Abstract
OBJECTIVE: To estimate costs of routine care for female urinary incontinence, health-related quality of life, and willingness to pay for incontinence improvement.
METHODS: In a cross-sectional study at 5 U.S. sites, 293 incontinent women quantified supplies, laundry, and dry cleaning specifically for incontinence. Costs were calculated by multiplying resources used by national resource costs and presented in 2005 United States dollars ($2005). Health-related quality of life was estimated with the Health Utilities Index. Participants estimated willingness to pay for 25-100% improvement in incontinence. Potential predictors of these outcomes were examined using multivariable linear regression.
RESULTS: Mean age was 56 ± 11 years; participants were racially diverse and had a broad range of incontinence severity. Nearly 90% reported incontinence-related costs. Median weekly cost (25%, 75% interquartile range) increased from $0.37 ($0, 4) for slight to $10.98 ($4, 21) for very severe incontinence. Costs increased with incontinence severity (P < .001). Costs were 2.4-fold higher for African American compared with white women (P < .001) and 65% higher for women with urge compared with those having stress incontinence (P < .001). More frequent incontinence was associated with lower Health Utilities Index score (mean 0.90 ± 0.11 for weekly and 0.81 ± 0.21 for daily incontinence; P = .02). Women were willing to pay a mean of $70 ± $64 per month for complete resolution of incontinence, and willingness to pay increased with income and greater expected benefit.
CONCLUSION: Women with severe urinary incontinence pay $900 annually for incontinence routine care, and incontinence is associated with a significant decrement in health-related quality of life. Effective incontinence treatment may decrease costs and improve quality of life.
LEVEL OF EVIDENCE: III
Urinary incontinence is common in women and is associated with tremendous “costs.” In addition to high economic costs, incontinence results in medical and psychological morbidity and adverse effects on quality of life.1,2 The most recent estimate of the annual direct costs of incontinence in all ages was over $16 billion (in 1995 dollars),3 which is greater than the annual direct costs for breast, ovarian, cervical, and uterine cancers combined.4 A majority (50-75%) of the cost of incontinence is attributed to routine care, including absorbent pads, protection, and laundry.3,5 Routine care costs are reported as $50 to $1,000 per person per year, varying widely between studies and by method of cost determination.6-9 Despite the great economic burden of incontinence, the largest cost category, routine care costs, is poorly described, and there are limited data on predictors of incontinence-related spending.
In addition to economic costs, incontinence substantially affects quality of life. Although there are many studies quantifying the effect of incontinence on general and incontinence-specific quality of life using instruments like the Short Form (SF-36) Health Survey and Incontinence Impact Questionnaire, respectively, there are few data on the impact of incontinence on health-related quality of life measured by health utilities instruments. In one study, urinary incontinence, Alzheimer’s disease, and stroke are the 3 chronic health conditions that most adversely effect an individual’s health-related quality of life.10 The advantage of determining health-related quality of life is that it allows comparison between different health conditions and can be used for cost-utility analysis. Willingness to pay for incontinence improvement is another measure of the physical and psychological burden of incontinence. The willingness-to-pay method ascertains what people would be willing to pay for a defined intervention and outcome. This method has been used in other chronic conditions like asthma, osteoarthritis, and migraine headache. To date, there are limited data on willingness to pay for incontinence improvement.11-13 We conducted this study to provide accurate estimates of the economic costs of routine care for incontinence, health-related quality of life associated with incontinence, and willingness to pay for incontinence improvement.
PATIENTS AND METHODS
From March through December 2004, 301 community-dwelling women were enrolled in the Diagnostic Aspects of Incontinence Study (DAISy), a cross-sectional study at 5 sites in the United States (Brown JS, Bradley CJ, Subak LL, et al. A simple test to distinguish urge and stress urinary incontinence. Ann Intern Med, in press). The study was designed to assess the reproducibility and accuracy of a self-administered questionnaire to distinguish urge from stress incontinence. The study protocol was approved by the Institutional Review Board at University of California, San Francisco, where the study was coordinated, and at each of the 5 clinical sites. All participants provided written informed consent.
Women were recruited through newspaper advertisements and flyers (93%) and urology and gynecology clinics (6%). Eligible women were ambulatory, 40 years of age or older, did not have a urinary tract infection, reported 3 or more incontinence episodes per week for at least 3 months, and were bothered enough by their incontinence to seek treatment. The study excluded incontinent women with complex problems more appropriate for specialist referral or who had been treated for incontinence in the prior 3 months.
Data were collected by self-report questionnaires. Resources used for routine care were assessed by the question “During a typical week, how many of each of the supplies listed below do you use specifically for your urine leakage?” Supplies included panty liners or minipads, maxipads, incontinence pads, urethral inserts, toilet paper (number of changes), and paper towels (number of sheets). Laundry was assessed by the question “During a typical week, how many loads of wash do you do because of your urine leakage?” and dry cleaning by “During a typical week, how many items of clothing do you dry clean because of your urine leakage?” Participants recorded the number of each type of clothing dry-cleaned per week, including pants, skirts, dresses, suits, and blouses.
