Abstract
Advanced clinical information systems have been proposed to improve patient care in terms of safety, effectiveness, and efficiency. In order to be effective, such systems require detailed patient-specific clinical information in a form easily reviewed by clinicians. We have developed a patient summary worksheet for use in outpatient clinics, which presents a structured overview of patient health information. The worksheet provides patient demographic information, specific problems and conditions, the patient’s current medication profile, laboratory test results pertinent to patient problems, and disease-specific or preventive care actionable advisories. Usage has grown from a few hundred to over 25,000 unique patients per month during a two-year period. Diabetic patients for whom the worksheet is accessed are significantly more likely to be in compliance with accepted testing regimens for glycosolated hemoglobin (OR 1.47, 95% CI 1.28, 1.61).
INTRODUCTION
Disadvantages of paper-based medical records are well-documented.1–3 Paper based systems are frequently illegible,3 difficult to search,4 fragmented across sites of care, and limited in their ability to provide decision support.5 They are also cumbersome for supporting care coordination, since they cannot be accessed remotely, and are available to only one person at a time.5 Computer-based patient records address the disadvantages of paper records, by providing access to all relevant data from a single location, automated decision support, and facilitating communication within the medical record.
However, overcoming the technical limitations of paper records has not ensured the success or widespread adoption of computerized medical record systems.6 This is in part because such systems have not matched the benefits of paper records.2, 7 Paper records are still used more widely than electronic records because they are simpler to use, have low implementation costs, have more widespread acceptance among clinicians, and fit within the physician workflow.2 The associated disadvantages of computerized records has resulted in unsuccessful implementations, limiting the potential benefits of such systems.8
We propose using paper-based summary reports or worksheets within an electronic medical record to achieve the benefits of a computerized patient record while also maintaining the benefits of a paper-based record. In this paper we analyze the usage of summary worksheets, and their impact on physician performance.
METHODS
At Intermountain Health Care, we have developed a computer-generated patient summary sheet within our existing electronic medical record system. This summary, called the Patient Worksheet, is a one to two-page printed report that contains a structured summary of a patient’s longitudinal health information in the electronic medical record. Clinicians can print the worksheet at the beginning of an outpatient visit, and carry it along with any other paper-based information used during the clinic visit, or access it directly on the computer during the patient encounter.
The worksheet displays patient demographic information, specific problems, allergies and conditions, the patient’s current medication profile, and common laboratory test results. It is thus consistent in content with the Continuity of Care Record (CCR).9 It also contains content directly related to a patient’s problems, such as disease-specific laboratory results and advisories, and other preventive care advisories based on available patient information. We enhanced a diabetes-oriented worksheet to address multiple chronic diseases.10 In its current form, the worksheet has data and disease management advisories for diabetes, heart failure, hypertension, and depression.
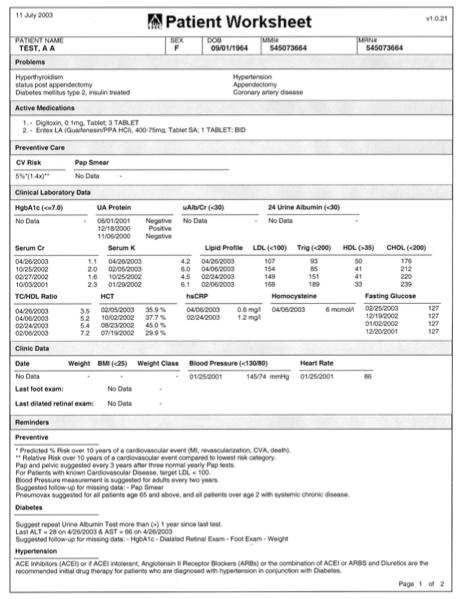
For example, if a patient has diabetes, an instance of the patient worksheet for that patient displays glycosolated hemoglobin (HbA1c) values and lipid profiles, as well as the last recorded foot and dilated retinal exams. It would also list recommendations for treatment based on the data and accepted clinical guidelines; e.g., HbA1c testing recommendations for diabetic patients, or hypertension evaluation recommendations for patients with multiple high blood pressure measurements. Finally, it would list available preventive care data, such as the date of the most recent pap smear, and give reminders for what preventive care tests were due (see Figure 1).
