Abstract
We hypothesize that a representation of drug-drug interactions (DDIs) based on physiologic, pharmacokinetic (PK), and pharmacodynamic (PD) mechanisms will provide more accurate and useful information to clinicians than current approaches that simply tabulate and index pairwise interactions of drugs. This paper explores the strengths, weaknesses, and difficulties of modeling drug mechanisms and reports on our initial work designing and implementing a drug Knowledge Base (KB) based on qualitative pharmacokinetic mechanisms.
COMPUTATIONAL MODELING OF DRUG INTERACTION KNOWLEDGE
Evaluating the potential for Adverse Drug Interaction (ADIs) requires a detailed understanding by the clinician of clinical pharmacology. A patient’s genetics and physiology interact with the clinical pharmacology to affect drug response. For example, a patient’s renal clearance can affect the serum level of a drug that is primarily eliminated by renal excretion. This pharmacokinetic outcome can lead to a pharmacodynamic effect; a change in drug concentration that alters the biological effect of the drug.
The prescribing clinician’s knowledge of the mechanisms by which drugs interact is invaluable to evaluating the risk of drug-drug interactions. Information which is useful for inferring the potential risk of ADI includes:1
known pharmacodynamic (PD) and pharmacokinetic (PK) interactions between each drug pair and the mechanisms by which they interact
the number and importance of pathways by which a drug is cleared
degree to which a drug is absorbed if orally administered
the relationship between drug dose and plasma concentration
the ratio between the effective dose and the toxic dose (therapeutic index)
the time it takes a drug to reach steady-state plasma concentration
Constructing a computational model of the mechanisms for drug-drug interactions (DDIs) may lead to better clinical decision tools that:
provide sufficient information on the mechanisms of interaction to support DDI management
support reasoning about the potential effects of removing a drug from a patient’s regimen
support reasoning about the potential for interactions in patients taking multiple prescriptions (e.g. does a specific combination of drugs result in multiple pathway inhibition of a narrow-therapeutic index drug?)
avoid alerting clinicians to DDIs that are not feasible based on mechanisms
A HYPOTHETICAL EXAMPLE
In theory, at least a portion of drug pharmacokinetic and pharmacodynamic knowledge can be modeled as a set of rules expressing the effect of a precipitanta drug on the absorption, distribution, and clearance of an object drug.
For example, the following First Order Logic (FOL)b predicates describe metabolic drug-drug interactions whereby a drug, x, modulates (inhibits or induces) the primary clearance enzyme, z, of another drug, y, leading to a change (increase or decrease) in drug y’s clearance:
Other rules may describe DDIs occurring due to a change in pH or gastro-intestinal (GI) motility. For example, if a drug, y, inhibits the hydrolyzation of an acid-hydrolyzable prodrug, x, then a reduction in y’s absorption follows.
Rules such as these can be referred to by other rules to construct a simple theory to predict harmful DDIs. For example, the following rules refer to the previous rules to define sufficient conditions for a potentially harmful DDI.
If a drug, y, causes an increase in the clearance of another drug, x, then y decreases the bio-availability (the amount of drug in a patient’s bloodstream) of x.
If a drug, y, causes a decrease in the clearance of another drug, x, then y increases the the bio-availability (the amount of drug in a patient’s bloodstream) of x.
If a drug, y, reduces the gastro-intestinal absorption of another drug, x, then y reduces the bio-availability of drug x.
If the ratio of the dose at which a drug, x, is toxic over the dose at which it is therapeutic is small, and another drug, y, causes an increase or decrease in the bio-availability of x then a potentially harmful DDI is implied:
Our hypothetical model can be extended to include reasoning on the effects of three or more drugs prescribed simultaneously. Take the hypothetical case of an elderly patient who has had a stroke and suffers from ulcers. Such a patient may require medication to treat the ulcers as well as the underlying cardiovascular etiology of the stroke. The prescribing clinician must evaluate the risk of potential DDIs in the context of the combined effect of all drugs.
