The diagnosis of acute appendicitis is predominantly a clinical one; many patients present with a typical history and examination findings. The cause of acute appendicitis is unknown but is probably multifactorial; luminal obstruction and dietary and familial factors have all been suggested.1 Appendicectomy is the treatment of choice and is increasingly done as a laparoscopic procedure. This article reviews the presentation, investigation, treatment, and complications of acute appendicitis and appendicectomy.
How common is appendicitis?
Appendicitis is the most common abdominal emergency and accounts for more than 40 000 hospital admissions in England every year.2 Appendicitis is most common between the ages of 10 and 20 years, but no age is exempt.3 A male preponderance exists, with a male to female ratio of 1.4:1; the overall lifetime risk is 8.6% for males and 6.7% for females in the United States.3 Since the 1940s the incidence of hospital admission for acute appendicitis has been falling, but the reason for this decline is not clear.w1
How do I diagnose it?
Diagnosis of acute appendicitis relies on a thorough history and examination.w2
History
Abdominal pain is the primary presenting complaint of patients with acute appendicitis. The diagnostic sequence of colicky central abdominal pain followed by vomiting with migration of the pain to the right iliac fossa was first described by Murphy but may only be present in 50% of patients.4 Typically, the patient describes a peri-umbilical colicky pain, which intensifies during the first 24 hours, becoming constant and sharp, and migrates to the right iliac fossa. The initial pain represents a referred pain resulting from the visceral innervation of the midgut, and the localised pain is caused by involvement of the parietal peritoneum after progression of the inflammatory process. Loss of appetite is often a predominant feature, and constipation and nausea are often present. Profuse vomiting may indicate development of generalised peritonitis after perforation but is rarely a major feature in simple appendicitis. A meta-analysis of the symptoms and signs associated with a presentation of acute appendicitis was unable to identify any one diagnostic finding but showed that a migration of pain was associated with a diagnosis of acute appendicitis.5
Sources and selection criteria
We reviewed the Cochrane database for articles relating to acute appendicitis. We searched Medline for the past two years (up to June 2006) to find any recent meta-analyses, systematic reviews, or randomised controlled trials relating to appendicitis that JS had not included in the latest Clinical Evidence review. We also included important historical articles
Summary points
Appendicitis is the most common abdominal surgical emergency
Not all patients present in a typical manner
Patients at the extremes of age have increased mortality because of late presentation or subtle signs
Specialist investigations should not delay definitive treatment
Computed tomography scanning is more sensitive and specific than ultrasonography when diagnosing acute appendicitis
Laparoscopic appendicectomy is becoming increasingly common, and clinical evidence suggests that it has some advantages over open surgery
Wound infections can be decreased with the use of perioperative antibiotics
This classic presentation can be influenced by the age of the patient and anatomical position of the appendix (box 1).w3 Patients at the extremes of the age spectrum can present diagnostic difficulty because of non-specific presentation, often with subtle clinical signs. Infants and young children often seem withdrawn, and elderly people may present with confusion. A high index of suspicion for acute appendicitis is needed in such patients.
Box 1: Anatomical considerations in the presentation of acute appendicitis
The vermiform appendix is a tubular structure attached to the base of the caecum at the confluence of the taeniae coli. It is approximately 8-10 cm long in adults and represents the underdeveloped distal end of the large caecum seen in other animals. In humans it is regarded as a vestigial organ, and acute inflammation of this structure is called acute appendicitis
Retrocaecal/retrocolic (75%)—Right loin pain is often present, with tenderness on examination. Muscular rigidity and tenderness to deep palpation are often absent because of protection from the overlying caecum. The psoas muscle may be irritated in this position, leading to hip flexion and exacerbation of the pain on hip extension (psoas stretch sign)
