Abstract
The A2A adenosine receptor (A2AR) has been shown to be a critical and nonredundant negative regulator of immune cells in protecting normal tissues from inflammatory damage. We hypothesized that A2AR also protects cancerous tissues by inhibiting incoming antitumor T lymphocytes. Here we confirm this hypothesis by showing that genetic deletion of A2AR in the host resulted in rejection of established immunogenic tumors in ≈60% of A2AR-deficient mice with no rejection observed in control WT mice. The use of antagonists, including caffeine, or targeting the A2 receptors by siRNA pretreatment of T cells improved the inhibition of tumor growth, destruction of metastases, and prevention of neovascularization by antitumor T cells. The data suggest that effects of A2AR are T cell autonomous. The inhibition of antitumor T cells via their A2AR in the adenosine-rich tumor microenvironment may explain the paradoxical coexistence of tumors and antitumor immune cells in some cancer patients (the “Hellstrom paradox”). We propose to target the hypoxia→adenosine→A2AR pathway as a cancer immunotherapy strategy to prevent the inhibition of antitumor T cells in the tumor microenvironment. The same strategy may prevent the premature termination of immune response and improve the vaccine-induced development of antitumor and antiviral T cells. The observations of autoimmunity during melanoma rejection in A2AR-deficient mice suggest that A2AR in T cells is also important in preventing autoimmunity. Thus, although using the hypoxia→adenosine→A2AR pathway inhibitors may improve antitumor immunity, the recruitment of this pathway by selective drugs is expected to attenuate the autoimmune tissue damage.
Keywords: autoimmunity, cancer, therapy, hypoxia, inflammation
The coexistence of tumors and antitumor immune cells is currently explained by the inhibition of immune cells in a poorly understood “hostile” tumor microenvironment (1–3). This unidentified immunosuppressive mechanism limits promising cancer therapies using antitumor T cells (4–14). We hypothesized that cancerous tissues are protected from antitumor T cells because of immunosuppressive signaling via T cell A2A adenosine receptor (A2AR) (15–17) activated by extracellular adenosine produced from hypoxic tumor (Fig. 1a). Indeed, hypoxic cancerous tissues may be protected by the same hypoxia→adenosine→A2AR pathway that was recently shown to be critical and nonredundant in preventing excessive damage of normal tissues by overactive immune cells in vivo (18). It is well established that some areas of solid tumors often have transient or chronic hypoxia (19, 20), which is conducive to extracellular adenosine accumulation (21). Hypoxia has been implicated in mechanisms of tumor protection against ionizing radiation and some chemotherapeutic agents (19) and is associated with poor prognosis (20).
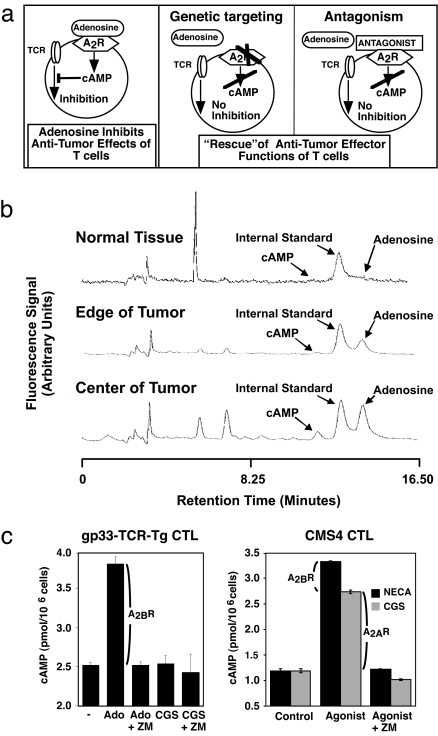
Fig. 1.
Overview of experimental strategy to test the hypothetical mechanism of tumor protection. (a) It is assumed that adenosine and A2AR, which inhibit overactive immune cells to protect normal tissues (18), may protect malignant tissues from antitumor T cells. The transient or chronic hypoxia in the tumor microenvironment (19, 20) could be conducive to accumulation of adenosine (15, 27), which then may inhibit antitumor CD8+ T cells by increasing their immunosuppressive intracellular cAMP levels (15–17). Genetic targeting of A2AR may deinhibit CD8+ T cells and thereby facilitate their antitumor effector functions, as was shown in models of T cell-dependent viral and autoimmune hepatitis (18). A similar outcome could be accomplished by using A2AR antagonists, e.g., ZM241,385, which were shown to prevent adenosine-triggered cAMP elevation (26), reverse the adenosine-mediated inhibition of activated CD8+ T cells (24) in vitro, and deinhibit activated immune cells in vivo (18). Evidence for such a tumor-protecting mechanism may also be interpreted as proof of principle for the feasibility of a novel strategy of tumor destruction, where the interruption of hypoxia→adenosine→A2AR signaling in tumors may rescue the antitumor immune response from inhibition in the hostile tumor environment. (b) Demonstration of a gradient of increased levels of extracellular adenosine and cAMP in a solid tumor environment using an equilibrium microdialysis probe (see Supporting Text). (c) Expression of functional A2AR and/or A2BR on tumor-specific CD8+ T cells. CMS4 sarcoma-specific CD8+ T cells and anti-gp33 CD8+ T cells were used in the experiments of Figs. 4 and 11. The levels of A2AR-selective agonist CGS21680-induced cAMP reflect the expression of A2AR, and the adenosine- or 5′-(N-ethylcarboxamido) adenosine (NECA)-induced cAMP represents the sum of signaling by both A2AR and A2BR. The difference between adenosine/NECA and CGS21680 provides an indication as to the relative contribution of A2BR.
