Abstract
OBJECTIVE: Data on the sexual activity of middle-aged and older women are scant and vary widely. This analysis estimates the prevalence and predictors of sexual activity and function in a diverse group of women aged 40-69 years.
METHODS: The Reproductive Risk Factors for Incontinence Study at Kaiser (RRISK) was a population-based study of 2,109 women aged 40-69 years who were randomly selected from long-term Kaiser Permanente members. Women completed self-report questionnaires on sexual activity, comorbidities, and general quality of life. Logistic and linear regression and proportional odds models were used when appropriate to identify correlates of sexual activity, frequency, satisfaction, and dysfunction.
RESULTS: Mean age was 55.9 (± 8) years and nearly three fourths of the women were sexually active. Of the sexually active women, 60% had sexual activity at least monthly, approximately two thirds were at least some- what satisfied, and 33% reported a problem in one or more domains. Monthly or more frequent sexual activity was associated with younger age, higher income, being in a significant relationship, a history of moderate alcohol use, and lower body mass index (BMI) (all P < .05). Satisfaction with sexual activity was associated with African-American race, lower BMI, and higher mental health score (all P < .05). More sexual dysfunction was associated with having a college degree or greater, poor health, being in a significant relationship, and a low mental health score (all P < .05).
CONCLUSION: Middle-aged and older women engage in satisfying sexual activity, and one third reported problems with sexual function. Demographic factors as well as some issues associated with aging can adversely affect sexual frequency, satisfaction, and function. (Obstet Gynecol 2006;107:755-64)
LEVEL OF EVIDENCE: II-3
There is limited information on the prevalence, incidence, and antecedents of female sexual dysfunction. Community-based studies indicate that the prevalence of sexual dysfunction among all women is between 25% and 63%.1-3 The prevalence of sexual dysfunction in postmenopausal women varies from 68% to 86.5%, depending on the setting in which the study was performed.4,5 An analysis of data from the National Health and Social Life Survey found that sexual dysfunction is more prevalent in women (43%) than in men (31%); prevalence varied among women of different racial groups and was associated with a history of traumatic sexual experiences and with deteriorating social position.6 Sexual dysfunction impacts significantly women’s self-esteem and quality of life and causes emotional distress, leading to relationship problems.7
Relatively little research has been focused on factors that are associated with sexual frequency, satisfaction, and dysfunction. Studies suggest that the same disease processes and risk factors that are associated with male erectile dysfunction, such as aging, hypertension, smoking, and pelvic surgery, are also associated with female sexual dysfunction.8 However, previous studies have been limited by their selected populations, evaluation of a limited number of potential risk factors, inadequate control for potential confounding variables, and unvalidated measures of sexual function.9-13
To determine the prevalence of and risk factors for the frequency of sexual activity, satisfaction, and sexual dysfunction among middle-aged and older women, we studied 2,109 community-dwelling women aged 40-69 years who participated in the population-based Reproductive Risk Factors for Incontinence Study at Kaiser (RRISK), originally a study of risk factors for urinary incontinence.
MATERIALS AND METHODS
The Reproductive Risk Factors for Incontinence Study at Kaiser (RRISK) had enrolled 2,109 women aged 40-69 years as of January 1, 1999. Women were recruited from within the Kaiser Permanente Medical Care Program of Northern California, a health maintenance organization with over 3 million members, approximately 25-30% of the population in the areas served. Previous studies have found that members of Kaiser underrepresent those groups of people in the lowest and highest socioeconomic classes.14 In addition, members of the organization tend to be slightly more educated than the general populace (63% high school graduates versus 56% in the general population), but they are very similar in terms of other demographic characteristics such as race and ethnicity.
The design and sampling methods have been previously described.15 Briefly, random samples within age and race strata were drawn such that a roughly equal number of women would be in 5-year age groups, and the race distribution would be approximately 40% white, 20% African American, 20% Hispanic, and 20% Asian. Informed consent was obtained by phone and written form at the time of the interview. The Institutional Review Boards at University of California, San Francisco, and Kaiser Permanente approved this study.
Data for the study were collected by self-reported questionnaires and in-person interviews. Data on demographics, medical and surgical history, current medications, menopause, hormone therapy use, anal incontinence, pelvic organ prolapse, and functional status (using the Medical Outcomes Study SF-36) were obtained using a structured questionnaire and a trained interviewer. Height and weight were measured by the interviewer. Most interviews took place either in the home of the participant (57%) or at a Kaiser Permanente Medical Care Program clinic (28%).
Three general areas of sexual functioning were defined for this study: sexual frequency, sexual satisfaction, and sexual problems. The sexual functioning questionnaire contained questions on frequency of sexual activity in the past 12 months, sexual satisfaction, and sexual dysfunction (Appendix 2). In the questionnaire, sexual activity is defined as “any activity that is sexually arousing to you, including masturbation.” Frequency of sexual activity was defined as never, less than monthly, monthly, weekly, and daily activity in the last 12 months. For the purposes of analysis, we grouped the weekly and daily activity due to small numbers in the “daily” category. Women were considered satisfied with their sexual activity in the last 12 months if they stated “somewhat satisfied” or “very satisfied.”
