Abstract
Background
Severe acute respiratory syndrome (SARS) is continuing to spread around the world. All hospitals must be prepared to care for patients with SARS. Thus, it is important to understand the transmission of this disease in hospitals and to evaluate methods for its containment in health care institutions. We describe how we cared for the first 2 patients with SARS admitted to our 419-bed community hospital in Richmond Hill, Ont., and the response to a SARS outbreak within our institution.
Methods
We collected clinical and epidemiological data about patients and health care workers at our institution who during a 13-day period had a potential unprotected exposure to 2 patients whose signs and symptoms were subsequently identified as meeting the case definition for probable SARS. The index case at our hospital was a patient who was transferred to our intensive care unit (ICU) from a referral hospital on Mar. 16, 2003, where he had been in close proximity to the son of the individual with the first reported case of SARS in Toronto. After 13 days in the ICU, a diagnosis of probable SARS was reached for our index case. Immediately upon diagnosis of our index case, respiratory isolation and barrier precautions were instituted throughout our hospital and maintained for a period of 10 days, which is the estimated maximum incubation period reported for this disease. Aggressive surveillance measures among hospital staff, patients and visitors were also maintained during this time.
Results
During the surveillance period, 15 individuals (10 hospital staff, 3 patients and 2 visitors) were identified as meeting the case definition for probable or suspected SARS, in addition to our index case. All but 1 individual had had direct contact with a symptomatic patient with SARS during the period of unprotected exposure. No additional cases were identified after infection control precautions had been implemented for 8 days. No cases of secondary transmission were identified in the 21 days following the implementation of these precautions at our institution.
Interpretation
SARS can easily be spread by direct personal contact in the hospital setting. We found that the implementation of aggressive infection control measures is effective in preventing further transmission of this disease.
Severe acute respiratory syndrome (SARS) is a newly recognized illness associated with infection from a novel coronavirus.1,2,3 The first case of SARS in Canada was diagnosed in Toronto on Mar. 13, 2003.4 As of Apr. 24, 2003, 140 probable and 187 suspect cases of SARS had been reported in Canada,5 most in Toronto and surrounding communities. The virus has now been transmitted through 4 generations of cases in Canada.
York Central Hospital is a community hospital in Richmond Hill, Ont., in the Toronto area. It is a 419-bed facility with 219 acute care beds, 52 chronic care beds, 32 rehabilitation beds and 116 long-term care beds. There are over 1800 hospital staff, 300 physicians and 800 volunteers affiliated with this institution.
Between Mar. 16 and Mar. 28, 2003, there was unprotected exposure to 2 patients at our institution who were subsequently found to meet the epidemiological criteria for probable SARS.6 On Mar. 16, 2003, a 77-year-old man who required urgent hemodialysis was transferred from Scarborough Hospital, Grace Division, in Toronto to the intensive care unit of York Central Hospital. At the time of transfer, it was not known that the patient had been exposed to the SARS virus at the referring institution, thus, no specific respiratory isolation precautions were used. After he had spent 13 days in intensive care, the diagnosis of SARS was made.
On March 21, the wife of the first patient was also admitted to York Central Hospital and stayed there until March 26. Her presenting complaints were chest pain and dyspnea. She also had exposure to the SARS virus while visiting her husband at the referring hospital and while visiting her husband in intensive care during the period of unprotected exposure to the SARS virus at York Central Hospital. She was transferred to a nursing home for respite care on March 26. On March 29 she was readmitted to York Central Hospital with persisting respiratory symptoms. Because of the patient's history of direct contact with a probable SARS case (her husband), she was immediately placed in respiratory isolation and transferred to our SARS Assessment and Treatment Unit (SATU) upon her arrival.
We describe the hospital-wide infection control procedures that were used to prevent the further transmission of SARS within our hospital and the greater community and the clinical outcomes of the subsequent 14 cases of SARS that we managed.
