Abstract
Opsonophagocytic killing assays (OPAs) are essential for developing and improving pneumococcal vaccines. There is a need for a high-throughput, reliable, standardized, and fully characterized OPA for pneumococcal antibodies. To meet the need, we have developed and characterized a fourfold multiplexed OPA (MOPA4) against 13 serotypes (1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, and 23F) of pneumococci. Thirteen target bacteria were made resistant to only one of the following antibiotics: optochin, streptomycin, spectinomycin, and trimethoprim. Following optimization of assay conditions, accuracy of MOPA4 was determined by testing 30 sera from old adults in the MOPA4 and the single-serotype assays. The opsonization titers obtained with both assays agreed well (r2 > 0.95). Although 22 (out of 390; ∼6%) results differed more than twofold, the differences were not reproducible. The assay was specific: preabsorbing test sera with homologous polysaccharide (PS) completely abrogated opsonic activity, but a pool of unrelated PS (5 μg/ml of each) had no effect. Intra- and interassay coefficients of variation were 10 and 22%, respectively. MOPA4 results were unaffected by having different target pneumococcal serotypes in each assay group. Also, HL60 cell-to-bacteria ratios could be varied twofold without affecting the results. We conclude that MOPA4 is sensitive, accurate, specific, precise, and robust enough for large-scale clinical studies. Furthermore, MOPA4 should allow evaluation of multivalent pneumococcal vaccines with the limited volume of serum typically available from young children.
Streptococcus pneumoniae is a significant human pathogen, primarily for young children and elderly adults (4). A pneumococcal vaccine effective for these two target populations is therefore highly desirable. To obtain such a vaccine, there are active efforts to improve currently available vaccines, which are designed to elicit antibodies to pneumococcal capsular polysaccharide (PS). A 23-valent pneumococcal PS vaccine (PPV23) contains capsular PS of 23 different serotypes and is widely used for the elderly (15). Because PPV23 is not useful for young children, a 7-valent pneumococcal conjugate vaccine (PCV7) was developed (14, 21), and its use has significantly reduced the incidence of invasive pneumococcal infections (20, 23). To extend the serotypic coverage of PCV7, 10- and 13-valent conjugate vaccines are now in late stages of development.
The development or improvement of pneumococcal vaccines requires measuring their immunogenicity, determined primarily by measuring anticapsular PS antibody levels with the use of enzyme-linked immunosorbent assay (ELISA). Use of the pneumococcal antibody ELISA has established that an antibody level of 0.35 μg/ml is associated with protection from invasive pneumococcal infections in children (7). However, old adults generally have more than 0.35 μg/ml of pneumococcal antibodies and yet are susceptible to pneumococcal infections (16, 19). Thus, old adults may have nonfunctional pneumococcal antibodies (18), and ELISA for pneumococcal antibodies may be inadequate to accurately measure immunogenicity of pneumococcal vaccines in the elderly. It is preferable to measure the protective capacity of pneumococcal antibodies directly.
Since antibodies to pneumococcal capsular PS protect the host by opsonizing pneumococci for phagocytes, the opsonophagocytic killing assay (OPA) has been widely accepted as the reference method for measuring the protective capacity of pneumococcal antibodies (16). Because pneumococcal vaccines contain many (7 to 23) serotypes, a comprehensive evaluation requires many OPAs to be performed. Since many vaccine studies involve infants, only a small amount of serum is available for such analyses. To overcome these limitations, we have demonstrated the feasibility of a multiplexed OPA with antibiotic-resistant pneumococci as target bacteria (9, 11). To help meet the need for a practical assay useful for large-scale pneumococcal vaccine evaluations, we have now developed, optimized, and validated a fourfold multiplexed OPA (MOPA4) for 13 serotypes.
MATERIALS AND METHODS
Bacteria.
Thirteen different antibiotic-resistant strains used for the assay and their wild-type origins are described in Table 1. Table 1 also shows the concentrations of the four antibiotics used in the assay (all purchased from Sigma, St. Louis, MO). Wild-type strains DBL5, L82006, BG25-9, and EF6796 came from D. Briles at the University of Alabama at Birmingham. EMC23F (strain 1212458) and EMC9V (derived from strain 1081748) were provided by P. Hermans in The Netherlands (2). Wu2 was previously described (3). All other wild-type strains came from G. Carlone at the Centers for Disease Control and Prevention (Atlanta, GA).
TABLE 1.