Detailed information on sexual problems and function were collected by using the sexual problem assessment tool and scale from the Medical Outcomes Study. The Medical Outcomes Study tool identifies sexual problems in patients with a variety of chronic diseases. It also concentrates on current sexual problems, rather than on changes in usual sexual functioning. The questionnaire contains 3 items that are appropriate for men and women, one for women only, and one for men only (which was not used in our study). This questionnaire has been validated in the usual fashion with an initial pilot study to identify item variability and frequency, to analyze different sexual functioning measures using multitrait scaling techniques, and to define the most effective 5 questions. These questions were chosen by eliminating the items with low variability and low item-total correlations. The final measure, when analyzed, was found to be reliable and valid. Based on this scale, sexual dysfunction was assessed over the past 4 weeks in 4 domains: lack of sexual interest, inability to relax and enjoy sexual activity, difficulty in becoming aroused, and difficulty in having an orgasm.16 An overall sexual function score was calculated by assigning a score of 1 (“not a problem”) to 4 (“very much a problem”) to each of the 4 domain questions, calculating a mean score, and transforming the mean score to a 0-100 scale. Additionally, on each separate domain, we defined sexual dysfunction as having answered “somewhat of a problem” or “very much a problem.” This is eithera3ora4onour Likert scale. Participants were defined as having any sexual dysfunction if they answered “somewhat of a problem” or “very much a problem” in at least 1 of the 4 domains.
Other variables of interest were measured by the self-report questionnaires (alcohol use, smoking, education, race/ethnicity, relationship status, employment, general overall health, current pelvic organ prolapse, hysterectomy, former or current hormone therapy, and weekly or greater urinary incontinence). Body mass index (BMI) was calculated from the height and weight measurements obtained by the interviewer. Age at interview was calculated by using the birth date and the RRISK visit date and classified into 10-year groups. The mental health scale from the Medical Outcomes Study SF-36 was calculated by using the standardization technique described in the SF-36 Summary Measures Manual.17,18
Univariate associations of potential risk factors with study outcomes were examined by using χ2, Wilcoxon rank-sum, t,or F tests, as appropriate. In addition to risk factors with univariate P < .20, clinically relevant variables (age, race, income, job status, parity) were included in all multivariate models for face validity. Proportional odds models and data for the entire sample were used to assess risk-factor effects on frequency of sexual activity as an ordinal categorical outcome.19 These models capture the ordering of the outcome categories but avoid treating them as quantitative. In these models, an odds ratio greater than 1.00 signals an association with less frequent activity. The proportional odds assumption was validated by informally comparing the magnitude of odds ratios for the association of each predictor with different dichotomizations of the ordinal frequency outcome, that is, with any activity, at least monthly activity, and at least weekly activity. The remaining analyses were conducted using data for the subset of women reporting any sexual activity. Linear regression was used to assess independent associations with the sexual dysfunction score, whereas different sexual problems and satisfaction were assessed as binary outcomes using logistic models. In exploratory analysis, possible confounding, mediation, and interactions were investigated. Interactions between relationship status and African-American race found in several models were accommodated by estimating the association between African-American race and each outcome stratified by whether or not the participant reported a significant relationship. P ≤ .05 was considered statistically significant in all multivariate models. All analyses were carried out with SAS 8.02 (SAS Institute, Cary, NC).
RESULTS