Methods
Because of uncertainty pertaining to the infectivity of the SARS virus at the time our first patient was identified as having probable SARS, it was assumed that all individuals who had visited or were working at York Central Hospital during the 13-day period from Mar. 16 to Mar. 28, 2003, had potential unprotected exposure to the SARS virus. All of these individuals were instructed to enter a voluntary quarantine of 10 days from their last exposure to the hospital under the directive of the Regional Public Health Unit and the SARS Provincial Operations Centre for the Ontario Ministry of Health and Long-Term Care. All hospital employees and volunteers were contacted by telephone and told about the quarantine requirements. A list of all patients admitted, discharged, transferred or deceased who were at York Central Hospital between March 16 and March 28 was provided to the Provincial Operations Centre who then had the local public health units contact the relevant individuals, informing them of the quarantine directives. The news media were also used to facilitate the dissemination of this information.
Asymptomatic hospital staff were allowed to continue working at York Central Hospital during the quarantine period, but were prohibited from working at other institutions. All hospital staff and visitors were required to complete a SARS screening questionnaire7 before being permitted to enter the building. The screening process occurred outside the hospital's entrance in a heated tent that was erected specifically for this purpose. A pool of the hospital's nursing staff reviewed each person's responses on the questionnaire and took his or her temperature. Individuals who did not pass the screening questionnaire were referred to either the hospital's emergency department or to the occupational health department.
All individuals who entered the hospital were required to use full respiratory precautions consisting of gowns, gloves and N95 respirator masks during the hospital's 10-day quarantine period.
Two of the authors (H.D. and H.H.) interviewed patients regarding epidemiological risks and potential exposures to other patients and institutions affected by SARS. Potential occupational exposures for hospital employees were cross-referenced with employee work schedules. Physicians caring for patients with SARS at other Toronto area hospitals were surveyed by email for possible SARS-related admissions that were associated with the period of unprotected exposure at our hospital. The charts of all probable and suspect SARS cases treated at York Central Hospital were reviewed by 2 of the authors (H.D. and H.H.).
Because of quarantine constraints, ethics approval was obtained from the hospital's research committee by communication with committee members by electronic means. Written informed consent for the release of medical information for use in this study was obtained from all patients.
Case descriptions
Patient 1
Patient 1, a 77-year-old man, was transferred to York Central Hospital's intensive care unit from Scarborough Hospital, Grace Division, in Toronto for emergency hemodialysis, a service that was not available at the referring hospital. His past medical history was significant for type 2 diabetes mellitus, coronary artery disease, congestive heart failure and chronic renal failure. He had no recent travel history. Patient 1 was first admitted at the referring hospital on Mar. 7, 2003, and remained there until Mar. 10, 2003, for the treatment of congestive heart failure (Fig. 1). It was during this admission that patient 1, while in the emergency department of the referring hospital on March 7, had an unprotected exposure to another patient in the same treatment area who was subsequently identified as having probable SARS (Dr. David Rose, Scarborough Hospital, Grace Division, Toronto, Ont.: personal communication, Apr. 23, 2003).4 He returned to the emergency department of the referring hospital on March 14 with fever, dyspnea and pulmonary infiltrates. Recurrent congestive heart failure and pneumonia were diagnosed, and the patient was started on intravenous levofloxacin. He developed further deterioration in his renal function and respiratory status and was started on noninvasive positive-pressure ventilation (NIPPV). He was transferred to York Central Hospital on March 16, while on NIPPV for urgent hemodialysis for his acute respiratory and renal failure. On Mar. 17, 2003, his antibiotics were changed to intravenous ceftriaxone and intravenous azithromycin. Patient 1 was intubated on Mar. 18, 2003, for worsening respiratory failure consistent with acute respiratory distress syndrome. He remained febrile for 5 days until March 18. The condition of patient 1 continued to deteriorate, leading to progressive multi-organ dysfunction. He was started on intravenous methylprednisolone, 40 mg every 12 hours, on March 23 for unresolving acute respiratory distress syndrome. A pulmonary artery catheter was inserted on Mar. 25, 2003, demonstrating a pulmonary capillary wedge pressure (PCWP) of 15 mm Hg, while the patient received 18 cm H2O of positive end-expiratory pressure (PEEP) from the ventilator. Because of increasing concern regarding the number of SARS cases at the referring hospital, patient 1 was placed in respiratory isolation on March 27. He was not prescribed ribavirin therapy, because it was felt that antiviral medication would have limited effectiveness, given that the patient had had progressive symptoms for 2 weeks. On Mar. 29, 2003, patient 1 died of multi-organ failure. No autopsy was performed.