T cells, including antitumor T cells, do predominantly express cAMP-elevating Gs protein-coupled high-affinity A2AR and/or low-affinity A2B adenosine receptors (A2BR) (16, 17, 22–24); the number of A2AR per T cell may determine the intensity of maximal T cell response to adenosine (25, 26). Whereas we focused on A2AR, others have discounted A2 receptors and suggested the A3 adenosine receptors as responsible for inhibition of antitumor killer T cells (27, 28). Here we report that genetic deletion of A2AR accomplishes the complete rejection of immunogenic tumors by antitumor CD8+ T cells in the majority (≈60%) of mice, whereas the antagonists of A2 receptors facilitate CD8+ T cell-mediated retardation of tumor growth.
Results
The Gradient of T Cell-Inhibiting Extracellular Adenosine in Tumors.
It was important to confirm the presence of elevated extracellular adenosine levels in cancerous tissues using a reliable method (29). The HPLC analysis and the use of equilibrium dialysis probes demonstrated higher levels of extracellular adenosine (Fig. 1b), increased adenosine metabolism, and the concomitant increase in cAMP (29) in a solid tumor microenvironment (Fig. 7, which is published as supporting information on the PNAS web site). We also confirmed that antitumor CD8+ T cells used in this study do express the cAMP-elevating functional A2AR and A2BR (Fig. 1c). To directly test whether A2AR inhibit antitumor T cells in vivo, we studied the effects of A2AR gene deletion or competitive antagonists on tumor growth in mice using different CD8+ T cell-dependent cancer immunosurveillance and adoptive immunotherapy models.
A2AR Deficiency in the Host Leads to Complete Tumor Rejection.
To provide genetic evidence of the role of A2AR in protecting tumors from antitumor T cells, we compared the growth of immunogenic CL8-1 melanoma (Fig. 2) and RMA T lymphoma (Fig. 3) in C57BL/6-background A2AR gene-deficient (A2AR−/−) and in WT control C57BL/6 mice. We selected these well established tumor models because the growth of CL8-1 melanoma (30, 31) and RMA T lymphoma (32) is controlled by endogenous antitumor CD8+ T cells up to a certain size, and then the tumor kills 100% of tumor-bearing mice (see Supporting Text, which is published as supporting information on the PNAS web site). The key role of CD8+ T cells in response to CL8-1 is confirmed in control experiments (Fig. 8, which is published as supporting information on the PNAS web site), where similar acceleration of the onset of CL8-1 growth was observed in RAG-1−/− and CD8−/− mice, but not in CD4−/− mice, as compared with WT mice. This finding was also confirmed in WT mice depleted of either CD4+ or CD8+ T cells by injecting anti-CD8 or anti-CD4 antibodies (see Supporting Text).
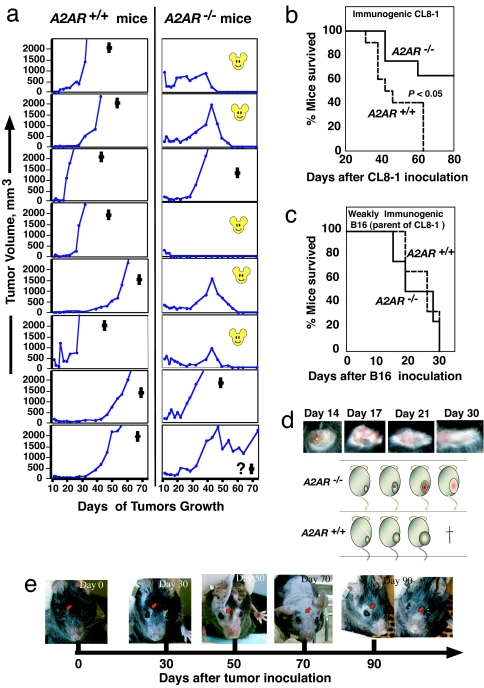
Fig. 2.
Genetic deficiency of A2AR may lead to complete rejection of established CL8-1 melanoma and to survival of tumor-bearing mice. (a) A2AR inactivation by genetic mutation may lead to complete tumor rejection. The A2AR−/− mice or WT mice were inoculated s.c. with 3 × 106 CL8-1 melanoma cells. The mouse faces on the graph indicate complete tumor rejection and mouse survival, whereas the cross indicates that the mouse had to be euthanized according to an animal care protocol when tumors reached ≈2 cm in diameter. The question mark in the lowest graph of tumor rejection by A2AR−/− mice indicates that this mouse would likely have completely rejected tumor and survived; even though the tumor itself was being destroyed by CD8+ T cells, the “wounded” tissue was ≈2 cm in diameter, and mice had to be euthanized according to the animal care protocol. Shown are representative results of two experiments. (b) Genetic evidence that inactivation of A2AR may lead to survival of mice with inoculated CL8-1 melanoma (the same experiment as in a). (c) A2AR inactivation by genetic mutation is not sufficient to ensure tumor rejection and survival of mice with inoculated nonimmunogenic B16 melanoma. Groups of A2AR−/− mice or WT mice were inoculated s.c. with 5 × 104 B16 melanoma cells, and tumor growth was monitored. No rejection of B16 has been observed in any mice, and no differences in survival were observed between WT C57BL/6 and A2AR−/− mice. Shown are representative results of two experiments. (d) Photographs of a typical tumor’s wound-healing process during and after an immune attack by anti-CL8-1 CD8+ T cells in A2AR−/− mice. (e) Unusual appearance of mice with CL8-1 melanoma tumor, which grew to a large size and then was rejected. Two mice with such a phenotype were observed among five A2AR−/− survivors of CL8-1 melanoma.
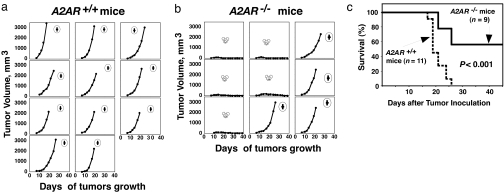
Fig. 3.