Assume the patient is on warfarin to treat the cardiovascular condition and cimetidine for ulcer treatment. Warfarin is a substrate of the enzymes CYP3A4, CYP2C19, CYP1A2, and CYP2C9 while cimetidine inhibits CYP2C19. If this patient requires treatment for an infection clarythromycin may be considered. However, clarythromycin is an inhibitor of CYP3A4, CYP1A2, and CYP2D6. The clinician may note that this drug would inhibit two of the three remaining metabolic clearance pathways for Warfarin, and avoid prescribing it.
To our knowledge, no DDI software is capable of predicting this sort of interaction, although it is theoretically possible to encode the reasoning. The following rule defines a state where three of the metabolic pathways of a drug, x, are inhibited by two other drugs; y, which inhibits two pathways, and z, which inhibits one.
CONSTRUCTING A TEST DRUG KNOWLEDGE BASE
To better understand the issues of formally representing DDI knowledge, we constructed a simple model involving rules on metabolic mechanisms. A large number of DDIs can be explained by metabolic mechanisms, especially for drugs metabolized by the Cytochrome-P450 enzymes (CYP450) enzymes. Furthermore, for many drugs, data exists on their metabolic mechanisms. FDA guidelines encourage detailed investigations into the metabolic mechanisms of a drug and its potential for drug interactions during that drug’s early development.2 These investigations are often followed by clinical trials to determine the significance of potential drug interactions.2, 3
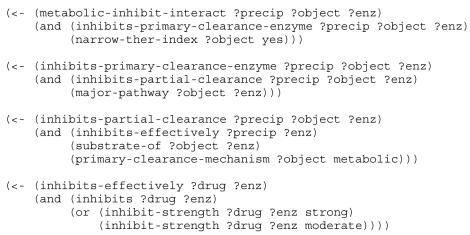
We first created a FOL representation of metabolic mechanisms of drug-drug interaction from the lectures and class notes of a graduate class on drug-interactions. Figure 1 shows the rules pertaining to inhibition of clearance; a similar set of rules was implemented for metabolic induction.
Figure 1.
Rules in mock Prolog implementing metabolic interactions between drugs.
We then constructed a small drug knowledge-base (KB) containing the necessary drug facts for inference with the selected rules. Facts on the important metabolic enzymes for 249 currently prescribed drugs were input into the KB from a widely used pocket reference on clinically significant drug interactions.4 This reference (Reference A) also included facts on each drug’s potential for inhibition or induction of CYP450 enzymes.
We augmented our KB with information from a Continuing Education Module containing pharmacokinetic information on drugs commonly prescribed to elderly epileptic patients.1 In addition to facts on potential CYP450 modulation, this reference (Reference B) listed the relative importance of each drug’s clearance enzymes. Several drugs not found in Reference A were also added. Since terms regarding the strength of enzyme inhibition and induction varied between the resources, we constructed the mapping shown in Table 1. As of the time of this writing, our drug KB contains facts useful for mechanism based inference for 267 currently prescribed drugs.
Table 1.
Mapping between strength of inhibition in Reference A and Reference B and the Drug KB used to test mechanism based drug-drug interaction prediction
We implemented both the rules and the database in Lisp. The implementation uses a simple pattern matching and backward chaining program taken verbatim from chapter 15 of Paul Graham’s popular Common Lisp book.5 Graham’s code uses a Prolog-like syntax, where the macro <− is analogous to the Prolog :− connector, but as usual in Lisp, prefix notation is used. So, the list expressions have <− followed by a head expression and optionally a tail expression. Rules that have multiple terms in the tail use combinations of the operators and, or, and not to combine them.