Subcaecal and pelvic (20%)—Suprapubic pain and urinary frequency may predominate. Diarrhoea may be present as a result of irritation of the rectum. Abdominal tenderness may be lacking, but rectal or vaginal tenderness may be present on the right. Microscopic haematuria and leucocytes may be present on urine analysis
Pre-ileal and post-ileal (5%)—Signs and symptoms may be lacking. Vomiting may be more prominent, and diarrhoea may result from irritation of the distal ileum
Examination
The patient is often flushed, with a dry tongue and an associated fetor oris. The presence of pyrexia (up to 38°C) with tachycardia is common. Abdominal examination reveals localised tenderness and muscular rigidity after localisation of the pain to the right iliac fossa. Rebound tenderness is present but should not be elicited to avoid distressing the patient. Patients often find that movement exacerbates the pain, and if they are asked to cough the pain will often be localised to the right iliac fossa. The site of maximal tenderness is often said to be over McBurney's point, which lies two thirds of the way along a line drawn from the umbilicus to the anterior superior iliac spine.6 Findings on per rectal and vaginal examination may be normal, although tenderness to the right may be present particularly in a pelvic appendix. Tenderness on rectal examination may be suggestive but is not diagnostic of appendicitis.5 Percussion tenderness, guarding, and rebound tenderness are the most reliable clinical findings indicating a diagnosis of acute appendicitis.5
Further examination techniques that may aid in the diagnosis of appendicitis are Rovsig's sign (palpation of the left iliac fossa causes pain in the right iliac fossa), psoas stretch sign, and the obturator sign.w4
Terminology
Simple appendicitis—Inflamed appendix, in the absence of gangrene, perforation, or abscess around the appendix
Complicated appendicitis—Perforated or gangrenous appendicitis or the presence of periappendicular abscess
Negative appendicectomy—Term used for an operation done for suspected appendicitis, in which the appendix is found to be normal on histological evaluation
Box 2: Investigation of acute appendicitis
Urine analysis—up to 40% can have abnormalities
Pregnancy test—to exclude pregnancy
Full blood count—neutrophil (> 75%) predominant leucocytosis is present in 80-90%
C reactive protein—raised concentration may be present, but its absence should not exclude a diagnosis of appendicitis
What investigations might help?
Specialist investigations are rarely needed to confirm a diagnosis of acute appendicitis, and the diagnosis is predominantly a clinical one. No specific diagnostic test for appendicitis exists, but the judicious use of simple urine and blood tests, particularly inflammatory response variables, should allow exclusion of other pathologies and provide additional evidence to support a clinical diagnosis of appendicitis (box 2).5 Scoring systems and algorithms have been proposed to aid the diagnosis of acute appendicitis but have not been widely used.w5-w7
Radiological tests can be used to aid the diagnosis of acute appendicitis. The table describes the role of these investigations, and we consider the use of ultrasonography and computed tomography scanning (fig 1) in more detail below.
Table 1.
Imaging and diagnosis of acute appendicitis
| Investigation | Diagnostic criteria | Evidence |
|---|---|---|
| Plain radiography |
None |
No role in diagnosis of acute appendicitis,w6 although in some cases a faecolith may be shown |
| Ultrasonography |
Aperistaltic and non-compressible structure with diameter >6 mmw8 |
Sensitivity of 86%; specificity of 81%7 |
| Computed tomography scanning |
Abnormal appendix identified or calcified appendicolith seen in association with periappendiceal inflammation or diameter >6 mmw8 |
Sensitivity of 94% and specificity of 95% in diagnosis of acute appendicitis7 |
| Magnetic resonance imaging | Not confirmed | Restricted to cases in which radiation and diagnostic difficulties preclude use of other modalities (for example, pregnancy)8w9 |
Fig 1.
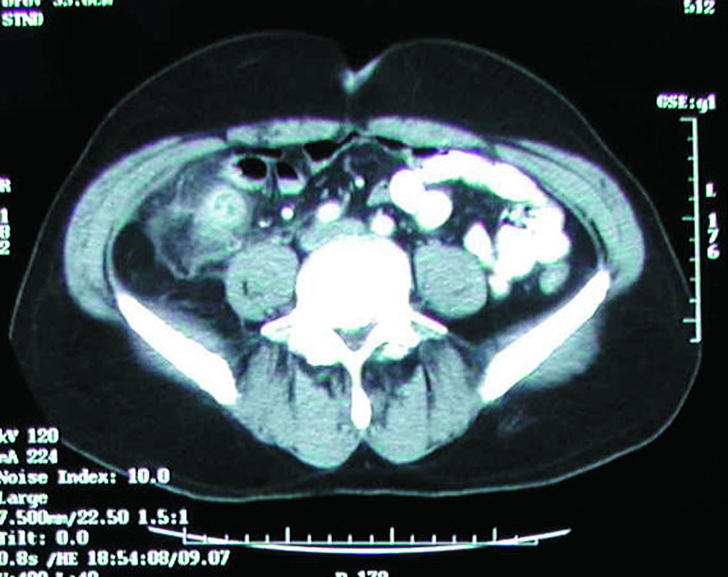
Computed tomography scan showing inflammatory mass in right iliac fossa secondary to acute appendicitis
