Abstract
With more clinical trials involving evaluations of new drugs or vaccines, monitoring for early detection of adverse events is essential. The overall goal of this study was to develop an interactive-computer system using cell phones for real-time collection and transmission of adverse events related to metronidazole administration among female sex workers (FSW) in Peru. We developed an application for cell phones in Spanish, called Cell-PREVEN, based on a system from Voxiva Inc. We used cell phones to enter data collected by interviewers from FSW in three communities. Information was stored in an online database, where it could be immediately accessed worldwide and exported over a secure Internet connection. E-mail and text messages sent to mobile devices alerted key personnel to selected symptoms. This pilot project has demonstrated that it is feasible to develop a public-health-surveillance system based on cell phones to collect data in real-time in Peru (http://www.prevenperu.org).
INTRODUCTION
Early detection and treatment of sexually transmitted diseases (STD) represents one major strategy for preventing transmission of STD, including infection with HIV1. In a national survey conducted in 2002, the prevalence of STD and bacterial vaginosis of FSW in Peru was 26% and 34% respectively2. Early detection of STD in FSWs, as well as promoting and providing condoms for commercial sex workers, are needed to prevent HIV/STD in Peru, as in much of the developing world1. New technologies and information systems can help programs and trials not only in STD/HIV, but in other fields of public health involving prevention, surveillance, and management of data.
Cell-PREVEN is part of large randomized trial in Peru in 20 cities called PREVEN which seeks to lower STD rates in Peru. PREVEN2 is a collaborative effort between the Universidad Peruana Cayetano Heredia (Peru), Imperial College (London) and the University of Washington (Seattle), in collaboration with Peru’s Ministry of Health.
One of the components of the intervention used in PREVEN includes using mobile teams to reach marginalized FSW. The mobile team is comprised of a health worker and a peer educator and performs on-site screening and treatment of STD, promotion of STD services, and promotion of condom use. The mobile team visits each identified sex venue every eight weeks to conduct STD screening, offer presumptive treatment of bacterial vaginosis with metronidazole, and treat other STDs diagnosed by the screening. One week after they provide treatment, the mobile team returns to the participants and asks for any adverse events. An adverse event is any untoward medical occurrence (e.g., vomiting, diarrhea) in a patient administered a medicinal product.
The PREVEN project registered expected and unexpected adverse events produced within the first week of treatment with metronidazole. Many times, identifying a medication as the cause of an adverse event can often be difficult and uncertain.
It’s important for public health workers to monitor adverse effects of metronidazole in female sex workers so the women won’t abandon the medicine. Failing to take metronidazole is a risk factor for co-infection with other STDs and could be a factor to not participate in the mobile team activities.
Before Cell-PREVEN, reports were collected on paper. Weeks or months could pass before public health workers, physicians, and team leaders learned of trends and patterns and were able to respond. Cell phones were chosen for this project because they are widely used in many developing countries, and they can collect data electronically even in remote settings. In Peru, the market for cell phones has been increasing since 1993, with major growth from about 200,000 sales in 1996 to 2.5 million sales by mid-20033.
Cell phones are ideal tools for a mobile team and the equipment is less likely to be stolen compared with laptops or personal digital assistants (PDAs). Cell phones don’t stick out in the field because from an outside observer, it looks like a health worker is just making a phone call. Computers and personal digital assistants are also limited in developing countries because of their expense and requirement for additional equipment.
Review of the literature
Applications involving the phone and the Internet have been described previously in literature.
For example, Voxiva developed Alerta, a system that involves the phone and the Internet for communication and disease surveillance. Alerta4 was piloted initially in health clinics of the Ministry of Health in Peru, and later in October, 2002, Alerta was implemented in the Peruvian Navy. Lescano et al.5 reported that the introduction of Alerta has led to early outbreak identification/response, timely case management, and increased review of clinical procedures within reporting units. They concluded that Alerta represented a fully functional alternative for cost-effective real-time disease surveillance.
