It has long been known that certain cardiovascular and metabolic risk factors tend to cluster together. For example, in the 1940s the French clinician, Vague, described the diabetic and atherogenic risk associated with android (upper body) obesity.
The relatively recent concept of a metabolic syndrome suggested that the clustering represents a discrete entity due to a single underlying aetiology (insulin resistance). Yet, despite several definitions and its own International Classification of Diseases code its validity and utility remains unclear.
The evidence does not fully support the existence of a single underlying aetiology, and most, but not all, evidence suggests that the syndrome as currently defined appears to have little value in predicting cardiovascular disease risk over other approaches that consider individual risk factors. At present there is no specific treatment for the syndrome other than targeting the individual risk factors.
It is concluded that at this time its main utility is as a reminder to the clinician that certain risk factors tend to cluster, and as an indicator of the public health importance of the risk factor clustering associated with obesity and physical inactivity.
INTRODUCTION
The metabolic syndrome (sometimes also known as syndrome X or insulin resistance syndrome) has been recognized since the late 1980s, arguably long before, and at the time of writing, there are at least five published definitions of it. Most recently the International Diabetes Federation has proposed ‘... a new worldwide definition’.1 Prospective data evaluating its prognostic importance for the development of both diabetes and cardiovascular disease have shown that it identifies high risk individuals.2,3 The metabolic syndrome even has its own ICD (International Classification of Diseases) code. Yet the apparent consensus on the existence and importance of the syndrome belies the considerable debate and uncertainty that remains.4-6 Questions remain on the underlying pathogenesis of the syndrome:
what components should be included within in?
what are the cut points for those components?
to what extent these should differ between men and women and across different ethnic groups?
whether taking the components together as a syndrome provides greater predictive value for cardiovascular disease and diabetes than considering them separately?
ultimately most importantly, what is the utility of the syndrome, for both clinical practice and public health?
The aim of this paper is to provide a critical overview of the concept of the metabolic syndrome, and in particular to reach a conclusion, based on current evidence, on its clinical and public health utility.
METHODS
The paper starts by tracing some of the origins of the concept of the metabolic syndrome, as these are informative for today's debate. It then provides a description of some of the definitions of the syndrome, and reviews some of the analyses that have addressed the issue of clustering of proposed components of the syndrome. Finally, studies that have investigated the prognostic implications of some of the definitions are discussed, before attempting to reach a conclusion on the current utility of the concept of the syndrome. The article is based on a detailed Medline review that aimed to identify all articles concerned with the clustering of cardiovascular disease risk factors between 1966 and 2004, with other articles identified from the references of those reviewed. This literature search was updated to June 2005. In addition, the author also benefited from being part of the International Diabetes Federation (IDF) meeting in 2004 that reviewed the evidence on which the recent IDF definition is based.1
ORIGINS OF THE CONCEPT OF THE METABOLIC SYNDROME
Most authors on the metabolic syndrome relate their work to description by Reaven in 1988 of syndrome X or ‘the insulin resistance syndrome’.7 However, the roots of the concept run deeper and broader than what is covered in this description, and can be seen as the culmination of several strands of observational and experimental work over the second half of the last century. The common thread to this work was the observation that certain metabolic and biological characteristics, associated with an increased risk of diabetes and atherosclerotic disease, tend to cluster (occur together greater than predicted by chance) within individuals.
Broadly, two lines of work can be identified: one based on the epidemiological studies established to identify risk factors for cardiovascular disease; and the other based on clinical and experimental studies concerning the pathogenesis of diabetes and atherosclerosis.
