Abstract
The personal health record has potential to improve health care transition for an emerging population of pediatric patients with complex chronic conditions who survive to adulthood. In this study qualitative techniques were used to assess how young adults with spina bifida and their parents interact with their medical records. Condensation and categorization strategies for inductive research based on Grounded Theory were used to analyze 1) Who is involved in record keeping 2) How the information is stored 3) What information is kept and shared among the different constituencies and 4) When patients and parents need the information. Theme analysis revealed that mothers play a central role in the medical record management of adolescents with spina bifida. The parent-maintained home based records served as a linking pin in a heterogeneous healthcare information environment. These records tended to be organized as time-lines. Both parents and patients were concerned about how best to transition health information management to adult children. Patients and parents uniformly supported the idea of accessing medical record on-line.
Introduction
The vast majority of children with severe chronic conditions such as cystic fibrosis, childhood cancer, congenital heart disease, and spina bifida now survive to adulthood.(1) The movement of these young adults from pediatric-oriented care to adult-oriented care is an emerging health care concern that has implications for health information management.(2) It is generally acknowledged that health care transition for this population is sup-optimal.(3) Barriers to successful transition for these “pioneer survivors” include 1) adult providers’ lack of training in pediatric-onset chronic conditions, 2) poor communication between pediatric providers and adult providers, and 3) the expectation of independence in navigating the adult health care system.(4)
The net effect of these system level barriers is that “pioneer survivors” are expected to relay and explain what is often an exceedingly complex past medical history to adult health care providers. A concise medical summary or “transition note,” i.e., the personal health record, has been proposed as a mechanism for improving health care transition.
The personal health record occupies one of the three principal dimensions of the National Health Information Infrastructure(5). It is a linear descendant of the patient-held record, long seen as having the potential to increase both patient knowledge and patient adherence to treatment (6, 7). Thompson(8) described this education specifically: patients would know, from holding their own records, what services were available to them in the healthcare system, especially the identities of and the roles played by multiple providers in that system.
The patient-held record was envisioned as useful in diverse geriatric care situations: acute hospitalization at night, change to a new general practitioner, transfer to residential care, or anything involving travel. In the pediatric domain, one pediatric oncologist (9) also saw great advantages of the patient-held record in making information more easily available to healthcare providers: “the patient’s family will not be able to provide accurate and useful information about treatment received or treatment that is due” (p. 330). Patient-held records could reduce errors of dosage repetition, dosage omission, or dosage errors in situations where treatment instructions were shared across staff and across and between institutions.
No studies to date have examined how “pioneer survivors” currently interact with their medical record or whether they view the personal health record as a transition support tool. In this study we examined how adolescents with spina bifida and their families interact with their medical records during the transition from pediatric to adult-oriented care.
Spina bifida is a complex congenital malformation, resulting in both physical disability (paraplegia) and learning disability. Patients with spina bifida typically require multiple sub-specialists to manage medical and surgical complications. Improvements in neurosurgical techniques, the introduction of the cerebrospinal fluid shunt, and advances in urologic care have dramatically improved survival for children born with this condition.
The young adult with spina bifida thus is a prototypical “pioneer survivor”. Careful examination of his/her interaction with the medical record provides a prototypical instance for examining the role of the medical record in supporting health care transition for pioneer survivors in general. The results have implications for future healthcare information and personal healthcare record systems, and in particular what role patients and parents play in the management of their medical information.
Methods
Focus groups and structured interviews were conducted to examine if and how young adults with spina bifida interact with their medical record during their transition to adult health care. Participants were drawn from a population base of 34 young adults aged 18–21 years receiving comprehensive care at a regional referral center for persons with spina bifida and spinal cord injury. Recruitment felt in two phases.
First, all 34 patients and their families received an invitation to participate in the study followed up by a phone call. Secondly, the medical director of the referral center extended the invitation during routine visits. Recruitment was hampered by the great distances this largely rural based patient population had to traverse to participate in the study. A convenience sample of six patients (4 young men and 2 young women), six family members (4 mothers and 2 fathers) and one private duty home nurse committed to participate. Highly motivated parents and well functioning patients with little cognitive impairment were overrepresented in this sample. All participants were provided with a $20 incentive. Using a standard protocol the focus groups were conducted by two researchers with expertise in health informatics and by a pediatric researcher who is medical director of the referral center.
