.
FIG. 5.
Frequency of LLO-specific CD8 and CD4 T cells in spleens of mice orally immunized with 5 × 109 CFU of nontransformed Y. pseudotuberculosis yopK-null mutant strain pIB155 or of pIB155 expressing a hybrid YopE/LLO protein encoded by the indicated plasmid. Spleens from mice infected with L. monocytogenes were used as controls. The frequency of LLO-specific T cells in the spleen of each mouse was determined by ELISPOT assay as described in Materials and Methods. The frequency of cells reactive with LLO91-99 (filled bars) or LLO190-201 (open bars) is shown as the number of reactive cells per 105 splenocytes. The dotted line at 0.2 × 10−5 indicates the detection limit of the ELISPOT assay. The standard deviation of three cultures from 12 individual mice per group is indicated.
Vaccine-induced protection against listeriosis depends on translocation but not on secretion of chimeric YopE/LLO.
Eight weeks after oral immunization with the Y. pseudotuberculosis yopK-null mutant strain expressing hybrid YopE proteins, CB6F1 mice were intravenously challenged with 103 CFU of L. monocytogenes. To compare the contributions of translocated and of secreted LLO to vaccine-induced protection, CFU were determined in spleens 3 days after the challenge. Spleens of animals infected with the nontransformed vaccine strain pIB155 were colonized with (5.0 ± 2.4) × 105 CFU of Listeria (Fig. 6). In contrast, no bacteria were detected in spleens of mice that had received a sublethal intraperitoneal dose of 5 × 103 CFU of Listeria 8 weeks before the challenge infection. Mice immunized with pIB155(pHR429) secreting but not translocating LLO showed no significant difference of the bacterial load in spleens ([3.8 ± 3.6] × 105 CFU) from mice immunized with the nontransformed yopK-null mutant strain. However, animals orally inoculated with pIB155(pHR430) translocating LLO revealed a significant reduction of bacterial colonization in their spleens ([1.2 ± 1.5] × 102 CFU, P < 0.05). After single oral immunization, this protection against a primary Listeria infection was presumably mediated by LLO91-99-specific CD8 T cells (55).
FIG. 6.
Ability of secreted versus translocated hybrid YopE/LLO proteins to induce protective immunity against listeriosis in mice orally immunized with Y. pseudotuberculosis pIB155 carrying the indicated plasmid. Positive-control mice received a sublethal intraperitoneal dose of 5 × 103 CFU of Listeria 8 weeks prior to the challenge infection. Negative-control mice received the attenuated, nontransformed Yersinia carrier strain pIB155. Mice were intravenously challenged with 103 CFU of L. monocytogenes sv1/2a EGD 8 weeks after immunization. The bacterial load of spleens with L. monocytogenes was determined 72 h postinfection. Results are expressed as the mean log10 CFU ± standard deviation of 24 mice per group. The asterisk indicates a value that differs significantly from that of the negative-control group (*, P < 0.05).
DISCUSSION
A variety of attenuated Salmonella, Mycobacterium, and Listeria mutant strains have been reported elsewhere to enable the presentation of heterologous antigens to the immune system of vaccinated mice for proper CD8 T-cell priming (1, 11, 13, 34, 44, 48). A characteristic feature of these bacterial carrier vaccines is their ability to invade host cells. Thus, their intracellular localization facilitates the delivery of foreign proteins into the endogenous pathway of antigen processing. In contrast to intracellular bacteria, Yersinia species have evolved a strategy to survive and multiply within the lymphoid tissue, predominantly extracellularly (35, 49). This strategy might be an advantageous feature for a carrier vaccine strain. Extracellular location may help the host's immune system to eliminate the recombinant strain after a decent interval post-oral immunization and thus prevent a chronic colonization.