National unit costs were estimated for each type of supply by a survey of 14 stores in 6 states (California [n = 8], Florida [n = 1], Colorado [n = 1], Massachusetts [n = 1], New Jersey [n = 1], and Washington [n = 1]) and one national Internet source accessed in 2001. Costs were similar between California and other states. Store types included drug chain (n = 5), food chain (n = 6), discount variety store (n = 1), medical supply store (n = 1), and Internet drug store (n = 1). The cost of a load of laundry was estimated by using the cost of one washer and dryer load at San Francisco laundromats ($1.60 wash and $1.60 dry). We used 80% of this cost ($2.50 per load) to adjust for laundromat rent and profit. The cost of dry cleaning was estimated as the average cost per garment type determined by a survey of 5 dry cleaners in each of 5 geographically distant areas in the United States (pants or skirt $4.82, blouse $4.84, 2-piece suit $9.17, dress $7.61). Because routine care costs are paid out-of-pocket by women in the United States, the analysis is from the patient’s perspective.
Health-related quality of life was evaluated with a validated patient preference measure, the Health Utilities Index Mark 3.14 The Health Utilities Index is a generic health-related quality of life measure based on standard gamble theory that has been used in both clinical and population-based health studies and provides a rapid and reproducible quantification of utilities for diverse health states. The Health Utilities Index instrument has 15 multiple-choice questions or attributes (vision, hearing, speech, ambulation, dexterity, emotion, cognition, and pain) with 5-6 severity levels per attribute, ranging from highly impaired to normal. Although none of the domains is directly associated with incontinence, the Health Utilities Index captures areas affected by the condition and is independently sensitive to incontinence.10 These categorical data on health status are translated into a utility score that reflects global health-related quality of life.
Willingness to pay for incontinence improvement was estimated by using questions derived from prior studies of incontinence.11-13 Women were asked to “imagine that a new treatment for incontinence becomes available that has no side effects. This new treatment reduces the number of times you leak urine by one quarter (25%). (For example, if you currently leak urine 4 times a day, with this new treatment you would leak urine only 3 times a day. Or if you leak urine every day, this would be reduced to 3 days out of 4.)” Women were asked to estimate “the most money that you would be willing to pay per month out of your own pocket for this treatment?” with response options of $0, $5, $10, $15, $20, $25, $30, $40, $50, $75, $100, $150, or $200 or more. Similar questions were asked for 50%, 75%, and 100% (dry) improvement in incontinence episode frequency.
Factors potentially associated with costs, health-related quality of life, and willingness to pay were assessed by self-reported questionnaires on demographic characteristics and medical history. To assess the severity of incontinence and impact on condition-specific quality of life, participants also completed a 3-day voiding diary and the Sandvik Severity Index,15 which is a combined measure of frequency and volume of loss. Incontinence episode frequency was classified as weekly (less than 7 incontinence episodes per week) or daily (7 or more incontinence episodes per week) based on the participant’s 3-day voiding diary.
Diagnosis of type of incontinence (urge alone or mixed incontinence with urge predominate [urge], stress alone or mixed incontinence with stress predominate [stress], mixed with no predominate type [mixed], or other incontinence) was determined by a urologist or urogynecologist based on an extended evaluation including medical, surgical, reproductive, and incontinence history, review of all medications, physical and pelvic examination, cough stress test, measurement of postvoid residual volume, and review of the participant’s completed 3-day voiding diary. Women with other type of incontinence (n = 8) were excluded from the analyses.
Total routine care cost was calculated by multiplying units of resources used by the average cost per unit and presented in 2005 United States dollars ($2005). Because costs were not normally distributed, we calculated the median and interquartile range, as well as mean and standard deviation (SD), for total routine care costs. Because quantile-quantile plots showed that the distributions of some costs were not normal, sensitivity analyses using Winsorization16 were also used; specifically, costs more than 2 standard deviations above the mean were reset to that limit and the analyses rerun on the data thus transformed. Summary statistics were computed for all women and recalculated, excluding women with no reported costs. Health-related quality of life was determined using the Health Utilities Index score. Health utilities are measured on a scale of zero to one, where zero is the least desirable state, associated with death, and one is the most desirable, or the best attainable health. States of health between death and perfect health are then quantified on the continuum between these extremes. We characterized willingness to pay for improvements in incontinence by plotting the proportions of women willing to pay according to the amount to be paid, stratified by the level of expected improvement.