Bacteria strain composition of opsonization assay groups and their antibiotic resistance
| Assay group | Assay group strain no.a
|
|||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| A | OREP4 (DS2382-94) | SPEC6B (BG25-9) | STREP14 (DS2214-94) | TREP19A (DS3519-97) |
| B | OREP18C (GP116) | SPEC19F (DS2217-94) | EMC9V (1081748) | EMC23F (1212458) |
| C | OREP7F (DS2617-97) | SPEC1 (L82006) | STREP5 (DBL5) | TREP6A (EF6796) |
| D | OREP3 (Wu2) | None | None | None |
The names of the wild-type strains are included in parentheses. The antibiotics (and concentrations in overlay) used were the following: strain 1, optochin (2 μg/ml); strain 2, spectinomycin (150 μg/ml); strain 3, streptomycin (250 μg/ml); strain 4, trimethoprim (25 μg/ml).
EMC23F was a clinical isolate naturally resistant to trimethoprim only, but the remaining 12 strains listed in Table 1 were derived from the wild-type strains by selecting natural variants resistant to increasing concentrations of antibiotics as described before (2, 11). In addition to the 13 strains listed in Table 1, OREP19F and STREP23F, which were described previously (9), were used to evaluate washing of the target bacteria for OPA.
Phagocytes.
HL60 cells were originally obtained from ATCC (catalog no. CCL-240, lot no. 3346359; Manassas, VA) and were cryopreserved (5). An aliquot of HL60 cells was thawed and propagated up to 6 months in culture medium (CM), consisting of RPMI 1640 with 10% fetal bovine serum (FBS) (Fetalclone I; HyClone, Logan, UT) and 1% l-glutamine. To obtain phagocytes for the OPA, HL60 cells were differentiated for 5 to 6 days in CM with 0.8% dimethyl formamide at a starting density of 4 × 105 cells/ml.
Serum samples.
Pool 18 was prepared by mixing sera from three adult donors who were vaccinated with a 23-valent PS vaccine. Pool 20 was prepared from equal volumes of 180 elderly individuals who had been vaccinated with either a PPV23 (Merck, West Point, PA) or 9-valent conjugate vaccine (Wyeth Vaccines, Rochester, NY). Pool 22 was made by pooling two outdated plasma samples from a blood bank and converting the pool to serum using thromboplastin. Thirty single-donor serum samples used throughout this study were obtained from old adults (more than 65 years old). Five of these sera were obtained prevaccination, and the remainders were collected 4 months after vaccination with a PPV23. All serum samples and pools contained no antibiotics, as judged by their inability to inhibit growth of a rough strain of pneumococcus (R36A). The serum samples were collected and used following the guidelines approved by the institutional review board.
Rabbit complement.
Several lots of complement from 3- to 4-week-old rabbits (PelFreeze Biologicals, Rogers, Arkansas) were tested for opsonophagocytic killing of the 13 strains in the absence of human sera (see Results) using the MOPA4 procedure described below. Lots demonstrating less than 30% nonspecific killing were selected.
OPA.
All serum samples were incubated at 56°C for 30 min before serial dilutions. Serially diluted serum samples (20 μl/well) were tested in duplicate in round-bottom 96-well plates (Corning Inc., Corning, NY). Eleven 2.3-fold serial dilutions were used for interassay variability experiments, and eight threefold dilutions were used for all other experiments. Frozen aliquots of target pneumococci were thawed, washed twice (unless otherwise indicated) with opsonization buffer B (Hanks' balanced salt solution [HBSS] with Mg and Ca, 0.1% gelatin, and 10% FBS) by centrifugation (12,000 × g, 2 min), and diluted to the proper bacterial density (∼105 CFU/ml for single-serotype assays and ∼2 × 105 CFU/ml of each serotype for multiplexed assays). For MOPA4, equal volumes of four bacterial suspensions in one assay group were pooled. Ten microliters of bacterial suspension was added to each well.
