Diabetes reduces life expectancy by five to 10 years. Premature cardiovascular disease is the most common cause of morbidity and mortality, but the microvascular complications specific to diabetes (box 1) are also contributory factors. Diabetes is the most common reason for renal replacement therapy worldwide, the most common cause of blindness in the under 65s, and the most common cause of non-traumatic amputation. With our current knowledge, most of these devastating events could be prevented or delayed, or their impact minimised. This review focuses on the prevention, early detection, and initial management of the vascular complications of diabetes in adults.
Why are the complications of diabetes important?
Complications are common and the cost to the individual and society is enormous. The onset of complications reduces quality of life, particularly when both microvascular and macrovascular disease are present.w1 The CODE-2 study gathered data on 7000 people with type 2 diabetes from eight European studies—72% had at least one complication and 24% had both (microvascular and macrovascular) complications.w2 Over six months, 13% of the patients were admitted to hospital for a mean of 23 days. The estimated average yearly cost per patient was €2834 (£1934, $3585); 55% of this cost was attributable to hospital admissions and only 7% to the cost of insulin and oral drugs for lowering glucose.1
Who develops complications?
The risk of developing complications is variable (table 1). For nephropathy, in particular, a strong but unknown genetic influence exists. The duration of diabetes, glycaemic control, and hypertension are the strongest risk factors for microvascular disease; smoking, blood pressure, lipids, and albuminuria are the strongest risk factors for macrovascular disease.
Table 1.
Risk factors and markers for the development of complications of diabetes
| Factors | Microvascular disease | Macrovascular disease |
|---|---|---|
| Non-modifiable | ||
| Genetic (susceptibility or protective) | ++ | ++ |
| Ethnic origin | + | + |
| Duration of diabetes | ++ | + |
| Modifiable or potentially modifiable | ||
| Glycaemic control | ++ | + |
| Blood pressure | ++ | ++ |
| Blood lipids | + | ++ |
| Smoking | + | ++ |
| Body mass index or waist to hip ratio | + | + |
| Other microvascular complications | + | + |
| Cardiovascular complications | + | + |
| Social deprivation | + | + |
| Novel risk markers | ||
| Markers of inflammation (such as C reactive protein) | + | + |
| Markers of endothelial dysfunction (such as von Willebrand factor) | + | + |
+=Moderate risk factor or marker; ++=strong risk factor or marker.
Macrovascular disease
Excess mortality from cardiovascular disease is seen in all age groups, particularly in young people with type 1 diabetes (box 2), and is exacerbated by social deprivation (table).w3 Premenopausal women with diabetes lose their protection against macrovascular disease (fig A on bmj.com).2 w4 w5 In type 2 diabetes, the risk of myocardial infarction and stroke is two to five times higher than in the general population.
Summary points
Patients with diabetes have an average reduction in life expectancy of five to 10 years, mainly because of premature cardiovascular disease
The microvascular complications specific to diabetes (retinopathy, nephropathy, neuropathy) also contribute to premature mortality and morbidity
The risk of vascular complications can be greatly reduced by tight control of glucose and blood pressure and by aggressive management of cardiovascular risk factors
Early detection of complications, by systematic annual screening, allows prompt intervention that may prevent or delay the emergence of end stage disease
A multifactorial approach to tightening the management of risk factors reduces the progression of microvascular and macrovascular complications
Retinopathy
The World Health Organization estimates that diabetic retinopathy is the cause of blindness in 5% of blind people worldwide.3 Almost everyone with diabetes has some degree of retinopathy after 20 years (see appendix on bmj.com for the grading of diabetic retinopathy), but only 20-50% of patients develop sight threatening disease. In some centres the cumulative incidence of sight threatening retinopathy is falling.4 w6 w7
Nephropathy
About half of patients with diabetes develop microalbuminuria at some point. Approximately one third will progress to proteinuria, one third will remain microalbuminuric, and one third will revert to normal albumin excretion (fig 1).w8 Microalbuminuria and proteinuria are more common in ethnic minorities worldwide.w9 w10 Once proteinuria is present, progression to end stage renal disease is inevitable. From 20% to 50% of patients who start renal replacement therapy have diabetes.5 w11 The rapid increase in the numbers of patients with diabetes requiring renal replacement in Europe in recent years is due mainly to the rise in the number of patients with type 2 diabetes (fig B on bmj.com).6
Fig 1.