One meta-analysis and one systematic review on the role of ultrasonography and computed tomography scanning in the diagnosis of acute appendicitis have concluded that these investigations should be done only in patients in whom a clinical and laboratory diagnosis of appendicitis cannot be made. As ultrasonography studies are operator dependent and need careful examination, these authors also recommend the use of computed tomography in preference to ultrasonography in this group of patients as it has a greater diagnostic accuracy.7,9
The impact of the introduction of imaging techniques on the negative appendicectomy rate is unclear. A longitudinal study has suggested that despite the introduction of ultrasonography and computed tomography scanning the rates of negative appendicectomy have remained unchanged.10 The moderate diagnostic accuracy of ultrasonography in such studies was stated as a possible reason for this.7 However, two prospective studies have evaluated the use of computed tomography, and both showed a decrease in the number of unnecessary admissions and appendicectomies.w10 w11 Importantly, some authors have highlighted the risk of unnecessary exposure to ionising radiation caused by excessive use of computed tomography scans, and low dose protocols have been advocated.w12
Differential diagnosis
The differential diagnosis of appendicitis is that of an acute abdomen (box 3). At the extremes of age, the threshold for referral for further assessment should be low because of the high mortality associated with delayed presentation or diagnosis.
How do I treat it?
Herbert Fitz was the first author to publish on the need for early diagnosis and surgery for acute appendicitis.11 Appropriate resuscitation followed by expedient appendicectomy is the treatment of choice. No good evidence exists to support the notion that analgesia should be withheld on the grounds that it may cloud the clinical picture.12 w13 All patients should receive broad spectrum perioperative antibiotics (one to three doses), as they have been shown to decrease the incidence of postoperative wound infection and intra-abdominal abscess formation.13
Timing of surgery
A recent retrospective study found no significant differences in complications between early (less than 12 hours after presentation) or later (12-24 hours) appendicectomy.14 This does not, however, take into account the actual time from the onset of symptoms to presentation, which can have a bearing on the rate of perforation.15 After the first 36 hours from the onset of symptoms the average rate of perforation is between 16% and 36%, and the risk of perforation is 5% for every subsequent 12 hour period.16 w14 Once a diagnosis is made, appendicectomy should therefore be done without any unnecessary delays.
Operative procedure
Traditionally, open appendicectomy has been done through a muscle splitting gridiron incision over McBurney's point made perpendicular to a line joining the umbilicus and anterior superior iliac spine or through a more cosmetically acceptable Lanz's incision. The proportion of open procedures done has fallen with the increased use of laparoscopic techniques. Compared with open surgery, a systematic review found that laparoscopic appendicectomy in adults reduces wound infections, postoperative pain, length of hospital stay, and time taken to return to work, although the number of intra-abdominal abscesses was higher after the laparoscopic approach.17 However, this view is not shared by a recent study, which found no significant differences between the two procedures except higher quality of life scores at two weeks in the laparoscopic group.18 In children, laparoscopic appendicectomy reduced the number of wound infections and the length of hospital stay compared with open surgery, but no significant differences in postoperative pain, time to mobilisation, or proportion of intra-abdominal abscesses were seen.17
Although in the light of these findings laparoscopic appendicectomy is becoming more common, it is often technically more demanding and requires specialist equipment (fig 2). As a result, the method of approach for appendicectomy is dictated by the level of expertise of the operating surgeon and the facilities available. An added advantage of laparoscopic techniques is the ability to do diagnostic laparoscopy initially, which may show alternative pathology as the cause of the presentation.
Fig 2.