After 30 min of incubation at room temperature, 10 μl of complement and 40 μl of HL60 cells were added to each well. HL60 cells were washed twice before use with HBSS by centrifugation (350 × g, 5 min), and 4 × 105 cells were added to each well (unless otherwise indicated). Plates were incubated in a tissue culture incubator (37°C, 5% CO2) with shaking (mini orbital shaker; Bellco Biotechnology, Vineland, NJ) at 700 rpm. After a 45-min incubation, plates were placed on ice for 10 to 15 min and an aliquot of the final reaction mixture (5 μl for single-serotype assays, 10 μl for all other assays) was spotted onto four different Todd-Hewitt broth-yeast extract (0.5%) agar plates for MOPA4 (9). After application of an overlay agar containing one of the four antibiotics to each Todd-Hewitt broth-yeast extract (0.5%) agar plate and overnight incubation at 37°C, the number of bacterial colonies in the agar plates was enumerated (9). Opsonization titers (OT) were defined as the serum dilution that kills 50% of bacteria (9). A detailed protocol is posted at a website (www.vaccine.uab.edu).
RESULTS
(i) Development of target bacterial strains.
The 13 pneumococcal isolates that were selected as target bacteria (summarized in Table 1) were made resistant to one of the four antibiotics (optochin, spectinomycin, streptomycin, or trimethoprim). All strains were resistant to the antibiotic used for the selection, even at twofold-higher antibiotic concentrations than those used in the assay, but they were sensitive to the other three antibiotics, even at half the concentration used in the assay. All strains were sensitive to many other antibiotics. Commercially available antibiotic disks (Sensi-disc; Becton Dickinson and Company, Sparks, MD) containing erythromycin, cefotaxime, clindamycin, tetracycline, vancomycin, or oxacillin produced a large zone of growth inhibition in blood agar plates. OREP18C consistently displayed a mixture of transparent and opaque colonies, whereas all other strains were predominately (>98%) opaque.
(ii) Assay optimization.
To develop a reliable OPA, many analytical parameters were investigated and optimized. Various amounts of free capsular PS are present in target bacterial preparations, and the PS can function as a competitive inhibitor even at a very low concentration (<1 μg/ml) (6). We found that the washing of target bacteria reduced variability in assay sensitivity associated with using different preparations of target bacteria (data not shown). Hu et al. reported that assay plates for OPA required a unique shaking rate for each serotype (6). Since MOPA includes multiple serotypes simultaneously, one cannot employ serotype-specific shaking speeds. After investigating different shakers, we found that a shaker with a small shaking radius could produce comparable opsonization titers for all serotypes at shaking speeds from 650 to 800 rpm (data not shown). The shaker and 700 rpm were chosen for MOPA4.
A major difficulty in OPA is in nonspecific killing of pneumococci by rabbit serum that is used as a source of complement. For some serotypes, especially 6A, 6B, and 14, many lots of rabbit serum had a high level (≥50%) of nonspecific killing (data not shown). Nonspecific killing was defined as 100 × [1 − (CFU in wells containing rabbit serum and HL60)/(CFU in wells with bacteria alone)]. All CFU were determined at the end of the assay due to bacterial growth during the assay. Nonspecific killing was considerably reduced when the phagocytosis phase of the assay was performed in air containing 5% CO2 (data not shown). For all subsequent assays, the phagocytosis for phase was performed in air with 5% CO2.
(iii) Assay validation. (a) Specificity.
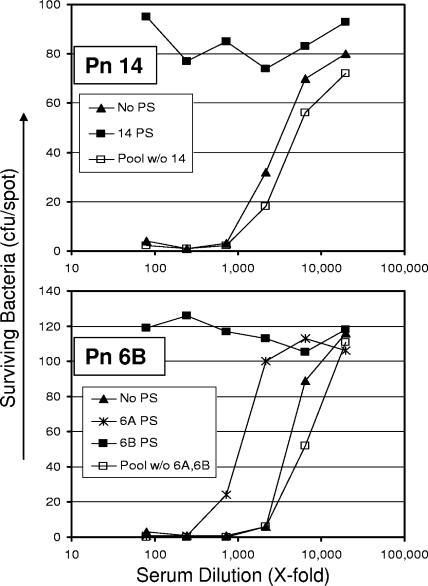
Once the assay conditions were optimized, we investigated assay specificity by neutralizing a serum pool with homologous PS (5 μg/ml), a pool of heterologous capsular PS (5 μg/ml of each), or with no PS before being tested in OPA (Fig. 1). Heterologous PS pools contained PS from all 13 serotypes, except for the homologous PS and PS from the same serogroup. For instance, the heterologous pool for 6B did not contain 6B and 6A PS but contained the remaining 11 PSs; for serotype 14, the heterologous PS pool contained 12 other PSs (all except for serotype 14). Evaluation was performed for all 13 serotypes using MOPA4, and two representative results are shown in Fig. 1. For serotype 14, the heterologous pool did not inhibit the opsonic capacity of the serum pool, but serotype 14 PS completely abrogated the opsonic capacity (upper panel). In the case of serotype 6B, opsonic activity was completely abrogated by 6B PS, reduced (∼3-fold) by 6A PS, and unaffected by the heterologous PS mixture (lower panel). These data indicate that the multiplexed OPA is serotype specific.