A2AR inactivation by genetic mutation may lead to a complete rejection of established RMA T lymphoma by antitumor CD8+ T cells, ensuring survival of tumor-bearing mice. (a and b) A2AR inactivation by genetic mutation may lead to complete RMA T lymphoma tumor rejection. The A2AR−/− mice (n = 9) or WT mice (n = 11) were inoculated s.c. with 2 × 105 RMA T lymphoma cells. Representative results of two experiments are shown. (c) A2AR inactivation by genetic mutation may lead to survival of mice with inoculated RMA lymphoma. Shown are representative results of two experiments.
Remarkably, in ≈60% of A2AR−/− tumor-bearing mice, both CL8-1 (Fig. 2a) and RMA (Fig. 3b) tumors have been completely rejected after reaching a relatively large size. The elimination of tumor resulted in mouse survival (Figs. 2b and 3c). In contrast, no tumor rejection and no mice survival was observed in parallel controls with tumor-inoculated WT mice (Figs. 2a and 3a), which do express the tumor-protecting A2AR on their antitumor CD8+ T cells. In an important internal control, no tumor rejection or mouse survival was observed when the parent of CL8-1, the nonimmunogenic B16 melanoma, was inoculated into either WT or A2AR−/− mice (Fig. 2c).
The anti-CL8-1 melanoma response of CD8+ T cells in the A2AR−/− host was accompanied by different appearance of tumors and of tumor-rejecting mice as compared with WT mice (Fig. 2 d and e). Whereas the solid, spherical, and well defined tumors were continuously increasing in size in WT mice, the soft, flat, poorly defined tumors in A2AR−/− mice often showed central necrosis, and, in some mice, their disappearance and healing were accompanied by hair loss. In addition, the signs of spontaneously resolved autoimmunity were observed in some A2AR−/− mice, which rejected tumors. As shown in Fig. 2e, these tumor-rejecting mice lost hair around the eyes around day 30, and then (day 70) became “nude”-like. On day 90 the hair was regrown. These observations resemble reports of autoimmunity in melanoma-rejecting mice (13) and melanoma patients who were undergoing immunotherapy with melanoma antigen-specific T cells (14).
Importantly, the deficiency in A2AR did not prevent the establishment or the early growth of inoculated tumors; rather, it has improved the destruction of larger, developed tumors (Figs. 2 and 3). In some experiments the CL8-1 tumors started growing similarly in both WT and A2AR−/− host, and then the tumor seemed to disappear (around day 14) in both WT and A2AR−/− mice only to reappear in WT mice but not in A2AR−/− mice (data not shown). The early time course of growth and rejection of RMA tumors in A2AR−/− mice, but not in WT controls, is shown in Fig. 9, which is published as supporting information on the PNAS web site.
The outcome described here depended on the size of the tumor inoculum, which determines the capability of antitumor CD8+ T cells to completely reject tumors. A smaller number of injected cells resulted in rejection of tumors even in WT mice, although the rejection was statistically significantly accelerated in A2AR−/− mice (Fig. 9).
A2AR and A2BR Antagonists Facilitate the Retardation of Tumor Growth Mediated by Antitumor CD8+ T Cells.
To test whether the pharmacological inhibition of A2AR would render antitumor CD8+ T cells resistant to inhibition by tumor-produced adenosine (Fig. 1), we studied the effects of ZM241,385 [a competitive and selective antagonist of both A2AR and A2BR (23, 33, 34)] or of caffeine (1,3,7-trimethylxanthine) [which at physiologically relevant concentrations preferentially antagonizes A2AR (35)]. The effects of antagonists were tested in models of cancer immunosurveillance by endogenous CD8+ T cells and in adoptive immunotherapy models using in vivo induced and ex vivo expanded antitumor CD8+ T cells of defined antigen specificity (30, 31, 36–39).
Effect of A2 Adenosine Receptor Antagonists on Adoptively Transferred Antitumor CD8+ T Cells.
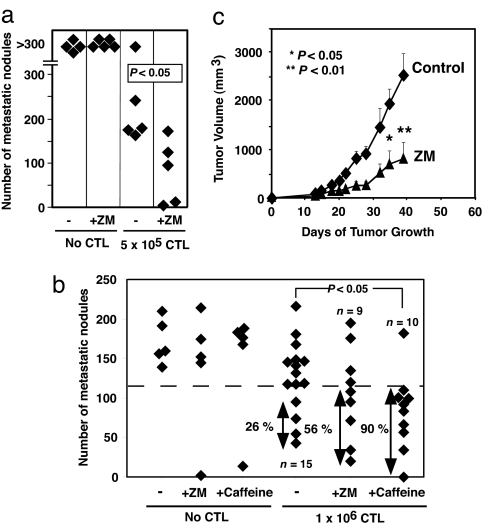
The A2 receptors antagonists ZM241,385 and caffeine were found to enhance the antitumor effects of CD8+ T cells in studies of anti-CMS4 sarcoma CD8+ T cells in a lung metastasis model. Controls confirmed that CD8+ T cells used are tumor peptide-specific (data not shown), and they do express functional A2AR and A2BR (Fig. 1c) because the adenosine-induced increase of cAMP could be blocked by either ZM241,385 or caffeine (Fig. 10, which is published as supporting information on the PNAS web site). The combined treatment of mice with adoptive transfer of CD8+ T cells and antagonists resulted in statistically better destruction of lung metastasis than with CD8+ T cells alone (Figs. 4 a and b and 10).
Fig. 4.
