Abstract
Objective: This study investigated the level of knowledge about schizophrenia of primary care doctors working in the city of Brescia, Italy, and variables associated with better information.
Method: The study design was devised after 2 joint meetings with leading figures of the Italian College of General Practitioners. A cross-sectional evaluation of 215 general practitioners was performed (June 2002). A random subgroup was selected to participate in a 4-month retest session in order to evaluate the reliability of the schedule (October 2002). The setting was the local health unit of Brescia, which involves 706 primary care doctors working in the city and its province. Of these, 30.5% took part in the study. A structured self-report questionnaire (SAKS) was devised for this study. General practitioners were also asked to rate videotaped cases of 5 patients with different DSM-IV diagnoses. The main outcome measures were the scores from subscales measuring knowledge of schizophrenia symptoms and signs, knowledge of antipsychotics and their adverse events, and correct diagnoses of 5 videotaped cases.
Results: Primary care doctors identified positive (79.0%), negative (72.6%) and general (72.1%) symptoms of schizophrenia (p < .001). Of the 5 cases on videotape, they correctly rated a mean of 3.1 cases. The mean percentage of anti-psychotics correctly identified was 34.1% (older) and 51.2% (novel) (p < .001). Better answers were given by doctors who knew the diagnostic criteria, had read books on psychiatry, and had attended previous courses.
Conclusion: More teaching on the diagnosis of schizophrenia and clinical psychopharmacology should be given to general practitioners.
The worldwide shift of schizophrenia patients from psychiatric hospitals into the community is now placing a heavy burden on general practitioners (GPs), who are faced not only with the management of physical comorbidities, but also with visits for psychiatric symptoms, emergencies, and counseling to patients and their families.1–8 Furthermore, general practitioners are sometimes the first and only provider of treatment for schizophrenia patients.9–13
In Italy, the closure of admissions to psychiatric hospitals in 1978 has placed a strong emphasis on community care,14 so that Italian GPs are often confronted with the management of schizophrenia patients; this calls for a greater effort to improve GPs' knowledge of schizophrenia and the use of antipsychotics.
It has been speculated15 that the goals of training courses could be either “deficit” based or “epidemiology” based. In the first instance, objectively assessed deficits in knowledge point to learning needs, while in the latter case, epidemiology could give priority to illnesses with high prevalence. Once a learning need is identified, dedicated training courses can be implemented to cover deficits in knowledge. The 2 approaches are not mutually exclusive, and, in the case of schizophrenia, both epidemiologic data about GPs' burden of care and deficits in their knowledge might guide training programs.
The aims of our study were to assess GPs' knowledge about schizophrenia in the areas of symptoms, diagnosis, drug treatment, and potentially related adverse events. Another objective was to investigate what demographic and professional variables for GPs were related to their knowledge about schizophrenia. Since no other studies of the recent literature have so far investigated these aspects, our aim was to contribute new data on what family doctors actually know about schizophrenia and whether they should have more teaching on this topic.
METHOD
Health Care Setting and General Practitioners
Practice organization within the health care system in Italy can be described, according to some parameters,16 by a capitation payment system and single-handed practices. GPs are the gatekeepers (with the exception of access to psychiatric services), most have no additional staff, and there is no competition from specialists in primary care. Visits are usually not booked by patients, who attend their GPs whenever they feel in need, and doctors make home visits when necessary. When symptoms are severe, patients may be taken directly to the emergency room of main hospitals.
The study took place in the city of Brescia, whose local health unit involves 706 GPs, working in the city or in its province. Letters were sent to all GPs in the catchment area to give details of the study design, and to ask for their participation in a teaching course devised for research purposes and the assessment of reliability data.
Admission to the main session, which took place on 15 June 2002, was limited to the first 220 participants who responded to the letter, on a first-come first-served basis. A subgroup of 100 GPs was randomly selected to rate the questionnaire again in a follow-up session 4 months later (19 October 2002), in order to assess the instrument's test-retest reliability.
During the meeting, where no formal teaching was given, GPs were asked to complete questionnaires and were shown videotapes of 5 patients with different DSM-IV diagnoses.
Questionnaire Design
Two meetings took place with leading figures (O.B., G.M.) of the Italian College of General Practitioners to discuss the content and the format of the instruments and videotapes for this research on schizophrenia knowledge.