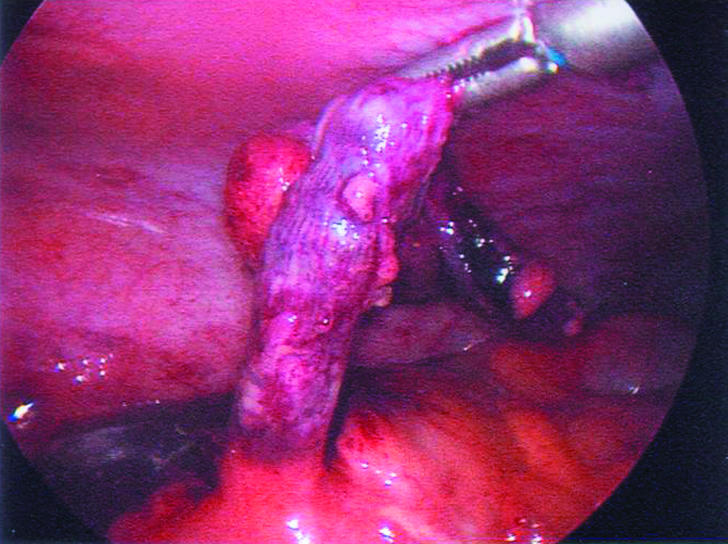
Laparoscopic appendicectomy
Box 3: Differential diagnosis of acute appendicitis
Surgical
Intestinal obstruction
Intussusception
Acute cholecystitis
Perforated peptic ulcer
Mesenteric adenitis
Meckel's diverticulitis
Colonic/appendicular diverticulitis
Pancreatitis
Rectus sheath haematoma
Urological
Right ureteric colic
Right pyelonephritis
Urinary tract infection
Gynaecological
Ectopic pregnancy
Ruptured ovarian follicle
Torted ovarian cyst
Salpingitis/pelvic inflammatory disease
Medical
Gastroenteritis
Pneumonia
Terminal ileitis
Diabetic ketoacidosis
Preherpetic pain on the right 10th and 11th dorsal nerves
Porphyria
Spontaneous resolution of early appendicitis can occur, and antibiotics alone can be used to treat appendicitis if no facilities for appendicectomy are available.19 w15 However, a 14-35% readmission rate was associated with antibiotic treatment, and because of the high recurrence rate and relatively low morbidity and mortality associated with appendicectomy early operative intervention remains the treatment of choice. This study nevertheless does provide support for the immediate starting of intravenous antibiotics once a diagnosis of appendicitis is made and the patient is waiting for theatre.
What are the complications?
Appendicectomy is a relatively safe procedure with a mortality rate for non-perforated appendicitis of 0.8 per 1000.20 The mortality and morbidity are related to the stage of disease and increase in cases of perforation; mortality after perforation is 5.1 per 1000.20 As stated above, the average rate of perforation at presentation is between 16% and 30%,16 w14 but this is significantly increased in elderly people and young children, in whom the rate can be up to 97%, usually because of a delay in diagnosis.w4 w16
The increased mortality and morbidity associated with perforation has been used as justification for high rates of negative appendicectomy, quoted as between 20% and 25%.20 Despite this, complications can occur after removal of a normal appendix, and the surgical community continues to strive to reduce the numbers of negative procedures.w17-w19 According to a large historical cohort study, a perforated appendix during childhood does not seem to have a long term detrimental effect on subsequent female fertility.21
Wound infection
The rate of postoperative wound infection is determined by the intraoperative wound contamination. Rates of infection vary from < 5% in simple appendicitis to 20% in cases with perforation and gangrene. The use of perioperative antibiotics has been shown to decrease the rates of postoperative wound infections.13
Ongoing research
Characterisation of the causes of the condition
Adjuvants to the diagnosis of appendicitis
Tips for GPs
History and findings on examination should form the mainstay of diagnosis of appendicitis
Patients at risk of atypical presentation are those at the extremes of age and pregnant women
Intra-abdominal abscess
Intra-abdominal or pelvic abscesses may form in the postoperative period after gross contamination of the peritoneal cavity. The patient presents with a swinging pyrexia, and the diagnosis can be confirmed by ultrasonography or computed tomography scanning. Abscesses can be treated radiologically with a pigtail drain, although open or per rectal drainage may be needed for a pelvic abscess. The use of perioperative antibiotics has been shown to decrease the incidence of abscesses.13
Special considerations
Pregnancy
The most common non-obstetric emergency needing surgery in pregnancy is appendicitis, with an incidence of 0.15 to 2.10 per 1000 pregnancies.22 Previous studies have suggested an equal incidence in pregnant and non-pregnant women, but a recent large scale case-control study has suggested a reduction in the incidence of appendicitis during pregnancy, particularly during the third trimester.23
Displacement of the appendix by the gravid uterus means that the presentation is often atypical or may be mistaken for the onset of labour. Nausea and vomiting are often present, with associated tenderness located anywhere on the right hand side of the abdomen.