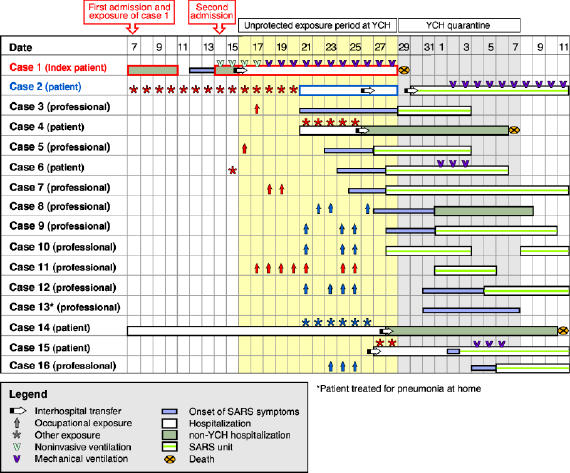
Fig. 1: Timeline of the SARS outbreak at York Central Hospital (YCH), Richmond Hill, Ont., from Mar. 7, 2003, to Apr. 11, 2003. The period of unprotected exposure extends from the admission of the first SARS case to YCH on Mar. 16, 2003, to the implementation of hospital-wide respiratory isolation and barrier precautions. That index patient's exposure and first and second admission to hospital were at Scarborough Hospital, Grace Division, Toronto. Photo: Myra Rudakewich
Patient 2
Patient 2, a 77-year-old woman, was the spouse of patient 1. She presented to York Central Hospital's emergency department on Mar. 21, 2003, with chest discomfort, fever (38.4°C) and dyspnea. Her past medical history was significant for atrial fibrillation, transient ischemic attack and osteoarthritis. Her chest radiograph demonstrated a 10% apical pneumothorax of the right lung with bilateral pulmonary infiltrates. She was admitted to the general surgery service for management of her pneumothorax, which was treated conservatively, without surgical intervention. She was then transferred to a nursing home on March 26, because her husband could not take care of her. On March 29, patient 2 was readmitted to York Central Hospital's SATU due to concern regarding her potential exposure to the first index case and persisting dyspnea. She had worsening respiratory failure, with the development of acute respiratory distress syndrome requiring orotracheal intubation and mechanical ventilation on Apr. 2, 2003. Bronchiolar lavage identified only normal respiratory flora. On Mar. 29, 2003, ribavirin therapy was started with a 2-g intravenous bolus, then 1 g intravenously every 6 hours for 4 days and then 500 mg intravenously every 8 hours for 6 days. On Mar. 30, 2003, she was started on systemic corticosteroids with intravenous methylprednisolone, 40 mg every 12 hours. She was successfully extubated after 10 days of mechanical ventilation and remains in hospital, as of April 24.
Results
Upon recognition of the unprotected exposure to the SARS virus at our hospital, respiratory isolation and barrier precautions were implemented throughout our hospital at 1800 hours on Mar. 28, 2003. Infection control measures and organizational interventions in restricting hospital access were implemented and the SATU was set up based on directives from the SARS Provincial Operations Centre of the Ontario Ministry of Health and Long-Term Care (Fig. 2).