It was tempting to hypothesize that the attenuated Y. pseudotuberculosis yopK-null mutant strain previously reported to hypertranslocate wild-type YopE has the potential to induce a pronounced antigen-specific CD8 T-cell response after increased cytosolic delivery of YopE/LLO. In this study, in vitro experiments revealed that hypertranslocation of hybrid YopE into the cytosol of APC indeed resulted in a significantly better MHC class I-restricted antigen presentation of LLO91-99 than did translocation mediated by wild-type Y. pseudotuberculosis. Moreover, single oral application of the yopK-null mutant strain resulted in the induction of a prominent LLO-specific CD8 T-cell response in mice. An important question arises from these in vivo vaccination data. Does an attenuated Y. pseudotuberculosis mutant strain regularly translocating YopE/LLO induce a comparable frequency of LLO-specific CD8 T cells in orally vaccinated mice as the hypertranslocating Y. pseudotuberculosis yopK-null mutant strain does, or is hypertranslocation of the antigenic fusion protein absolutely required for efficient in vivo T-cell priming? To address this question, we used a Y. pseudotuberculosis ypkA mutant strain (15) for further experiments (data not shown). Previously, it has been demonstrated that the YpkA protein exhibits a Ser/Thr kinase activity, which is required for the virulence of Y. pseudotuberculosis (15, 16). Like pIB155, the ypkA mutant strain pIB44 was able to colonize the Peyer's patches of BALB/c mice for several days after oral inoculation but was unable to disseminate into the spleen (16). A biochemical fractionation of macrophages infected with pIB44(pHR430) or pIB102(pHR430) and additional immunofluorescence microscopy studies revealed that the amount of hybrid YopE/LLO translocated by wild-type Y. pseudotuberculosis was indistinguishable from the amount of chimeric YopE translocated by the isogenic ypkA mutant strain (data not shown). This observation was confirmed by an in vitro antigen presentation assay with LLO91-99-specific CD8 T cells. APC infected with Y. pseudotuberculosis strains pIB44(pHR430) and pIB102(pHR430), which translocate hybrid YopE/LLO, were similarly recognized by LLO-specific CD8 T cells, whereas the hypertranslocating strain pIB155(pHR430) was recognized significantly better (data not shown). In the murine model of infection, we directly compared the influence of regular YopE/LLO translocation mediated by an attenuated Y. pseudotuberculosis ypkA mutant strain with chimeric YopE hypertranslocation mediated by the yopK-null mutant strain on the efficiency of CD4 and CD8 T-cell priming. Mice immunized with pIB44(pHR430) or pIB155(pHR430) revealed no significant differences in the number of IFN-γ-producing T cells reactive with LLO91-99 and LLO190-201 (data not shown). Thus, it is important to point out that hypertranslocation per se is not a prerequisite for T-cell activation in vivo. However, it is also conceivable that hypertranslocation in contrast to regular translocation of an antigen might be advantageous in a situation when a certain critical threshold value of the cytosolic protein is needed for proper antigen processing and presentation.
To assess the influence of secreted versus translocated antigen display on antigen processing and T-cellular priming, we constructed two different plasmid-encoded hybrid YopE/LLO proteins. By engaging well-defined secretion and translocation domains of the type III molecule YopE (26, 45, 46, 54) fused to more than 300 amino acids of LLO, chimeric YopE was expressed in either secreted or translocated form. Biochemical fractionation of Yersinia-infected macrophage-like cells clearly revealed that YopE1-138/LLO encoded by pHR430 was translocated to the cytosol of host cells, whereas YopE1-18/LLO encoded by pHR429 lacking the translocation domain was efficiently secreted to the infection medium but was not detected in the Triton X-100-soluble P388D1 cell lysate fraction. Western blot analysis of serial dilutions of the different bacterium-free infection medium fractions indicated that the amounts of secreted YopE1-18/LLO expressed by pIB102(pHR429) and pIB155(pHR429) were approximately 25 times higher than the amounts of YopE1-138/LLO secreted by pIB102(pHR430) and pIB155(pHR430) (data not shown). Thus, we theoretically expected that the well-secreted version of chimeric YopE1-18/LLO could have the potential to enter the exogenous MHC class II-restricted antigen presentation pathway for proper CD4 T-cell priming. Strikingly, results from in vitro antigen presentation assays and also the enumeration of LLO-specific CD4 T cells from immunized mice indicated a superior efficacy of translocated over secreted LLO for MHC class II-restricted antigen processing and CD4 T-cell induction, respectively. We have to emphasize the fact that Yersinia-mediated translocation of a single hybrid protein results in simultaneous antigen-specific CD4 and CD8 T-cell priming. This desirable feature of a bacterial carrier vaccine appears to be specific for Yersinia. Our laboratory has previously demonstrated (46) that YopE1-138/LLO translocated by attenuated Salmonella results in MHC class I-restricted antigen presentation and efficient CD8 T-cell induction in mice. However, use of this construct did not induce any measurable MHC class II-restricted antigen presentation in vitro or CD4 T-cell responses in vivo (H. Rüssmann and G. Geginat, unpublished observations).