Development of nephropathy
Box 1: Long term vascular complications of diabetes
Microvascular complications
Retinopathy
Nephropathy
Neuropathy
Macrovascular complications
Cerebrovascular disease
Ischaemic heart disease
Peripheral arterial disease
Neuropathy
Patients with diabetes have a 30-50% lifetime risk of developing chronic peripheral neuropathy (box 3), and 10-20% of patients develop severe symptoms.7 w12 w13 Peripheral neuropathy contributes to foot ulceration and amputation of lower limbs.8 Erectile dysfunction occurs in up to 50% of men over 50 years, compared with 15-20% of men without diabetes. Other neuropathies are rare but have a major impact on quality of life and life expectancy.
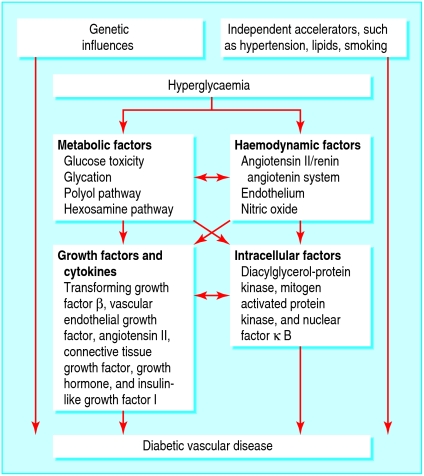
Pathophysiology
Both the metabolic and haemodynamic abnormalities of diabetes contribute to the development of complications. Intracellular hyperglycaemia develops in cells that cannot downregulate the uptake of glucose. This stimulates biochemical and haemodynamic pathways (fig 2). Signalling molecules and growth factors are activated, with consequent tissue damage.9 Genetic factors and external “accelerators” also contribute. A mechanism that links the activation of these pathways to the overproduction of superoxide by the mitochondrial electron transport chain has been suggested.10
Fig 2.
Metabolic pathways that contribute to vascular complications of diabetes
Sources and selection criteria
We searched PubMed with the keywords “diabetic complications”, “retinopathy”, “diabetic nephropathy”, “microalbuminuria”, “diabetic foot”, “peripheral neuropathy”, “cardiovascular disease”, “ischaemic heart disease”, “peripheral arterial disease”, and “cerebrovascular disease”. We gave preference to original articles published within the past three years and to reviews in journals with a high impact factor (rate of citation)
We searched the Cochrane database of systematic reviews; Cochrane database of abstracts and reviews of effectiveness; and Cochrane central registry of controlled trials
We searched personal archives of references
Microvascular complications are strongly associated with cardiovascular disease. A familial or genetic process may influence the development of both cardiovascular disease and microvascular pathology.w14-w16
How do I prevent complications?
Box 4 lists the main strategies to prevent the complications of diabetes.
Glucose control
The diabetes control and complications trial (DCCT) in type 1 diabetes and the UK prospective diabetes study (UKPDS) in type 2 diabetes showed that the lower the glycated haemoglobin achieved the lower the risk of microvascular complications.11,12 During the eight year open follow-up of the DCCT cohort, glycated haemoglobin values were similar in patients who had previously been managed intensively or conventionally.13,14 w17 Despite this, patients who had previously been in the intensively managed group were less likely to have microvascular complications (fig 3). Thus, a period of good glycaemic control reduces the risk of complications for longer than the duration of tight control, a phenomenon known as metabolic memory.
Fig 3.