Epidemiological studies
The early epidemiological studies established to identify risk factors for cardiovascular disease initially described the importance of risk factor concurrence. For example, the first major publication from the Framingham study based on 6 years follow up (in which the term ‘risk factor’ was coined) identified raised blood pressure, raised serum cholesterol and electrocardiograph evidence of left ventricular hypertrophy as risk factors.8 It also demonstrated that the concurrence of these risk factors tended to increase risk in a multiplicative rather than an additive fashion. The multiplicative nature of concurrent cardiovascular disease risk factors was subsequently described in many other studies and is now considered established fact.9-11
Explicit recognition and analysis of cardiovascular disease risk factor clustering, the concurrence of risk factors in individuals greater than predicted by chance (based on their prevalence in the underlying population), in published epidemiological studies is not found until the 1970s. Descriptions included the clustering of socio-economic, lifestyle (such as smoking and aspects of diet) and biological factors,12-14 as well as the clustering of biological factors alone, such as glucose, lipids, blood pressure and anthropometry.15,16 It was noted that these clusters of risk factors predispose individuals to the development of both diabetes and cardiovascular disease, and, based largely on epidemiological evidence, Jarrett proposed that ‘... atherosclerosis and diabetes share a number of antecedents, the balance between them determining the clinical outcome’.17
Clinical studies
Of the early clinical and experimental work it is that of Vague, initially published in the late 1940s and 1950s, that is most clearly the forerunner of today's concept of the metabolic syndrome.18 His work built on observations made several decades earlier.19-21 Vague et al. described the strong relationship between android (upper body) fat distribution and adult onset (type 2) diabetes, atherosclerosis and gout. In contrast to android obesity, they concluded that although gynoid (predominantly lower body) obesity is associated with mechanical complications it ‘... does not exercise any influence on the metabolic disorders, such as diabetes, gout... and atherosclerosis’. One of the potential mechanisms discussed by Vague was that android obesity is associated with an absolute or relative over activity of the hypothalamic pituitary adrenal axis, one of the effects of which is to oppose the peripheral action of insulin.
Recognition of the potential pathophysiological importance of insulin resistance can be traced to Himsworth in the 1930s. He first recognized its potential importance in the pathogenesis of diabetes.22 Thirty to forty years later Reaven et al. confirmed the insulin resistant nature of clinical non-insulin dependent or maturity onset diabetes (i.e. type 2) and lesser forms of glucose intolerance.23-25 Reaven's group also described the fact that insulin resistance, and associated hyperinsulinaemia, is common in individuals with normal glucose tolerance.7 This observation led directly to a consideration of whether despite normal or at least non-diabetic glucose levels insulin resistance is related to other adverse consequences, and consideration of this question to the formulation of syndrome X or the insulin resistance syndrome.7
DEFINITIONS AND DESCRIPTIONS OF THE METABOLIC SYNDROME
Reaven's original description of ‘syndrome X’
In the 1988 Banting Lecture, Reaven used the term syndrome X to refer to the tendency of glucose intolerance, hypertension, low high density lipoprotein (HDL) cholesterol and raised triglycerides, and hyperinsulinaemia to occur in the same individual7 (Table 1). He proposed that the common feature of the syndrome is insulin resistance and that ‘... all other changes are likely to be secondary to this basic abnormality’. Neither obesity nor abdominal obesity was included in Reaven's original description, although secondary sources often state that they were included. However, Reaven did suggest that avoiding obesity and remaining physically active were measures that would protect against insulin resistance.
Table 1.