Figure 1.
IHC Patient Worksheet. This is a printed summary sheet used in outpatient clinics, which displays patient health information with disease-specific results and advisories.
The Patient Worksheet was released as a pilot project in late 2002. In early 2003, we incorporated the worksheet in the existing outpatient electronic medical record (EMR) application. We then trained users on-site with our standard clinician training processes, emailed users information about how to use the worksheet, and incorporated training in the standard information systems training at workshops. Total development costs were approximately one person-year.
We have created audit mechanisms to track patient encounters for which the Patient Worksheet is accessed for a patient. These audit data have been collected since the worksheet was first released, and can be used to track the number of times it is used each month. These data were combined with patient clinic visit information from October 2004 to measure the proportion of adult patients per day for whom a worksheet was used in each clinic. In February 2005, we surveyed physicians at one clinic with open-ended questions to understand the various levels of use among physicians, and how the patient worksheet is used within clinics.
To evaluate the impact of the Patient Worksheet on physician performance and patient care, we completed a retrospective cohort study comparing diabetic patients for whom the Patient Worksheet was accessed for a visit with matched controls. We measured compliance with testing protocols for glycosolated hemoglobin, or hemoglobin-A1c (HbA1c) tests, which is our primary indicator for diabetes management. The goal is to improve appropriate use of this indicator, which will lead to improved diabetic control.11
Patients being treated for an ICD-9 250.xx code, where xx indicates a sub-diagnosis of diabetes, were selected from IHC’s outpatient clinic patient population. Study patients were required to have at least one outpatient visit between 10/1/2003 and 12/31/2003. The first outpatient visit during that period was marked as their reference visit. In addition to having a qualifying office visit, study participants had to have at least one HbA1c measurement during the time period 10/1/2002 and 9/30/2003. This measurement served as the patient’s baseline measurement. The patients were divided into two groups (nintervention =2929 and ncontrol =7679) based on whether or not they had a Patient Worksheet printed for their reference visit.
The predictor variables included in the logistic model were Patient Worksheet (Y/N), Age, Gender, Average HbA1c prior to reference visit, and number of HbA1c tests prior to the reference visit. Based on accepted clinical best practices among physicians at IHC, the frequency at which a diabetic patient should be have their HbA1c tested is contingent upon previous test results. Patients that had HbA1c >= 7% on their previous test are due to be tested again within three months. Patients with a HbA1c < 7% should be tested again within six months. The Patient Worksheet calculates whether a patient is due for testing based on the result and date of the most recent HbA1c test in the patient record. If the patient is due, an alert is printed in the Reminders section of the worksheet. The outcome of interest was whether patients due for testing at their reference visit received an HbA1c. The intent of the alert is to keep patients compliant with testing and maintaining HbA1c levels that were shown to reduce risks 50–76% for kidney, nerve, or eye disease.12
To validate the control matching, statistical tests (Chi-square for discrete variables and Student t-tests for continuous variables) were performed to determine whether there were any significant differences between the control and intervention groups at baseline. This analysis showed that patients in the intervention group were tested slightly more often in the year prior to their reference visit (intervention = 2.33, control = 2.28, p = 0.0286) than patients in the control group. While this difference was statistically significant such a small difference in the mean number of HbA1c tests is unlikely to translate into a clinical difference. A potential cause of this difference is improved testing rates due to compliance with reminders on previous instances of the Patient Worksheet for the intervention patients. None of the other covariates were significantly different for the two groups. Multivariate logistic regression controlling for age, sex, and previous testing history was used to evaluate the effectiveness of the intervention in improving adherence to HbA1c testing guidelines.