Prevalence of complications at open follow-up of patients who completed the diabetes control and complications trial. Prevalence of progression at *four years and †eight years
The association between glucose control and cardiovascular disease is less strong but is still important. UKPDS found a 14% reduction in the risk of myocardial infarction for each 1% reduction in glycated haemoglobin.w18 In the long term follow-up of DCCT, the risk of a cardiovascular event was 42% lower in the intensively managed group (fig C on bmj.com).15
Box 2: Macrovascular disease in diabetes
Macrovascular disease is the main cause of death in type 1 and type 2 diabetes
Excess mortality is seen in all age groups, especially the young
Premenopausal women lose their protection against macrovascular disease
Disease is diffuse, distal, and affects many vessels
Reocclusion and reinfarction rates are higher after thrombolysis
Restenosis rates are higher after angioplasty, although drug eluting stenting may help
Five year survival after coronary artery bypass grafting is lower than in non-diabetic patients
Box 3: Neuropathies in diabetes
Peripheral neuropathies
Distal symmetric sensorimotor neuropathy
Femoral neuropathy (amyotrophy)
Mononeuropathies (ocular or truncal)
Pressure palsies (median, ulnar, or lateral popliteal)
Autonomic neuropathy
Postural hypotension
Bladder dysfunction
Gastric paresis
Constipation or diarrhoea, or both
Gustatory sweating (on the forehead, face, scalp, and neck after eating)
Erectile dysfunction
Blood pressure
In UKPDS, tight control of blood pressure (144/82 v 154/87 mm Hg) reduced the incidence of a microvascular event by 37%.16 A reduction in systolic blood pressure of 10 mm Hg was associated with a 13% reduction in risk for a microvascular event and an 11% reduction for myocardial infarction.w19 Other studies have shown that the reduction in relative risk is at least as great in the diabetic population as in the non-diabetic population, so that the absolute benefits of a reduction in blood pressure are greater.17,18
The choice of initial antihypertensive drug is less important than reducing blood pressure. Tight targets (< 130/80 mm Hg) are difficult to reach and require at least three antihypertensive drugs. Drugs that are taken once daily and that have good 24 hour cover should be used.
A Cochrane review suggests that angiotensin converting enzyme inhibitors are the best drugs to prevent microalbuminuria and nephropathy.19 w20 A recent meta-analysis that did not support this conclusion has been criticised for many reasons.w21
Lipids
Two placebo controlled trials have shown that treatment with statins reduces the risk of a major cardiovascular event by 37% in patients with type 2 diabetes without clinically apparent cardiovascular disease.20,21 The reduction in relative risk is as great in the diabetic population as in the non-diabetic population, so that the absolute benefit is greater.22 Thus, all patients with diabetes aged 40 years or more should be offered statins. Younger patients have a high lifetime risk of cardiovascular disease even though their 10 year risk is relatively low. Statins should be offered to those at particularly high risk (box 4).
When fibrates should be prescribed is unclear. In a recent large, randomised, controlled trial, fenofibrate did not reduce the risk of primary coronary events in type 2 diabetes.23 Despite the lack of robust evidence, however, once low density lipoprotein-cholesterol and control of blood glucose are optimal, clinicians should consider adding a fibrate to statin therapy if triglycerides are still greater than > 2.3 mmol/litre.
Box 4: Preventing complications
Glucose control
Glycated haemoglobin should be as low as possible (but avoid undue hypoglycaemia)—aim for < 7.0% if the patient is on insulin or < 6.5% if not on insulin
Blood pressure
Blood pressure should be as low as possible (avoiding symptoms of postural hypotension)—aim for < 130/80 mm Hg or < 125/75 mm Hg if proteinuria is present, if the glomerular filtration is < 60 ml/min/1.73 m2, or if the patient has cardiovascular disease
Lipids
Statins should be prescribed for patients over 40
Statins should be prescribed for patients under 40 who have microvascular or macrovascular complications, hypertension, metabolic syndrome, or a strong family history of cardiovascular disease
Total cholesterol should be < 4.5 mmol/litre
Low density lipoprotein-cholesterol should be < 2.5 mmol/litre
Fibrates should be prescribed if triglycerides are > 2.3 mmol/litre and low density lipoprotein-cholesterol values are < 2.5 mmol/litre
Aspirin
Aspirin should be prescribed for all patients over 40
Smoking
Patients should be encouraged to stop smoking
Lifestyle
Patients should be encouraged to lose weight if necessary, exercise, and eat healthily
Smoking
It is essential that patients stop smoking to reduce the risk of cardiovascular disease and probably the risk of microvascular complications.