Treatment of mice with A2AR/A2BR antagonist enhanced the destruction of established tumors by tumor antigen-specific CD8+ T cells. (a) The antagonist ZM241,385 improved destruction of CMS4 lung metastasis by antitumor CD8+ T cells. (b) Enhancement of destruction of CMS4 lung metastasis by adoptively transferred CD8+ T cells in mice that consumed caffeine in drinking water. Based on the aggregation of the data points in the control “only tumor” and “caffeine alone” groups, an arbitrary cutoff value (a more than ≈20% decrease in the number of metastatic nodules) was assigned to illustrate a potential therapeutic efficacy threshold (shown as the percentage of mice with decreased number of metastases) for those groups of mice that were treated with both CD8+ T cells and A2 receptor antagonists. (c) ZM241,385, an antagonist of A2AR and A2BR, enhances CD8+ T cell-mediated antitumor immune response in mice with established s.c. solid CL8-1 melanoma. Data represent mean ± SEM.
A2 adenosine receptor antagonists also improved the antitumor activity of effector CD8+ T cells specific for the poorly immunogenic tumor LL-LCMV as evidenced by strongly enhanced CD8+ T cell-mediated destruction of LL-LCMV tumor and tumor growth retardation after administration of caffeine (Fig. 11, which is published as supporting information on the PNAS web site).
Effect of A2 Adenosine Receptor Antagonist on Endogenously Developed Antitumor CD8+ T Cells.
The antagonists significantly delayed the onset of rapid growth of CL8-1 melanoma, even if injections of ZM241,385 started after tumors reached a relatively large size (Fig. 4c). No tumor rejection or mouse survival was observed during the course of treatments with antagonists in any tested model, although both tested antagonists did significantly improve the CD8+ T cell-mediated delay of the onset of rapid tumor growth. Further improvement of the effects of antagonists may require compounds with significantly extended half-lives in vivo, because the antagonists used here have a very short half-life in mice (≈30–50 min; see Fig. 12, which is published as supporting information on the PNAS web site). Of promise, caffeine has a much longer half-life in vivo in humans (40).
A2AR/A2BR Antagonists May Deinhibit the Production of IFN-γ by Antitumor T Cells in the Tumor Microenvironment.
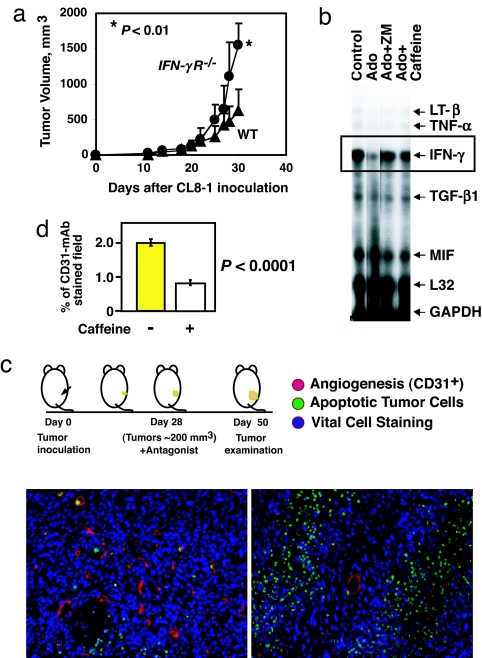
The neovascularization-inhibiting properties of IFN-γ were shown to be crucial for antitumor action of T cells in vivo (8), and better tumor destruction in mice with inactivated A2AR/A2BR (Figs. 2–4) could be at least partially explained by the release of CD8+ T cells from A2AR-mediated inhibition of IFN-γ production in the adenosine-rich tumor microenvironment (Fig. 1). The acceleration of CL8-1 melanoma growth in IFN-γ receptor gene-deficient mice (Fig. 5a) and observations of capacity of A2AR/A2BR-mediated signaling to inhibit the T cell receptor-triggered up-regulation of IFN-γ mRNΑ, lymphotoxin-β mRNA, and TNF-α mRNA in antitumor T cells (Fig. 5b) are consistent with this hypothesis.
Fig. 5.
Treatment with caffeine inhibits neovascularization and increases apoptosis of CL8-1 melanoma in mice. (a) Genetic evidence that growth of inoculated CL8-1 melanoma cells depends on functional IFN-γ receptors (IFN-γR). The IFN-γR−/− or WT C57BL/6 mice (8–10 mice per group) were inoculated s.c. with 3 × 106 CL8-1 melanoma cells. All data represent mean ± SEM. (b) Extracellular adenosine inhibits up-regulated IFN-γ gene transcription in activated antitumor T cells, and this inhibition is prevented by adenosine receptor antagonists ZM241,385 (ZM) and caffeine. mRNA levels were analyzed by an RNase protection assay. (c) Immunohistochemical demonstration of increased tumor destruction and inhibition of angiogenesis in tumors in mice treated with caffeine. Mice were inoculated with CL8-1 and treated with caffeine. CL8-1 melanomas growing in C57BL/6 mice were removed at day 50 from control (Lower Left) and caffeine-treated (Lower Right) mice. (d) The degree of angiogenesis was determined as the percentage of CD31+ staining to the total field. The y axis (percentage of fields positive for CD31) reflects the percentage of area occupied by blood vessels in comparison to the total tumor area. The summary of measurements of two tumors per group is presented. Methods for the RNase protection assay and immunohistochemistry are provided in Supporting Text.
The increased levels of IFN-γ near or within tumors in mice with inactivated A2AR/A2BR were, in turn, expected to inhibit neovascularization and thereby enhance tumor cell death. This expectation was confirmed by observations of antagonist (caffeine)-mediated inhibition of tumor neovascularization and by increased apoptosis of tumor cells (Fig. 5c). Significantly more blood vessels and sprouting capillaries were observed in tumors from untreated mice than in tumors from caffeine-treated mice (Fig. 5 c and d). The large established blood vessel visible in the center of Fig. 5c Lower Right (red) reflects the fact that treatment with caffeine started at day 28, when the tumor was already large (≈200 mm3). In addition, fewer surrounding new small vessels or endothelial cells were observed in a representative field. Tumor cells (blue) around this vessel area are normal and viable; however, farther away from this vessel area there are almost no new sprouting capillaries, and there are numerous apoptotic tumor cells (Fig. 5c Lower Right, green).