The mean age of the women was 55.9 years (± 8), and 89% reported good-to-excellent overall general health. Slightly less than half the women self-identified as white (47.6%), with the remaining half approximately equally self-identifying as African American (18.2%), Hispanic (16.6%), and Asian American (16.4%). Most women were married or in a long-term relationship (69%). Eighty percent had some college education, and 65% were employed. Over three fourths of the women had delivered at least one baby, and 65% were postmenopausal (Table 1).
Table 1. Characteristics of the RRISK cohort (n=2109).
| VARIABLE |
MEAN±SD OR
N (%) |
|---|---|
|
| |
| Age | 55.9±8.6 |
| Race/Ethnicity | |
| Caucasian | 1003 (47.6) |
| African-American | 383 (18.2) |
| Asian | 345 (16.4) |
| Hispanic | 350 (16.6) |
| Native American/Other | 28 (1.3) |
| Relationship Status | |
| Married/In relationship | 1464 (69.4) |
| Education | |
| ≤ High School | 421 (20.0) |
| Some College\Bachelor’s | 1421 (67.4) |
| Graduate Degree | 265 (12.6) |
| Income (dollars/year) | |
| <40,000 | 471 (22.3) |
| 40,000-59,999 | 436 (20.7) |
| 60,000-79,999 | 411 (19.5) |
| 80,000-99,999 | 263 (12.5) |
| ≥100,000 | 368 (17.5) |
| Job Status | |
| Retired/Student/Homemaker | 645 (30.6) |
| Employed | 1364 (64.7) |
| Unemployed/Other | 97 (4.6) |
| Smoking | |
| Never | 1202 (57.0) |
| Former | 695 (33.0) |
| Current | 212 (10.1) |
| Alcohol Consumption | |
| Never | 335 (15.9) |
| Former | 493 (23.4) |
| Current | 1281 (60.7) |
| Health | |
| Excellent | 362 (17.2) |
| Very Good/Good | 1503 (71.3) |
| Fair/Poor | 244 (11.6) |
|
| |
| Body Mass Index (BMI, kg/m2) | |
| <25 | 717 (34.0) |
| 25-<30 | 661 (31.3) |
| ≥30 | 719 (34.1) |
| Waist-hip ratio | 0.81±0.07 |
| Parity (+/−) | 1716 (81.4) |
| Menopause | 1378 (65.3) |
| Ever HRT use | 1048 (49.7) |
| Hysterectomy | 475 (22.5) |
| Ever POP | 159 (7.5) |
| ≥Weekly Urinary Incontinence (UI) | 603 (28.6) |
| SF-36 Mental Component Scale (MCS) | 44.5±5.8 |
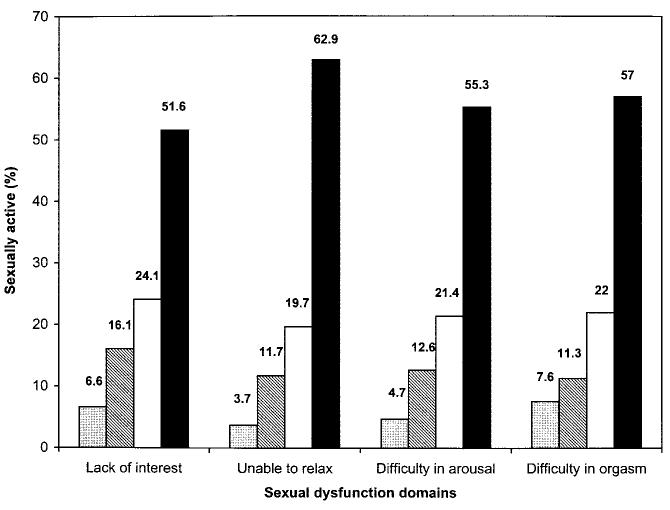
Overall, 71% (n = 1,493) of the women were sexually active in the last year, with 37% reporting monthly or less often sexual activity, 33% weekly, and less than 1% having daily sexual activity. Among sexually active women, nearly two thirds were some- what or very satisfied with their sexual activity. The prevalence of sexual dysfunction was 45% in the entire group and 33% of those who reported sexual activity. When we included only those responses of “somewhat of a problem” and “very much a problem,” the prevalence of sexual dysfunction was 24% (Table 2 and Fig. 1).
Table 2. Summary of Sexual Outcomes in RRISK cohort**.
| Variable | n (%) |
|---|---|
|
| |
| * Any sexual activity | 1493 (70.8) |
|
| |
| * Sexual Frequency | |
| No activity | 587 (27.8) |
| <Monthly | 249 (11.8) |
| Monthly | 536 (25.4) |
| Weekly | 696 (33.0) |
| Daily | 18 (0.85) |
|
| |
| † Sexual Satisfaction | |
| Very Dissatisfied | 100 (6.7) |
| Somewhat Dissatisfied | 137 (9.2) |
| Neither Satisfied nor Dissatisfied | 263 (17.6) |
| Somewhat Satisfied | 490 (32.8) |
| Very Satisfied | 478 (32.0) |
|
| |
| † Sexual Dysfunction | |
| Any dysfunction | 486 (32.6) |
due to missing responses from participants, percents will not add exactly
% out of entire cohort (n=2109)
% out of women who reported sexual activity (n=1493)
Fig.1.
Sexual dysfunction among subjects who are sexually active (n = 1,493).Gray bars,very much of a problem; hatched bars, some what of a problem; white bars, little bit of a problem; black bars, not a problem.
Table 3 reports sexual activity across selected demographic and other characteristics. This distribution shows that younger women report more sexual activity. About 70% of women in a significant relationship and 33% of those not in a relationship have at least monthly sexual activity. Women with higher levels of education and income reported higher frequencies of sexual activity. The monthly and greater than weekly sexual frequency groups were more likely to be women who had never smoked, currently drank alcohol, had lower BMI levels, and better health status.
Table 3. Univariate Predictors of Frequency of Sexual Activity in the RRISK cohort*.
| Variable | No activity n=587 |
< Monthly activity n=226 |
Monthly activity n=535 |
≥Weekly activity n=712 |
p-value |
|---|---|---|---|---|---|
|
| |||||
| Age | 60.5±8.1 | 56.9±8.0 | 54.9±8.2 | 52.5±7.8 | <0.001 |
| Relationship Status | |||||
| Not in relationship | 352 (54.8) | 66 (10.3) | 107 (16.7) | 102 (15.9) | <0.001 |
| Married/In relationship | 235 (16.1) | 160 (10.9) | 426 (29.1) | 610 (41.7) | |
| Race | |||||
| White/Caucasian | 291 (29.0) | 106 (10.6) | 242 (24.1) | 345 (34.4) | 0.07 |
| African-American | 120 (31.3) | 44 (11.5) | 98 (25.6) | 107 (27.9) | |