Multivariable linear and proportional odds regression was used to estimate the independent associations of potential predictors, established a priori, and outcomes. To meet distributional assumptions, costs were modeled on the log scale; the exponentiated coefficients in this model are interpretable as the ratios of average costs in the comparison and reference groups. The ordinal scale of categorized dollar amounts capturing willingness to pay was analyzed using proportional odds models17; the trend in repeated measures of willingness across levels of improvement was evaluated using generalized estimating equations18 to account for withinsubject correlation of the amounts selected for each level of improvement. Predictors considered were age, race, annual income, health status, incontinence type (urge, stress, mixed), incontinence severity (slight, moderate, severe, very severe),15 and incontinence episode frequency (weekly, daily). Clinical site and variables with P values < .2 after adjustment were retained in the final multivariable models. The sample size was determined according to the primary aims of the study (Brown et al, Ann Intern Med, in press). In addition, confidence intervals are provided for all associations to help interpret negative as well as positive findings.19 All analyses were carried out in SAS 9.1 (SAS Institute, Cary, NC).
RESULTS
The mean (± standard deviation) age of this cohort of 293 women was 56 ± 11 years, participants were racially diverse (69% white, 13% African American, 12% Latina, and 2% Asian), and over 75% had attended college or held an advanced degree. Women reported annual household income of less than $40,000 (53%), $40,000-$99,999 (35%), and $100,000 or more (12%). Women reported a mean of 7 ± 7 years of incontinence and 30 ± 27 incontinence episodes per week. The range of incontinence severity was broad (mild 6%, moderate 58%, severe 25%, very severe 12%), and 88% had daily incontinence. Fortyone percent of women were diagnosed with urge, 45% with stress, and 14% with mixed incontinence.
Resources used each week for incontinence among women using resources are described in Table 1. Nearly 90% of women reported some costs associated with incontinence, but the 10% of women with the highest costs accounted for 50% of the total, and 50% of women accounted for 93% of the total costs. Nearly 75% of women reported using pads, with minipads the most commonly used type. Over half of women reported additional loads of laundry, and 18% reported additional dry cleaning each week for incontinence.
Table 1.
Resources Used and Costs per Week for Urinary Incontinence Among Women Using Each Resource in DAISy
| Number Used per Week | Cost per Week ($2005) | ||||||
|---|---|---|---|---|---|---|---|
| Item | Resource Users [n (%)] | Mean±SD | Median (IQR) | Range | Mean±SD | Median (IQR) | Range |
| Pads (total) | 216 (74) | 12.2± 10.4 | 10.0 (6, 15) | 1-72 | 1.69±2.21 | 0.87 (0.44, 2.21) | 0.06-19.93 |
| Minipads | 151 (52) | 10.2±7.7 | 7.0 (5, 14) | 1-42 | 0.64±0.48 | 0.44 (0.31, 0.87) | 0.06-2.61 |
| Maxipads | 57 (19) | 8.3±7.8 | 6.0 (2, 10) | 1-36 | 1.36±1.29 | 0.99 (0.33, 1.64) | 0.16-5.91 |
| Incontinence pads | 56 (19) | 10.8±9.5 | 8.0 (6, 14) | 1-63 | 3.43±3.02 | 2.53 (1.74, 4.43) | 0.32-19.93 |
| Diapers | 14 (5) | 13.0±11.0 | 10.5 (6, 14) | 1-35 | 33.84±28.72 | 27.33 (15.62, 36.44) | 2.60-91.11 |
| Toilet paper (no. of changes) | 79 (27) | 7.1±10.2 | 3.0 (2, 6) | 1-56 | 0.12±0.17 | 0.05 (0.03, 0.10) | 0.02-0.95 |
| Paper towels (no. of sheets) | 19 (6) | 7.6±6.6 | 6.0 (2, 12) | 1-22 | 5.68±4.93 | 4.50 (1.50, 9.00) | 0.75-16.50 |
| Laundry (no. of loads) | 167 (57) | 2.4±1.8 | 2.0 (1, 3) | 1-8 | 6.09±4.37 | 5.00 (2.50, 7.50) | 2.50-20.00 |
| Dry cleaning (no. of items) | 53 (18) | 3.21±2.42 | 3.0 (1, 4) | 1-11 | 17.29±14.29 | 14.46 (4.82, 19.28) | 4.82-67.34 |
$2005, dollar value in 2005.
Values are expressed as mean ± standard deviation (SD) or median (25%, 75% interquartile range [IQR]).
Estimated mean cost for all women can be calculated by the mean cost among women with any costs multiplied by the proportion of women in this group. For example, the mean cost for pads (total) is $1.69 × 0.74 = $1.25.