Antitumor Effects of A2AR Targeting Are CD8+ T Cell-Dependent.
The genetic deletion or pharmacological antagonism of A2AR resulted in complete rejection or growth retardation of tumors only if they were immunogenic and generated antitumor CD8+ T cells in an immunocompetent host. The complete tumor rejection in an A2AR−/− host (Figs. 2 and 3) or the delay of rapid tumor growth in WT mice by antagonists (Fig. 4) was due to augmentation of effects of CD8+ T cells rather than to effects on some other cells that are unrelated to CD8+ T cell functions. This finding is supported by several lines of evidence. In one of the controls we compared the genetically engineered immunogenic CL8-1 melanoma with the parent cell line, B16 melanoma. The CL8-1 melanoma was established from nonimmunogenic B16 melanoma by increasing expression of H-2Kb MHC class I molecules to increase CL8-1 immunogenicity (30, 41). The growth of CL8-1 in WT mice was delayed compared with growth of B16 cells because of anti-CL8-1 CD8+ T cells (Fig. 2 b and c). In addition, many CD8+ T cells have been observed among infiltrating lymphocytes in CL8-1 tumors, whereas no infiltration of antimelanoma T cells was observed in tumors developed after inoculation of B16 melanoma (30, 41). If the rejection of CL8-1 tumor in A2AR−/− mice (Fig. 2a) was due to A2AR deficiency in cells other than CD8+ T cells or in cells that are unrelated to CD8+ T cell functions, then complete B16 melanoma rejection would be also expected in A2AR−/− mice, because B16 differ from CL8-1 only in the ability to generate antitumor CD8+ T cells. The opposite was found. B16 melanoma was growing equally fast in both WT and A2AR−/− mice, and none of A2AR−/− mice survived B16 inoculation (Fig. 2c).
It is shown that ZM241,385 (or caffeine; data not shown) significantly delayed CL8-1 growth in WT mice, which developed anti-CL8-1 CD8+ T cells (Fig. 4c), but did not affect tumor growth in a control group of nude mice with no anti-CL8-1 CD8+ T cells (data not shown). These control experiments with immunodeficient mice support the view that antitumor effects of antagonist require CD8+ T cells. In addition, the reduction in tumor growth by antagonists in adoptive immunotherapy models has been observed when antagonists were given in combination with anti-CD8+ T cells, but not alone (Fig. 4).
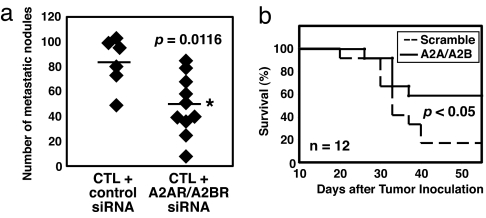
Finally, we found improvement of adoptive immunotherapy when A2AR and A2BR expression in antitumor CD8+ T cells was specifically blocked by siRNA pretreatment before their adoptive transfer (Fig. 6). The pretreatment of antitumor T cells with A2AR and A2BR siRNA reduced CMS4 lung metastasis from 83 to 49 (P = 0.0116) and also improved survival of RMA-inoculated mice (control, 2/12; A2AR/A2BR, 7/12; P < 0.05), suggesting that, indeed, the A2AR expressed on antitumor CD8+ T cells play an inhibitory role during attack on tumor. Taken together, these controls also provide genetic evidence for the critical role of A2AR in regulation of effector functions of antigen-specific CD8+ T cells in vivo and, possibly, in control of T cell-mediated autoimmunity.
Fig. 6.
Suppression of A2AR/A2BR expression in T cells improved adoptive immunotherapy. (a) siRNA against A2AR and A2BR was transfected into anti-CMS4 CD8+ T cells before adoptive transfer (see Supporting Text). Lung metastasis was examined 11 days after injection of T cells (1 × 106 cells per mouse) as described in Methods. T cell-specific knockdown of A2AR/A2BR facilitated inhibition of lung metastasis by antitumor T cells (∗, P = 0.0116 by ANOVA). (b) Survival of RMA tumor-bearing WT mice was improved by the transfer of A2AR/A2BR siRNA-pretreated T cells (P < 0.05 by log-rank test). Anti-RMA T cells were obtained from WT mice immunized with RMA tumor cells. Unseparated spleen and lymph node cells (5 × 107) were transfected with either control or A2AR and A2BR siRNA and injected into tumor-bearing mice 10 days after inoculation of RMA cells (2 × 105).
Discussion
The data presented suggest that antitumor T cells are inhibited by tumor-produced extracellular adenosine because of the A2AR-triggered elevation of intracellular levels of cAMP. Increase of intracellular cAMP induces protein kinase A-mediated phosphorylation and activation of COOH-terminal Src kinase (Csk). Csk then may phosphorylate and inhibit Lck, which, in turn, diminishes TCR signaling and IFN-γ production (22). Recent studies of CD26 (adenosine deaminase) (42) support our hypothesis that a decrease in adenosine signaling is immunoenhancing. Among the CD8+ T cell responses that could be inhibited by A2AR/A2BR are proliferation (16), lethal hit delivery (12, 43), Fas ligand up-regulation (24), and production of cytokines such as IFN-γ (17, 44). IFN-γ has been demonstrated to play an important role in antitumor effects of CD8+ T cells because of inhibition of tumor angiogenesis (8). The data presented suggest a combined therapy in which the antineovascularization approach (45) could be complemented by the A2AR/A2BR-targeting strategy described here to deinhibit and therefore enhance IFN-γ production by antitumor T cells.