| Asian | 84 (24.4) | 45 (13.0) | 95 (27.5) | 112 (32.5) | |
| Hispanic | 88 (25.1) | 29 (8.3) | 92 (26.3) | 135 (38.6) | |
| Native American/Other | 4 (14.3) | 2 (7.1) | 8 (28.6) | 13 (46.4) | |
| Education | |||||
| ≤HS | 166 (39.4) | 40 (9.5) | 82 (19.5) | 125 (29.7) | <0.001 |
| Some college/Bachelor’s | 371 (26.1) | 154 (10.8) | 372 (26.2) | 489 (34.4) | |
| Graduate Degree | 49 (18.5) | 32 (12.1) | 81 (30.6) | 98 (37.0) | |
| Income (dollars/year) | |||||
| <40,000 | 233 (49.5) | 51 (10.8) | 84 (17.8) | 92 (19.5) | <0.001 |
| 40,000-59,999 | 140 (32.1) | 48 (11.0) | 117 (26.8) | 120 (27.5) | |
| 60,000-79,999 | 94 (22.9) | 49 (11.9) | 101 (24.6) | 160 (38.9) | |
| 80,000-99,999 | 32 (12.2) | 20 (7.6) | 94 (35.7) | 113 (43.0) | |
| ≥100,000 | 30 (8.2) | 46 (12.5) | 107 (29.1) | 183 (49.7) | |
| Job Status | |||||
| Retired\Student\Homemaker | 256 (39.7) | 76 (11.8) | 141 (21.9) | 160 (24.8) | <0.001 |
| Employed | 298 (21.9) | 139 (10.2) | 370 (27.1) | 523 (38.3) | |
| Unemployed\Other | 32 (33.0) | 10 (10.3) | 24 (24.7) | 29 (29.9) | |
| Smoking | |||||
| Never | 299 (24.9) | 133 (11.1) | 312 (26.0) | 429 (35.7) | 0.02 |
| Former | 217 (31.2) | 70 (10.1) | 181 (26.0) | 213 (30.7) | |
| Current | 71 (33.5) | 23 (10.9) | 42 (19.8) | 70 (33.0) | |
| Alcohol Consumption | |||||
| Never | 127 (37.9) | 34 (10.2) | 70 (20.9) | 96 (28.7) | <0.001 |
| Former | 174 (35.3) | 59 (12.0) | 121 (24.5) | 127 (25.8) | |
| Current | 286 (22.3) | 133 (10.4) | 344 (26.9) | 489 (38.2) | |
| Health | |||||
| Excellent | 80 (22.1) | 33 (9.1) | 93 (25.7) | 148 (40.9) | <0.001 |
| Very Good/Good | 402 (26.8) | 165 (11.0) | 391 (26.0) | 511 (34.0) | |
| Fair/Poor | 105 (43.0) | 28 (11.5) | 51 (20.9) | 53 (21.7) | |
|
| |||||
| BMI (kg/m2) | |||||
| <25 | 155 (21.6) | 77 (10.7) | 183 (25.5) | 288 (40.2) | <0.001 |
| 25-<30 | 182 (27.5) | 64 (9.7) | 175 (26.5) | 217 (32.8) | |
| ≥30 | 246 (34.2) | 82 (11.4) | 176 (24.5) | 203 (28.2) | |
| Waist-hip ratio | 0.83±0.06 | 0.82±0.07 | 0.81±0.07 | 0.80±0.06 | <0.001 |
| Parity (+/−) | 475 (27.7) | 179 (10.4) | 443 (25.8) | 578 (33.7) | 0.76 |
| Menopause | 488 (35.4) | 159 (11.5) | 344 (25.0) | 358 (26.0) | <0.001 |
| Ever HRT use | 336 (32.1) | 120 (11.5) | 254 (24.2) | 317 (30.3) | <0.001 |
| Hysterectomy | 159 (33.5) | 42 (8.8) | 119 (25.1) | 147 (31.0) | 0.02 |
| Ever POP | 60 (37.8) | 20 (12.6) | 35 (22.0) | 42 (26.4) | 0.02 |
| UI (≥Weekly) | 195 (32.3) | 73 (12.1) | 142 (23.6) | 183 (30.4) | 0.009 |
| SF-36 MCS | 44.3±6.2 | 44.4±6.2 | 44.4±5.6 | 44.7±5.4 | 0.71 |
Kruskal-Wallis, ANOVA, or chi-squared test used where appropriate.
In our proportional odds model for frequency, with frequency being defined as never, less than monthly, monthly, and weekly/daily, we found that older women and Asian women reported less frequent sexual activity whereas women with a higher income, those in a significant relationship, and those who had moderate alcohol intake reported more frequent sexual activity (Table 4).
Table 4. Predictors of Sexual Frequency* (n=2060).
| Variable | Odds Ratio |
95% CI | p-value |
|---|---|---|---|
|
| |||
| Age (per 10 years) | 2.33 | 1.97-2.75 | <0.001 |
| Race | |||
| White | ref | -- | -- |
| African-American, relationship | 0.74 | 0.53-1.02 | 0.07 |
| African-America, no relationship | 1.15 | 0.79-1.67 | 0.48 |
| Asian | 1.48 | 1.13-1.94 | 0.005 |
| Hispanic | 0.95 | 0.73-1.23 | 0.69 |
| Native Amer./Other | 0.85 | 0.37-1.99 | 0.71 |
| Income | |||
| <$40,000 | ref | -- | -- |
| $40,000-$59,999 | 0.79 | 0.60-1.03 | 0.09 |
| $60,000-$79,999 | 0.71 | 0.53-0.94 | 0.02 |
| $80,000-$99,000 | 0.61 | 0.44-0.85 | 0.003 |
| ≥$100,000 | 0.55 | 0.41-0.75 | <0.001 |
| Job Status | |||
| Retired\Student\Homemaker | ref | -- | -- |
| Employed | 0.98 | 0.77-1.24 | 0.86 |
| Unemployed\Other | 1.30 | 0.81-2.08 | 0.28 |
| Parity | |||
| None | ref | -- | -- |
| ≥One | 0.86 | 0.68-1.10 | 0.23 |
| Relationship Status | |||
| Married/In relationship vs. none | 0.24 | 0.18-0.31 | <0.001 |
| Drinking Status | |||
| None | ref | -- | -- |
| Former | 0.70 | 0.52-0.94 | 0.02 |
| Current | 0.48 | 0.37-0.63 | <0.001 |
| Ever HRT use (vs. none) | 0.87 | 0.71-1.07 | 0.18 |
| Daily/Weekly UI (vs. none) | 1.00 | 0.82-1.23 | 0.98 |
| Menopause (vs. pre-menopause) | 1.13 | 0.87-1.46 | 0.35 |
| BMI | |||
| <25 | ref | -- | -- |
| 25-<30 | 1.50 | 1.19-1.87 | <0.001 |
| ≥30 | 1.70 | 1.34-2.15 | <0.001 |
Sexual frequency is categorized as never, less than monthly, monthly, and weekly/daily.