| Reaven 1988 | WHO 1999 | NCEP 2001 | IDF 2005 |
|---|---|---|---|
| Components of the syndrome | |||
| Resistance to insulin-stimulated glucose uptake | Insulin resistance (highest quartile for background population) | ||
| Hyperinsulinaemia Glucose intolerance | Impaired glucose regulation or diabetes (WHO 1999 definitions) | Fasting plasma glucose ≥ 6.1 mmo/LI−1 or diagnosed diabetes* | Fasting plasma glucose ≥ 5.6 mmol/L−1 or diagnosed diabetes |
| Central obesity: waist to hip ratio > 0.9 in men, > 0.85 in women, and or BMI > 30 kgm−2 | Abdominal obesity: waist circumference > 102 cm in men; > 88 in women | Abdominal obesity: ethnic group specific cut points | |
| Increased-very-low density lipoprotein triglyceride | Raised plasma triglycerides: ≥ 1.7 mmol/L−1 and/or low HDL cholesterol: < 0.9 mmol−1 in men; < 1 mmol/L−1 in women | Raised serum triglycerides: ≥ 1.7 mmol/L−1 | Raised serum triglycerides: ≥ 1.7 mmol/L−1 |
| Decreased high-density lipoprotein cholesterol | Low HDL cholesterol: < 1.0 mmol/L−1 (40 mg/dL−1) in men; < 1.3 mmolL−1 (50 mg/dL−1) in women | Low HDL cholesterol: < 1.0 mmol/L−1 (40 mg/dL−1) in men; < 1.3 mmolL−1 (50 mg/dL−1) in women | |
| Hypertension | Raised arterial pressure (≥ 140/90 mmHg) | Blood pressure ≥ 130/85 or diagnosed and treated hypertension* | Blood pressure ≥ 130/85 diagnosed and treated hypertension |
| Microalbuminuria (urinary albumin excretion rate ≥ 20 μg min−1 or albumin/creatinine ratio ≥ 30 mg g−1) | |||
| Definition of the syndrome | |||
| Criteria for the definition of ‘syndrome X’ not given. Common feature is insulin resistance, but not all five of its consequences need be present in the same individual | Glucose intolerance and/or insulin resistance plus at least two of the other features | Presence of three or more of the components | Presence of central obesity plus at least two other components |
In fact the NCEP definition does not explicitly state how diagnosed diabetes or hypertension should be treated but in practice they are included within the definition
Europids: men ≥ 94cm, women ≥ 80cm; South Asian and Chinese: ≥ 90cm, ≥ 80cm; Japanese: ≥ 85cm, ≥ 90cm; sub Saharan African, eastern Mediterranean and middle east origin populations: Europid values until specific data available; ethnic central and south Americans: South Asian values until specific data are available
WHO, World Health Organization; NCEP, National Cholesterol Education Program; IDF, International Diabetes Federation; BMI, body mass index; HDL, high density lipoprotein
Recent descriptions and definitions
The term syndrome X failed to gain widespread acceptance. ‘Insulin resistance syndrome’ is still used, but suggests a single underlying mechanism. The term ‘the metabolic syndrome’ is more neutral, and used to indicate the tendency of certain risk factors to cluster without tying it to a single underlying mechanism. It is now the most widely used.
Until earlier this year there were two widely used definitions of the metabolic syndrome: that of the World Health Organization26 and that of the National Cholesterol Education Program, Adult Treatment Panel III.27 The components of each definition and criteria for making the diagnosis of the metabolic syndrome are summarized in Table 1. In addition, definitions were proposed by the European Group for the Study of Insulin Resistance28 and the American Association of Clinical Endocrinologists.29 Essentially, these are modifications of the WHO and NCEP definitions, respectively.
Recently the International Diabetes Federation has proposed a new definition (see Table 1) that it hopes will become the international standard.1 This definition is similar to the NCEP definition, being based on relatively simple measures, applicable in a clinical or epidemiological setting, but differs in three important respects. Central obesity, as determined by waist circumference, is mandatory, and different waist cut points for different ethnic groups are given based on available data linking waist circumference to other components of the syndrome. Finally, the IDF definition uses a lower fasting glucose level than the original NCEP definition, using the American Diabetes Association 2003 cut point for impaired fasting glucose.30
The prevalence of the metabolic syndrome
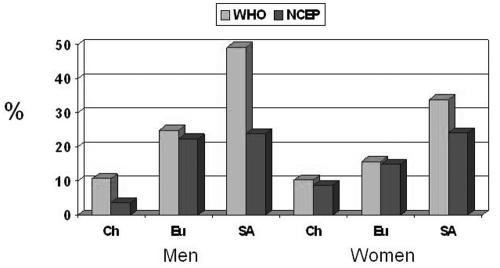
The metabolic syndrome by any of the definitions so far examined is very common in adults in many parts of the world, typically being found from one in six to one in three adults (sometimes more), rising with age and being higher in men than women.31 Figure 1 shows the prevalence in adults (25-64 years) from three ethnic groups resident in Newcastle upon Tyne, UK,32 with differences between the ethnic groups mainly reflecting differences in the prevalence of diabetes and obesity. Although common by both definitions, agreement between the definitions is not particularly good. Thus, even in the Europeans (see Figure 1) where the overall NCEP and WHO prevalence was similar, between 20-30% of individuals categorized as having the syndrome on one definition were not classified as metabolic syndrome on the other. Studies reporting agreement between the new IDF definition and others are awaited.