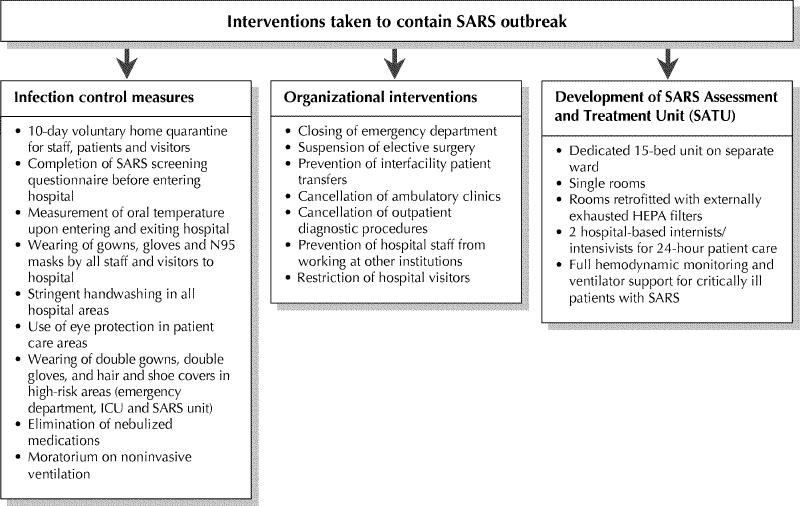
Fig. 2: Interventions taken to contain a SARS outbreak at York Central Hospital, Richmond Hill, Ont. SARS = severe acute respiratory syndrome, ICU = intensive care unit, HEPA = high efficiency particulate air.
The dedicated 15-bed SATU was created on a separate medical ward. This was accomplished within 24 hours. The ward had previously been empty as part of our hospital's ongoing expansion and redevelopment. The ventilation system for this ward was isolated from the rest of the hospital. The entire unit was kept at negative pressure relative to the hospital by 2 externally vented 1000-cfm exhaust fans. Each of the private patient rooms was maintained at a negative pressure relative to the corridor by externally vented 270-cfm HEPA (high efficiency particulate air) air filters. Appropriate monitoring equipment was used to allow for the care of critically ill and mechanically ventilated patients with SARS in the SATU. A dedicated team of physicians, nurses and other allied health care providers provided care to the patients on the SATU. Using an approach similar to that taken at Mount Sinai Hospital8 in Toronto, staff members for the SATU were recruited from the intensive care unit and the medical–respiratory ward for their expertise in the treatment of both critically ill patients and patients requiring respiratory isolation. In order to limit the number of physicians working in both the SATU and other areas of the hospital, a weekly call roster assigned all patients admitted to the SATU to a single attending physician. Two critical care physicians provided 24-hour attending physician coverage for the SATU. Two additional critical care physicians provided additional support in the management of mechanically ventilated SARS patients on the SATU. The follow-up of recovered SARS patients discharged from hospital was performed in accordance with the World Health Organization (WHO) guidelines.9
Ten hospital staff members who met the case definition for either probable or suspect SARS were identified (Table 1).6 The SARS screening tool identified 3 of the 10 hospital staff when they arrived at work. Four hospital staff had direct personal contact with patient 1 during the period of unprotected exposure. Five hospital staff had direct personal contact with patient 2 during the period of unprotected exposure. One hospital employee (case 13) had no identifiable direct contact with either patient, but was working at the hospital during the period of unprotected exposure and met the clinical criteria for probable SARS.
Table 1
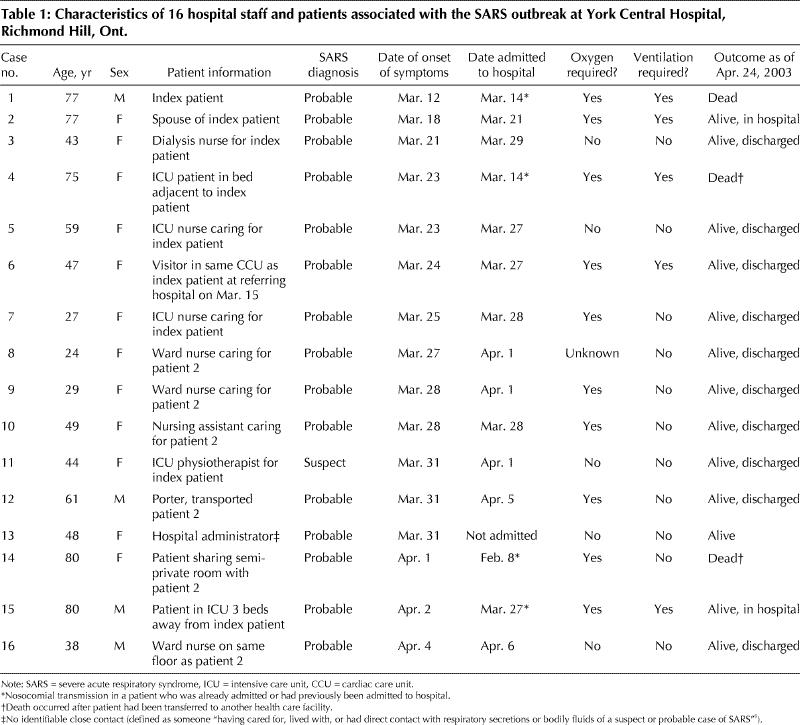
Four patients were identified who met the case definition for either probable or suspect SARS. Two hospital patients were exposed to patient 1 while in the intensive care unit before the implementation of hospital-wide respiratory precautions. One patient had shared the same room as patient 2 during the period of unprotected exposure. Another patient (case 6) was a visitor at the referring hospital for patient 1 on Mar. 15, 2003, where she was visiting a patient in the same cardiac care unit where patient 1 was being treated.