At the end of this preliminary work, the joint committee devised 2 instruments. The first was a questionnaire collecting information on the key sociodemographic variables of the GPs, professional profile (academic learning, specialty, and general knowledge of psychiatry), and how they cope with schizophrenia patients (what treatment strategies were their first choice and to whom they would refer these patients).
The second instrument was a self-report questionnaire, the Schedule for the Assessment of Knowledge about Schizophrenia (SAKS, available from the authors by request), aimed at investigating actual knowledge. The SAKS was structured into 3 main areas: (I) clinical, (II) drug therapy, and (III) antipsychotic-related adverse events.
Section I lists a series of 61 psychiatric symptoms and signs, 27 of which are commonly found in schizophrenia and may be clustered as positive, negative, or general symptoms. These had to be correctly rated by the respondents, through a yes/no answer, and an overall score (range 0–61) was assigned that sums true positives (correctly labeled schizophrenia symptoms) and true negatives (other symptoms, correctly labeled as not pertaining to schizophrenia). In this section, questions on the duration of untreated psychosis, diagnostic criteria, substance abuse and suicide risk were also included.
Section II lists a series of 68 psychotropic drugs currently marketed in Italy, including 15 antipsychotics, 22 antidepressants, 19 benzodiazepines, 6 mood stabilizers, 4 “neurotrophics,” and 2 anticholinergics. GPs were asked to select those drugs used to treat psychotic symptoms of schizophrenia. From this section an overall score of “total antipsychotics” (true positives) was used for analysis.
Section III asks questions about some of the most common and potentially dangerous adverse events occurring during treatment with antipsychotics, namely prolactin elevation, agranulocytosis, and extrapyramidal symptoms (EPS); questions on the treatment of these conditions were also given.
The information covered by the SAKS was considered by the committee to be the minimum requirement for clinical practice. The time needed to complete the 2 questionnaires was about 1 hour.
Videotape Cases
GPs were also asked to diagnose 5 cases on videotape, each lasting 10 to 15 minutes; actors played the roles of the patient and interviewer. Four cases were modeled according to the DSM-IV-TR17 criteria for (1) major depressive disorder with psychotic features, (2) schizophrenia, recent onset, (3) borderline personality disorder with comorbid substance abuse, and (4) somatization disorder. A fifth case was added with “normal” features.
The tapes were arranged by C.T. and were then blindly rated by 2 other experienced psychiatrists (P.V. and P. Cacciani). The mean kappa coefficient for the agreement of the 2 raters on the diagnoses was 0.91.
The project group found the style of the videotape interviews congruent with GPs' standard approach to a psychiatric patient.
Statistical Analysis
The main outcome measures used in the statistical analysis were the scores from SAKS subscales measuring knowledge of schizophrenia symptoms and signs, knowledge of antipsychotics and their adverse events, and correct diagnoses of videotaped cases. Associations with continuous variables were tested with parametric statistics (Pearson r, Student t, analysis of variance); non-parametric statistics (ρ, Mann-Whitney U) were used for ordinal variables. Categorical variables were analyzed using χ2 statistics. All statistics were performed with the SPSS package.18
RESULTS
Profile of the General Practitioners
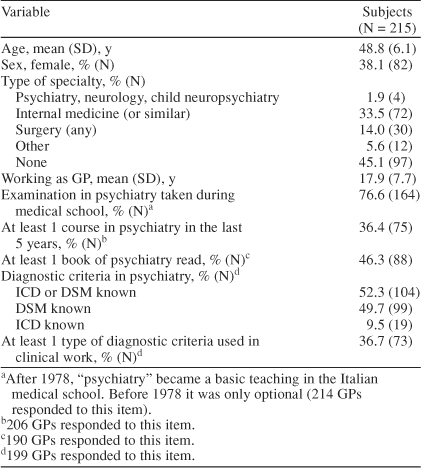
Five of the GPs did not attend, so that the final group consisted of 215 GPs (30.5% of the total number of GPs working in the community). The participants were mostly middle-aged, male, and had at least 1 medical specialty and about 18 years of experience in their practice. Only 36.4% had taken postdegree courses on psychiatry, but one half had read books on psychiatry and knew some diagnostic criteria (either DSM or ICD). These criteria were used only by 36.7% in clinical practice (Table 1).