In our multivariate logistic model for satisfaction, less satisfaction was correlated with an increasing BMI. Compared with white women, women in each of the other race/ethnicity groups were more sexually satisfied, but the results were only significant for African-American women. Higher (more favorable) scores on the SF-36 scale for mental health were associated with greater sexual satisfaction (Table 5).
Table 5. Predictors of Sexual Dissatisfaction* (n=1420).
| Variable | Odds Ratio |
95% CI | p-value |
|---|---|---|---|
|
| |||
| Age (per 10 years) | 1.07 | 0.86-1.32 | 0.55 |
| Education | |||
| <=HS | ref | -- | -- |
| Some college\Bachelor’s | 0.84 | 0.62-1.15 | 0.28 |
| Graduate Degree | 1.11 | 0.73-1.68 | 0.63 |
| Race | |||
| White | ref | -- | -- |
| African-American | 0.68 | 0.48-0.95 | 0.02 |
| Asian | 0.89 | 0.64-1.24 | 0.49 |
| Hispanic | 0.88 | 0.63-1.22 | 0.43 |
| Native Amer./Other | 0.73 | 0.27-1.97 | 0.54 |
| Job Status | |||
| Retired\Student\Homemaker | ref | -- | -- |
| Employed | 0.97 | 0.71-1.32 | 0.85 |
| Unemployed\Other | 0.99 | 0.53-1.82 | 0.97 |
| Relationship Status | |||
| Married\In relationship vs. none | 0.78 | 0.58-1.04 | 0.09 |
| Health | |||
| Excellent | ref | -- | -- |
| Very Good/Good | 1.09 | 0.80-1.48 | 0.59 |
| Fair/Poor | 1.44 | 0.89-2.31 | 0.13 |
| Parity | |||
| None | ref | -- | -- |
| ≥One | 0.91 | 0.67-1.22 | 0.52 |
| Ever HRT use (vs. never) | 1.11 | 0.85-1.44 | 0.46 |
| ≥Weekly UI (vs. none) | 1.00 | 0.77-1.30 | 0.98 |
| Menopause (vs. pre-menopause) | 1.22 | 0.89-1.68 | 0.22 |
| BMI | |||
| <25 | ref | -- | -- |
| 25-<30 | 1.39 | 1.05-1.84 | 0.02 |
| ≥30 | 1.47 | 1.09-1.98 | 0.01 |
| SF-36 MCS | 0.97 | 0.95-0.99 | 0.006 |
Sexual dissatisfaction is defined as very dissatisfied, somewhat dissatisfied, neither satisfied nor dissatisfied. Satisfaction is defined as somewhat satisfied or very satisfied.
Table 6 shows the correlates for the overall sexual dysfunction score. Because we found an interaction between African-American race and relationship, the African American group was split into significant relationship and no relationship. African-American women in significant relationships and women with better mental health scores reported lower levels of sexual dysfunction (a lower score on the continuous sexual dysfunction scale) compared with other women. Correlates for increased sexual dysfunction were being in a higher educational level, poor health, and being in a significant relationship. When we defined sexual dysfunction as a response of greater than or equal to “somewhat” in one of the four domains, we found that less dysfunction was correlated with a decreased score on the mental health scale while greater dysfunction was correlated with being in a significant relationship and daily or weekly urinary incontinence (data not presented).
Table 6. Multivariate Predictors of Sexual Problem Scale Among Women Who are Sexually Active (n=1418).