The mean (± SD) and median (interquartile range) estimated weekly routine care costs for incontinence for all women were $9.47 ± 17 and $3.65 (1, 10; range $0-190). For the 262 (89%) women reporting any cost, the mean and median weekly costs were $10.59 ± 18 and $5.00 (2, 12; range $1-194). This represents an annual mean cost of $492 ± 898 for all women and $550 ± 933 for women with any cost. In univariate analysis, median (interquartile range) costs per week increased with increasing frequency ($0.62 [0, 3] for weekly to $5.00 [2, 12] for daily incontinence; P < .001) and severity ($0.37 [0, 4] for slight to $10.98 [4, 21] for very severe; P < .001) of incontinence and varied by type of incontinence ($6.57 [0, 19] for urge, $2.31 [0, 18] for stress, $3.96 [1, 8] for mixed incontinence; P < .001). The proportion of women with any incontinence-related costs also increased with increasing frequency and severity of incontinence (P < .001 for both).
In multivariable adjusted models, incontinence costs were 2.4-fold higher for African-American than for white women (P < .001) and 65% higher for women with urge (P < .001) and 47% higher for women with mixed (P = .05) compared with women with stress incontinence (Table 2). Incontinence costs also increased with severity of incontinence: women with severe and very severe incontinence had over 2-fold higher costs than did women with slight incontinence. Greater incontinence episode frequency was also associated with higher costs (results not reported). There was no association between annual household income and incontinence costs. Sensitivity analyses using Winsorized costs produced similar results and trends in costs and predictors of cost.
Table 2.
Predictors of Routine Care Costs for Incontinence in Multivariable Linear Regression
| Predictor | n | Relative Cost* | 95% CI | P† | P‡ |
|---|---|---|---|---|---|
| Age (per 10-year increase) | 262 | 1.11 | 0.99-1.25 | .07 | |
| Race | |||||
| White | 178 | Ref | <.001 | ||
| African American | 37 | 2.40 | 1.63-3.54 | <.001 | |
| Asian | 5 | 1.14 | 0.45-2.89 | .78 | |
| Latina | 32 | 1.24 | 0.79-1.96 | .35 | |
| Other | 10 | 1.63 | 0.87-3.05 | .12 | |
| Annual household income ($) | |||||
| <40,000 | 131 | Ref | .11 | ||
| 40,000-59,999 | 32 | 0.79 | 0.55-1.15 | .22 | |
| 60,000-79,999 | 33 | 0.83 | 0.58-1.20 | .33 | |
| 80,000-99,999 | 22 | 0.59 | 0.38-0.92 | .02 | |
| ≥100,000 | 31 | 0.72 | 0.49-1.05 | .09 | |
| Incontinence severity§ | |||||
| Slight | 10 | Ref | <.001 | ||
| Moderate | 151 | 1.40 | 0.76-2.58 | .28 | |
| Severe | 68 | 2.04 | 1.09-3.81 | .03 | |
| Very severe | 33 | 2.71 | 1.37-5.37 | .004 | |
| Type of incontinence∥ | |||||
| Stress | 122 | Ref | <.001 | ||
| Urge | 105 | 1.65 | 1.27-2.14 | <.001 | |
| Mixed | 35 | 1.47 | 1.00-2.14 | .05 |
CI, confidence interval; Ref, reference.
This analysis includes women with any incontinence-related cost (cost > $0; n = 262).
Relative cost is the cost ratio compared to the reference group.
P value for contrast with reference from multivariable logistic regression models.
P value for heterogeneity (race, incontinence type) or trend (income, incontinence severity, health status).
Sandvik severity score.15
Clinician diagnosis using the extended evaluation. Urge plus urge predominant incontinence combined as “urge” and stress plus stress predominant incontinence combined as “stress” incontinence.
In univariate analyses. decreased health-related quality of life assessed by the Health Utilities Index was associated with increasing incontinence episode frequency, with a 10% lower mean Health Utilities Index score among women with daily compared with weekly incontinence (0.81 ± 0.21 versus 0.90 ± 0.11, respectively; P = .02). Compared with women with stress incontinence, those with urge had about 6% lower scores on the Health Utilities Index (0.85 ± 0.18 and 0.80 ± 0.21, respectively; P = .03). We did not observe an association between health-related quality of life and incontinence severity. In multivariable analyses, adjusted health-related quality of life scores were significantly lower among older women, women with lower annual household income and those reporting good, fair, or poor versus excellent health (Table 3). There was no association with ethnicity, severity, or type of incontinence.
Table 3.