We interpret our data as (i) evidence for the major role of A2AR in cancerous tissue protection from antitumor T cells and (ii) demonstration of the feasibility of the strategy to enhance the immune-mediated tumor destruction by genetic deletion or pharmacological antagonism of A2AR and possibly A2BR. These observations also suggest future studies to establish whether A2AR may be involved as a primary trigger (17, 44) of expression of other tumor-protecting immunosuppressive molecules (37). The proposed strategy to counteract immunosuppressive signaling by adenosine near solid tumors is complementary to other approaches directed to improve the development and function of antitumor T cells (4, 10, 11, 14).
The limitation of this approach is that it is applicable only to immunogenic tumors (Fig. 2c). In addition, this strategy so far resulted in complete tumor rejection in only ≈60% of mice with genetically targeted A2AR; antagonists caused significant, but not complete, tumor growth retardation. The tumors’ escape from CD8+ T cells observed in ≈40% of A2AR−/− mice (Figs. 2 and 3) was not due to the loss of antigen-presenting molecules (data not shown) but could be explained by the tumor-protecting A2BR, which could be expressed in the absence of A2AR on A2AR−/− CD8+ T cells (Fig. 1c and Supporting Text). Activated A2BR may inhibit CD8+ T cells in the adenosine-rich tumor microenvironment, and both A2AR and A2BR are expressed on some antitumor CD8+ T cells (Fig. 1c). It remains to be determined whether A2BR may account for CD8+ T cell failure to destroy tumors in the 40% A2AR−/− mice that failed to reject tumors (Figs. 2 and 3) and whether even better tumor rejection by CD8+ T cells could be accomplished by inactivation of both A2AR and A2BR in antitumor T cells. It is also important to carefully consider the known cardiovascular and neurological (35) [as well as possible proinflammatory (17, 18, 44)] effects of A2AR and A2BR antagonists, including caffeine, as well as the “effect inversion” observed when comparing acute versus chronic administration of caffeine (17, 35, 46).
Further studies of spontaneous immunogenic tumors may determine whether A2 adenosine receptors also account for the failure of T cells to destroy spontaneously arising tumors at early stages. We propose to target the hypoxia→extracellular adenosine→A2AR/A2BR signaling pathway as a cancer immunotherapy strategy to prevent the inhibition of antitumor T cells in the tumor microenvironment. The same strategy may prevent the premature termination of immune response and improve the vaccine-induced development of antitumor and antiviral T cells.
Methods
Induction of Tumor-Specific Cytotoxic T Cells.
Anti-CMS4 sarcoma CD8+ T cells were prepared as described previously (38). CMS4-specific CD8+ T cells (1 × 106) were expanded by stimulating with 5 × 105 irradiated CMS4 cells in the presence of 5 × 106 BALB/c spleen cells and IL-2. Anti-LCMV gp33 CD8+ T cells were prepared from LCMV33–41 peptide-specific 318 T cell receptor transgenic mice as described in Fig. 11. cAMP accumulation in these cells was measured as described in Supporting Text (26).
Studies of Rejection of Tumors by Endogenous CD8+ T Cells in A2AR−/− Mice.
CL8-1 melanoma clone was isolated after transfection of B16BL6 melanoma clone BL6-8 with the H-2Kb gene to increase immunogenicity (30, 41). No progressively growing tumors were detected after s.c. inoculation of 1 × 104 to 2 × 105 CL8-1 cells in immunocompetent C57BL/6 mice. The antitumor resistance in C57BL/6 mice can be overcome by inoculating a higher dose of CL8-1 (e.g., 1–3 × 106) cells. With the same reason, RMA T lymphoma cells that express the H-2Kb molecule were inoculated at 2 × 105 cells to overcome antitumor resistance in C57BL/6 mice. Tumor cells were washed and suspended in PBS and injected s.c. (100 μl per mouse). Perpendicular tumor diameters were measured and tumor volumes were calculated according to the formula a2 × b × 0.52, where a is the smaller and b is the larger tumor diameter (31). The experiment was terminated when tumors reached 2.0 cm in diameter or became ulcerated. Animal experiments were performed according to the protocol approved by the institutional animal care and use committees of the University of Pittsburgh and the National Institute of Allergy and Infectious Diseases.
Effects of Adenosine Receptor Antagonists on s.c. Tumor Growth.
CL8-1 cells (1.3 × 106) were injected s.c. into C57BL/6 mice. When tumors reached ≈8 mm in diameter mice were divided randomly into groups of 10 mice with similar tumor size (≈200 mm3; CL8-1 tumors reached this size around day 28 in C57BL/6 mice).
ZM241,385 (Tocris, Ellisville, MO) treatment was done by daily i.p. injections of 0.2 mg per mouse per day. Caffeine (Sigma, St. Louis, MO) was given as drinking water (0.1% wt/vol). The effects of these antagonists in vivo serve only as an indication that either individual A2AR or A2BR (23, 40) or both are involved in down-regulation of antitumor CD8+ T cells in vivo. In control assays of ex vivo serum from antagonist-treated mice (Fig. 12 and data not shown) we confirmed that, during treatment, the initial in vivo levels of ZM241,385 and caffeine in serum are sufficiently high to prevent (antagonize) the adenosine→A2AR-induced cAMP accumulation in cells.
Effects of Adenosine Receptor Antagonists on Lung Metastasis.
CMS4 sarcoma cells were injected i.v. into the lateral tail vein of BALB/c mice (2.5 × 105 cells in 100 μl total volume). Ten days later (4 days after in vitro stimulation), therapeutic CD8+ T cells were injected i.v (38). Treatment with ZM241,385 or caffeine started on the day of adoptive transfer. One to 2 weeks after adoptive transfer, the lungs were removed and processed for enumeration of metastasis. Lungs were inflated with a 15% solution of india ink, resected, and fixed in Fekete’s solution. The number of pulmonary nodules was enumerated under a dissecting microscope in blind tests.
Statistics.