Analysis
The focus group discussions were transcribed verbatim. To analyze the data we used the qualitative and inductive research technique known as Grounded Theory (10, 11). Data coding and analysis were done using NVIVO qualitative software (QSR, Sydney, Australia). NVIVO permitted coding of dominant themes in text and was well suited for analysis of transcribed oral interviews. The data analysis consisted of two phases.
Condensation: The three investigators read through all interview transcripts to identify issues and topics that relate to the use of documents in the transition from pediatric to adult care. Each investigator aggregated these to arrive at a set of common or recurring themes. The investigators then met and present their individual aggregated themes. A shared set of common theses were generated. The investigators then returned to the data and reexamined those in terms of the new set of common condensed themes.
Categorization: These themes were used to categorize and code interviews. This allowed us to structure the extensive material, give an overview, detect differences in document use behaviors among the different participants, and quantify the responses.
Results
The focus group results clustered around four questions: 1) Who is involved in record keeping? 2) How is the information stored? 3) What information is kept and shared among the different constituencies? 4) When do patients and parents need the information? Theme analysis around these questions revealed the following:
Who
Three groups emerged as central to patients’ medical record keeping: hospitals, subspecialty providers, and mothers. Notably absent were documents generated by primary care physicians. “The pediatrician deferred to all the specialists, and so…they are at limited knowledge, that’s the problem”. School records and learning disability documents were also absent from medical records maintained by families. Only when prompted did families acknowledge that the school system maintained records.
All patients regarded their parents, and, in particular, their mothers, as the key to their record keeping. “All my doctors, the spina bifida clinic, my parents, people of that nature.” Typically, patients disregarded themselves when it came to medical record keeping. They recognized the importance of managing their healthcare information but largely delegated this management function to their parents. “I’ve always thought of my medical records as the engine in my car. I wouldn’t know the first thing about what to do with a car engine and I’ve never looked up my medical records. I just figured they’d be all in medical terms that I wouldn’t know the first thing about.”
How
Patients and parents did not have a clear conception of how healthcare providers managed their medical records. They presumed that each institution or clinic had developed their own record keeping practices. “I think it is personal style and how their practice is set up.” There was also a general sense that no one healthcare provider harbored a complete history. One mother explained: “I don’t think one institution has a complete idea of what I have been through in my life” She stated also “There are overlaps; I don’t think one place has the whole story.”
Medical records maintained by families were organized chronologically. One mother used her child’s baby book to keep track of major and minor health events: “In the baby book I kept significant information, for instance, if he had surgery and when he vomited after surgery, or how he reacts to medication – those kind of things.” A second family kept a timeline of records in a filing cabinet in their living room. The home nurse kept a binder with dated and timed entries summarizing daily health status and major healthcare events. The sole patient in this study reporting that she maintained her own health record had created a folder to take with her to college. This folder contained sequentially ordered sheets from doctors’ visits, a medication list, and a calendar diary to monitor her headaches.
Memory was considered essential for keeping track of the sequence of healthcare events: “The records you (healthcare providers) have on paper I have in my head. I have jotted notes down that I keep for my own memory but I am a walking sheet of information and if something happens to me, who else is going to know that? And that’s the thing that as parents we all do that. And I think that we forget that some day our kids are going to grow up and they are going to need to know this or that.
Patients reported that they would remember some of their pertinent healthcare events but not to the same degree as their mothers. One patient explained: “You are expected to know, you are expected to know your allergies and you have had your mother tell the doctor all this. And now your father is saying to you that you should know this. It’s like, wait a minute, when did I get in charge of all this?”
The urge to gather a comprehensive record seems to stem from the parents’ perception that they were the only entity with access to the complete healthcare history. This urge to document their comprehensive knowledge was put in perspective when they considered handing off responsibility to their children. One mother describe how she created a three-ring binder for her child: “We said, ok, it is going to take us awhile to figure out what is what. But, let’s go back and we will do all your medical history, here is where everything started, here’s what you had happen, here’s where we have been, here’s your doctors. Things that work for various systems that you have had problems with, and we went through and we tried this. These are the vendors that we went to, this is where you got your wheelchair and then had that in a three-ring binder.”