Aspirin
Although no studies have been performed on primary prevention of cardiovascular disease in diabetes, low dose aspirin is usually recommended, even in the absence of overt cardiovascular disease.
How do I detect and screen for complications?
Complications must be diagnosed early—prompt intervention may prevent or delay the emergence of end stage disease such as blindness, the need for renal replacement therapy, or amputation. A systematic, structured screening programme, run annually, is most cost effective as a “one stop” package.
Macrovascular disease
Screening for macrovascular disease rests on symptoms of angina or claudication and with a low threshold for investigation. Routine exercise tolerance testing or stress echocardiography are not recommended. A 12 lead resting electrocardiogram has low sensitivity and specificity, although it does provide a useful baseline.
Box 5: Screening for peripheral neuropathy and peripheral arterial disease
Inquire about symptoms of peripheral neuropathy and peripheral vascular disease
Ask about previous foot ulceration or amputation
Ask about physical or visual difficulty in self management of foot care
Inspect feet for evidence of deformity, neuropathy, ischaemia, infection
Detect neuropathy with a 10 g monofilament or 128 Hz tuning fork or biosthesiometer. Use non-traumatic pin prick testing
Assess arterial circulation by measuring dorsalis pedis and posterior tibial foot pulses; measure Doppler ankle: brachial pressure ratio if available
Retinopathy
Corrected visual acuity should be measured and retinopathy assessed. Retinal photography, usually through dilated pupils and performed and interpreted by trained healthcare professionals, is the preferred method. Sensitivity and specificity must be acceptable, there must be an ongoing quality assurance programme, and the number of images that cannot be graded must be low.w22 Screening with static or “mobile” cameras can be performed in the community; the retinal images are read on site or at a distant centre.
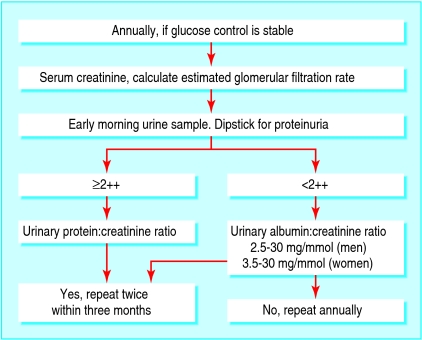
Nephropathy
Urine albumin and serum creatinine should be measured annually (fig 4). Positive urine samples should be repeated at least twice. Trends in albumin excretion with time are important. An estimated glomerular filtration rate is a better reflection of glomerular filtration than serum creatinine. Laboratories in the United Kingdom now do such estimations automatically, and web based calculators are available. Table 2 shows the agreed classification of renal disease based on estimated glomerular filtration rate.
Fig 4.
Screening for diabetic nephropathy
Table 2.
Classification of chronic kidney disease
| Stage | Description |
|---|---|
| 1 | Normal glomerular filtration rate (>90 ml/min/1.73 m2) with other evidence of kidney disease* |
| 2 | Mild impairment: glomerular filtration rate 60-90 ml/min/1.73 m2 with other evidence of kidney disease* |
| 3 | Moderate impairment: glomerular filtration rate 30-59 ml/min/1.73 m2 |
| 4 | Severe impairment: glomerular filtration rate 15-29 ml/min/1.73 m2 |
| 5 | Established renal failure: glomerular filtration rate <15 ml/min/1.73 m2 or on dialysis |
Other evidence of kidney disease: microalbuminuria, persistent proteinuria, persistent haematuria after exclusion of all other causes, structural abnormalities of the kidney on ultrasound, or biopsy confirmed glomerular nephritis.
Neuropathy and peripheral arterial disease
Box 5 shows what needs to be done to identify the four classic risk factors for developing diabetic foot problems (deformity, neuropathy, ischaemia, and infection).24 Questions should be asked about erectile function. Tests of autonomic function are not performed routinely.
How do I manage early complications?
General
Tight control of blood glucose and blood pressure reduces the risk of progression of background diabetic retinopathy to sight threatening disease and the progression of neuropathy.11,12,16 The effect of glucose control on progression of nephropathy is less certain. Blood pressure and lipid control are extremely important.