Table 1.
Characteristics of General Practitioners (GPs) Participating in a Cross-Sectional Evaluation of Knowledge About Schizophrenia
GPs reported that they took take care of 3.7 (SD = 2.7) schizophrenia patients each, and, during the last 2 years, they reported having considered for the first time ever the diagnosis of schizophrenia in 1.0 (SD = 1.1) patient. Most (69.3%) would better manage the new schizophrenia patient by sending him/her to a psychiatrist; only 9.3% favored joint care. Pharmacotherapy was regarded by 88.0% as the best treatment for schizophrenia.
Symptoms and Signs, Course of Schizophrenia, and Videotaped Cases
Table 2 reports on the identification of schizophrenia symptoms taken from section I of the SAKS. The rate of correct identification among “positive,” “negative,” and “general” symptoms differed significantly (F = 15.5, p < .001) and post-hoc analysis showed that significance was related to contrasts of “positive” vs. “negative” (F = 14.8, p < .001) and “positive” vs. “general” (F = 27.9, p < .001).
Table 2.
Symptoms and Signs of Schizophrenia (Positive, Negative, and General) Endorsed by General Practitionersa
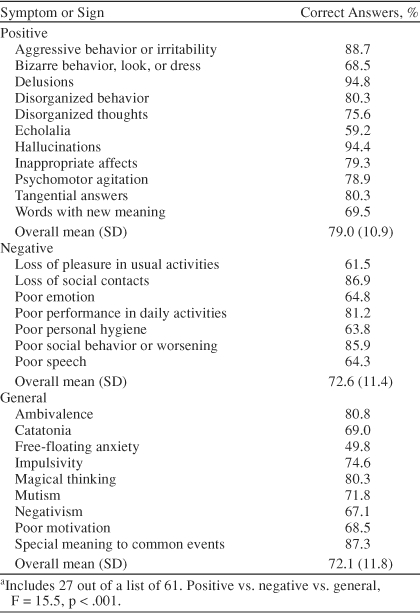
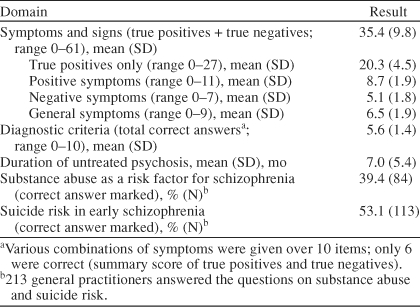
Table 3 summarizes data on symptoms and other variables drawn from the clinical section of the SAKS. The overall score of “symptoms and signs” was only in the middle range, but the performance was definitely better when only true positives (i.e., sensitivity) were considered; a mean of 20 “right” answers out of 27 was given.
Table 3.
Summary Results of Symptoms and Signs, Diagnostic Criteria, Risk Factors, and Complications of Schizophrenia
GPs gave also a correct diagnosis to a mean of 3.1 out of 5 videotaped cases. Performance was good at diagnosing major depressive disorder with psychotic features (75.0%), somatization disorder (89.4%), and the “healthy” case (92.0%), but schizophrenia was correctly diagnosed by only 46.0%; and borderline personality disorder, by 15.4% of the sample. The most frequent wrong diagnoses given to the schizophrenia case were “other psychoses” (19.0%, most often “delusional disorder”) and “personality disorder” (17.5%, with 7.4% indicating a cluster A personality disorder). A diagnosis of schizophrenia (false positive) was given by 9.5% of GPs to the major depressive disorder case, and by 14.8% to the borderline case.
For the GPs' opinion about the duration of untreated psychosis and its consequences, the mean duration of untreated psychosis was estimated to be 7.0 months. A minority (20.5%) of respondents thought that a delay in the diagnosis of schizophrenia had no influence on prognosis, while 40.5% and 34.4% judged this to moderately or severely affect prognosis, respectively. Substance abuse and suicidal thoughts were not commonly marked by our sample as risk factors for and complications of schizophrenia.