Maternal mortality is negligible in cases of simple appendicitis but rises to 4% with advanced gestation and perforation. Fetal mortality ranges from 0-1.5% incases of simple appendicitis to 20-35% in cases of perforation.22
Additional educational resources
Sauerland S, Lefering R, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 2004;(4):CD001546
Simpson J, Speake W. Appendicitis. Clin Evid 2005;31: 529-35
Information for patients
NHS Direct (www.nhsdirect.nhs.uk/en.aspx?articleId=31§ionId=5579)—Very informative summary that provides links to access health care
Prodigy Knowledge (www.prodigy.nhs.uk/ProdigyKnowledge/PatientInformation/Content/pils/PL437.htm)—Good patient information leaflet offering a brief summary of the condition
National Digestive Diseases Information Clearinghouse (digestive.niddk.nih.gov/ddiseases/pubs/appendicitis/index.htm)—American site with a more comprehensive patient focused explanation of the condition
A patient's perspective
I am a 20 year old student at the University of Nottingham. In March this year I had appendicitis. I had been having stomach pains for a week before I sought medical help. The pains were vague, and the night before I was admitted to hospital they woke me from my sleep and became more prominent on the right lower side. For the entire week I had felt feverish and had been off my food. I had not noticed any other symptoms, and nothing had relieved the pain (not even beer!).
I went to my general practitioner, who promptly diagnosed appendicitis. On admission to hospital I was in considerable pain with a mild fever. The surgical team told me that I needed an operation. I was relieved that a diagnosis had been made and a treatment was available. I had a little discomfort from my scar after the operation and some vomiting, but within two days I was eating and drinking again.
Following my operation the pain resolved, and I am looking forward to returning to my studies.
(Account of a patient with appendicitis who was admitted under the general surgical take at Queen's Medical Centre, Nottingham)
Chronic (recurrent) appendicitis
Recently, with the advent of neurogastroenterology, the concept of neuroimmune appendicitis has evolved. After a previous minor bout of intestinal inflammation, subtle alterations in enteric neurotransmitters are seen, which may result in altered visceral perception from the gut; this process has been implicated in a wide range of gastrointestinal conditions.w21 Further work is needed to determine if the clinical entity of “neuroimmune appendicitis” truly exists, but it remains an interesting area.w22
Inflammatory bowel disease
A history of appendicectomy is associated with delayed onset of disease and a less severe disease phenotype in patients with ulcerative colitis.24 w23 w24 The influence of appendicectomy in Crohn's disease is not as clear; some evidence suggests a delayed onset of disease in patients after appendicectomy,w23 w25 although contradictory evidence also exists to suggest an increased risk of developing the condition depending on the patient's age, sex, and diagnosis at the time of operation.25
Supplementary Material
Appendix mass
In patients with a delayed presentation, a tender mass with overlying muscle rigidity may be felt in the right iliac fossa. The presence of a mass may be confirmed on ultrasonography or computed tomography scan; underlying neoplasia must be excluded, especially in elderly people. The initial treatment in a patient who is otherwise well is conservative, with initiation of appropriate resuscitation and intravenous broad spectrum antibiotics. In most cases the mass will decrease in size over the subsequent days as the inflammation resolves, although patients need careful observation to detect early signs of progress of the inflammatory process. As appendicitis can recur, management after resolution of the mass is usually an interval appendicectomy; a conservative approach with outpatient follow-up has been suggested, but no definitive evidence exists to support this.w20
Appendix abscess
Patients with an appendix abscess have a tender mass with a swinging pyrexia, tachycardia, and leucocytosis. The abscess is most often located in the lateral aspect of the right iliac fossa but may be pelvic; a rectal examination is useful to identify a pelvic collection. The abscess can be shown by ultrasonography or computed tomography scanning, and a percutaneous radiological drainage may be done. Open drainage has the added advantage of allowing an appendicectomy to be done.w20
 References w1-w25 are on bmj.comContributors: Both authors reviewed the literature and wrote the article.
References w1-w25 are on bmj.comContributors: Both authors reviewed the literature and wrote the article.
Competing interests: None declared.
References
- 1.Larner AJ. The aetiology of appendicitis. Br J Hosp Med 1988;39: 540-2. [PubMed] [Google Scholar]
- 2.Hospital Episode Statistics. Primary diagnosis: summary. www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937&categoryID=202 (accessed 28 Aug 2006).