| Beta Coefficient (95% CI) | p value | |
|---|---|---|
| Age (per 10 years) | −1.18 (−3.63, 1.27 ) | 0.35 |
| Race | ||
| Caucasian | ref | -- |
| African American (significant relationship) | −7.72 (−12.02, −3.42) | <0.001 |
| African American (no relationship) | −1.66 (−8.28, 4.95) | 0.62 |
| Asian | −3.14 (−6.85, 0.57) | 0.10 |
| Hispanic | −1.78 (−5.53, 1.96) | 0.35 |
| Native American/Other | −6.12 (−16.84, 4.60) | 0.26 |
| Job Status | ||
| Retired/Student/Homemaker | ref | -- |
| Employed | −0.34 (−3.85, 3.17) | 0.86 |
| Unemployed | −5.62 (−12.77, 1.52) | 0.12 |
| Education level | ||
| ≤ High School Graduate | ref | -- |
| ≤College Graduate | 2.87 (−0.72, 6.46) | 0.11 |
| Graduate Degree | 5.52 (0.66, 10.39) | 0.03 |
| Health | ||
| Excellent | ref | -- |
| Very Good/Good | 0.82 (−2.55, 4.20) | 0.63 |
| Fair/Poor | 6.87 (1.45, 12.28) | 0.013 |
| Parity | ||
| None | ref | -- |
| ≥1 | 2.13 (−1.34, 5.60) | 0.23 |
| Significant Relationship vs. No Relationship | 13.33 (9.43, 17.23) | <0.001 |
| Hormone Replacement Therapy vs. None | 2.42 (−0.64, 5.49) | 0.12 |
| Daily/Weekly Urinary Incontinence vs. None | 0.45 (−2.50, 3.39) | 0.77 |
| Menopause (vs. pre-menopause) | 4.42 (0.78, 8.06) | 0.02 |
| Mental Health (SF-36, per 1 point) | −0.93 (−1.17, −0.70) | <0.001 |
DISCUSSION
In this analysis of RRISK, a cohort of 2,109 women, we examined the correlates for sexual activity and frequency, satisfaction, and sexual dysfunction. In each of these categories, demographic characteristics were strongly predictive. Younger age, being in a relationship, higher education, not smoking, a history of moderate alcohol use, and lower BMI were associated with reporting sexual activity. Of sexually active women, those with a higher income, in a significant relationship, and with moderate alcohol intake were more likely to report more frequent sexual activity. Satisfaction with sexual activity was correlated with being African American, having a lower BMI, and a higher score on our mental health scale. Women reporting sexual dysfunction were more likely to have a higher education level, have poor health, and be in a significant relationship.
There is little epidemiologic data on prevalence and predictors of female sexual dysfunction, particularly for older women. The 4 categories of sexual dysfunction that we evaluated were sexual desire disorder, sexual arousal disorder, orgasmic disorder, and sexual pain disorder. The diagnostic classification system adapted for this study reflects internationally recognized classification and definitions of sexual dysfunction.8 This analysis examines a large group of middle-aged and older women for the correlates to sexual function and activity. For prevalence of sexual dysfunction, our data are consistent with data from previous studies.
Initial studies have reported a decline in sexual activity in women as they age, associated with a decline in subjective and objective health ratings.20,21 One study confirmed that sexual activity among both women and men decreases with age and is highly dependent on marital status.22 Additional population studies have confirmed these limited findings.13,23 Studies of general populations of women of all ages have found that between 40% and 60% of women report some sexual dysfunction.9-12,24 In an analysis of the National Health and Social Life Survey, 43% of women reported sexual dysfunction, encompassing lack of interest, inability to achieve orgasm, pain with sex, lack of pleasure, anxiety, and trouble lubricating. This analysis also found that dysfunction in women was correlated with nonwhite race, lower education level, and psychosocial stress.6 more recently, the same investigator reported prevalence of sexual dysfunction among 40- to 80-year-old women as 43% worldwide.25
An analysis of sexual functioning in a young group of postmenopausal women (mean age 56 years) found that the most reported reason for sexual inactivity was lack of a healthy partner. In this study 64% of the women reported sexual activity. A higher BMI, increased physical activity, increased life satisfaction, and unmarried status were related to higher global sexual function.26 In a cohort of older postmenopausal women (mean age 68 years) with osteoporosis, baseline data showed that 46% reported some sexual activity, and among those women the most reported problem was difficulty with orgasm.27 Correlates for sexual dysfunction noted in additional studies include increasing age, low education level, and chronic disease.12
We also found that with increased age comes a decrease in sexual activity. Aging and menopausal status have been negatively associated with sexual activity.3 Declining estrogen and testosterone affect sexual desire, sexual response, and urogenital health.5 Commonly reported sexual problems include change in sexual desire and dyspareunia.4 Our findings were slightly different when examining sexual activity and function in aging women. Although younger women were more likely to have more sexual activity, we found no age difference when examining sexual satisfaction or dysfunction.
We showed that higher socioeconomic status (higher education and higher income) was correlated with increased sexual activity, but increased education status was also correlated with increasing sexual dysfunction. These results do not necessarily agree with previous epidemiologic findings about sexual dysfunction in women.6 These results could differ from past findings because of differences in our population (older women, members of a large health management organization, versus a wide age range from a national sample) or differences in our research design (population-based cohort versus a probability sample study).
Relationship status was a significant correlate in many of our models. Women in a relationship were much more likely to have greater than monthly sexual activity. We also found that being in a relationship was correlated with more sexual dysfunction when compared with women not in a relationship. This finding is surprising, yet agrees with a recent report on a large group of postmenopausal women with heart disease.28 This association remained significant in a model that stratified the subjects by frequency of sexual activity.
In our analysis for satisfaction, we found that African-American race was correlated with increased sexual satisfaction when compared with white women. In our analysis for sexual dysfunction, African-American participants in a relationship were inversely correlated with any sexual dysfunction. This result is different from previous findings that analyzed women of all ages. This finding could be due to the age range of our cohort compared with those previously analyzed. Another possible explanation is that, because we included a larger number of African-American women than were included in other studies, we were able to find an inverse association that had not been previously reported.
We found that a higher education level was correlated with an increase in overall dysfunction. One reason for this correlation between dysfunction and education level could be the different stressors in the lives of women with different education levels. Another explanation could be the differing priorities and expectations for sexual activity in women with different levels of education.
Our study presents novel results for satisfaction with sex, an outcome that has not been studied in detail. As noted above, we found that African-American race is correlated with increased satisfaction. Better mental health is also correlated with increased satisfaction, whereas increased BMI was correlated with less satisfaction with sex. These correlates for satisfaction reveal new data that has not been shown in other epidemiologic studies.