AN EXPERIMENT WITH PAIR-WISE INTERACTIONS
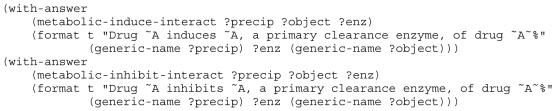
We performed two simple queries (Figure 2) against the drug KB for any drugs that inhibit or induce the primary clearance enzyme for another narrow-therapeutic index drug whose clearance is primarily metabolism. Results were returned in the form of “DRUG-A inhibits/induces ENZYME, a primary clearance enzyme of drug DRUG-B”. For example:
Figure 2.
Queries for any drugs that inhibit or induce the primary clearance enzyme for another NTI drug whose clearance is primarily metabolism
PHENYTOIN induces CYP2C9, a primary clearance enzyme, of drug WARFARIN
The queries returned a total of 90 predicted DDIs. These included 12 induction interactions involving three precipitants (Carbamazepine, Phenobarbital, and Phenytoin) and five object drugs (Valproate, Phenobarbital, Phenytoin, Warfarin) and 78 inhibition interactions involving 35 precipitant and four object drugs.
We checked the interactions predicted with four online drug reference databasesc A predicted drug-drug interaction was considered clinically viable if it was reported in any of the four sources. Fourteen of the 90 (16%) predicted interactions could not be found in any KB (see Table 2).
Table 2.
14 speculative inhibition interactions not documented in any of the four online references. In each row, the precipitant drug inhibits the primary clearance enzyme (PCE) of the object drug based on information in the drug KB.
| Precipitant | PCE | Object |
|---|---|---|
| amiodarone | CYP2C9 | phenobarbitol |
| disulfiram | CYP2C9 | phenobarbitol |
| fluorouracil | CYP2C9 | phenobarbitol |
| fluconazole | CYP2C9 | phenobarbitol |
| gemfibrozil | CYP3A4 | carbamazepine |
| gemfibrozil | CYP2C9 | phenobarbitol |
| gemfibrozil | CYP2C9 | phenytoin |
| leflunomide | CYP2C9 | phenobarbitol |
| miconazole | CYP3A4 | carbamazepine |
| sulfamethizole | CYP2C9 | phenobarbitol |
| sulfamethoxazole | CYP2C9 | phenobarbitol |
| sulfinpyrazone | CYP2C9 | phenobarbitol |
| sulphaphenazole | CYP2C9 | phenobarbitol |
| zafirlukast | CYP3A4 | carbamazepine |
| zafirlukast | CYP2C9 | phenytoin |
| zafirlukast | CYP2C9 | phenobarbitol |
Close examination of the fourteen speculative interactions revealed that some of the facts in the drug database were weakly supported. For example, phenobarbitol has been shown to be metabolized by CYP2C9 in vitro but there is little in vivo evidence to support this assertion. Unfortunately, in vitro evidence on drug interactions does not always map to predictions of in vivo occurrences.2, 3 Also, the DDI KB listed disulfiram as a CYP2C9 inhibitor based on Reference A. Incorporating information from other sources may weaken this assertion because, while some human studies indicate that disulfiram may be a CYP2C9 inhibitor, it has not been found to inhibit S-warfarin or tolbutamide, both CYP2C9 substrates.
DISCUSSION AND CONCLUSIONS
We have shown that it is possible to qualitatively model DDIs based on pharmacokinetic (PK) and phar-macodynamic (PD) mechanisms. A KB that uses such a model could be used to infer both well-known interactions and those that are feasible but have not yet studied, including interactions resulting from the combination of more than two drugs in a patient. It would also be possible to infer of the effect of removing a drug from a patient with the information in the KB. A mechanisms-based KB could lead to improved tools for reasoning about DDIs because mechanistic information is useful to clinicians for reasoning about potential interactions. Furthermore, better tools for predicting or detecting potential DDIs could be built by applying automated inference techniques to the knowledge in the KB.