Cardiovascular disease
Most importantly, all patients with symptoms that might reflect vascular disease, particularly ischaemic heart disease, should be investigated. The absolute benefits of treatment with statins in secondary prevention of vascular disease are greater in people with diabetes.22
Retinopathy
Frequent retinal examination may be required, with referral to the ophthalmology department when sight threatening disease is apparent (table 3).
Table 3.
Urgency of referring patients with diabetic retinopathy to the ophthalmology department
| Problem | Time within which patient should be seen by ophthalmologist |
|---|---|
| Sudden loss of vision | Same day |
| Retinal detachment | Same day |
| New vessel formation | 2 weeks |
| Vitreous or preretinal haemorrhage | 2 weeks |
| Rubeosis iridis | 2 weeks |
| Hard exudates within 1 disc diameter of fovea | 12 weeks |
| Clinically important macular oedema | 12 weeks |
| Unexplained retinal findings | 12 weeks |
| Severe non-proliferative disease | 12 weeks |
Adapted from National Screening Programme for Diabetic Retinopathy workbook, version 3 (www.nscretinopathy.org.uk).
Nephropathy
All patients should be prescribed a long acting, once daily angiotensin converting enzyme inhibitor or angiotensin receptor blocker titrated up to the maximum recommended or tolerated dose.w23-w26 Additional antihypertensives should be used to achieve tight control of blood pressure. A target of 125/75 mm Hg is recommended for patients with proteinuria or an estimated glomerular filtration rate less than 60 ml/min/1.73 m2, although these guidelines are not evidence based. Combining an angiotensin converting enzyme inhibitor with an angiotensin receptor blocker or adding an aldosterone antagonist further reduces urine albumin excretion and blood pressure in the short term.w27-w29 However, long term benefits are unclear. Box 6 lists the indications for referral to the nephrology department.
Box 6: Indications for referring patients to the nephrology department
The glomerular filtration rate is < 45 ml/min/1.73 m2 (if possible, refer when < 60 ml/min/1.73 m2) or serum creatinine is > 150 μmol/litre
The estimated glomerular filtration rate falls by more than 20% each year
Presence of nephrotic syndrome
The diagnosis is unclear
Blood pressure is uncontrolled
Haemoglobin is < 100 g/litre and other causes have been excluded
Presence of abnormalities in bone chemistry
Neuropathy and peripheral arterial disease
Patients whose feet have a high risk of ulceration or gangrene need support and education about foot care; they also need to be given prophylactic foot care and special footwear.24 These measures can reduce amputation rates by 30-50%.w30 w31 Early referral of patients with ulcers (and those who have had ulcers in the past) to a specialist multidisciplinary team is essential.
Support and counselling should be available for men with erectile dysfunction. Investigations to exclude other causes (measurement of prolactin, follicle stimulating hormone, luteinising hormone, testosterone, and sex hormone binding globulin) may be necessary. Oral phosphodiesterase type 5 inhibitors are effective in about 60% of men with diabetes, less than in the non-diabetic population. Alternatives include sublingual apomorphine, intraurethral drugs, intracavernosal drugs, vacuum devices, and penile prostheses.
The importance of multifactorial care
A small randomised controlled trial of patients with type 2 diabetes, microalbuminuria, and hypertension showed the importance of a structured, protocol driven, multifactorial approach to managing the complications of diabetes.25 The intensively managed group received lifestyle advice, aspirin, and angiotensin converting enzyme inhibitors, with tight targets for glucose, blood pressure, and lipids in a specialist setting. The conventionally managed group received usual structured care in a primary care setting. Over eight years, the risks of progression of microvascular and macrovascular disease were reduced by 40-60% in the intensively managed group (table 4).
Table 4.
Benefits of multifactorial intervention25
| Complication | Hazard ratio (95% confidence interval) |
|---|---|
| Cardiovascular disease | 0.47 (0.24 to 0.73) |
| Nephropathy | 0.39 (0.17 to 0.87) |
| Retinopathy | 0.42 (0.21 to 0.86) |
| Autonomic neuropathy | 0.37 (0.18 to 0.79) |
How well are we doing?