Figure 1.
Prevalence of the metabolic syndrome as defined by the World Health Organization (WHO) and National Cholesterol Education Program (NCEP) in adults (25 to 64 years) of Chinese (Ch), European (Eu), and South Asian (SA) origin, in Newcastle, UK
Proposed additional components of the metabolic syndrome
The definitions of the metabolic syndrome in Table 1 are based on what are considered its core components; but several other putative components have been suggested. These include hyperuricaemia,26 prothrombotic factors such as raised plasminogen activating inhibitor-1 and fibrinogen,27 and proinflammatory factors such as C-reactive protein.27 The IDF statement recommended that such potential components should be the subject of future research, in particular on their ability to add to the ability to predict cardiovascular disease and diabetes.1
Multivariate analyses of risk factor clustering—one or more clusters?
Multivariate methods of analysis have been widely used to investigate the clustering of defined and suggested components of the metabolic syndrome. The most widely used technique has been factor analysis, although its value is not without controversy and its interpretation often subjective. Nonetheless, it can provide some insight into the underlying relationships between a set of interrelated variables. A basic assumption of factor analysis is that it is possible to explain the correlation between two or more variables by a common underlying, but unmeasured, factor. It has been argued, for example, that if the proposed components of metabolic syndrome tend to cluster because of a single underlying cause, such as insulin resistance, they should all group into one factor. In the vast majority of populations studied using factor analysis (there are over 20 published studies) more than one factor has been extracted. At a broad level the components of the factors were similar, with for example, blood pressure and lipids in separate factors. Figure 2 illustrates this by summarizing the results from two of the earliest studies to apply factor analysis to the metabolic syndrome.33,34 Both studies found three, to some extent overlapping, factors. One interpretation of the factors is that they represent underlying physiological domains. The names given to each of the factors in Figure 2 are those given by the authors and reflect this interpretation. Overall the results of the factor analyses are against the unity hypothesis that a single underlying determinant (such as insulin resistance) is responsible for the clustering.4 The results suggest that more than one, possibly several, determinants contribute to the interrelationships of glucose, insulin, lipids, blood pressure and other related variables.
Figure 2.
Graphical representation of the results of factor analysis on the putative components of the metabolic syndrome from Edwards 1994 (Ref. 33) (on left) and Meigs 1997 (Ref. 34) (on right). Fast, fasting; ins, insulin; gluc, glucose; WHR, waist to hip ratio; BMI, body mass index; tgs, triglycerides; Hdl, Hdl cholessterol; Ldl-ppd, Ldl cholesterol peak particle diameter; sBP/dBP, systolic/diastolic blood pressure; neg, negative correlation between the variable and the factor
METABOLIC SYNDROME AND FUTURE DISEASE RISK
The current definitions of the metabolic syndrome are somewhat disjunctive, in the sense that it is possible for two individuals to be labelled as having the syndrome but to have different risk factor profiles. In the case of the NCEP definition two individuals labelled as having the metabolic syndrome need share only one of the five features in common (see Table 1). In the case of the WHO definition it is possible (although unlikely) that two individuals could have none of the different components in common. Thus, within these definitions there is considerable scope for heterogeneity and it is highly likely this will be associated with heterogeneity in the prognostic implications of the diagnostic label of metabolic syndrome. Certainly, applying the definitions to populations with different prevalences and patterns of the components of metabolic syndrome, such as is often the case between different populations, whether defined geographically or by ethnic group, is likely to result in different phenotypes.32
The weight of evidence strongly suggests that individuals with the metabolic syndrome (WHO or NCEP definitions, publications on the IDF definition are awaited) have a much higher risk for cardiovascular disease and diabetes than individuals without the syndrome. This is hardly surprising given that the components of the syndrome are well known risk factors. The estimates of the increased risk vary from 30-400%,5 probably mainly representing differences in the underlying populations studied and the length of follow up. In such studies it has been found that excess risk remains after adjustment for other conventional cardiovascular risk factors.5
Of importance to the clinical value of the metabolic syndrome is whether it provides more predictive information than considering its components individually, i.e. is it greater than the sum of its parts? Five studies that address this issue were recently reviewed,5 and none found that considering the components together (as a syndrome) had any greater predictive value than considering them separately. However, one recent study has suggested that the syndrome does provide predictive power for cardiovascular disease (CVD) events even after adjusting for its individual components.35
Also relevant to its clinical value is whether it provides a better alternative to other approaches to predicting CVD risk, such as those based on the Framingham risk equation and made widely available for use in clinical practice. Studies addressing this issue are limited and somewhat inconsistent in their findings, but overall suggest that the metabolic syndrome performs no better or worse than the Framingham risk equation. For example, in the San Antonio Heart Study, using data on subjects free of diabetes and CVD at baseline and followed for 7-8 years, the Framingham risk equation had a higher sensitivity for predicting cardiovascular disease events than the presence of the syndrome, and adding metabolic syndrome did not improve the prediction of events.36 Similar comparisons with alternative risk prediction scores, such as the European version (SCORE)37 would be worthwhile.