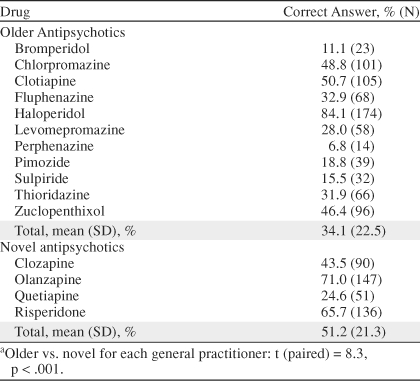
Psychotropic Drugs
Overall, a mean of 5.8 (SD = 3.0) antipsychotics were correctly identified, and a mean of 3.6 (SD = 4.9) false positives were found among all other classes. Table 4 shows the correct identification for each antipsychotic. Only 4 antipsychotics were known by more than half of GPs, with a significantly worse performance for identifying conventional antipsychotics when compared with novel drugs (34.1% vs. 51.2%, t = 8.3, p < .001).
Table 4.
General Practitioners' (N = 207) Knowledge of Antipsychotic Drugsa gc
Adverse Events and Their Treatment
Answers to section III on some common adverse events of typical and atypical antipsychotics revealed that 31.3% knew of agranulocytosis due to clozapine; 21.9%, of elevation of prolactin serum levels; and 43.5%, of EPS. On treatment of EPS, GPs gave a mean of 3.2 correct answers out of a list of 8.
The Test-Retest Reliability of the SAKS
Eighty-two of the 100 sampled GPs rated the questionnaire again after 4 months, in order to test the stability of the SAKS over time. The correlation values were high and significant for all the main outcome measures (symptoms and signs, r = 0.61, p = .001; total antipsychotics, r = 0.66, p = .001; conventional antipsychotics, r = 0.71, p = .001; novel antipsychotics, ρ = 0.64, p = .001; diagnostic criteria, ρ = 0.40, p = .001; treatment of EPS, ρ = 0.35, p = .002; agranulocytosis, Cohen κ = 0.35, p = .002; EPS, κ = 0.49, p = .001; prolactin serum elevation, κ = 0.37, p = .001).
Variables Associated With GPs' Knowledge
The various measures of GPs' knowledge were tested for association with the main sociodemographic and educational variables (age, sex, years of practice, specialization, courses, books read, knowledge, and use of diagnostic criteria in clinical practice). Table 5 lists most of the significant associations found in our sample, with details of scores and significance level.
Table 5.
General Practitioners' Knowledge and Associated Variables
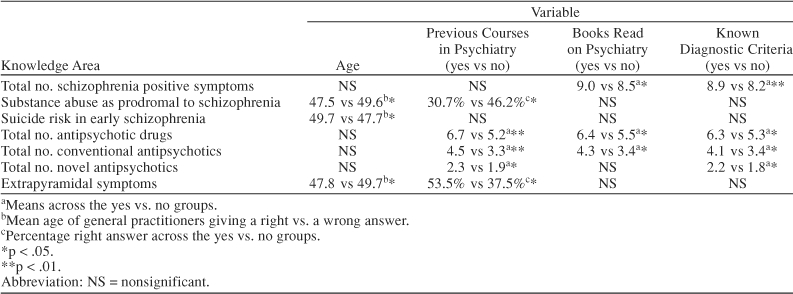
Age gave some conflicting results; better answers were given by younger doctors on EPS and drug abuse, while older doctors knew more about suicide risk in schizophrenia.
Better answers to the questionnaire were given by practitioners who had previously attended psychiatric courses, had read books on psychiatry, and knew of diagnostic criteria.
DISCUSSION
This study investigated basic knowledge about schizophrenia in a large group of GPs, using an ad hoc schedule that has proved reliable in its main components. This is the first study on GPs that addresses the issue of information about symptoms and diagnosis of schizophrenia, treatment, and adverse events.
The performance of the GPs in identifying true symptoms of schizophrenia was rather good and even better with positive symptoms. Current diagnostic standards in psychiatry, such as DSM-IV-TR17 and ICD-10,19 stress the positive symptoms in the diagnostic criteria for schizophrenia. However, our GPs did not perform very well when they had to diagnose videotaped cases. Performance was also disappointing in the overall score of symptoms and signs (a mean of 35 correct items out of 61), due to false positives among nonschizophrenia symptoms, so that a trend for our GPs to be overinclusive was definitely present.