Of the 15 cases with probable or suspect SARS associated with our index patient, 11 were admitted to the SATU, 3 were treated at other hospitals and 1 was treated at home. Nine of the 11 cases admitted to the SATU have since been discharged home. No further cases of probable or suspect SARS related to the 13-day period of unprotected exposure were identified in the 10 days following the hospital-wide quarantine period, which ended on Apr. 7, 2003.
Interpretation
The initial public health response to the SARS outbreak within our hospital involved the mass voluntary quarantine of over 5000 people.10 The rationale for this action was the hypothesis that our hospital was “grossly contaminated” during the period of unprotected exposure. The quarantine measures affected over 1800 hospital staff, 225 physicians, 170 neighbouring high school students who use the hospital cafeteria and hundreds more volunteers, patients and visitors. There was also tremendous disruption to the community's ability to access acute medical care services. The vast majority of SARS cases identified in this study had clearly identifiable direct personal contact with a symptomatic probable SARS patient. In only 1 of the 15 cases identified was there no identifiable period of close contact with a probable SARS patient. Although this case did meet the case definition for probable SARS, the clinical course was different from the other SARS cases and, in the opinion of the authors, this individual probably did not have SARS at all.
Our knowledge about the natural history, diagnosis and treatment of SARS grows each week. In retrospect, many of the treatments that are commonly used in the acute management of respiratory disease may have actually facilitated the transmission of the SARS coronavirus.11 The index patient at our hospital and the index patient at the referring hospital to whom he was exposed were both treated with NIPPV.4 The use of NIPPV and nebulized medications should be avoided in SARS patients.
There are several limitations to our study. Due to the still uncertain natural history of this disease, it is conceivable that patients with subclinical or very mild disease may not have been identified by the screening tool (e.g., patients without fever or cough). The opportunity for transmission of SARS by such patients would have been prevented by the hospital-wide implementation of respiratory isolation and barrier precautions. It is also possible that some visitors to the hospital may not have been made aware of the risk of potential SARS exposure and quarantine instructions, despite the high media profile given to this outbreak. These individuals would also be at a much lower risk of contracting SARS due to the lack of opportunity for close contact with a symptomatic patient. Our precision at diagnosing infection caused by the SARS coronavirus is limited by the current epidemiologically based definition. It is possible that some of the current staff and patients diagnosed with probable or suspect SARS were not actually infected by the SARS coronavirus, because many of the clinical features of SARS are shared by a variety of common nosocomial infections, as well as community-acquired respiratory infections. As the identification of an epidemiological link becomes more difficult through successive generations of transmission, our ability to accurately distinguish SARS from other illnesses is impaired. This highlights the urgent need for a rapid laboratory test to identify illness caused by the SARS coronavirus.
In this study, we illustrate how the rigorous application of respiratory isolation and barrier precautions is an effective means of controlling the spread of this disease in the hospital setting. Hospital workers remain on the front lines in the global response to SARS. They are at considerable risk of contracting SARS when there is an opportunity for unprotected exposure.4,8,11 Continued vigilance is required in the screening of hospital staff, patients and visitors to prevent the future introduction of this disease into hospitals. Public health efforts focused on identifying the close contacts of new patients should help to limit the spread of SARS from the hospital setting to the community. Further study of the utility of mass voluntary quarantine measures in the management of future SARS outbreaks is warranted.