Predictors of Health Utilities Index Score in Multivariable Linear Regression
| Predictor | n | Effect Estimate* | 95% CI | P† | P‡ |
|---|---|---|---|---|---|
| Age (per 10-year increase) | 293 | -0.03 | -0.05 to -0.01 | <.001 | |
| Race | |||||
| White | 201 | Ref | .15 | ||
| African American | 38 | -0.06 | -0.13 to 0.01 | .09 | |
| Asian | 7 | -0.10 | -0.26 to 0.05 | .19 | |
| Latina | 35 | 0.04 | -0.0 to 0.12 | .31 | |
| Other | 12 | 0.04 | -0.06 to 0.14 | .45 | |
| Annual household income ($) | |||||
| <40,000 | 148 | Ref | .007 | ||
| 40,000-59,999 | 38 | 0.10 | 0.04 to 0.16 | .002 | |
| 60,000-79,999 | 36 | 0.06 | 0.00 to 0.13 | .05 | |
| 80,000-99,999 | 23 | 0.05 | -0.03 to 0.13 | .20 | |
| ≥100,000 | 34 | 0.08 | 0.02 to 0.15 | .01 | |
| Health status | |||||
| Excellent | 100 | Ref | <.001 | ||
| Good | 144 | -0.05 | -0.10 to -0.01 | .02 | |
| Fair/poor/very poor | 49 | -0.30 | 0.36 to -0.23 | <.001 | |
| Incontinence severity§ | |||||
| Slight | 16 | Ref | .64 | ||
| Moderate | 170 | 0.04 | -0.05 to 0.13 | .35 | |
| Severe | 73 | 0.06 | -0.04 to 0.15 | .22 | |
| Very severe | 34 | 0.06 | -0.05 to 0.17 | .29 | |
| Type of incontinence∥ | |||||
| Stress or mixed stress | 132 | Ref | .64 | ||
| Urge or mixed urge | 119 | -0.02 | -0.06 to 0.03 | .42 | |
| Mixed | 42 | 0.01 | -0.06 to 0.07 | .85 |
CI, confidence interval; Ref, reference.
Effect estimate is the difference in adjusted mean Health Utilities Index score compared to the reference group
P value for contrast with reference from multivariable logistic regression models.
P value for heterogeneity (race, incontinence type) or trend (income, incontinence severity, health status).
Sandvik severity score.15
Clinician diagnosis using the extended evaluation.
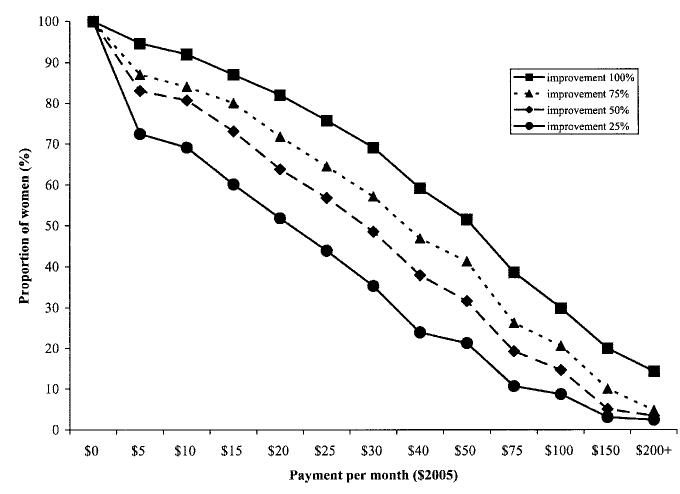
Women were willing to pay more for greater expected improvement in incontinence episode frequency, from a mean (± SD) of $28 (± 37) per month for 25% improvement to $39 (± 43) for 50% improvement, $49 (± 50) for 75% improvement, and $70 (± 64) for 100% improvement in incontinence episode frequency (P < .001 for trend; Fig. 1). The median women were willing to pay for each level of improvement in incontinence episode frequency was $20 per month for 25% improvement, $25 for 50% improvement, $30 for 75% improvement, and $50 for 100% improvement (P < .001).
Fig. 1.
Willingness to pay for improvement in incontinence. The percent of women willing to pay each dollar amount per month for varying levels of improvement in incontinence frequency is depicted. Women are willing to pay more for greater expected improvement in incontinence episode frequency, increasing from a mean of $28 per month for a 25% improvement to $70 for 100% improvement in incontinence episode frequency. Women were willing to pay more per month for increased expected improvement in incontinence episode frequency (P < .001 for trend). $2005 = value expressed in 2005 U.S. dollars.
In multivariable analyses, willingness to pay for incontinence improvement was higher with greater expected benefit (P < .001; Table 4). African-American women were willing to pay 4- to 6-fold more than white women for a similar improvement in incontinence (P < .001). Willingness to pay for complete resolution of incontinence increased with household income to over 2.3-fold more in the highest compared with the lowest income categories (P = .02 for trend). We did not observe an association with type or severity of incontinence and willingness to pay for improvement.
Table 4.