Finally, comparison to the Framingham, or other risk equations, highlights another potential shortcoming of the metabolic syndrome in any of its current definitions. In the Framingham and European equations different risk factors are given different weights - some contribute more to risk than others. In the metabolic syndrome each component is weighted equally.
CONCLUSIONS—SYNDROME OR TENDENCY, AND IS IT USEFUL?
The concept of the metabolic syndrome grew out of the recognition that certain risk factors tend to cluster together greater than predicted by chance. The clearest forerunner of the concept, particularly as recently defined by the IDF, is the description by Vague of diabetic and atherogenic risk associated with android obesity.18 The attempt to link the syndrome to a single underlying aetiology—insulin resistance—has in large part failed. The model of single cluster linked together by a single underlying mechanism (insulin resistance) does not match the empirical data. This is not to deny, of course, that insulin resistance is often associated with many of the proposed components of the syndrome. Thus current evidence does not support the use of the term ‘syndrome’ in the sense of a distinct clinical entity with a single underlying pathology. However, it may be justified in the way it is often used in epidemiology;38 and that is to indicate the more frequent coexistence of certain characteristics, in this case cardiovascular and metabolic risk factors, than would be expected by chance. More work is needed to fully understand the physiological basis of the tendency for certain risk factors to occur together.
The available studies do not suggest that the metabolic syndrome provides greater predictive value for cardiovascular disease than the sum of its parts, or that it performs better than other approaches to its risk prediction. In addition, it is worth noting that, at the time of writing, there are no specific interventions for the syndrome. Treatment of the syndrome entails treating the individual components, along with the type of lifestyle advice (healthy diet and regular physical activity) that is common to the prevention of many non-communicable diseases.
Given all of the above, does the concept of the metabolic syndrome as currently defined and understood have any utility, whether in clinical or public health terms? Perhaps its main value in clinical terms is to remind the practitioner that certain risk factors tend to cluster within individuals. Its main value in public health terms is to highlight the clustering of risk factors associated with obesity, particularly abdominal obesity, and physical inactivity. The prevalence of the metabolic syndrome within a population may provide a simple summary measure of the level of cardiovascular disease risk related to obesity and physical inactivity that can be used to compare different populations and to track changes over time. What the best definition of the syndrome would be to be used in this way requires further evaluation.
Competing interests None declared.