FIG. 1.
Number of surviving bacteria (y axis) at various dilutions of serum (x axis). Serotype of pneumococci (Pn) was serotype 14 (top panel) or serotype 6B (bottom panel). For the top panel, the serum sample was absorbed with nothing (solid triangle), 5 μg/ml of serotype 14 PS (solid square), or a mixture of heterologous PS (open square). For the bottom panel, the serum sample was absorbed with nothing (solid triangle), 5 μg/ml of serotype 6B PS (solid square), 5 μg/ml of serotype 6A PS (symbol “X”), or a mixture of heterologous PS (open square). The heterologous PS pool had PS (5 μg/ml each) of all the unrelated serotypes, but PS of cross-reactive serotypes was omitted for serotypes 6A, 6B, 19A, and 19F. The cross-reactive PS was tested separately (also at 5 μg/ml). w/o, without.
(b) Accuracy.
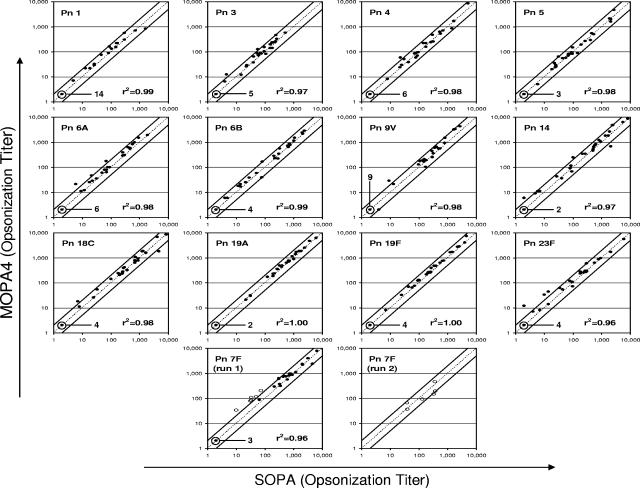
A primary concern with the multiplexed OPA was its ability to produce results comparable to those with the single-serotype OPA. To address this issue, 30 serum samples (5 prevaccination, 25 postvaccination) were tested in the single-serotype OPA format and the MOPA4 format (Fig. 2). The data for all 13 serotypes are shown in Fig. 2 along with the line of identity (dotted line) and lines showing twofold deviation (solid lines) from the identity for each serotype. The data obtained from each format agreed very well, and only 22 data points out of 390 data points (13 serotypes/sample × 30 samples) deviated more than twofold (i.e., outside of the two solid lines). Since six outlier data points were found in 7F serotype (run 1), we investigated potential difficulties in the 7F assay by retesting the six samples. Upon retesting (run 2), the six samples produced comparable results (Fig. 2, bottom two panels). Thus, we believe the outliers were not due to assay inaccuracy but rather random errors.
FIG. 2.
Comparison of opsonization titers of 30 serum samples determined with MOPA4 (y axis) and with single-serotype OPA (SOPA) (x axis). Each panel contains an identity line (dotted line) and two lines indicating twofold deviation from identity (solid lines). The serotypes and the r2 values are indicated in each panel. In the bottom row of the panels, two panels show comparisons for serotype 7F. In run 1, six samples (open circles) showed a more-than-twofold deviation, but their results deviated less than twofold in run 2. In most panels, several samples had opsonization titers below the detection limit, which was 4. These samples were assigned an opsonization titer of 2, and the number of such serum samples is indicated in each panel. Pn, pneumococcal serotype.
(c) Precision.
Intra-assay variation for the 13 serotypes was assessed by testing a serum pool 10 times in a single assay run. As shown in Table 2, the average coefficient of variation (CV) was about 10%, ranging from 4% to 19%. Interassay variation was estimated for the 13 serotypes by testing several sera in six independent experiments over a 2-week interval (Table 2). For this study, the same lot of target bacteria and lot of complement were used for each assay. Under these conditions, the overall average CV of the serum samples for 13 serotypes was 22%. No specific serotypes could be associated with high CV. There was a slight trend for high CVs for samples with high OT, suggesting that serial dilution errors of these samples may slightly increase the imprecision. Two cases with high CVs (≥50%) were observed with one sample (pool 22) but not with other samples. Pool 22 was made by converting plasma to serum, whereas all other samples were collected as serum. Thus, the high CVs may be associated with the sample (pool 22) itself rather than the assay.