Predictors of Willingness to Pay for 50% and 100% Improvement in Incontinence in Multivariable Proportional Odds Regression
| 50% Improvement | 100% Improvement | ||||||
|---|---|---|---|---|---|---|---|
| Predictor | n | OR (95% CI) | P* | P† | OR (95% CI) | P* | P† |
| Race | |||||||
| White | 201 | Ref | <.001 | Ref | <.001 | ||
| African American | 38 | 6.47 (3.14-13.47) | .001 | 4.43 (2.1-9.22) | <.001 | ||
| Asian | 7 | 0.44 (0.08-2.48) | .34 | 0.29 (0.05-1.56) | .14 | ||
| Latina | 35 | 1.29 (0.53-3.14) | .58 | 1.34 (0.55-3.29) | .52 | ||
| Other | 12 | 0.72 (0.22-2.28) | .57 | 0.69 (0.22-2.18) | .53 | ||
| Annual household income ($) | |||||||
| < 40,000 | 148 | Ref | .19 | Ref | .02 | ||
| 40,000-59,999 | 38 | 1.01 (0.51-1.97) | .99 | 0.88 (0.45-1.71) | .70 | ||
| 60,000-79,999 | 36 | 1.38 (0.69-2.74) | .36 | 1.87 (0.96-3.64) | .06 | ||
| 80,000-99,999 | 23 | 2.32 (1.03-5.28) | .04 | 2.36 (1.04-5.43) | .04 | ||
| ≥100,000 | 34 | 1.75 (0.85-3.58) | .12 | 2.55 (1.25-5.24) | .01 | ||
| Incontinence severity‡ | |||||||
| Slight | 16 | Ref | .47 | Ref | .99 | ||
| Moderate | 170 | 0.80 (0.28-2.30) | .68 | 1.18 (0.39-3.64) | .76 | ||
| Severe | 73 | 0.63 (0.21-1.90) | .41 | 1.18 (0.37-3.77) | .78 | ||
| Very severe | 34 | 0.47 (0.13-1.64) | .24 | 1.15 (0.32-4.17) | .83 | ||
| Type of incontinence§ | |||||||
| Stress or mixed stress | 132 | Ref | .11 | Ref | .24 | ||
| Urge or mixed urge | 119 | 1.47 (0.90-2.40) | .12 | 1.36 (0.83-2.21) | .22 | ||
| Mixed | 42 | 1.95 (0.97-3.96) | .06 | 1.70 (0.86-3.39) | .13 | ||
OR, odds ratio; CI, confidence interval; Ref, reference.
P value for contrast with reference from multivariable logistic regression models.
P value for heterogeneity (race, incontinence type) or trend (income, incontinence severity, health status).
Sandvik severity score.15
Clinician diagnosis using the extended evaluation.
DISCUSSION
Urinary incontinence is a costly condition. Our findings verify the high economic and “human” costs of incontinence, including decreased health-related quality of life and physical and psychological burden, reflected by high willingness to pay for incontinence improvement. Because a majority of the annual costs of incontinence are associated with routine care, accurate and generalizable assessment of these costs is critical. We present a detailed assessment of resource use and calculate associated costs using nationally generalizable unit costs. The mean weekly incontinence cost we observed ($10) falls in the range of observations in other studies ($1 to $20).6-9 In multivariable analyses that controlled for identified potential predictors, we observed increasing costs associated with increasing frequency and severity of incontinence and urge compared with stress incontinence. This is consistent with other studies that found increased cost among women with urge versus stress incontinence.6,8,9 The mean Health Utilities Index score of community-dwelling women in our study (0.82) was consistent with Health Utilities Index scores reported among women with incontinence in population-based surveys in Canada (0.82) and Finland (0.84).10,20 For context, the mean Health Utilities Index score for women 45 years and older with no chronic medical conditions is reported as 0.92, and a difference in Health Utilities Index scores of 0.09 or greater represents severe clinical impact.10,21 The health-related quality-of-life impact of incontinence is similar to that observed with other chronic medical conditions like osteoarthritis, chronic obstructive pulmonary disease, and stroke.10 Health-related quality of life was independently associated with annual household income with a threshold effect at $40,000, where women with a greater annual income had higher Health Utilities Index scores.
Our study confirms findings of others that women with incontinence perceive substantial benefits from a reduction in the number of incontinence episodes. Women in this study were willing to pay almost $40 per month for 50% improvement to over $70 per month for cure of incontinence, similar to what women were willing to pay for incontinence improvement in other studies11-13 and what women are willing to pay for partial relief of other chronic medical conditions like migraine headaches or gastroesophageal reflux.22,23 Because willingness to pay for improvement exceeds routine care costs by 3-7 times in our study, effective incontinence treatment, not simply symptom management, may be economically beneficial as well as improve quality of life.
In multivariable analyses, African-American women had both higher routine care costs for incontinence and were willing to pay significantly more than white women for incontinence improvement. This is interesting because individuals in racial and ethnic minority groups are less likely to receive preventive, diagnostic, medical, or surgical interventions and incur lower costs for these services.24 Perhaps African-American women are less likely to seek or receive health care, resulting in increased routine care costs for incontinence symptom management. A previous study, designed to assess whether preferences for improvements in health vary among ethnic groups, found that African Americans were willing to pay significantly less than whites for improvements in osteoarthritis.25 No differences were observed across racial and ethnic groups in the values placed on nonhealth items (eg, new car, nice dinner, week’s vacation), suggesting that the differences in value placed on health are real, not due to a methodological bias. Incontinence may be perceived as a bigger burden or more socially debilitating in the African-American community, therefore resulting in greater costs to control the condition and a willingness to pay more for symptom improvement.