At least one previous study has shown that post-menopausal women abstinent from alcohol for a longer period of time show greater satisfaction with the sexual aspects of their lives.29 We did not find this result in our study, with sexual satisfaction being similar among women of all drinking statuses (never, former, and current). There was no difference in function or frequency between these groups either. We did find a correlation between current and former alcohol use and increase in frequency of sexual activity (at least monthly) versus never-users. This could be explained by the possible decrease in inhibitions that is theoretically caused by drinking, or drinking may be a marker for other factors that are associated with increasing sexual activity.
Our results may not be generalizable to a variably insured or uninsured population because of the nature of our study population. Our cohort included relatively few women who were not in significant relationship, and with stratification we found that our statistical models for this group were underpowered, leading us to believe that, with a larger group of women not in a relationship, we might have discovered more correlates for sexual frequency and dysfunction in this group.
In summary, we found that middle-aged and older women engage in frequent and satisfying sexual activity and also report sexual dysfunction. Women’s health providers need to be aware of their patients' continuing interest in sexual activity, screen for sexual dysfunction, and treat any dysfunction with care and sensitivity.
APPENDIX 1: MEMBERS OF THE REPRODUCTIVE RISK FACTORS FOR INCONTINENCE STUDY AT KAISER (RRISK) STUDY GROUP
Jeanette Brown, MD (UCSF) Leslee L. Subak, MD (UCSF) W. Conrad Sweeting Jr, MD (Kaiser Northern California) David H. Thom, MD, MPH, PhD (UCSF) Stephen Van Den Eeden, PhD (Kaiser Northern California Division of Research) Ching S. Lin, PhD (UCSF) Emil A. Tanagho, MD (UCSF) Tom F. Lue, MD, Co-Director (UCSF) Eric Vittinghoff, PhD (UCSF)
APPENDIX 2: SEXUAL FUNCTIONING
These next questions are about the way health problems might interfere with your sex life. These questions are personal, but your answers are important in understanding how health problems affect women’s lives.
- 1. During the past 12 months, have you been sexually active? Sexual activity is any activity that is sexually arousing to you, including masturbation.
- ___ Yes → Go to question 2.
- ___ No
- If no, indicate reason and then go to next section of questionnaire.
- 1a. I am not sexually active because (mark as many items that apply)
- ___ I am not interested
- ___ I have a physical problem that makes sexual activity difficult or uncomfortable
- ___ I do not have a partner at this time
- ___ I have a partner, but my partner is not interested
- ___ My partner has a physical problem that makes sexual activity difficult or uncomfortable
- ___ Other
- 2. During the past 12 months, have you had a sexual partner?
- ___ No
- ___ Yes
- 3. During the past 12 months, on average, how frequently did you have sexual activity? Sexual activity is any activity that is sexually arousing to you, including masturbation.
- ___ Less than monthly
- ___ Monthly (once or more each month)
- ___ Weekly (once or more each week)
- ___ Daily (once or more each day)
- 4. How much of a problem was each of the following during the past 12 months?
- Not a problem
- Little bit of a problem
- Somewhat of a problem
- Very much a problem
- Not applicable
- Lack of sexual interest
- Unable to relax and enjoy sexual activity
- Difficulty in becoming sexually aroused
- Difficulty in having an orgasm
- During the past 12 months, on average, how would you rate your overall level of sexual satisfaction?
- ___ Very dissatisfied
- ___ Somewhat dissatisfied
- ___ Neither satisfied nor dissatisfied
- ___ Somewhat satisfied
- ___ Very satisfied
REFERENCES
- 1.Frank E, Anderson C, Rubinstein D. Frequency of sexual dysfunction in “normal” couples. N Engl J Med. 1978;299:111–5. doi: 10.1056/NEJM197807202990302. [DOI] [PubMed] [Google Scholar]
- 2.Spector IP, Carey MP. Incidence and prevalence of the sexual dysfunctions: a critical review of the empirical literature. Arch Sex Behav. 1990;19:389–408. doi: 10.1007/BF01541933. [DOI] [PubMed] [Google Scholar]
- 3.Rosen RC, Taylor JF, Leiblum SR, Bachmann GA. Prevalence of sexual dysfunction in women: results of a survey study of 329 women in an outpatient gynecological clinic. J Sex Marital Ther. 1993;19:171–88. doi: 10.1080/00926239308404902. [DOI] [PubMed] [Google Scholar]
- 4.Sarrel PM. Sexuality and menopause. Obstet Gynecol. 1990;75(suppl):26S–35S. [PubMed] [Google Scholar]
- 5.Sarrel PM, Whitehead MI. Sex and menopause: defining the issues. Maturitas. 1985;7:217–24. doi: 10.1016/0378-5122(85)90043-x. [DOI] [PubMed] [Google Scholar]
- 6.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]; JAMA. JAMA. 1999;1999;281281:1174, 537–44. [Google Scholar]