TABLE 2.
Intra- and interassay precision of MOPA4a
| Serotype | CVb (name of serum)
|
||||
|---|---|---|---|---|---|
| Intra-assay | Interassay | ||||
| Pn 1 | 7 (S1) | 38 (P22) | 13 (S1) | 42 (S3) | 31 (S5) |
| Pn 3 | 9 (S1) | 50 (P22) | 21 (S1) | 20 (S6) | 21 (S7) |
| Pn 4 | 6 (P20) | 14 (P22) | 10 (S1) | NA (S2) | 21 (P18) |
| Pn 5 | 4 (S1) | 25 (P22) | 7 (S1) | 6 (S3) | 28 (S5) |
| Pn 6A | 14 (S1) | 42 (P22) | 20 (S1) | NA (S3) | 32 (S5) |
| Pn 6B | 9 (P20) | 22 (P22) | 22 (S1) | 19 (S2) | 18 (P18) |
| Pn 7F | 10 (S1) | 66 (P22) | 27 (S1) | 19 (S3) | 34 (S5) |
| Pn 9V | 16 (P20) | 22 (P22) | 19 (S1) | 30 (S4) | 14 (P18) |
| Pn 14 | 19 (P20) | 32 (P22) | 7 (S1) | 34 (S2) | 40 (P18) |
| Pn 18C | 15 (P20) | 8 (P22) | 6 (S1) | 7 (S4) | 4 (P18) |
| Pn 19A | 11 (P20) | 23 (P22) | 9 (S1) | 12 (S2) | 18 (P18) |
| Pn 19F | 6 (P20) | 13 (P22) | 16 (S1) | 15 (S4) | 24 (P18) |
| Pn 23F | 9 (P20) | 6 (P22) | 24 (S1) | 12 (S4) | 13 (P18) |
CV is expressed in percentages. NA (not applicable) was used when the sample had results below the detection limit for the serotype. The name of the serum sample is listed in parenthesis. P18, P20, and P22 indicate pool 18, pool 20, and pool 22, respectively. S1 through S7 indicate single-donor serum 1 through serum 7, respectively. These sera were postvaccination sera.
Intra-assay average CV, 10%; interassay average CV, 22%. When the interassay CV was determined with the samples diluted only once, the interassay CV could be reduced to 15%. The average intra-assay CV was determined from 10 experiments; the average interassay CV was determined from 6 experiments.
(iv) Effect of different E:T ratios.
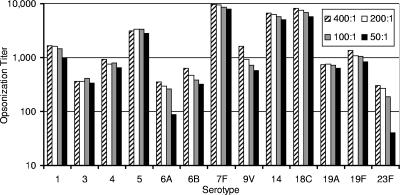
As a part of assessing the robustness of MOPA4, we determined the effect of different numbers of HL60 cells in each well (8 × 105, 4 × 105, 2 × 105, or 1 × 105 cells/well) by performing OPA for all 13 serotypes (serotype 3 in single-serotype OPA format, other serotypes in MOPA4 format) with one serum sample (serum 1) with a constant number of bacteria (500 CFU/well of each strain) per well (Fig. 3). The OT for most serotypes tended to decrease as effector-to-target (E:T) ratios were reduced from 400:1 to 100:1, but the reduction was modest. When an E:T ratio of 200:1 was compared to 400:1, the maximum OT reduction for all serotypes was less than 20%, except serotypes 6B (25%) and 9V (44%). When an E:T ratio of 100:1 was compared to 200:1, the maximal reduction in OT was 29% for 23F and 21% for 9V but remained less than 20% for all other serotypes. When the E:T ratio was reduced to 50:1, however, the reduction in OT was more pronounced and occurred in multiple serotypes. The reduction, however, was not consistently reproduced (data not shown). For the 13 serotypes, the average OT at 200:1 was 86% of that obtained at 400:1, and the average OT at 100:1 was 92% of that at 200:1. These data show that the E:T ratio of 200:1 used in the MOPA4 produces results comparable to the conventional ratio of 400:1 and has an adequate margin of safety (twofold).