RESULTS
Patient Worksheet Usage
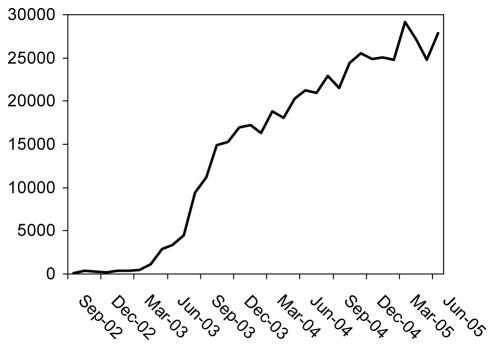
Figure 2 shows the increased use of the Patient Worksheet since its development. Since it was incorporated in the outpatient EMR less than 3 years ago, it has been available to 472 employed physicians in 70 clinics. Its usage has grown from less than 500 patients/month to more than 25,000 patients/month. The number of unique users of the worksheet has grown to over 400 during the same period.
Figure 2.
Patient Worksheet Usage per Month. Through 2005, it has been accessed for over 25,000 patients per month.
During October 2004, the worksheet was used at least once for adult patients in 48 of 92 outpatient clinics. For 7 clinics, it was used for more than 50% of adult patients; at one geriatric clinic, the worksheet was accessed for 87% of patients. Sixteen clinic locations accounted for 90% of all worksheet use, and 5 clinics accounted for 50% of all use. Individual physician use reached 100% for 4 physicians, and was above 80% for 14 physicians.
At some clinics, the patient worksheet has been incorporated in the physician workflow. At the beginning of the day, the worksheet is printed by office staff for all patients scheduled for a physician visit for that day. The worksheet is then attached to the front of the patient chart, or to any paper-based documentation used by the physician. At the end of the visit, the physician either gives the patient the worksheet with indications for self management, or uses the worksheet to complete the visit documentation. When a patient is referred to a specialist, the physician gives the patient a copy of the worksheet to take to the specialist visit.
We surveyed all 7 physicians in one clinic concerning their use of the Patient Worksheet. This clinic used the worksheet for 59% of all adult patients, and was the second highest clinic in total worksheets accessed. In addition, this clinic has implemented a paperless medical record, where all documentation is either entered or scanned in the EMR. Four physicians indicated they use the worksheet for every patient seen, and three openly stated they liked it. Two identified how they use it to track either vital signs or laboratory results for their patients. One indicated he only used it sometimes, but also stated intent to use it more. One physician said he reviews every field, while other physicians use it either for following disease-specific lab values or for reviewing medications and trending blood pressure and weight. One physician who indicated limited use said he does review the reminders specifically. Two physicians requested additional information be added to the worksheet.
Patient Worksheet Impact on HbA1c Testing
Of the 10,608 diabetic patients in the impact study, 5373 (nintervention =1508, ncontrol = 3865) were due for testing at their reference visit. Among the patients due for testing 3800 were tested. This included 1156 patients from the intervention group, and 2644 patients from the control group (see Table 1). A multivariate logistic regression controlling for age, sex, and previous testing history showed that overdue patients in the intervention group odds of being tested at their reference visit were 1.47 (OR =1.47, 95% CI 1.28, 1.61) times the odds of overdue patients in the control group.
Table 1.
HbA1c testing for patients overdue for testing at a visit.
| Tested | Not tested | |
|---|---|---|
| Patient Worksheet used | 1156 (76.7%) | 352 (23.3%) |
| Worksheet not used | 2644 (68.4%) | 1221 (31.6%) |
DISCUSSION
Our results demonstrate that computer-generated patient summaries, such as the Patient Worksheet, can achieve the identified benefits of both computerized and paper-based medical records. The Patient Worksheet provides access to relevant data within a single location, facilitates communication of patient information among providers, and provides automated decision support. The worksheet has significantly improved physician performance in disease management for diabetes; patients were nearly 50% more likely to be tested when they were overdue for the testing. At the same time, the worksheet has a low development and implementation cost, is simple to use for physicians, has widespread acceptance, and fits within the physician workflow. It has high use in both paper-dependent and paperless clinics. It has been one of the most rapidly accepted components of our EMR application.