References
- 1.Alberti KGMM, Zimmet P, Shaw J. The metabolic syndrome: a new worldwide definition. Lancet 2005. ;366:1059 -62 [DOI] [PubMed] [Google Scholar]
- 2.Laaksonen D, Lakka H, Niskanen L, Kaplan G, Salonen J, Lakka T. Metabolic syndrome and the development of diabetes mellitus: application and validation of recently suggested definitions of the metabolic syndrome in a prospective cohort study. Am J Epidemiol 2002. ;156:1070 -7 [DOI] [PubMed] [Google Scholar]
- 3.Lakka HM, Laaksonen DE, Lakka TA, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2002. :288:2709 -16 [DOI] [PubMed] [Google Scholar]
- 4.Meigs J. Invited commentary: Insulin Resistance Syndrome? Syndrome X? Multiple Metabolic Syndrome? A syndrome at all? Factor analysis reveals patterns in the fabric of correlated metabolic risk factors. Am J Epidemiol 2000;152:908 -11 [DOI] [PubMed] [Google Scholar]
- 5.Kahn R, Buse J, Ferrannini E, Stern M. The metabolic syndrome: time for a critical appraisal. Joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2005. ;28:2289 -304 [DOI] [PubMed] [Google Scholar]
- 6.Hanson R, Imperatore G, Bennett P, Knowler W. Components of the “metabolic syndrome” and incidence of type 2 diabetes. Diabetes 2002. ;51:3120 -7 [DOI] [PubMed] [Google Scholar]
- 7.Reaven G. Role of insulin resistance in human disease. Diabetes 1988. ;37:1595 -607 [DOI] [PubMed] [Google Scholar]
- 8.Kannel WB, Dawber TR, Kagan A, Revotskie N, Stokes J. Factors of risk in the development of coronary heart disease-six-year follow-up experience. The Framingham Study. Ann Internal Med 1961. ;55:33 -50 [DOI] [PubMed] [Google Scholar]
- 9.Tyroler HA. Coronary heart disease epidemiology in the 21st century. Epidem Rev 2000. ;22:7 -13 [DOI] [PubMed] [Google Scholar]
- 10.Meigs JB, D'Agostino RD Snr, Wilson PW, Cupples LA, Nathan DM, Singer DE. Risk variable clustering in the insulin-resistance syndrome. The Framington Offspring Study. Diabetes 1997. ;46:1594 -600 [DOI] [PubMed] [Google Scholar]
- 11.Braunwald E. Shattuck lecture—cardiovascular medicine at the turn of the millennium: triumphs, concerns, and opportunities. N Engl J Med 1997;337:1360 -9 [DOI] [PubMed] [Google Scholar]
- 12.Criqui MH, Barrett-Connor E, Holdbrook MJ, Austin M, Turner JD. Clustering of cardiovascular disease risk factors. Preventive Med 1980;9:525 -33 [DOI] [PubMed] [Google Scholar]
- 13.Hjermann I, Helgeland A, Holme I, Lung-Larsen G, Leren P. The intercorrelation of serum cholesterol, cigarette smoking and body weight. The Oslo Study. Acta Med Scand 1976. ;200:479 -85 [PubMed] [Google Scholar]
- 14.Salonen JT, Puska P, Kottke TE, Heinonen OP. Coronary risk factor clustering patterns in eastern Finland. Int J Epidemiol 1981;10:203 -10 [DOI] [PubMed] [Google Scholar]
- 15.Ostrander L, Lamphiear D. Coronary risk factors in a community. Findings in Tecumseh Michigan. Circulation 1976. ;53:152 -6 [DOI] [PubMed] [Google Scholar]
- 16.Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR. Diabetes, blood lipids, and the role of obesity in coronary heart disease risk for women. The Framingham study. Ann Internal Med 1977. ;87:393 -7 [DOI] [PubMed] [Google Scholar]
- 17.Jarrett RJ. Type 2 (non-insulin-dependent) diabetes mellitus and coronary heart disease-chicken, egg or neither? Diabetologia 1984. ;26:99 -102 [DOI] [PubMed] [Google Scholar]
- 18.Vague J. The degree of masculine differentiation of obesities: a factor determining predisposition to diabetes, atherosclerosis, gout and uric calculus disease. Am J Clin Nutrition 1956. ;4:20 -34 [DOI] [PubMed] [Google Scholar]
- 19.Richer P. Nouvelle Anatomie Artistique Du Corps Humain. I. Cour Practique. Elements D'anatomie. L'homme. II. Cours Superieur. Morphologie. La Femme: Plon Edit, 1920