- 3.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990;132: 910-25. [DOI] [PubMed] [Google Scholar]
- 4.Murphy J. Two thousand operations for appendicitis, with deductions from his personal experience. Am J Med Sci 1904;128: 187-211. [Google Scholar]
- 5.Andersson R. Meta-analysis of the clinical and laboratory diagnosis of appendicitis. Br J Surg 2004;91: 28-37. [DOI] [PubMed] [Google Scholar]
- 6.McBurney C. Experiences with early operative interference in cases of diseases of the vermiform appendix. N Y Med J 1889;50: 676-84. [Google Scholar]
- 7.Terasawa T, Blackmore CC, Bent S, Kohlwes RJ. Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med 2004;141: 537-46. [DOI] [PubMed] [Google Scholar]
- 8.Cobben LP, Groot I, Haans L, Blickman JG, Puylaert J. MRI for clinically suspected appendicitis during pregnancy. Am J Roentgenol 2004;183: 671-5. [DOI] [PubMed] [Google Scholar]
- 9.Weston A, Jackson T, Blamey S. Diagnosis of appendicitis in adults by ultrasonography or computed tomography: a systematic review and meta-analysis. Int J Technol Assess Health Care 2005;21: 368-79. [DOI] [PubMed] [Google Scholar]
- 10.Flum DR, McClure TD, Morris A, Koepsell T. Misdiagnosis of appendicitis and the use of diagnostic imaging. J Am Coll Surgeons 2005;201: 933. [DOI] [PubMed] [Google Scholar]
- 11.Fitz R. Perforating inflammation of the vermiform appendix, with special reference to its early diagnosis and treatment. Trans Assoc Am Physicians 1886;1: 107-44. [Google Scholar]
- 12.Thomas SH, Silen W. Effect on diagnostic efficiency of analgesia for undifferentiated abdominal pain. Br J Surg 2003;90: 5-9. [DOI] [PubMed] [Google Scholar]
- 13.Andersen BR, Kallehave FL, Andersen HK. Antibiotics versus placebo for prevention of postoperative infection after appendicectomy. Cochrane Database Syst Rev 2005;(3):CD001439. [DOI] [PMC free article] [PubMed]
- 14.Abou-Nukta F, Bakhos C, Arroyo K, Koo Y, Martin J, Reinhold R, et al. Effects of delaying appendectomy for acute appendicitis for 12 to 24 hours. Arch Surg 2006;141: 504-7. [DOI] [PubMed] [Google Scholar]
- 15.Temple CL, Huchcroft SA, Temple WJ. The natural history of appendicitis in adults: a prospective study. Ann Surg 1995;221: 278-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bickell NA, Aufses JAH, Rojas M, Bodian C. How time affects the risk of rupture in appendicitis. J Am Coll Surg 2006;202: 401-6. [DOI] [PubMed] [Google Scholar]
- 17.Sauerland S, Lefering R, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 2004;(4):CD001546. [DOI] [PubMed]
- 18.Katkhouda N, Mason RJ, Towfigh S, Gevorgyan A, Essani R. Laparoscopic versus open appendectomy: a prospective randomized double-blind study. Ann Surg 2005;242: 439-48, discussion 448-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Styrud J, Eriksson S, Nilsson I, Ahlberg G, Haapaniemi S, Neovius G, et al. Appendectomy versus antibiotic treatment in acute appendicitis: a prospective multicenter randomized controlled trial. World J Surg 2006;30: 1033. [DOI] [PubMed] [Google Scholar]
- 20.Blomqvist PG, Andersson RE, Granath F, Lambe MP, Ekbom AR. Mortality after appendectomy in Sweden, 1987-1996. Ann Surg 2001;233: 455-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Andersson R, Lambe M, Bergstrom R. Fertility patterns after appendicectomy: historical cohort study. BMJ 1999;318: 963-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guttman R, Goldman RD, Koren G. Appendicitis during pregnancy. Can Fam Physician 2004;50: 355-7. [PMC free article] [PubMed] [Google Scholar]
- 23.Andersson REB, Lambe M. Incidence of appendicitis during pregnancy. Int J Epidemiol 2001;30: 1281-5. [DOI] [PubMed] [Google Scholar]
- 24.Andersson RE, Olaison G, Tysk C, Ekbom A. Appendectomy and protection against ulcerative colitis. N Engl J Med 2001;344: 808-14. [DOI] [PubMed] [Google Scholar]
- 25.Andersson RE, Olaison G, Tysk C, Ekbom A. Appendectomy is followed by increased risk of Crohn's disease. Gastroenterology 2003;124: 40. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