What
Patients and parents reported that standard questions on medical forms failed to capture the complexity of spina bifida care “There is never enough room for our kids there is just never enough room for anything.” Patient and parents all agreed that the information provided from healthcare providers greatly lacked detail and comprehensiveness. The generic information provided in hospital discharge summaries was mentioned several times. “The discharge papers, all they do [is] give you a number to call if something happens and just tell you what to look for if there’s a problem.”
They noted that providers asked them the same generic questions again and again, and stated that this was so even within the same healthcare institution. “It is pretty much the same thing over and over and over and over again.” When asked what kind of healthcare information was useful in their medical documents patients and parents reported that baseline information on vital signs, x-rays, and baseline physical exam findings was important. Yet, they preferred to have access to all records. In the words of a father: “First the baseline and from there everything else.”
Patients and parents felt that many healthcare providers deliberately did not want them to have access to their medical record. They were bewildered by this. They perceived that their medical information belonged to them and not to the healthcare providers and institutions. In the words of one mother: “I was told that your records are your own records and you should be able to ask for your records at any time. But, at most institutions or even doctors offices, they say ‘oh no, no, no! They are our records. They belong to us. If you want them, you are certainly going to have to request them through our records office and if you would like a copy, it’s going to cost you X amount per page.’ Somehow, that just never seemed right to me.” Another mother was asked if she minded repeating the history every time she went to different doctors. She responded: “I wouldn’t mind so much, if they were as good giving the information back as [we] are about giving it.”
Patients and parents also expressed a related concern that medical records and information were not shared between healthcare institutions. Typically, parents took an active role in facilitating the sharing of records and medical information. “In our case things aren’t really shared at all. We actually have to get that information to tell them to talk to each other or tell them to share information. They would never do it on their own.” Privacy issues stood out as a secondary concern compared to successful medical information sharing. Parents perceived HIPAA regulations as hampering information sharing.
Parents and patients uniformly supported the idea of having access to the medical record on-line. Interestingly, patients were particularly animated by the prospects of on-line access to their medical records. They liked the idea of being able to select the information that they needed and use in organizing the information in a format helpful to them. “I think it would be helpful in the sense that you could pick what you would want to keep or print out, instead of having a thick pile of discharge papers and summaries. You could pick out what would pertain to certain situations, like what would help the most, if you needed quick information.”
When
Patient and parents emphasized that medical emergencies highlighted their need for a complete and accessible medical record. Several patients described situations where a simple base-line CT scan would have saved them hours of uncertainty and confusion in the Emergency Room. Patients and parents came to realize the distributed and incomplete nature of their medical record also when moving or long-distance travel. They worried what would happen when they were faced with a new healthcare institution and no easy access to even rudimentary medical histories. “What kind of shunt does he have? I know that it goes into his stomach but I don’t know if the parts are universal. If I show up in Hospital X and something is wrong with his shunt, will they have to pull it out and start over? Those types of questions concern me.”
Discussion
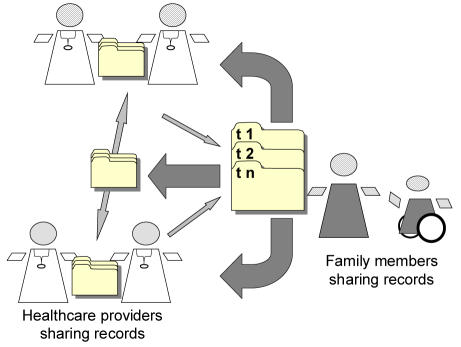
Parents play a central role in the medical information and record management of adolescents with spina bifida as they transition from pediatric care to adult oriented care. As summarized in Figure 1, medical records are distributed among a large numbers of healthcare providers and institutions, with no central record or healthcare person in charge of coordinating and keeping a complete medical history. As a result no official record captured the continuity of care over the patient’s lifespan or the distributed nature of their care involving many institutions and sub-disciplines.
Figure 1.
Medical record sharing as perceived by patients and parents
As represented by the small light gray arrows in Figure 1, parents and patients found that healthcare providers share a limited set of medical records with each other and with the patient. None of the participants reported having access to “transition notes” or other information tools. In this environment parents seemed to serve as the axle in their children’s medical history management. They incessantly furnish different healthcare institutions with information and often coordinated information sharing among healthcare institutions (i.e., the large dark gray arrows in Figure 1). As a central part of this effort, parents kept detailed records of their children’s medical history. These records tended to be organized as time-lines (i.e., t1, t2, t3, tn), which can be seen as an effort to capture the temporal continuity of care over the patient’s lifespan. Furthermore, the home records brought together information from all healthcare providers.