Our use and investigation of printed summaries from an EMR is not unique. Thomas et al. compared printed patient summaries with palm-based computers, and found that the user acceptance was equivalent for providing access to data during hospital rounds.13 Our study, however, is novel in its demonstration of the rapid acceptance of printed summaries among outpatient physicians and in its impact on patient care.
Findings that the Patient Worksheet would increase compliance with care process models is consistent with findings by Casalino et al. in their evaluation of the association among information technology and the adoption of care process models.14 They identified six components of clinical information technology that influenced care process models: standardized problem list, progress notes, medications prescribed, medication ordering reminders, laboratory results, and radiology results. The worksheet includes 4 of 6 components identified.
Our evaluation is limited by the fact that use of the worksheet was not randomized among physicians. All the physicians received the same training on the system, and had the same access to the worksheet within the EMR, but physicians individually chose to use it or not. In this environment we were able to assess the acceptance of the application within a simple implementation. However, there may be confounders in the evaluation of impact; while we controlled for age, sex, and previous testing history, we were unable to control for physician preference for the worksheet. It is possible that the physicians who preferred to use the worksheet were just better in testing for HbA1c. This finding itself would be important, and would indicate at least a perceived value of the worksheet by higher-performing physicians.
Our analysis was also limited by the measure of worksheet use through audit logs rather than direct observation. Worksheets accessed within the system were counted as “used,” even if the printed worksheet was not actually used by the physician during the office visit. However, this bias should only underestimate the effect of the worksheet.
It is important to note that the Patient Worksheet was not the only initiative at IHC to improve HbA1c testing and diabetes management. This effort was one component of a quality improvement initiative for diabetes management.11 We have adopted a multi-faceted approach to chronic disease management similar to Wagner’s Chronic Care Model.15, 16 Administrative and clinical management teams at IHC actively lead quality improvement initiatives throughout the organization. Organized groups of clinical experts and opinion leaders are paid to review current research and define appropriate clinical practice guidelines and initiatives for the organization.11 These groups agree upon targeted standards of care and methods to measure adherence to these standards. The adherence to and the outcomes from the guidelines are routinely reviewed by the clinical leadership, and adjustments are made to adjust processes necessary to improve outcomes.17 These practice guidelines are communicated by clinical leaders during interactive educational workshops. We facilitate adherence to the guidelines through reminders, alerts and suggestions within the electronic health record, and produce quarterly performance feedback to individuals and groups of providers.18 The reminders on the Patient Worksheet are one way these alerts are delivered. This quality improvement initiative focused on improving outcomes rather than analyzing the particular effect of each component. Even though this study evaluated the specific contribution of the worksheet, it should not be assumed that the effect in this study would be observed if the worksheet were implemented independently of this initiative. For example, the worksheet has other alerts for disease management that are not yet part of an institutional quality improvement initiative, where there was no observed effect of the worksheet. Preliminary analysis of the impact of an alert within the Patient Worksheet for managing hypertension showed no significant difference in blood pressure measurements between patients for whom the worksheet was accessed or not. However, this finding may be related to findings by Murray et al., who observed that computer-based interventions did not improve treatment for uncomplicated hypertension.19
CONCLUSION
Computer-generated patient summary worksheets are easily adopted by clinicians, and can improve physician performance in adhering to accepted standards of care for chronic disease management.
ACKNOWLEDGMENTS
This study was supported by a grant from the John A. Hartford Foundation.