Our study also shows a poor knowledge of clinical psychopharmacology by GPs, although the 3 more commonly prescribed drugs, haloperidol, olanzapine, and risperidone, were well known. In this domain, poor sensitivity in identifying antipsychotics was balanced by a valuable specificity, since the number of other drugs wrongly labeled as antipsychotics was very low. Not surprisingly, the main side effects of psychotropic drugs were also poorly known, with rates ranging from 22% to 44%.
Analyses of associations showed that having attended previous courses, knowing diagnostic criteria, and having read books on psychiatry were the variables most often related to a better performance.
Among the limits of our study, it must be reported that the sample, although large, may not be representative of the population of Italian GPs. The doctors included had chosen to participate in a rather complex educational course on psychiatry. In addition, Brescia is a largely industrial city in the north of Italy, where psychiatric services are well developed in the community, and GPs probably have facilitated access to consultation with psychiatrists. It must be noted that 63.6% of the participants had never attended a psychiatric course before, so that selection of a group with an unusually high interest in psychiatry seems unlikely.
Practice organization in primary care varies in different European countries. A capitation payment system and single-handed practices, most with no additional staff, are features common to other European countries.16 Italian GPs do not function as “gatekeepers” for psychiatry; direct access to psychiatric services is possible.
Finally, the schedule did not investigate other adverse events of novel antipsychotics, such as diabetes.20 However, this is a much debated issue,21 and in Italy GPs can prescribe novel antipsychotics only after a care plan has been written by a psychiatrist of the mental health services.
Our sample would seem to be comparable, in the number of treated schizophrenia patients (3.7), with those of others studies in the recent literature, such as the Australian study of Lewin and Carr,9 where general practitioners reported a mean number of “about 3” treated patients. Similarly, in the Canadian study of Toews et al.,4 53.5% of family physicians indicated that they saw 1 to 2 patients with schizophrenia each month.
As far as learning needs are concerned, to our knowledge, the only study in the recent literature that is roughly comparable to ours is that of Toews et al.4, who assessed learning needs about schizophrenia in Canadian GPs. However, this was a mailing survey, with a brief self-report questionnaire and no reliability data, and it reported that knowledge of psychopharmacologic agents and monitoring and adjusting medications were the areas in which improvement of knowledge was most needed. This estimate was based on the areas in which GPs would like to improve their knowledge, not an assessment of the real status of knowledge in this domain.
In summary, the key learning needs determined by our study were about the specificity of schizophrenia symptoms and the knowledge of both older and novel antipsychotics and their adverse events. The exposure to videotapes has also shown that more teaching should be given both on schizophrenia and severe personality disorders, which in some cases may share common features and make diagnosis difficult.
Having assessed learning needs is just the first step in improving the management of schizophrenia in primary care. Teaching tailored to these specific needs must indeed prove effective in changing diagnostic skills, prescription of psychotropics, and referrals to psychiatric services when appropriate, and this must be tested by further research.
Drug names: chlorpromazine (Thorazine, Sonazine, and others), clozapine (Clozaril, FazaClo, and others), fluphenazine (Prolixin and others), haloperidol (Haldol and others), olanzapine (Zyprexa), pimozide (Orap), quetiapine (Seroquel), risperidone (Risperdal).
Footnotes
This study was supported with a grant (Project 153) from the Health Authority of the Lombardia Region, Italy.
Dr. Sacchetti has served as a consultant to and on the speakers or advisory boards for and has received grant/research support and honoraria from Abbott, AstraZeneca, Bristol-Myers Squibb, Eli Lilly, GlaxoSmithKline, InnovaFarma, Pfizer, Janssen, and Wyeth. Drs. Turrina, Valsecchi, Bonomi, Corsini, Cacciani, Brignoli, and Medea report no other significant commercial relationships relevant to the study.