The results of our experiments suggest that a mechanism-based DDI KB will require more complex knowledge representation than simply stated drug facts to realize the potential benefits of this approach. Progress in building a qualitative model of DDI theory will require making concise definitions on the meanings of seemingly simple terms. For example, what does it mean for a drug to have a narrow-therapeutic index (NTI)? In constructing our drug KB we found NTI drugs listed by the FDAd, which differ from those in other publications discussing “critical dose” drugs.
Incorporating evidence for the assertions in the drug KB may be necessary for sound inference. For example, in vitro data from early drug development is less useful for predicting interactions of clinical relevance unless similar results have been found during clinical trials in humans. Similarly, conflicting evidence about an assertion weakens the inferences that can be made it. Since there are many commonly prescribed drugs for which little in vivo metabolic information can be found, or the information is conflicting, the DDI KB needs to handle missing information and uncertainty.
We have attempted to start off very simply and construct only a small DDI KB involving a portion of DDI knowledge. As such, we have chosen to not include many important components of DDI theory. For example, drug inhibition can be classified into competitive, mechanistic, and irreversible. Both mechanistic or irreversible enzyme inhibition have effects after the precipitant drug is removed. Reasoning on long-lasting effects increases the complexity of the model as it requires some conception of time.
Constructing qualitative rules requires making artificial distinctions between certain parameters. For example, our drug database models both induction and inhibition as being weak, moderate, and strong (see Table 1). While the strength of inhibition can be quantified for CYP3A4 inhibitors by based on the change in AUC of Midazolam (a drug cleared primarily by CYP3A4) in the presence of the inhibitor,6 not all enzymes have ideal probe substrates.
Since no standard meaning for strength classification across drugs and enzymes exists, using such parameters in reasoning may yield false results. A similar difficulty occurs in making qualitative statements about the level of first-pass metabolism a drug undergoes, or the amount an enzyme contributes to a drug’s clearance.
In conclusion, these results suggest that a DDI theory will require more complex logic and knowledge representation than rules and supporting drug facts. Also, it is important to agree on exact definitions of the terms used to reason about DDIs. Our future work will involve further research to exploring these issues and proposing solutions.
ACKNOWLEDGMENTS
This work was partially supported by NIH grant T15 LM07442 from the National Library of Medicine. Thanks to Brent Louie for helping to insert information into the project’s drug database and for evaluating the output of our Knowledge Base.
Footnotes
For a given DDI, a drug causing some pharmacologic change on another drug is called the precipitant while the affected drug is called the object.
Throughout this paper we use ’∧’ to represent conjunction (e.g. X and Y ), ’∨’ to represent disjunction (e.g. X or Y ), ’⇒’ to represent implication (e.g. X implies Y ), and ¬ to imply negation.
First Data Bank’s Micromedex, WebMD’s Medscape, Discovery health.discovery.com, and Cerner Multum’s Drugs.com.
References
- 1.Collins C and Levy R. Drug-drug interaction in the elderly with epilepsy: Focus on antiepileptic, psychiatric, and cardiovascular drugs. Profiles in Seizure Management 2004;3(6).
- 2.Lin JH. Sense and nonsense in the prediction of drug-drug interactions. Current Drug Metabolism. 2000;1(4):305–32. doi: 10.2174/1389200003338947. [DOI] [PubMed] [Google Scholar]
- 3.Ito K, Brown HS, Houston JB. Database analyses for the prediction of in vivo drug drug interactions from in vitro data. British Journal of Clinical Pharmacology. 2003;57(4):473–86. doi: 10.1111/j.1365-2125.2003.02041.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hansten PD and Horn HR. The Top 100 Drug Iteractions, A Guide to Patient Management. H&H Publications, 2004.
- 5.Graham P. ANSI Common Lisp Prentice Hall, 1996.
- 6.Levy RH, Thummel KE, Trager WF, Hansten PD, and Eichelbaum M, eds. Metabolic Drug Interactions - Kenneth E. Thummel and Kent L. Kunze and Danny D. Shen. Lippincott, Williams, and Wilkens, 2000.