References
- 1.Dick R, Steen E, editors. The computer-based patient record: An essential technology for health care. Washington, DC: National Academy Press; 1991. [PubMed]
- 2.Tange HJ. The paper-based patient record: is it really so bad? Comput Methods Programs Biomed. 1995;48(1–2):127–31. doi: 10.1016/0169-2607(95)01672-g. [DOI] [PubMed] [Google Scholar]
- 3.Hippisley-Cox J, Pringle M, Cater R, Wynn A, Hammersley V, Coupland C, et al. The electronic patient record in primary care--regression or progression? A cross sectional study. Bmj. 2003;326(7404):1439–43. doi: 10.1136/bmj.326.7404.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nygren E, Wyatt JC, Wright P. Helping clinicians to find data and avoid delays. Lancet. 1998;352(9138):1462–6. doi: 10.1016/S0140-6736(97)08307-4. [DOI] [PubMed] [Google Scholar]
- 5.Sujansky WV. The benefits and challenges of an electronic medical record: much more than a "word-processed" patient chart. West J Med. 1998;169(3):176–83. [PMC free article] [PubMed] [Google Scholar]
- 6.Institute of Medicine. Crossing the Quality Chasm: A new health system for the 21st century. Washington, DC: National Academy Press; 2001. [PubMed]
- 7.Pratt W, Reddy MC, McDonald DW, Tarczy-Hornoch P, Gennari JH. Incorporating ideas from computer-supported cooperative work. J Biomed Inform. 2004;37(2):128–37. doi: 10.1016/j.jbi.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Treister NW. Physician acceptance of new medical information systems: the field of dreams. Physician Exec. 1998;24(3):20–4. [PubMed] [Google Scholar]
- 9.Kibbe DC, Phillips RL, Jr, Green LA. The continuity of care record. Am Fam Physician. 2004;70(7):1220, 1222–3. [PubMed] [Google Scholar]
- 10.Narus S, Wilcox A. Disease-specific data sheets in the management of chronic conditions - case example: diabetes (abstract). In: AMIA Annual Fall Symposium; 2002; San Antonio, TX; 2002.
- 11.Larsen DL, Cannon W, Towner S. Longitudinal assessment of a diabetes care management system in an integrated health network. J Manag Care Pharm. 2003;9(6):552–8. doi: 10.18553/jmcp.2003.9.6.552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993;329(14):977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 13.Thomas SM, Overhage JM, Warvel J, McDonald CJ. A comparison of a printed patient summary document with its electronic equivalent: early results. Proc AMIA Symp. 2001:701–5. [PMC free article] [PubMed] [Google Scholar]
- 14.Casalino L, Gillies RR, Shortell SM, Schmittdiel JA, Bodenheimer T, Robinson JC, et al. External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. Jama. 2003;289(4):434–41. doi: 10.1001/jama.289.4.434. [DOI] [PubMed] [Google Scholar]
- 15.Bodenheimer T. Interventions to improve chronic illness care: evaluating their effectiveness. Dis Manag. 2003;6(2):63–71. doi: 10.1089/109350703321908441. [DOI] [PubMed] [Google Scholar]
- 16.Rothman AA, Wagner EH. Chronic illness management: what is the role of primary care? Ann Intern Med. 2003;138(3):256–61. doi: 10.7326/0003-4819-138-3-200302040-00034. [DOI] [PubMed] [Google Scholar]
- 17.James BC. Implementing practice guidelines through clinical quality improvement. Front Health Serv Manage. 1993;10(1):3–37. discussion 54–6. [PubMed] [Google Scholar]
- 18.James B. Information system concepts for quality measurement. Med Care. 2003;41(1 Suppl):I71–9. doi: 10.1097/00005650-200301001-00008. [DOI] [PubMed] [Google Scholar]
- 19.Murray MD, Harris LE, Overhage JM, Zhou XH, Eckert GJ, Smith FE, et al. Failure of computerized treatment suggestions to improve health outcomes of outpatients with uncomplicated hypertension: results of a randomized controlled trial. Pharmacotherapy. 2004;24(3):324–37. doi: 10.1592/phco.24.4.324.33173. [DOI] [PubMed] [Google Scholar]