An important question arising from this study has to be addressed in future experiments. What is the underlying mechanism in Yersinia-infected APC that efficiently inhibits processing of secreted YopE/LLO via the exogenous MHC class II antigen presentation pathway? A better understanding of the Yersinia TTSS, which is crucial for the pathogenicity and the establishment of the extracellular ecological niche in lymphatic tissues, might contribute to elucidating some aspects of this question. The multicomponent TTSS of Yersinia is among the most complex protein secretion systems known. An essential part of such complexity and probably the most fascinating aspect of type III secretion is the fact that proteins are not only secreted from the bacterial cytoplasm but also delivered directly to the inside of the eukaryotic host cell, therefore effectively working as a “molecular syringe” (14, 30). Four translocated Yop effector proteins are known to disturb the cytoskeleton dynamics and inhibit phagocytosis (18). As mentioned earlier, YopE is a GTPase-activating protein that is active towards G proteins from the Rho family (4, 56). The tyrosine phosphatase YopH (19) disturbs focal adhesion sites by dephosphorylating the focal adhesion kinase, p130Cas, Fyn-binding protein, paxillin, and SKAP-HOM (3, 5, 20, 37). YopT, which is present in Y. enterocolitica but not in Y. pseudotuberculosis, modifies and inactivates RhoA (51, 58), and the threonine kinase YopO (YpkA in Y. pseudotuberculosis) is activated by actin and binds to GTP- and GDP-bound forms of Rho GTPases (12, 27). Does the concerted action of these antiphagocytic molecules also inhibit the uptake of secreted chimeric YopE/LLO and its subsequent endosomal MHC class II-restricted antigen processing? In our laboratory experiments are under way to answer this question.
The most interesting finding in this study is that translocation of antigen to the cytosol of APC rather than secretion of the same antigen results in enhanced CD4 T-cell activation. How do peptides derived from translocated YopE/LLO get associated with MHC class II molecules? Classically, APC are thought to present exogenous extracellular proteins on MHC class II to CD4 T cells and endogenous cytosolic proteins on MHC class I to CD8 T cells. Alternatively, it has been shown elsewhere that MHC class II can present peptides from cytosolic proteins (31). In fact, major peptides on MHC class II appear to be mainly from cellular rather than extracellular proteins (8, 43). Although this could be explained in some cases by endolysosomal processing of membrane proteins, many of these peptides are from cytosol-resident proteins. We are currently investigating the mechanism of how translocated endogenous YopE/LLO is converted into peptides for loading on MHC class II molecules. Leupeptin and pepstatin A, both inhibitors of endosomal proteolysis, do not inhibit MHC class II antigen presentation of Yersinia-translocated LLO (data not shown), indicating that endolysosomal processing is not involved. However, to dissect this complicated pathway further experiments are needed.
Taking the data together, we demonstrate for the first time that an extracellular attenuated Y. pseudotuberculosis strain can be used for simultaneous antigen-specific CD4 and CD8 T-cell induction in orally vaccinated mice, resulting in protection against murine listeriosis. A novel finding of this study is that cytosolic delivery of LLO into APC by the yopK-null mutant strain led to efficient MHC class II presentation of the bacterial antigen. In the future, the mechanism of Yersinia type III-dependent translocation may become a useful tool for vaccination against intracellular pathogens which are controlled by both CD4 and CD8 T cells.