- 20.Kading H. Alter und Fettpolsterdicke als alleininger Maastab fur den Ernahrungszustand. Munchen Med Wchnschr 1922. ;69:433 [Google Scholar]
- 21.Hille G. Die Fettpolsterdicke bei der Beurteilung des Ernahrungszustandes von Kindern. Arch Kinderheilkunde 1923. ;73:134 [Google Scholar]
- 22.Himsworth HP. Diabetes mellitus: its differentiation into insulin-senstive and insulin-insenstive types. Lancet 1936. ;i:127 -30 [Google Scholar]
- 23.Ginsberg H, Kimmerling G, Olefsky JM, Reaven GM. Demonstration of insulin resistance in untreated adult onset diabetic subjects with fasting hyperglycemia. J Clin Invest 1975. ;55:454 -61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reaven GM, Olefsky J, Farquhar JW. Does hyperglycaemia or hyperinsulinaemia characterise the patient with chemical diabetes? Lancet 1972. ;i:1247 -9 [DOI] [PubMed] [Google Scholar]
- 25.Shen SW, Reaven GM, Farquhar JW. Comparison of impedance to insulin-mediated glucose uptake in normal subjects and in subjects with latent diabetes. J Clin Invest 1970. ;49:2151 -60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization. Definition, Diagnosis, and Classification of Diabetes Mellitus and Its Complications. Report of a WHO Consultation. Part 1: Diagnosis and Classification of Diabetes Mellitus. Geneva: WHO, 1999
- 27.Expert Panel on Detection E, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III)[see comment]. JAMA 2001; 285:2486 -97 [DOI] [PubMed] [Google Scholar]
- 28.Balkau B, Charles MA. Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR). Diabet Med 1999. ;16:442 -3 [DOI] [PubMed] [Google Scholar]
- 29.Einhorn D, Reaven GM, Cobin RH, Ford E, Ganda OP, Handelsman Y, et al. American College of Endocrinology position statement on the insulin resistance syndrome. Endocrine Practice 2003. ;9:237 -52 [PubMed] [Google Scholar]
- 30.Genuth S, Alberti KG, Bennett P, et al. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 2003. ;26:3160 -7 [DOI] [PubMed] [Google Scholar]
- 31.Cameron AJ, Shaw JE, Zimmet PZ. The metabolic syndrome: prevalence in worldwide populations. Endocrinol Metab Clin N Am 2004. ;33:351 -75 [DOI] [PubMed] [Google Scholar]
- 32.Unwin N, Patel S, Bhopal R, Fischbacher C, White M, Alberti G. A comparision of the prevalence and metabolic characteristics of WHO and NCEP definitions of the metabolic in three UK-based ethnic groups. Diabet Med 2003. ;20(Suppl 2):66 [Google Scholar]
- 33.Edwards K, Austin M, Newman B, Mayer E, Krauss R, Selby J. Multivariate analysis of the insulin resistance syndrome in women. Arteriosclerosis Thrombosis 1994. ;14:1940 -5 [DOI] [PubMed] [Google Scholar]
- 34.Meigs JB RB DA, Wilson PW, Cupples LA, Nathan DM, Singer DE. Risk variable clustering in the insulin resistance syndrome. The Framingham Offspring Study. Diabetes 1997. ;46:1594 -600 [DOI] [PubMed] [Google Scholar]
- 35.Scuteri A, Najjar SS, Morrell CH, Lakatta EG. The metabolic syndrome in older individuals: prevalence and prediction of cardiovascular events: the cardiovascular health study. Diabetes Care 2005. ;28:882 -7 [DOI] [PubMed] [Google Scholar]
- 36.Stern MP, Williams K, Gonzalez-Villalpando C, Hunt KJ, Haffner SM. Does the metabolic syndrome improve identification of individuals at risk of type 2 diabetes and/or cardiovascular disease? Diabetes Care 2004;27:2676 -81 [DOI] [PubMed] [Google Scholar]; [erratum Diabetes Care 2005. ;28:238 ] [Google Scholar]
- 37.De Backer G, Ambrosioni E, Borch-Johnsen K, et al. European guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J 2003. ;24:1601 -10 [DOI] [PubMed] [Google Scholar]
- 38.Last JM. A Dictionary of Epidemiology, 3rd edn. New York: Oxford University Press, 1995