In the developing world, similar systems using the Voxiva platform for health solutions have been deployed in Latin America, Africa, Iraq, and India. For example, in Africa, Voxiva created a national HIV/AIDS information system for eight countries that monitors current data for national and global reporting requirements, and manages the use of antiretrovirals to reduce the spread of viral resistance. In India, Voxiva created, within a month, a surveillance system for Japanese encephalitis4.
In South Africa, the project Cell Life6 is using cell phones to monitor adherence for the management of HIV/AIDS in patients on antiretroviral therapy. Some of the platforms Cell Life is using include a global system for mobile communications (GSM), wireless Internet gateway (WIG), and a geographical information system (GIS) database.
Karras et al.7 reported that a Java-enabled wireless phone could be potentially used in disaster response and public health informatics. They emphasized that the technology was inherently deployable, portable and that minimal orientation to new hardware was needed since everyone was comfortable with entering numbers on a phone keypad and pushing the send button.
Objective
The overall goal of this study was to develop an interactive-computer system using cell phones and the Internet for real-time collection and transmission of adverse events related with metronidazole administration as presumptive treatment for vaginosis among FSW in Peru.
METHODS
Design of Cell-PREVEN
Cell-PREVEN is a system that combines the phone and the Internet to create a real-time surveillance system of adverse events as a component of the PREVEN Project.
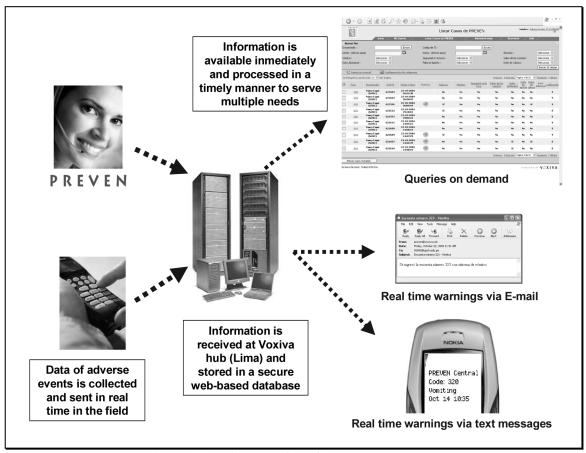
We developed an interactive voice response application for cell phones in Spanish, based on a system from Voxiva Inc, a telecommunications company based in Peru8. The architecture of the system has five elements: a central database and Web server; remote access to the database from any Internet-connected computer; telephone audio computer-assisted personal interviewing; voice messages and short-message service (SMS)-based communications to and from the server via cell phones (Figure 1).
Figure 1.
Architecture of the Cell-PREVEN system
Implementation of Cell-PREVEN
Public health workers received an account number, personal identification number (PIN), and a plastic card with simple instructions and codes for all the symptoms they need to report. By calling into a number in Lima using cell phones they could access the system and report adverse events from FSW systematically and in real-time in urban and rural areas.
We piloted the system in three cities of Peru: Chincha, Huanuco, and Piura. The system was incorporated in the mobile team activity of the PREVEN Project. Six public health workers were trained by one of the authors (W.H.C.) in the use of cell phones before we started the project. The report by cell phones contained the same questions as on the paper form.
The workshops consisted in two parts. The first part was a 30-minute lecture about the overview of the project, and an audio-demo of the system. The second part was a “hands-on” lesson with cell phones using different case studies and role playing. We provided a manual and a “hands-free” set for all the interviewers. The training sessions lasted about three hours for nurses and midwives and four hours for the peer educators.
Data collection and transmission of adverse events began in early September 2004.
Authorized users logged on to the system using a cell phone and followed instructions on a wallet-sized card, or a simple prompted menu, and entered digital information about participants with adverse events. The health workers could attach additional information in voice files.
Information was stored in an online database and could be immediately accessed worldwide and exported over a secure Internet connection. Safeguarding the privacy, confidentiality, and security of any public health informatics or e-health project is an important undertaking9. Our project does not collect the names in the database and uses only code numbers. Each time the health worker wants to make a report they have to enter a login, a password, and the specific code number of the participant.