Conclusion
The objective of this descriptive pilot study of adolescents with spina bifida was to gain a qualitative understanding of medical information management as perceived by “pioneer survivors” and their parents. We found that the patients and parents were less concerned with the transition from pediatric to adult medicine than with the prospects of the children taking over the management of their own medical information in a heterogeneous healthcare information environment. The study raises a number of issues with implications for medical information system development.
First, more research is needed into how electronic personal health records can take into account parents’ and patients’ central role as medical information managers. Such research should focus on parents and patients’ attempts to secure continuity in their medical histories and facilitate information sharing among distributed healthcare providers.
Second, efforts should be made to help parents transition their information management role to their adult children. Information systems tailored to this purpose and audience would be appropriate. Healthcare education tied into home-centered medical record systems would be particularly relevant for adolescents with developmental and learning disabilities.
Third, focus group participants stressed that internet-accessible medical records would be a helpful tool.
Fourth, given the failure of the healthcare industry to implement a universal patient record system, future information system design may seek inspiration from patients’ and parents’ current information management practices. Such systems could be managed by patients and their parents or trusted third party support.
Limitations and Future Research
The small sample and qualitative, exploratory, and descriptive nature of this study pose limits to the findings reported here. First, the focus group participants represented motivated parents and well functioning patients. We do not know how less engaged patients and parents perceive the sharing of their medical records. Secondly, the specific needs of spina bifida patients seeing a large number of sub-specialties may also shape participants’ responses. Finally, some ideas and perspectives may have been left out given the flow of the focus group interviews, although we did separate patients and parents for parts of the focus group interview to make sure that both groups got a chance to voice their opinions. Future research would benefit from the study of other populations. We can recommend that researchers schedule focus group studies around patient’s routine healthcare visits in an effort to involve more patients and family members.
References
- 1.Blum R. Transition to adult health care: Setting the Stage, Journal of Adolescent Health. Journal of Adolescent Health. 17:3–5. doi: 10.1016/1054-139X(95)00073-2. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Pediatrics, American Academy of Family Physicians, Medicine ACoP-ASoI. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110(6 part 2):1304–6. [PubMed] [Google Scholar]
- 3.Betz C. Transition of Adolescents with Special Needs: Review and Analysis of the Literature. Issues in Comprehensive Pediatric Nursing. 2004;27:179–241. doi: 10.1080/01460860490497903. [DOI] [PubMed] [Google Scholar]
- 4.Reiss J, Gibson R. Health care transition: destinations unknown. Pediatrics. 2002;110(6 part 2):1307–14. [PubMed] [Google Scholar]
- 5.FAQS about NHII. In: U.S. Department of Health and Human Services: U.S. Department of Health and Human Services; 2005.
- 6.Giglio RJ, Papazian B. Acceptance and use of patient-carried health records. J Am Med Rec Assoc. 1987;58(5):32–6. [PubMed] [Google Scholar]
- 7.Winkelman W, Leonard K, PG R. Patient-perceived usefulness of online electronic medical records: employing grounded theory in the development of information and communication technologies for use by patients living with chronic illness. J Am Med Inform Assoc. 2005;12(3):306–14. doi: 10.1197/jamia.M1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson M. Hypothesis: old people would benefit from a patient-held standardized primary health care record. Age Ageing. 1989;18(1):64–6. doi: 10.1093/ageing/18.1.64. [DOI] [PubMed] [Google Scholar]
- 9.Stevens M. "Shuttle sheet": a patient-held medical record for pediatric oncology families. Med Pediatr Oncol. 1992;20(4):330–5. doi: 10.1002/mpo.2950200412. [DOI] [PubMed] [Google Scholar]
- 10.Murphy E, Dingwall R, Greatbatch D, Parker S, Watson P. Qualitative research methods in health technology assessment: a review of the literature. Health Technology Assessment. 1998;2(16) [PubMed] [Google Scholar]
- 11.Strauss A, Corbin JM. Basic of Qualitative Research: Grounded Theory Procedures and Techniques. London: Sage; 1990.