The statistical differences between survival of mice in WT versus A2AR−/− mice were calculated according to the log-rank test. The statistical differences in the size of tumors were calculated by using the Student t test. For evaluation of the lung metastasis experiment, the more relevant Mann–Whitney test or ANOVA was used, because the lung metastasis may not be normally distributed.
Supplementary Material
Acknowledgments
We thank Drs. William Paul, Ronald Germain, Michael Lenardo, and Ronald Schwartz (National Institute of Allergy and Infectious Diseases) and Steven Rosenberg and Alfred Singer (National Cancer Institute, National Institutes of Health) for support, discussions, and help and Dr. Jane Kinsel and Brenda Marshall for help in preparation of the manuscript. M.S. was supported by an Intramural National Institutes of Health Program (National Institute of Allergy and Infectious Diseases) and then by National Institutes of Health Extramural Grant 1 R01 CA 112561 1-NIH. S.J.P. and F.R. were supported by grants from the Health Research Council and the Cancer Society of New Zealand. This research was supported in part by the Intramural Research Program of the National Institutes of Health (National Cancer Institute, Center for Cancer Research).
Abbreviations:
- A2AR
A2A adenosine receptor
- A2BR
A2B adenosine receptor.
Footnotes
Conflict of interest statement: No conflicts declared.
References
- 1.Hellstrom I., Hellstrom K. E., Pierce G. E. Int. J. Cancer. 1968;3:467–482. doi: 10.1002/ijc.2910030408. [DOI] [PubMed] [Google Scholar]
- 2.Hanson H. L., Donermeyer D. L., Ikeda H., White J. M., Shankaran V., Old L. J., Shiku H., Schreiber R. D., Allen P. M. Immunity. 2000;13:265–276. doi: 10.1016/s1074-7613(00)00026-1. [DOI] [PubMed] [Google Scholar]
- 3.Rosenberg S. A. J. Intern. Med. 2001;250:462–475. doi: 10.1046/j.1365-2796.2001.00911.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pardoll D., Allison J. Nat. Med. 2004:887–92. doi: 10.1038/nm0904-887. [DOI] [PubMed] [Google Scholar]
- 5.Shankaran V., Ikeda H., Bruce A. T., White J. M., Swanson P. E., Old L. J., Schreiber R. D. Nature. 2001;410:1107–1111. doi: 10.1038/35074122. [DOI] [PubMed] [Google Scholar]
- 6.Rapoport A. P., Stadtmauer E. A., Aqui N., Badros A., Cotte J., Chrisley L., Veloso E., Zheng Z., Westphal S., Mair R., et al. Nat. Med. 2005;11:1230–1237. doi: 10.1038/nm1310. [DOI] [PubMed] [Google Scholar]
- 7.Hahne M., Rimoldi D., Schroter M., Romero P., Schreier M., French L. E., Schneider P., Bornand T., Fontana A., Lienard D., et al. Science. 1996;274:1363–1366. doi: 10.1126/science.274.5291.1363. [DOI] [PubMed] [Google Scholar]
- 8.Qin Z., Blankenstein T. Immunity. 2000;12:677–686. doi: 10.1016/s1074-7613(00)80218-6. [DOI] [PubMed] [Google Scholar]
- 9.Zinkernagel R. M. Int. J. Cancer. 2001;93:1–5. doi: 10.1002/ijc.1305. [DOI] [PubMed] [Google Scholar]
- 10.Sutmuller R. P., van Duivenvoorde L. M., van Elsas A., Schumacher T. N., Wildenberg M. E., Allison J. P., Toes R. E., Offringa R., Melief C. J. J. Exp. Med. 2001;194:823–832. doi: 10.1084/jem.194.6.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dudley M. E., Wunderlich J. R., Robbins P. F., Yang J. C., Hwu P., Schwartzentruber D. J., Topalian S. L., Sherry R., Restifo N. P., Hubicki A. M., et al. Science. 2002;298:850–854. doi: 10.1126/science.1076514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pardoll D. Proc. Natl. Acad. Sci. USA. 2002;99:15840–15842. doi: 10.1073/pnas.262669499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Overwijk W. W., Lee D. S., Surman D. R., Irvine K. R., Touloukian C. E., Chan C. C., Carroll M. W., Moss B., Rosenberg S. A., Restifo N. P. Proc. Natl. Acad. Sci. USA. 1999;96:2982–2987. doi: 10.1073/pnas.96.6.2982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phan G. Q., Yang J. C., Sherry R. M., Hwu P., Topalian S. L., Schwartzentruber D. J., Restifo N. P., Haworth L. R., Seipp C. A., Freezer L. J., et al. Proc. Natl. Acad. Sci. USA. 2003;100:8372–8377. doi: 10.1073/pnas.1533209100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Takayama H., Trenn G., Sitkovsky M. V. J. Biol. Chem. 1988;263:2330–2336. [PubMed] [Google Scholar]
- 16.Huang S., Koshiba M., Apasov S., Sitkovsky M. Blood. 1997;90:1600–1610. [PubMed] [Google Scholar]
- 17.Sitkovsky M. V., Lukashev D., Apasov S., Kojima H., Koshiba M., Caldwell C., Ohta A., Thiel M. Annu. Rev. Immunol. 2004;22:657–682. doi: 10.1146/annurev.immunol.22.012703.104731. [DOI] [PubMed] [Google Scholar]