REFERENCES
- King MB. Management of patients with schizophrenia in general practice [editorial] Br J Gen Pract. 1992;42:310–311. [PMC free article] [PubMed] [Google Scholar]
- Nazareth ID, King MB. Controlled evaluation of management of schizophrenia in one general practice: a pilot study. Fam Pract. 1992;9:171–172. doi: 10.1093/fampra/9.2.171. [DOI] [PubMed] [Google Scholar]
- Nazareth I, King M, and Haines A. et al. Care of schizophrenia in general practice. BMJ. 1993 307:910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toews J, Lockyer J, and Addington D. et al. Improving the management of patients with schizophrenia in primary care: assessing learning needs a first step. Can J Psychiatry. 1996 41:617–622. [DOI] [PubMed] [Google Scholar]
- Lang FH, Johnstone EC, Murray GD. Service provision for people with schizophrenia, 2: role of the general practitioner. Br J Psychiatry. 1997;171:165–168. doi: 10.1192/bjp.171.2.165. [DOI] [PubMed] [Google Scholar]
- Carr VJ, Lewin TJ, and Barnard RE. et al. Attitudes and roles of general practitioners in the treatment of schizophrenia compared with community mental health staff and patients. Soc Psychiatry Psychiatr Epidemiol. 2004 39:78–84. [DOI] [PubMed] [Google Scholar]
- Falloon IR. General practice recruitment for people at risk of schizophrenia: the Buckingham experience. Aust N Z J Psychiatry. 2000;34:S131–S136. doi: 10.1080/000486700233. [DOI] [PubMed] [Google Scholar]
- Daumit L, Pratt LA, and Crum RM. et al. Characteristics of primary care visits for individuals with severe mental illness in a national sample. Gen Hosp Psychiatry. 2002 24:391–395. [DOI] [PubMed] [Google Scholar]
- Lewin TJ, Carr VJ. Rates of treatment of schizophrenia by general practitioners: a pilot study. Med J Aust. 1998;168:166–169. doi: 10.5694/j.1326-5377.1998.tb126771.x. [DOI] [PubMed] [Google Scholar]
- Carr VJ, Lewin TJ, and Barnard RE. et al. Comparisons between schizophrenia patients recruited from Australia general practices and public mental health services. Acta Psychiatr Scand. 2002 105:346–355. [DOI] [PubMed] [Google Scholar]
- Carr VJ, Johnston PJ, and Lewin TJ. et al. Patterns of service use among persons with schizophrenia and other psychotic disorders. Psychiatr Serv. 2003 54:226–235. [DOI] [PubMed] [Google Scholar]
- Loughland CM, Carr VJ, and Lewin TJ. et al. Potential sampling and recruitment source impacts in schizophrenia research. Psychiatry Res. 2004 125:117–127. [DOI] [PubMed] [Google Scholar]
- Phelan M, Mirza I. The needs of patients receiving depot antipsychotic medication within primary care. Fam Pract. 2003;20:126–128. doi: 10.1093/fampra/20.2.126. [DOI] [PubMed] [Google Scholar]
- Mosher LR. Italy's revolutionary mental health law: an assessment. Am J Psychiatry. 1982;139:199–203. doi: 10.1176/ajp.139.2.199. [DOI] [PubMed] [Google Scholar]
- Hodges B, Inch C, Silver I. Improving the psychiatric knowledge, skills, and attitudes of primary care physicians, 1950–2000: a review. Am J Psychiatry. 2001;158:1579–1586. doi: 10.1176/appi.ajp.158.10.1579. [DOI] [PubMed] [Google Scholar]
- Engels Y, Campbell S, and Dautzemberg M. et al. Developing a framework of, and quality indicators for, general practice management in Europe. Fam Pract. 2005 22:215–222. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistic Manual of Mental Disorders, Fourth Edition, Text Revision. Washington D.C.: American Psychiatric Association. 1994 [Google Scholar]
- SPSS Inc. SPSS Base 10.0 Applications Guide. Chicago, Ill: SPSS Inc. 1999 [Google Scholar]
- World Health Organisation. The ICD-10 classification of mental and behavioural disorder: diagnostic criteria for research. Geneva: World Health Organisation. 1993 [Google Scholar]
- Sacchetti E, Turrina C, and Parrinello G. et al. Incidence of diabetes in a general practice population: a database cohort study on the relationship with haloperidol, olanzapine, risperidone or quetiapine exposure. Int Clin Psychopharmacol. 2005 20:33–37. [DOI] [PubMed] [Google Scholar]
- American Diabetes Association, American Psychiatric Association, American Association Of Clinical Endocrinologists. et al. Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care. 2004 27:596–601. [DOI] [PubMed] [Google Scholar]