Acknowledgments
We thank J. E. Galán (Yale University School of Medicine, New Haven, Conn.) for helpful discussions. The expert technical assistance of S. Schenk and S. Sauer is acknowledged. Also, we thank R. Rosqvist (Umeå University, Umeå, Sweden) for providing anti-Y. pseudotuberculosis LPS polyclonal rabbit antiserum and P. Hearing (State University of New York, Stony Brook) for providing M45 MAb.
H.R. and J.H. were supported by the Deutsche Forschungsgemeinschaft (Schwerpunktprogramm “Neue Vakzinierungsstrategien”) and the Bavarian Research Foundation (FORGEN II). H.W.-W. and J.H. received grants from the European Commission (QLK2-1999-00780).
Editor: J. T. Barbieri
REFERENCES
- 1.Aldovini, A., and R. A. Young. 1991. Humoral and cell-mediated immune responses to live recombinant BCG-HIV vaccines. Nature 351:479-482. [DOI] [PubMed] [Google Scholar]
- 2.Azuma, M., H. Yssel, J. H. Phillips, H. Spits, and L. L. Lanier. 1993. Functional expression of B7/BB1 on activated T lymphocytes. J. Exp. Med. 177:845-850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Black, D. S., and J. B. Bliska. 1997. Identification of p130Cas as a substrate of Yersinia YopH (Yop51), a bacterial protein tyrosine phosphatase that translocates into mammalian cells and targets focal adhesions. EMBO J. 16:2730-2744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Black, D. S., and J. B. Bliska. 2000. The RhoGAP activity of the Yersinia pseudotuberculosis cytotoxin YopE is required for antiphagocytic function and virulence. Mol. Microbiol. 37:515-527. [DOI] [PubMed] [Google Scholar]
- 5.Black, D. S., A. Marie-Cardine, B. Schraven, and J. B. Bliska. 2000. The Yersinia tyrosine phosphatase YopH targets a novel adhesion-regulated signalling complex in macrophages. Cell. Microbiol. 2:401-414. [DOI] [PubMed] [Google Scholar]
- 6.Bölin, I., and H. Wolf-Watz. 1984. Molecular cloning of the temperature-inducible outer membrane protein 1 of Yersinia pseudotuberculosis. Infect. Immun. 43:72-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chang, A. C. Y., and S. N. Cohen. 1978. Construction and characterization of amplifiable multicopy DNA cloning vehicles derived from the P15A cryptic miniplasmid. J. Bacteriol. 134:1141-1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chicz, R. M., R. G. Urban, J. C. Gorga, D. A. Vignali, W. S. Lane, and J. L. Strominger. 1993. Specificity and promiscuity among naturally processed peptides bound to HLA-DR alleles. J. Exp. Med. 178:27-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collazo, C. M., and J. E. Galán. 1997. The invasion-associated type III system of Salmonella typhimurium directs the translocation of Sip proteins into the host cell. Mol. Microbiol. 24:747-756. [DOI] [PubMed] [Google Scholar]
- 10.Cornelis, G. R., A. Boland, A. P. Boyd, C. Geuijen, M. Iriarte, C. Neyt, M.-P. Sory, and I. Stainier. 1998. The virulence plasmid of Yersinia, an antihost genome. Microbiol. Mol. Biol. Rev. 62:1315-1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dietrich, G., A. Bubert, I. Gentchev, Z. Sokolovic, A. Simm, A. Catic, S. H. Kaufmann, J. Hess, J. Szalay, and W. Goebel. 1998. Delivery of antigen-encoding plasmid DNA into the cytosol of macrophages by attenuated suicide Listeria monocytogenes. Nat. Biotechnol. 16:181-185. [DOI] [PubMed] [Google Scholar]
- 12.Dukuzumuremyi, J. M., R. Rosqvist, B. Hallberg, B. Akerstrom, H. Wolf-Watz, and K. Schesser. 2000. The Yersinia protein kinase A is a host factor inducible RhoA/Rac-binding virulence factor. J. Biol. Chem. 275:35281-35290. [DOI] [PubMed] [Google Scholar]