Targets are not being met and drugs are not being prescribed appropriately in most patients with diabetes worldwide.w32 w33 Screening programmes for retinopathy and nephropathy are patchy or non-existent.w34 w35 In the UK, the uptake for retinal screening was 57.3% in 2005 (www.yhpho.org.uk). Patients find it difficult to comply with lifestyle advice, attendance for screening, and drugs,w36 w37 and those with most difficulty have worse outcomes.w38 w39
Additional educational resources
Diabetes UK (www.diabetes.org.uk)
American Diabetes Association (www.diabetes.org) International Diabetes Federation Clinical Guidelines Task Force. Global guidelines for type 2 diabetes.Brussels: International Diabetes Federation, 2005 (www.IDF.org)
European Union-Austrian conference on prevention of type 2 diabetes (www.diabetesconference.at)
The Finnish development programme for the prevention and care of diabetes in Finland (www.diabetes.fi/english/programme)
National service framework for renal services part 2. Chronic kidney disease, acute renal failure and end of life care. London: Department of Health 2005 (www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPAmpGBrowsableDocument/fs/en?CONTENT_ID=4102941&chk=aKHxDl)
National Screening Committee. Diabetic retinopathy screening workbook: guidance on setting up a systematic programme (www.nscretinopathy.org.uk)
Quality Outcomes Framework. Results for England 2004/5 (www.icservices.nhs.uk)
How can we improve?
Many changes are needed to prevent the complications of diabetes and minimise their impact. Under the auspices of the Austrian presidency, the European Union has developed a national plan of action for care in diabetes (www.diabetesconference.at), and such a plan has already been enacted in Finland (www.diabetes.fi/english/programme).
The most successful interventions include many components of care contained within the chronic care model,w40 w41 as described recently for foot care26:
Organisation of care
Clinical information systems
Support for clinical decisions
Delivery of care
Support for self management.26
Many examples of novel ways of improving outcomes exist. In the UK, the “payment by results” scheme of the primary care quality outcomes framework has resulted in many practices reaching the specified targets (www.icservices.nhs.uk). Overall, practices attained 93.2% of the total available points for diabetes. Appreciable benefits are likely to be seen as the targets for glycated haemoglobin, lipids, and blood pressure values are tightened.
Supplementary Material
 An appendix, extra references, and extra figures are on bmj.com. A long version of this paper is also on bmj.com
An appendix, extra references, and extra figures are on bmj.com. A long version of this paper is also on bmj.com
SMM is guarantor. Both authors contributed equally to preparing and writing this review.
Competing interests: SMM received payment from Novo-Nordisk for organising educational events and for attending conferences. She was a member of the International Diabetes Federation Clinical Guidelines Task Force. AF has been paid by Abbott Denmark, Astra Zenica R&D, GlaxoSmithKline Denmark, Novo-Nordisk A/S Denmark, Pfizer Denmark, Roche Pharmaceuticals, and Sanofi-Aventis/Bristol-Myers Squibb Denmark for speaking at educational programmes for nurses and doctors. He has served as a consultant for Pfizer International, Roche Pharmaceuticals, Sanofi-Aventis/Bristol-Myers Squibb Denmark, and Taisho Pharmaceuticals.
References
- 1.Jonsson B. CODE-2 advisory board. Revealing the cost of type II diabetes in Europe. Diabetologia 2002;45: S5-12. [DOI] [PubMed] [Google Scholar]
- 2.Laing SP, Swerdlow AJ, Slater SD, Botha JL, Burden AC, Waugh NR, et al. The British Diabetic Association cohort study II: cause-specific mortality in patients with insulin-treated diabetes mellitus. Diabetic Med 1999;16: 466-71. [DOI] [PubMed] [Google Scholar]
- 3.Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull World Health Organ 2004;82: 844-51. [PMC free article] [PubMed] [Google Scholar]
- 4.Rossing P. The changing epidemiology of diabetic microangiopathy in type 1 diabetes. Diabetologia 2005;48: 1439-44. [DOI] [PubMed] [Google Scholar]
- 5.US Renal Data System. USRDS 2005 annual data report. Bethesda, MD: National Institute of Health, National Institute of Diabetes, Digestive and Kidney Disease, 2005 (www.usrds.org/adr.htm).