FIG. 3.
Opsonization titers of one serum sample for 13 serotypes with the E:T ratio of 400:1 (hatched bars), 200:1 (open bars), 100:1 (gray bars), or 50:1 (black bars). Because serotype 3 is an odd member, it was tested in the single-serotype OPA format. All other serotypes were tested in MOPA4 format. Since opsonization titers for serotypes 6A, 9V, and 23F displayed a marked trend of decreasing opsonization titers with decreasing E:T ratios, the experiment was repeated for these three serotypes. This trend was not reproducible (data not shown).
DISCUSSION
To accommodate large demands for OPA, we have developed and optimized a fourfold multiplexed OPA (MOPA4) for pneumococcal antibodies against 13 serotypes. Once optimized, MOPA4 was found to be robust: assay conditions could be varied slightly without significant changes in assay results. Above all, E:T ratios can be changed twofold with little variation in results. In addition, we found that opsonization titers obtained by MOPA4 did not change when the assay was performed with a different combination of pneumococcal serotypes (r2 > 0.98) (data not shown). Also, the degree of multiplexing was not significant, and we could obtain comparable results with the twofold, threefold, and fourfold MOPA (data not shown).
MOPA4 was validated by investigating the assay's precision, accuracy, and specificity. Not surprisingly, the assay was found to be highly specific. Since no OPA standards with assigned values are currently available, we assessed the assay's accuracy by comparing MOPA4 results with those obtained with a single-serotype OPA. Both assays were found to yield similar results, and deviations from the identity were less than twofold in most samples in our comparison studies. Although MOPA4 gave slightly higher results than the single-serotype OPA in serotype 7F for several samples with low titers, the difference was not reproducible. In the future, we plan to compare our MOPA4 with other single-serotype OPAs by studying samples from vaccinated children and exchanging samples with other laboratories that perform single-serotype OPAs.
Under our assay conditions, we found the MOPA4 to be precise, with an interassay CV of about 20%. Indeed, this level of CV is comparable to those observed for ELISA results (12). Since this is short-term interassay precision, assay precision would be reduced as the assay is performed for a longer period using different batches of bacteria and complement. Thus, we are investigating various approaches to improve precision further, such as the use of a standard serum for each assay and a data analysis program that would utilize data obtained at all serum dilutions. With these improvements, we believe that MOPA4 would become as precise as ELISA, even though MOPA4 is a bioassay.
It is difficult to demonstrate assay sensitivity, because there are no established OPA standards. Since most serum samples obtained after a vaccination have measurable opsonization titers, our MOPA4 appears to have adequate assay sensitivity. However, assay sensitivity may depend on target bacteria, since we observed up to 5- to 10-fold variation in the magnitude of opsonization titers when different target bacteria were used (unpublished observation). Interstrain variation may occur because strains produce different amounts of capsule, express different phases (8), or differ in the expression of molecules affecting complement deposition on the bacterial surface (13). Due to these considerations, a set of target strains of pneumococci should be adopted as the standard. We plan to make our antibiotic-resistant bacteria available to qualified investigators.
Since pneumococci are pathogens, the safety of using antibiotic-resistant pneumococci should be a concern. However, MOPA4 uses antibiotics that are not relevant to managing pneumococcal infections. Also, we used natural antibiotic resistance by pneumococci and did not insert “antibiotic resistance” genes which could be transferred to other bacteria. In addition, we used an overlay method which seals the pneumococci within the agar plate and prevents exposure of the pathogen to the air. In addition to reducing biohazard, we found the overlay kept the colony size of type 3 pneumococci small. In conventional OPA, because of their large colony size, type 3 pneumococci required large agar surfaces, and this caused significant practical problems. Although the antibiotics we used do not pose serious safety concerns, one may develop target bacterial strains that depend on specific nutrient factors. In this way, the multiplex assay can be performed without using antibiotics.