Our study was cross-sectional and therefore cannot document causal associations. The participants in our study were healthy, community-dwelling volunteers with at least 3 incontinence episodes per week, who were bothered enough by their incontinence to seek treatment but had not been treated for incontinence in the prior 3 months. Therefore, these results may not be generalizable to other women. Recall of resource use during a typical week rather than diary recording was used to minimize participant burden. Because individuals may over- or underreport their use of resources,26-28 systematic variance in this discrepancy may bias research findings.
In summary, urinary incontinence is associated with substantial routine care “costs.” Women with severe incontinence pay about $900 per year out-of-pocket for incontinence routine care. Incontinence is associated with a clinically significant decrement in health-related quality of life that is similar to the impact of other chronic medical conditions like osteoarthritis, chronic obstructive pulmonary disease, and stroke.10 Women are willing to pay about $900 per year for 100% improvement in incontinence, which is similar to the willingness to pay for improvement of migraine headaches and gastroesophageal reflux.22,23 Interestingly, African-American women both pay more for incontinence care and are willing to pay more for incontinence improvement, demonstrating possible racial/ethnic differences in approach to incontinence and its treatment. Because increased frequency and severity of incontinence are associated with higher routine care cost and any incontinence is associated with deceased health-related quality of life, effective incontinence treatment may decrease routine care costs and improve quality of life.
APPENDIX
Members of the Diagnostic Aspects of Incontinence Study (DAISy) Group
| Principal Investigators | Co-Principal Investigators | Institution |
|---|---|---|
| Deborah Grady, MD, MPH | Jeanette S. Brown, MD | Coordinating Center,University of California, San Francisco |
| Holly E. Richter, PhD, MD | Kathryn Burgio, PhD | University of Alabama at Birmingham |
| Patricia Goode, MD | ||
| Leslee L. Subak, MD | University of California, San Francisco | |
| Ingrid Nygaard, MD | Catherine Bradley, MD | Iowa |
| Linda Brubaker, MD | Marypat Fitzgerald, MD | Loyola, Chicago, IL |
| Kimberly Kenton, MD | ||
| Stephen Kraus, MD | Ash M. Dabbous, MD | University of Texas Health Science Center at San Antonio, TX |
| Alyane Markland, DO |
Footnotes
This study was supported by a research contract from Astellas, Inc.
These data were presented in part at the 26 Annual Scientific Meeting of the American Urogynecologic Society, Atlanta, Georgia, September 15-17, 2005.
REFERENCES
- 1.Hunskaar S, Vinsnes A. The quality of life in women with urinary incontinence as measured by the sickness impact profile. doi: 10.1111/j.1532-5415.1991.tb02903.x. [DOI] [PubMed] [Google Scholar]; J Am Geriatr Soc. J Am Geriatr Soc. 1992;1991;4039:976, 378–7. [Google Scholar]
- 2.Mittmann N, Trakas K, Risebrough N, Liu BA. Utility scores for chronic conditions in a community-dwelling population. Pharmacoeconomics. 1999;15:369–76. doi: 10.2165/00019053-199915040-00004. [DOI] [PubMed] [Google Scholar]
- 3.Wilson L, Park GE, Luc KO, Brown JS, Subak LL. Annual direct cost of urinary incontinence. Obstet Gynecol. 2001;98:398–406. doi: 10.1016/s0029-7844(01)01464-8. [DOI] [PubMed] [Google Scholar]
- 4.Varmus H. Disease-specific estimates of direct and indirect costs of illness and NIH support. Department of Health and Human Services, National Institutes of Health; Bethesda (MD): 1997. [Google Scholar]
- 5.Wagner TH, Hu TW. Economic costs of urinary incontinence in 1995. Urology. 1998;51:355–61. doi: 10.1016/s0090-4295(97)00623-7. [DOI] [PubMed] [Google Scholar]
- 6.Tediosi F, Parazzini F, Bortolotti A, Garattini L. The cost of urinary incontinence in Italian women. A cross-sectional study. Gruppo di Studio Incontinenza. Pharmacoeconomics. 2000;17:71–6. doi: 10.2165/00019053-200017010-00005. [DOI] [PubMed] [Google Scholar]