Team leaders could receive the information immediately via the Internet, analyze the data, and use the system’s communication and messaging tools to respond. Team leaders could monitor incoming reports through a Web interface. Individual adverse event reports arrived in real-time with full-case details. Authorized users could also listen to voice files recorded by the remote health workers. Data were available immediately, and team leaders could export data to various programs for analysis and presentation.
Designated users received automatic notification of selected symptoms via e-mail and SMS messages. Team leaders could communicate with remote health professionals using voice mails as well as e-mails. The system was operational 24 hours a day, seven days a week.
RESULTS
During September–December 2004, the system collected 797 reports, of which 60 (7.5%) were reports of at least one adverse event (registered via voice file in the database). The distribution of reports per city is summarized in Table 1.
Table 1.
Number of reports successfully transmitted with the cell phones
| City | Positive reports | Negative reports | Total number of reports |
|---|---|---|---|
| Chincha | 2 | 199 | 201 |
| Huanuco | 31 | 188 | 219 |
| Piura | 71 | 306 | 377 |
| Total | 104 | 693 | 797 |
Positive report: At least one adverse event reported (spontaneously recalled)
Negative report: No adverse event reported
Overall, 374 adverse events were registered in the database. The most frequent was headache, reported by 105 participants. Second was nausea, reported by 77 participants. Third was dysgeusia (metallic taste), reported by 67 participants.
The system sent a total of 30 SMS alerts to cell phones and e-mail messages to the team leaders. These messages reported vomiting, the most serious adverse event reported (Table 2).
Table 2.
Number of SMS sent by the system to the team leaders
| No. of SMS by city | No | |||
|---|---|---|---|---|
| SMS | Chincha | Huanuco | Piura | Total |
| Vomiting | 0 | 8 | 22 | 30 |
DISCUSSION
The Cell-PREVEN system addresses three key ingredients of an effective surveillance system: a) Real-time data collection from health workers reporting an adverse event, or from a doctor reporting a disease outbreak; b) rapid analyses of data to make opportune decisions and rapid allocation of resources; and c) communications back to the field to coordinate response.
Real-time information is important for many reasons. For one, the health worker can give the sex worker immediate feedback from a doctor. Second, the health worker can track the history of a sex worker and modify the type of counseling he or she offers based on such information as past adverse events. Third, real-time eliminates the need for the health worker to carry lots of paper that not only might get misplaced but requires more time to enter and could increase data entry error.
Additional requirements for authentication may be required in the United States under HIPAA (Health Insurance Portability & Accountability Act), for example media access control address (MAC address) for wireless devices or internal serial number of registered telephones as proof of authentication.
The data collected during the time period did not modify the protocol in the three cities of the PREVEN trial, but the cell-phone system allows health care workers in remote settings to know whether a patient registered previous adverse events. The health worker might, then, provide counseling on how to prevent another adverse event, i.e., avoid alcohol. Side effects produced by metronidazole could get worse if FSW consumes alcohol. This is a relatively common practice by some FSW since they work in bars and nights clubs as a way to earn more money. FSW can earn 10% of the alcohol consumed by their clients10.
LESSONS LEARNED FROM THE PILOT STUDY
The lessons learned with the Cell-PREVEN pilot study are still evolving but include the following:
Even in a challenging social setting with limited wired infrastructure, it is possible to develop an effective surveillance system using cell phones. We used a low-tech system to create a sophisticated solution.
The infrastructure provided by Voxiva was significant. Partnership is key to overcoming technology barriers. We can attract top-tier industry partners if we have a comprehensive public health initiative. Public-private partnerships can increase access of developing countries to improved health technologies.
The system is applicable to a range of health problems -- from reporting and monitoring adverse events during clinical trials, or vaccination campaigns to reporting disease outbreaks. For example, real-time information of serious adverse events can potentially lead protocol modifications in clinical trials11. Another application can be monitoring certain adverse events in cases of bioterrorism. We can even apply the system to nonhealth settings -- for example, in reporting crime, or tracking commercial orders and distribution.
Training is one of the key factors in the success of this project. We customized training in each city; some cities received longer training than others.