β See related articles pages 1432 and 1434
Supplementary Material
Footnotes
Fast-tracked article, published at www.cmaj.ca on Apr. 25, 2003
Contributors: Dr. Dwosh was the principal investigator and initiated and developed the study thesis and design. He collected and reviewed clinical data and drafted and edited the manuscript. Dr. Hong provided clinical data, contributed substantially to the study design and framework, and critically revised the manuscript. Dr. Austgarden provided clinical data and a critical review of the manuscript. He prepared the background literature review. Dr. Herman provided clinical data and a critical review of the manuscript. Dr. Schabas contributed to conception of the study, critical review and revision of the manuscript. All authors approved the final version.
Competing interests: None declared.
Correspondence to: Dr. Hy Dwosh, ICU Director, York Central Hospital, 10 Trench St., Richmond Hill ON L4C 4Z3; fax 905 883-2802; hdwosh@yorkcentral.on.ca
References
- 1.Peiris JSM, Lai ST, Poon LLM, Guan Y, Yam LYC, Lim W, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet [early online release 2003 Apr 8]. Available: http://image.thelancet.com/extras/03art3477web.pdf (accessed 2003 Apr 24).
- 2.Ksiazek TG, Erdman D, Goldsmith CS, Zaki SR, Peret T, Emery S, et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med [early online release 2003 Apr 10]. Available: http://content.nejm.org/cgi/reprint/NEJMoa030781v3.pdf (accessed 2003 Apr 24). [DOI] [PubMed]
- 3.World Health Organization. Coronavirus never before seen in humans is the cause of SARS [press release]. Geneva: The Organization; 2003 Apr 16. Available: www.who.int/mediacentre/releases/2003/pr31/en/) (accessed 2003 Apr 24).
- 4.Poutanen SM, Low DE, Henry B, Finkelstein S, Rose D, Green K, et al. Identification of severe acute respiratory syndrome in Canada. N Engl J Med [early online release 2003 Mar 31]. Available: http://content.nejm.org/cgi/reprint/NEJMoa030634v3.pdf (accessed 2003 Apr 24). [DOI] [PubMed]
- 5.Health Canada. Latest Canadian numbers on SARS. 2003 Apr 25. Available: www.hc-sc.gc.ca/english/protection/warnings/sars/sars_numbers.html (accessed 2003 Apr 25).
- 6.World Health Organization. Global surveillance for severe acute respiratory syndrome (SARS). Weekly epidemiological record 2003;78(14):100-5. Available: www.who.int/wer/pdf/2003/wer7814.pdf (accessed 2003 Apr 23). [PubMed]
- 7.SARS Provincial Operations Centre for the Ontario Ministry of Health and Long-Term Care. Severe acute respiratory syndrome (SARS) screening tool for all Ontario healthcare settings, 2003. Available: www.oma.org/phealth/SARSScreeningTool.htm (accessed 2003 Apr 23).
- 8.Maunder R, Hunter J, Vincent L, Bennet J, Peladeau N, Leszcz M, et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003;168(10):1245-51 [early online release 2003 Apr 16]. Available: www.cma.ca/cmaj/early_releases/maunder.pdf (accessed 2003 Apr 24). [PMC free article] [PubMed]
- 9.World Health Organization. WHO hospital discharge and follow-up policy for patients who have been diagnosed with severe acute respiratory syndrome (SARS). Geneva: The Organization; 2003. Available: www.who.int/csr/sars/discharge/en/ (accessed 2003 Apr 24).
- 10.Queen L. Staff exposed to second SARS case. Liberal [Richmond Hill] 2003 Apr 10; Sect A:1-2.
- 11.Lee N, Hui D, Wu A, Chan P, Cameron P, Joynt GM, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med [early online release 2003 Apr 7]. Available: http://content.nejm.org/cgi/reprint/NEJMoa030685v2.pdf (accessed 2003 Apr 24). [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