- 7.Dowell CJ, Bryant CM, Moore KH, Simons AM. Calculating the direct costs of urinary incontinence: a new test instrument. BJU Int. 1999;83:596–606. doi: 10.1046/j.1464-410x.1999.00993.x. [DOI] [PubMed] [Google Scholar]
- 8.McClish DK, Wyman JF, Sale PG, Camp J, Earle B. Use and costs of incontinence pads in female study volunteers. Continence Program for Women Research Group. J Wound Ostomy Continence Nurs. 1999;26:207, 210–8. [PubMed] [Google Scholar]
- 9.Wyman JF. The “costs” of urinary incontinence. Eur Urol. 1997;32(suppl 2):13–9. [PubMed] [Google Scholar]
- 10.Schultz SE, Kopec JA. Impact of chronic conditions. Health Rep. 2003;14:41–53. [PubMed] [Google Scholar]
- 11.Kobelt G. Economic considerations and outcome measurement in urge incontinence. Urology. 1997;50(suppl):100–10. doi: 10.1016/s0090-4295(97)00602-x. [DOI] [PubMed] [Google Scholar]
- 12.O’Conor RM, Johannesson M, Hass SL, Kobelt-Nguyen G. Urge incontinence: quality of life and patients’ valuation of symptom reduction. Pharmacoeconomics. 1998;14:531–9. doi: 10.2165/00019053-199814050-00005. [DOI] [PubMed] [Google Scholar]
- 13.Johannesson M, O’Conor RM, Kobelt-Nguyen G, Mattiasson A. Willingness to pay for reduced incontinence symptoms. Br J Urol. 1997;80:557–62. doi: 10.1046/j.1464-410x.1997.00420.x. [DOI] [PubMed] [Google Scholar]
- 14.Feeny D, Furlong W, Boyle M, Torrance GW. Multi-attribute health status classification systems. Health Utilities Index. Pharmacoeconomics. 1995;7:490–502. doi: 10.2165/00019053-199507060-00004. [DOI] [PubMed] [Google Scholar]
- 15.Sandvik H, Hunskaar S, Seim A, Hermstad R, Vanvik A, Bratt H. Validation of a severity index in female urinary incontinence and its implementation in an epidemiological survey. J Epidemiol Community Health. 1993;47:497–9. doi: 10.1136/jech.47.6.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tukey JW. Exploratory data analysis. AddisonWesley; Reading (MA): 1977. [Google Scholar]
- 17.McCullagh P, Nelder J. Generalized linear models. 2nd ed. Chapman and Hall; London (UK): 1989. [Google Scholar]
- 18.Lipsitz SH, Kim K, Zhao L. Analysis of repeated categorical data using generalized estimating equations. Stat Med. 1994;13:1149–63. doi: 10.1002/sim.4780131106. [DOI] [PubMed] [Google Scholar]
- 19.Hoenig JM, Heisey DM. The abuse of power: the pervasive fallacy of power calculations for data analysis. Am Statistician. 2001;55:19–24. [Google Scholar]
- 20.Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Ann Med. 2001;33:328–36. doi: 10.3109/07853890109002086. [DOI] [PubMed] [Google Scholar]
- 21.Drummond M. Introducing economic and quality of life measurements into clinical studies. Ann Med. 2001;33:344–9. doi: 10.3109/07853890109002088. [DOI] [PubMed] [Google Scholar]
- 22.Lenert LA. Use of willingness to pay to study values for pharmacotherapies for migraine headache. Med Care. 2003;41:299–308. doi: 10.1097/01.MLR.0000044909.63278.0D. [DOI] [PubMed] [Google Scholar]
- 23.Kleinman L, McIntosh E, Ryan M, Schmier J, Crawley J, Locke GR, 3rd, et al. Willingness to pay for complete symptom relief of gastroesophageal reflux disease. Arch Intern Med. 2002;162:1361–6. doi: 10.1001/archinte.162.12.1361. [DOI] [PubMed] [Google Scholar]
- 24.Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in the quality of care for enrollees in medicare managed care. JAMA. 2002;287:1288–94. doi: 10.1001/jama.287.10.1288. [DOI] [PubMed] [Google Scholar]
- 25.Byrne MM, O’Malley KJ, Suarez-Almazor ME. Ethnic differences in health preferences: analysis using willingness-to-pay. J Rheumatol. 2004;31:1811–8. [PubMed] [Google Scholar]
- 26.Sandvik H, Hunskaar S. The epidemiology of pad consumption among community-dwelling incontinent women. J Aging Health. 1995;7:417–26. doi: 10.1177/089826439500700305. [DOI] [PubMed] [Google Scholar]
- 27.Wallihan DB, Stump TE, Callahan CM. Accuracy of self-reported health services use and patterns of care among urban older adults. Med Care. 1999;37:662–70. doi: 10.1097/00005650-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 28.Glandon GL, Counte MA, Tancredi D. An analysis of physician utilization by elderly persons: systematic differences between self-report and archival information. J Gerontol. 1992;47:S245–52. doi: 10.1093/geronj/47.5.s245. [DOI] [PubMed] [Google Scholar]