- 18.Ohta A., Sitkovsky M. Nature. 2001;414:916–920. doi: 10.1038/414916a. [DOI] [PubMed] [Google Scholar]
- 19.Harris A. L. Nat. Rev. Cancer. 2002;2:38–47. doi: 10.1038/nrc704. [DOI] [PubMed] [Google Scholar]
- 20.Giatromanolaki A., Sivridis E., Kouskoukis C., Gatter K. C., Harris A. L., Koukourakis M. I. Melanoma Res. 2003;13:493–501. doi: 10.1097/00008390-200310000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Decking U. K., Schlieper G., Kroll K., Schrader J. Circ. Res. 1997;81:154–164. doi: 10.1161/01.res.81.2.154. [DOI] [PubMed] [Google Scholar]
- 22.Torgersen K. M., Vang T., Abrahamsen H., Yaqub S., Tasken K. Cell. Signalling. 2002;14:1–9. doi: 10.1016/s0898-6568(01)00214-5. [DOI] [PubMed] [Google Scholar]
- 23.Fredholm B. B., Ijzerman A. P., Jacobson K. A., Klotz K.-N., Linden J. Pharmacol. Rev. 2001;53:527–552. [PMC free article] [PubMed] [Google Scholar]
- 24.Koshiba M., Kojima H., Huang S., Apasov S., Sitkovsky M. V. J. Biol. Chem. 1997;272:25881–25889. doi: 10.1074/jbc.272.41.25881. [DOI] [PubMed] [Google Scholar]
- 25.Armstrong J. M., Chen J. F., Schwarzschild M. A., Apasov S., Smith P. T., Caldwell C., Chen P., Figler H., Sullivan G., Fink S., et al. Biochem. J. 2001;354:123–130. doi: 10.1042/0264-6021:3540123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Apasov S. G., Chen J. F., Smith P. T., Schwarzschild M. A., Fink J. S., Sitkovsky M. V. Br. J. Pharmacol. 2000;131:43–50. doi: 10.1038/sj.bjp.0703532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blay J., White T. D., Hoskin D. W. Cancer Res. 1997;57:2602–2605. [PubMed] [Google Scholar]
- 28.Hoskin D. W., Butler J. J., Drapeau D., Haeryfar S. M., Blay J. Int. J. Cancer. 2002;99:386–395. doi: 10.1002/ijc.10325. [DOI] [PubMed] [Google Scholar]
- 29.Jackson E. K., Dubey R. K. Am. J. Physiol. 2001;281:F597–F612. doi: 10.1152/ajprenal.2001.281.4.F597. [DOI] [PubMed] [Google Scholar]
- 30.Itoh T., Storkus W. J., Gorelik E., Lotze M. T. J. Immunol. 1994;153:1202–1215. [PubMed] [Google Scholar]
- 31.Huang X., Wong M. K., Yi H., Watkins S., Laird A. D., Wolf S. F., Gorelik E. Cancer Res. 2002;62:5727–5735. [PubMed] [Google Scholar]
- 32.van Hall T., van Bergen J., van Veelen P. A., Kraakman M., Heukamp L. C., Koning F., Melief C. J., Ossendorp F., Offringa R. J. Immunol. 2000;165:869–877. doi: 10.4049/jimmunol.165.2.869. [DOI] [PubMed] [Google Scholar]
- 33.Linden J. Annu. Rev. Pharmacol. Toxicol. 2001;41:775–787. doi: 10.1146/annurev.pharmtox.41.1.775. [DOI] [PubMed] [Google Scholar]
- 34.Ji X.-D., Jacobson K. A. Drug Des. Discovery. 1999;16:217–226. [PMC free article] [PubMed] [Google Scholar]
- 35.Fredholm B. B., Battig K., Holmen J., Nehlig A., Zvartau E. E. Pharmacol. Rev. 1999;51:83–133. [PubMed] [Google Scholar]
- 36.Pircher H., Burki K., Lang R., Hengartner H., Zinkernagel R. M. Nature. 1989;342:559–561. doi: 10.1038/342559a0. [DOI] [PubMed] [Google Scholar]
- 37.Prevost-Blondel A., Zimmermann C., Stemmer C., Kulmburg P., Rosenthal F. M., Pircher H. J. Immunol. 1998;161:2187–2194. [PubMed] [Google Scholar]
- 38.Ryan M. H., Bristol J. A., McDuffie E., Abrams S. I. J. Immunol. 2001;167:4286–4292. doi: 10.4049/jimmunol.167.8.4286. [DOI] [PubMed] [Google Scholar]
- 39.Kemp R. A., Ronchese F. J. Immunol. 2001;167:6497–6502. doi: 10.4049/jimmunol.167.11.6497. [DOI] [PubMed] [Google Scholar]
- 40.Fredholm B. B. Pharmacol. Toxicol. 1995;76:93–101. doi: 10.1111/j.1600-0773.1995.tb00111.x. [DOI] [PubMed] [Google Scholar]
- 41.Tanaka K., Gorelik E., Watanabe M., Hozumi N., Jay G. Mol. Cell. Biol. 1988;8:1857–1861. doi: 10.1128/mcb.8.4.1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pacheco R., Martinez-Navio J. M., Lejeune M., Climent N., Oliva H., Gatell J. M., Gallart T., Mallol J., Lluis C., Franco R. Proc. Natl. Acad. Sci. USA. 2005;102:9583–9588. doi: 10.1073/pnas.0501050102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kagi D., Ledermann B., Burki K., Seiler P., Odermatt B., Olsen K. J., Podack E. R., Zinkernagel R. M., Hengartner H. Nature. 1994;369:31–37. doi: 10.1038/369031a0. [DOI] [PubMed] [Google Scholar]
- 44.Sitkovsky M. V. Biochem. Pharmacol. 2003;65:493–501. doi: 10.1016/s0006-2952(02)01548-4. [DOI] [PubMed] [Google Scholar]
- 45.Folkman J. Semin. Cancer Biol. 2003;13:159–167. doi: 10.1016/s1044-579x(02)00133-5. [DOI] [PubMed] [Google Scholar]
- 46.Jacobson K. A., von Lubitz D. K., Daly J. W., Fredholm B. B. Trends Pharmacol. Sci. 1996;17:108–113. doi: 10.1016/0165-6147(96)10002-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.