- 13.Everest, P., P. Griffiths, and G. Dougan. 1995. Live Salmonella vaccines as a route towards oral immunisation. Biologicals 23:119-124. [DOI] [PubMed] [Google Scholar]
- 14.Galán, J. E. 1998. Interactions of Salmonella with host cells: encounters of the closest kind. Proc. Natl. Acad. Sci. USA 95:14006-14008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galyov, E. E., S. Hakansson, A. Forsberg, and H. Wolf-Watz. 1993. A secreted protein kinase of Yersinia pseudotuberculosis is an indispensable virulence determinant. Nature 361:730-732. [DOI] [PubMed] [Google Scholar]
- 16.Galyov, E. E., S. Hakansson, and H. Wolf-Watz. 1994. Characterization of the operon encoding the YpkA Ser/Thr protein kinase and the YopJ protein of Yersinia pseudotuberculosis. J. Bacteriol. 176:4543-4548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geginat, G., S. Schenk, M. Skoberne, W. Goebel, and H. Hof. 2001. A novel approach of direct ex vivo epitope mapping identifies dominant and subdominant CD4 and CD8 T cell epitopes from Listeria monocytogenes. J. Immunol. 166:1877-1884. [DOI] [PubMed] [Google Scholar]
- 18.Grosdent, N., I. Maridonneau-Parini, M.-P. Sory, and G. R. Cornelis. 2002. Role of Yops and adhesions in resistance of Yersinia enterocolitica to phagocytosis. Infect. Immun. 70:4165-4176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guan, K. L., and J. E. Dixon. 1990. Protein tyrosine phosphatase activity of an essential virulence determinant in Yersinia. Science 249:553-556. [DOI] [PubMed] [Google Scholar]
- 20.Hamid, N., A. Gustavsson, K. Andersson, K. McGee, C. Persson, C. E. Rudd, and M. Fallman. 1999. YopH dephosphorylates Cas and Fyn-binding protein in macrophages. Microb. Pathog. 27:231-242. [DOI] [PubMed] [Google Scholar]
- 21.Harty, J. T., and M. J. Bevan. 1992. CD8+ T cells specific for a single nonamer epitope of Listeria monocytogenes are protective in vivo. J. Exp. Med. 175:1531-1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holmström, A., R. Rosqvist, H. Wolf-Watz, and A. Forsberg. 1995. Virulence plasmid-encoded YopK is essential for Yersinia pseudotuberculosis to cause systemic infection in mice. Infect. Immun. 63:2269-2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holmström, A., J. Pettersson, R. Rosqvist, S. Hakansson, F. Tafazoli, M. Fällman, K.-E. Magnusson, H. Wolf-Watz, and A. Forsberg. 1997. YopK of Yersinia pseudotuberculosis controls translocation of Yop effectors across the eukaryotic cell membrane. Mol. Microbiol. 24:73-91. [DOI] [PubMed] [Google Scholar]
- 24.Hueck, C. J. 1998. Type III protein secretion systems in bacterial pathogens of animals and plants. Microbiol. Mol. Biol. Rev. 62:379-433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Igwe, E. I., G. Geginat, and H. Rüssmann. 2002. Concomitant cytosolic delivery of two immunodominant listerial antigens by Salmonella enterica serovar Typhimurium confers superior protection against murine listeriosis. Infect. Immun. 70:7114-7119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jacobi, C. A., A. Roggenkamp, A. Rakin, R. Zumbihl, L. Leitritz, and J. Heesemann. 1998. In vitro and in vivo expression studies of yopE from Yersinia enterocolitica using the gfp reporter gene. Mol. Microbiol. 30:865-882. [DOI] [PubMed] [Google Scholar]
- 27.Juris, S. J., A. E. Rudolph, D. Huddler, K. Orth, and J. E. Dixon. 2000. A distinctive role for the Yersinia protein kinase: actin binding, kinase activation, and cytoskeleton disruption. Proc. Natl. Acad. Sci. USA 97:9431-9436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kerksieck, K. M., and E. G. Pamer. 1999. T cell responses to bacterial infection. Curr. Opin. Immunol. 11:400-405. [DOI] [PubMed] [Google Scholar]
