Abstract
Computerized drug prescribing alerts can improve patient safety, but are often overridden because of poor specificity and alert overload. We developed a selective knowledge base of only clinically significant drug alerts and designated only critical-high severity alerts to be interruptive to clinician workflow (a tiered approach). Using this approach, we were able to achieve a 67% clinician accept rate for ambulatory computerized prescribing alerts.
Background
Computerized drug prescribing, in which prescribers use computerized applications to enter prescriptions that can be checked by clinical decision support systems, can reduce medication error rates [1]. However, these systems may not be as effective for improving safety if clinicians override clinically important alerts. When the threshold for alerting is set too low, clinicians are inundated with alerts of low clinical significance, leading to high override rates and the potential to override even important alerts [2]. Our aim was to study clinician acceptance of a more selective set of drug alerts in the ambulatory care setting, describe the types of alerts that were most often accepted, and describe reasons clinicians gave for overriding them.
Methods
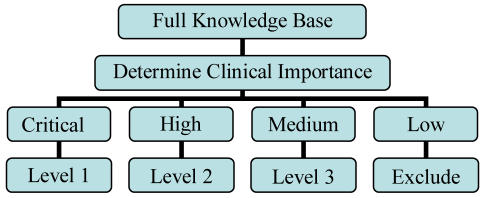
We developed a knowledge base of clinically significant drug alerts using a standardized knowledge base and designated only critical-high severity alerts to be interruptive, where clinicians were required to respond to the alert (a tiered approach). Alerts were presented to clinicians using an electronic medical record with computerized prescribing in 31 Boston-area practices. We collected information on all drug alerts generated over a six-month period and calculated the percentage of alerts that were accepted by clinicians. For alerts that were overridden, we examined in detail clinician reasons for the override.
Results
There were 18,115 drug alerts generated during the study; of these 12,933 (71%) were non-interruptive and 5,182 (29%) were interruptive. Prior to our intervention, all 18,115 alerts would have been interruptive; thus we were able to achieve a substantial decrease in interruptions. Of the 5,182 interruptive alerts, 67% were accepted by clinicians. Clinicians most commonly accepted duplicate drug class alerts (77%) and drug-disease alerts (53%), followed by drug-drug (42%), drug-lab (40%), and drug-pregnancy (10%) contraindication alerts. Reasons for overrides differed for each drug alert category and provided useful information for future drug alert improvement.
Conclusion
Clinician acceptance rates for drug alerts were high when using a knowledge base that had undergone careful clinical review and when workflow interruptions were minimized. These data suggest that it is possible to design computerized prescribing decision support with high rates of alert recommendation acceptance by clinicians.
References
- 1.Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA. 1998;280:1311–1316. doi: 10.1001/jama.280.15.1311. [DOI] [PubMed] [Google Scholar]
- 2.Weingart SN, Toth M, Sands DZ. Physicians’ decision to override computerized drug alerts in primary care. Arch Inter Med. 2003;163:2625–2631. doi: 10.1001/archinte.163.21.2625. [DOI] [PubMed] [Google Scholar]