CONCLUSION
This pilot project has demonstrated that cell phones are a feasible means of collecting and reporting data in real time in remote communities of Peru. The project shows that it's not necessary to have the latest Palm Pilot or Tablet PC to create a sophisticated public health surveillance system. Given the right technology partner, you can build a surveillance system using cell phones.
NEXT STEPS
We are monitoring the project by e-mail, chat, and phones. For updates, please refer to the Web site of the cell phone project: http://www.prevenperu.org
We plan to perform an evaluation of the system, including a satisfaction survey of the health professionals who reported adverse events by cell phones. We plan to compare the satisfaction of this group with the satisfaction of interviewers who report via a paper-based system. Additionally, we plan to perform a cost-benefit analysis. Based on the results of the pilot, we plan to modify the system and further implement it to other cities in Peru.
Acknowledgements
Special thanks: To Voxiva, Inc., especially Pamela Johnson, Francisco Rubio and Ernesto Gozzer for technical assistance; to the mobile team personnel for their hard work and enthusiasm; and to Bobbi Nodell for valuable suggestions to the manuscript.
Footnotes
This research was supported in part by the University of Washington International Training in Medical Informatics, a Fogarty International Center/NIH-funded grant (D43TW001286-04S1); the University of Washington Center for AIDS Research (CFAR), an NIH funded program (P30 AI27757), The Wellcome Trust Foundation (059131/Z/99/Z) and Voxiva, Inc.
Contact information:
Dr. Walter H. Curioso
E-mail: wcurioso@u.washington.edu
Web: http://www.prevenperu.org
UW Biomedical and Health Informatics, Public Health Informatics: http://phig.washington.edu
REFERENCES
- 1.Sanchez J, Campos PE, Courtois B, et al. Prevention of sexually transmitted diseases (STDs) in female sex workers: prospective evaluation of condom promotion and strengthened STD services. . Sex Transm Dis. 2003 Apr;30(4):273–279. doi: 10.1097/00007435-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 2.PREVEN. Urban Community Randomized Trial of STD Prevention. Universidad Peruana Cayetano Heredia, Lima, Peru. Available at: http://www.upch.edu.pe/faspa/preven/ (In Spanish) Accessed: July 1, 2005.
- 3.ONGEI. Peru: The use of information and communication technologies. Available at: http://www.pcm.gob.pe/portal_ongei/publica/indicadores/Lib0365/Libro.pdf (In Spanish) Accessed: July 1, 2005.
- 4.Prahalad C. The Voxiva Story. The Fortune at the Bottom of the Pyramid: Eradicating Poverty Through Profits First printing ed. New Jersey: Wharton School Publishing; 2005:361–379.
- 5.Lescano A, Ortiz M, Elgegren R, et al. Alerta DISAMAR: Innovative disease surveillance in Peru. Paper presented at: Annual Meeting of the American Society of Tropical Medicine and Hygiene Philadelphia, 2003.
- 6.Cell-Life. The Cell-Life Solution. Available at: http://www.cell-life.org/ Accessed: March 1, 2005.
- 7.Karras BT, Huq SH, Bliss D, Lober WB. National Pharmaceutical Stockpile drill analysis using XML data collection on wireless Java phones. Proc AMIA Symp. 2002:365–391. [PMC free article] [PubMed] [Google Scholar]
- 8.Voxiva. Available at: http://www.voxiva.net/ Accessed: July 1, 2005.
- 9.O'Carroll PW, Yasnoff WA, Ward E, Ripp L, Martin E. Public Health Informatics and Information Systems New York: Springer-Verlag New York, Inc.; 2002.
- 10.Segura PM, 2004. Evaluation of the characteristics and infection status of female sex workers participating in an STI/HIV mobile prevention team outreach program. Master of Public Health Thesis, School of Public Health, University of Washington, Seattle, Washington.
- 11.Liauw WS, Day RO. Adverse event reporting in clinical trials: room for improvement. Med J Aust. 2003;179(8):426–8. doi: 10.5694/j.1326-5377.2003.tb05621.x. [DOI] [PubMed] [Google Scholar]