- 29.Köhler, S., M. Leimeister-Wächter, T. Chakraborty, F. Lottspeich, and W. Goebel. 1990. The gene coding for protein p60 of Listeria monocytogenes and its use as a specific probe for Listeria monocytogenes. Infect. Immun. 58:1943-1950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kubori, T., Y. Matsushima, D. Nakamura, J. Uralil, M. Lara-Tejero, A. Sukhan, J. E. Galán, and S. I. Aizawa. 1998. Supramolecular structure of the Salmonella typhimurium type III protein secretion system. Science 280:602-605. [DOI] [PubMed] [Google Scholar]
- 31.Lechler, R., G. Aichinger, and L. Lightstone. 1996. The endogenous pathway of MHC class II antigen presentation. Immunol. Rev. 151:51-79. [DOI] [PubMed] [Google Scholar]
- 32.Lee, C. A. 1997. Type III secretion systems: machines to deliver bacterial proteins into eukaryotic cells? Trends Microbiol. 5:148-156. [DOI] [PubMed] [Google Scholar]
- 33.Lee, V. T., D. M. Anderson, and O. Schneewind. 1998. Targeting of Yersinia Yop proteins into the cytosol of HeLa cells: one-step translocation of YopE across bacterial and eukaryotic membranes is dependent on SycE chaperone. Mol. Microbiol. 28:593-601. [DOI] [PubMed] [Google Scholar]
- 34.Levine, M. M., J. Galen, E. Barry, F. Noriega, S. Chatfield, M. Sztein, G. Dougan, and C. Tacket. 1996. Attenuated Salmonella as live oral vaccines against typhoid fever and as live vectors. J. Biotechnol. 44:193-196. [DOI] [PubMed] [Google Scholar]
- 35.Lian, C.-J., W. S. Hwang, and C. H. Pai. 1987. Plasmid-mediated resistance to phagocytosis in Yersinia enterocolitica. Infect. Immun. 55:1176-1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Obert, S., R. J. O'Connor, S. Schmid, and P. Hearing. 1994. The adenovirus E4-6/7 protein transactivates the E2 promoter by inducing dimerization of a heteromeric E2F complex. Mol. Cell. Biol. 14:1333-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Persson, C., N. Carballeira, H. Wolf-Watz, and M. Fallman. 1997. The PTPase YopH inhibits uptake of Yersinia, tyrosine phosphorylation of p130Cas and FAK, and the associated accumulation of these proteins in peripheral focal adhesions. EMBO J. 16:2307-2317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rosqvist, R., I. Bolin, and H. Wolf-Watz. 1988. Inhibition of phagocytosis in Yersinia pseudotuberculosis: a virulence plasmid-encoded ability involving the Yop2b protein. Infect. Immun. 56:2139-2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rosqvist, R., A. Forsberg, M. Rimpiläinen, T. Bergman, and H. Wolf-Watz. 1990. The cytotoxic protein YopE of Yersinia obstructs the primary host defence. Mol. Microbiol. 4:657-667. [DOI] [PubMed] [Google Scholar]
- 40.Rosqvist, R., A. Forsberg, and H. Wolf-Watz. 1991. Intracellular targeting of the Yersinia YopE cytotoxin in mammalian cells induces actin microfilament disruption. Infect. Immun. 59:4562-4569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rosqvist, R., K. E. Magnusson, and H. Wolf-Watz. 1994. Target cell contact triggers expression and polarized transfer of Yersinia YopE cytotoxin into mammalian cells. EMBO J. 13:964-972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ruckdeschel, K., A. Roggenkamp, V. Lafont, P. Mangeat, J. Heesemann, and B. Rouot. 1997. Interaction of Yersinia enterocolitica with macrophages leads to macrophage cell death through apoptosis. Infect. Immun. 65:4813-4821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rudensky, A. Y., P. Preston-Hurlburt, S.-C. Hong, A. Barlow, and C. A. Janeway, Jr. 1991. Sequence analysis of peptides bound to MHC class II molecules. Nature 353:622-627. [DOI] [PubMed] [Google Scholar]