- 7.Laumann EO, Gagnon JH, Michael RT, Michaels S. The social organization of sexuality: sexual practices in the United States. University of Chicago Press; Chicago (IL): 1994. [Google Scholar]
- 8.Basson R, Berman J, Burnett A, Derogatis L, Ferguson D, Fourcroy J, et al. Report of the international consensus development conference on female sexual dysfunction: definitions and classifications. J Urol. 2000;163:888–93. [PubMed] [Google Scholar]
- 9.Mercer CH, Fenton KA, Johnson AM, Wellings K, Macdowall W, McManus S, et al. Sexual function problems and help seeking behaviour in Britain: national probability sample survey. doi: 10.1136/bmj.327.7412.426. [DOI] [PMC free article] [PubMed] [Google Scholar]; BMJ. BMJ. 2003;2003;327327:649, 426–7. [Google Scholar]
- 10.Nazareth I, Boynton P, King M. Problems with sexual function in people attending London general practitioners: cross sectional study. BMJ. 2003;327:423. doi: 10.1136/bmj.327.7412.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Geiss IM, Umek WH, Dungl A, Sam C, Riss P, Hanzal E. Prevalence of female sexual dysfunction in gynecologic and urogynecologic patients according to the international consensus classification. Urology. 2003;62:514–8. doi: 10.1016/s0090-4295(03)00487-4. [DOI] [PubMed] [Google Scholar]
- 12.Abdo CH, Oliveira WM, Moreira ED, Fittipaldi JA. Prevalence of sexual dysfunctions and correlated conditions in a sample of Brazilian women: results of the Brazilian Study on Sexual Behavior (BSSB) Int J Impot Res. 2004;16:160–6. doi: 10.1038/sj.ijir.3901198. [DOI] [PubMed] [Google Scholar]
- 13.Patel D, Gillespie B, Foxman B. Sexual behavior of older women: results of a random-digit-dialing survey of 2,000 women in the United States. Sex Transm Dis. 2003;30:216–20. doi: 10.1097/00007435-200303000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82:703–10. doi: 10.2105/ajph.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thom DH, Van den Eeden SK, Ragins AI, Wassel-Fyr CL, Vittinghof E, Subak LL, et al. Differences in prevalence of urinary incontinence by race/ethnicity. J Urol. 2006;175:259–64. doi: 10.1016/S0022-5347(05)00039-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sherbourne CD. Social functioning: sexual problems measures. In: Stewart AL, Ware JE, editors. Measuring functioning and well-being: the medical outcomes study approach. Duke University Press; Durham (NC): 1992. pp. 194–204. [Google Scholar]
- 17.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 18.Ware JE, Kosinski M, editors. The SF-36 Physical and Mental Health Summary Scales: a manual for users of version 1. 2 nd ed. QualityMetric Incorporated; Lincoln (RI): 2001. Norm-based scoring for physical and mental summary measures. [Google Scholar]
- 19.Ananth CV, Kleinbaum DG. Regression models for ordinal responses: a review of methods and applications. Int J Epidemiol. 1997;26:1323–33. doi: 10.1093/ije/26.6.1323. [DOI] [PubMed] [Google Scholar]
- 20.Verwoerdt A, Pfeiffer E, Wang H. Sexual behavior in senescence. II. Patterns of sexual activity and interest. Geriatrics. 1969;24:137–54. [PubMed] [Google Scholar]
- 21.Pfeiffer E, Davis GC. Determinants of sexual behavior in middle and old age. J Am Geriatr Soc. 1972;20:151–8. doi: 10.1111/j.1532-5415.1972.tb00789.x. [DOI] [PubMed] [Google Scholar]
- 22.Diokno AC, Brown MB, Herzog AR. Sexual function in the elderly. Arch Intern Med. 1990;150:197–200. [PubMed] [Google Scholar]
- 23.Avis NE. Sexual function and aging in men and women: community and population-based studies. J Gend Specif Med. 2000;3:37–41. [PubMed] [Google Scholar]
- 24.Nusbaum MR, Gamble G, Skinner B, Heiman J. The high prevalence of sexual concerns among women seeking routine gynecological care. J Fam Pract. 2000;49:229–32. [PubMed] [Google Scholar]
- 25.Laumann EO, Nicolosi A, Glasser DB, Paik A, Gingell C, Moreira E, et al. Sexual problems among women and men aged 40-80 y: prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. Int J Impot Res. 2005;17:39–57. doi: 10.1038/sj.ijir.3901250. [DOI] [PubMed] [Google Scholar]
- 26.Greendale GA, Hogan P, Shumaker S. Sexual functioning in postmenopausal women: the Postmenopausal Estrogen/Progestin Interventions (PEPI) trial. J Womens Health. 1996;5:445–58. [Google Scholar]
- 27.Modugno F, Ness RB, Ewing S, Cauley JA. Effect of raloxifene on sexual function in older postmenopausal women with osteoporosis. Obstet Gynecol. 2003;101:353–61. doi: 10.1016/s0029-7844(02)02589-9. [DOI] [PubMed] [Google Scholar]
- 28.Addis IB, Ireland CC, Vittinghoff E, Lin F, Stuenkel CA, Hulley S. Sexual activity and function in postmenopausal women with heart disease. Obstet Gynecol. 2005;106:121–7. doi: 10.1097/01.AOG.0000165276.85777.fb. [DOI] [PubMed] [Google Scholar]
- 29.Gavaler JS, Rizzo A, Rossaro L, Van Thiel DH, Brezza E, Deal SR. Sexuality of alcoholic postmenopausal women: effects of duration of alcohol abstinence. Alcohol Clin Exp Res. 1994;18:269–71. doi: 10.1111/j.1530-0277.1994.tb00013.x. [DOI] [PubMed] [Google Scholar]