- 6.Van Dijk PC, Jager KJ, Dtengel B, Gronhagen-Riska C, Feest TG, Briggs JD. Renal replacement therapy for diabetic end-stage renal disease: data from 10 registries in Europe (1991-2000). Kidney Int 2005;67: 1489-99. [DOI] [PubMed] [Google Scholar]
- 7.Tesfaye S, Kempler P. Painful diabetic neuropathy. Diabetologia 2005;48: 805-7. [DOI] [PubMed] [Google Scholar]
- 8.Boulton AJM, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet 2005;366: 1719-24. [DOI] [PubMed] [Google Scholar]
- 9.Schrijvers BF, De Vriese AS, Flyvbjerg A. From hyperglycemia to diabetic kidney disease: the role of metabolic, hemodynamic, intracellular factors and growth factors/cytokines. Endocr Rev 2004;25: 971-1010. [DOI] [PubMed] [Google Scholar]
- 10.Brownlee M. The pathobiology of diabetic complications. A unifying mechanism. Diabetes 2005;54: 1615-25. [DOI] [PubMed] [Google Scholar]
- 11.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329: 977-86. [DOI] [PubMed] [Google Scholar]
- 12.UK Prospective Diabetes Study. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet 1998;352: 837-53. [PubMed] [Google Scholar]
- 13.Writing Team for the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. Sustained effect of intensive treatment of type 1 diabetes mellitus on development and progression of diabetic nephropathy: the epidemiology of diabetes interventions and complications (EDIC) study. JAMA 2003;290: 2159-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martin CL, Albers J, Herman WH, Cleary P, Waberski B, Greene DA, et al, DCCT/EDIC Research Group. Neuropathy among the diabetes control and complications trial cohort 8 years after trial completion. Diabetes Care 2006;29: 340-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Research Group. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med 2005;353: 2643-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes. UKPDS 38. BMJ 1998;317: 703-13. [PMC free article] [PubMed] [Google Scholar]
- 17.Dahlof B, Sever PS, Poulter NR, Wedel H, Beevers DG, Caulfield M, et al, ASCOT Investigators. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethazide as required, in the Anglo-Scandinavian cardiac outcomes trial-blood pressure lowering arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet 2005;366: 895-906. [DOI] [PubMed] [Google Scholar]
- 18.ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. Major outcomes in high-risk hypertensive patients randomised to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). JAMA 2002;288: 2981-97. [DOI] [PubMed] [Google Scholar]
- 19.Strippoli GF, Craig M, Craig JC. Antihypertensive agents for preventing diabetic kidney disease. Cochrane Database Syst Rev 2005;4: CD004136. [DOI] [PubMed] [Google Scholar]
- 20.Heart Protection Study Collaborative Group. MRC/BHF heart protection study of cholesterol lowering with simvastatin in 20536 highrisk individuals: a randomised placebo-controlled trial. Lancet 2002;360: 7-22.12114036 [Google Scholar]
- 21.Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, et al, CARDS Investigators. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the collaborative atorvastatin diabetes study (CARDS): multicentre randomised placebocontrolled trial. Lancet 2004;364: 685-96. [DOI] [PubMed] [Google Scholar]
- 22.Costa J, Borges M, David C, Vaz Carneiro A. Efficacy of lipid lowering drug treatment for diabetic and non-diabetic patients: meta-analysis of randomised controlled trials. BMJ 2006;332: 1115-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keech A, Simes RJ, Barter P, Best J, Scott R, Taskinen MR, et al, FIELD Study Investigators. Effects of long-term fenofibrate therapy on cardiovascular events in 9795 people with type 2 diabetes (the FIELD study): randomised controlled trial. Lancet 2005;366: 1849-61. [DOI] [PubMed] [Google Scholar]
- 24.National Institute for Clinical Excellence. Clinical guideline 10; type 2 diabetes. Prevention and management of foot problems. National Institute for Clinical Excellence 2004 (www.NICE.org.uk/CGO10NICEguideline).
- 25.Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med 2003;348: 383-93. [DOI] [PubMed] [Google Scholar]
- 26.Reiber GE, Raugi GJ. Preventing foot ulcers and amputations in diabetes. Lancet 2005;366: 1676-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.