- 44.Rüssmann, H., H. Shams, F. Poblete, Y. Fu, J. E. Galán, and R. O. Donis. 1998. Delivery of epitopes by the Salmonella type III secretion system for vaccine development. Science 281:565-568. [DOI] [PubMed] [Google Scholar]
- 45.Rüssmann, H., A. Weissmüller, G. Geginat, E. I. Igwe, A. Roggenkamp, A. Bubert, W. Goebel, H. Hof, and J. Heesemann. 2000. Yersinia enterocolitica-mediated translocation of defined fusion proteins to the cytosol of mammalian cells results in peptide-specific MHC class I-restricted antigen presentation. Eur. J. Immunol. 30:1375-1384. [DOI] [PubMed] [Google Scholar]
- 46.Rüssmann, H., E. I. Igwe, J. Sauer, W.-D. Hardt, A. Bubert, and G. Geginat. 2001. Protection against murine listeriosis by oral vaccination with recombinant Salmonella expressing hybrid Yersinia type III proteins. J. Immunol. 167:357-365. [DOI] [PubMed] [Google Scholar]
- 47.Schesser, K., E. Frithz-Lindsten, and H. Wolf-Watz. 1996. Delineation and mutational analysis of the Yersinia pseudotuberculosis YopE domains which mediate translocation across bacterial and eukaryotic cellular membranes. J. Bacteriol. 178:7227-7233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schodel, F., and R. Curtiss III. 1995. Salmonellae as oral vaccine carriers. Dev. Biol. Stand. 84:245-253. [PubMed] [Google Scholar]
- 49.Simonet, M., S. Richard, and P. Berche. 1990. Electron microscopic evidence for in vivo extracellular localization of Yersinia pseudotuberculosis harboring the pYV plasmid. Infect. Immun. 58:841-845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Skoberne, M., S. Schenk, H. Hof, and G. Geginat. 2002. Cross-presentation of Listeria monocytogenes-derived CD4 T cell epitopes. J. Immunol. 169:1410-1418. [DOI] [PubMed] [Google Scholar]
- 51.Sorg, I., U. M. Goehring, K. Aktories, and G. Schmidt. 2001. Recombinant Yersinia YopT leads to uncoupling of RhoA-effector interaction. Infect. Immun. 69:7535-7543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sory, M.-P., K. Kaniga, S. Goldenberg, and G. R. Cornelis. 1992. Expression of the eukaryotic Trypanosoma cruzi CRA gene in Yersinia enterocolitica and induction of an immune response against CRA in mice. Infect. Immun. 60:3830-3836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sory, M.-P., and G. R. Cornelis. 1994. Translocation of a hybrid YopE-adenylate cyclase from Yersinia enterocolitica into HeLa cells. Mol. Microbiol. 14:583-594. [DOI] [PubMed] [Google Scholar]
- 54.Sory, M.-P., A. Boland, I. Lambermont, and G. R. Cornelis. 1995. Identification of the YopE and YopH domains required for secretion and internalization into the cytosol of macrophages, using the cyaA gene fusion approach. Proc. Natl. Acad. Sci. USA 92:1998-2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vijh, S., and E. G. Pamer. 1997. Immunodominant and subdominant CTL responses to Listeria monocytogenes infection. J. Immunol. 158:3366-3371. [PubMed] [Google Scholar]
- 56.Von Pawel-Rammingen, U., M. V. Telepnev, G. Schmidt, K. Aktories, H. Wolf-Watz, and R. Rosqvist. 2000. GAP activity of the Yersinia YopE cytotoxin specifically targets the Rho pathway: a mechanism for disruption of actin microfilament structure. Mol. Microbiol. 36:737-748. [DOI] [PubMed] [Google Scholar]
- 57.Yewdell, J. W., and J. R. Bennink. 1999. Immunodominance in major histocompatibility complex class I-restricted T lymphocyte responses. Annu. Rev. Immunol. 17:51-88. [DOI] [PubMed] [Google Scholar]
- 58.Zumbihl, R., M. Aepfelbacher, A. Andor, C. A. Jacobi, K. Ruckdeschel, B. Rouot, and J. Heesemann. 1999. The cytotoxin YopT of Yersinia enterocolitica induces modification and cellular redistribution of the small GTP-binding protein RhoA. J. Biol. Chem. 274:29289-29293. [DOI] [PubMed] [Google Scholar]