Because of its importance in pneumococcal vaccine development, various multiplexed opsonization assay formats have been developed (2, 9-11). While we have described here a killing-type multiplexed opsonization assay, Martinez et al. developed a flow-cytometric multiplexed opsonization assay (10). This approach uses, in place of target pneumococci, a mixture of latex particles that have distinct fluorescent characteristics and are coated with different capsular PSs. The particles are opsonized with antisera and complement, and their uptake into phagocytes is then determined with a flow cytometer. The flow-cytometric assay uses artificial targets instead of bacteria, measures phagocytosis but not actual killing, requires an expensive instrument, and requires more hands-on effort than the opsonophagocytic killing assay employing automated colony counting. Also, a killing-type multiplexed opsonization assay is similar to the conventional opsonization assay used as the reference assay in the past (17). Thus, multiplexed opsonophagocytic killing assays may be easier to adopt and validate than the multiplexed phagocytosis assay. Nevertheless, these multiplexed opsonization assays may be robust and rapid enough to replace pneumococcal antibody ELISA, which may not be specific for functional antibodies (1, 18, 22).
Acknowledgments
The work was supported by an NIH contract (AI-30021) from NIH/NIAID/DMID.
REFERENCES
- 1.Bhushan, R., B. F. Anthony, and C. E. Frasch. 1998. Estimation of group B streptococcus type III polysaccharide-specific antibody concentrations in human sera is antigen dependent. Infect. Immun. 66:5848-5853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bogaert, D., M. Sluijter, R. De Groot, and P. W. Hermans. 2004. Multiplex opsonophagocytosis assay (MOPA): a useful tool for the monitoring of the 7-valent pneumococcal conjugate vaccine. Vaccine 22:4014-4020. [DOI] [PubMed] [Google Scholar]
- 3.Briles, D. E., M. Nahm, K. Schroer, J. Davie, P. Baker, J. Kearney, and R. Barletta. 1981. Antiphosphocholine antibodies found in normal mouse serum are protective against intravenous infection with type 3 Streptococcus pneumoniae. J. Exp. Med. 153:694-705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fedson, D. S., and D. M. Musher. 1994. Pneumococcal vaccine, p. 517-564. In S. A. Plotkin and E. A. Mortimer (ed.), Vaccines, 2nd ed. W. B. Saunders Co., Philadelphia, Pa.
- 5.Fleck, R. A., S. Romero-Steiner, and M. H. Nahm. 2005. Use of HL-60 cell line to measure opsonic capacity of pneumococcal antibodies. Clin. Diagn. Lab. Immunol. 12:19-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu, B. T., X. Yu, T. R. Jones, C. Kirch, S. Harris, S. W. Hildreth, D. V. Madore, and S. A. Quataert. 2005. Approach to validating an opsonophagocytic assay for Streptococcus pneumoniae. Clin. Diagn. Lab. Immunol. 12:287-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jodar, L., J. C. Butler, G. Carlone, R. Dagan, C. E. Frasch, D. Goldblatt, H. Käyhty, K. Klugman, B. D. Plikaytis, G. Siber, R. Kohberger, I. Chang, and T. Cherian. 2003. Serological criteria for evaluation and licensure of pneumococcal conjugate vaccine formultions for use in infants. Vaccine 21:3265-3272. [DOI] [PubMed] [Google Scholar]
- 8.Kim, J. O., S. Romero-Steiner, U. B. Sorensen, J. Blom, M. Carvalho, S. Barnard, G. Carlone, and J. N. Weiser. 1999. Relationship between cell surface carbohydrates and intrastrain variation on opsonophagocytosis of Streptococcus pneumoniae. Infect. Immun. 67:2327-2333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim, K. H., J. Yu, and M. H. Nahm. 2003. Efficiency of a pneumococcal opsonophagocytic killing assay improved by multiplexing and by coloring colonies. Clin. Diagn. Lab. Immunol. 10:616-621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martinez, J. E., E. A. Clutterbuck, H. Li, S. Romero-Steiner, and G. M. Carlone. 2006. Evaluation of multiplex flow cytometric opsonophagocytic assays for determination of functional anticapsular antibodies to Streptococcus pneumoniae. Clin. Vaccine Immunol. 13:459-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nahm, M. H., D. E. Briles, and X. Yu. 2000. Development of a multi-specificity opsonophagocytic killing assay. Vaccine 18:2768-2771. [DOI] [PubMed] [Google Scholar]
- 12.Plikaytis, B. D., D. Goldblatt, C. E. Frasch, C. Blondeau, M. J. Bybel, G. S. Giebink, I. Jonsdottir, H. Kayhty, H. B. Konradsen, D. V. Madore, M. H. Nahm, C. A. Schulman, P. F. Holder, T. Lezhava, C. M. Elie, and G. M. Carlone. 2000. An analytical model applied to a multicenter pneumococcal enzyme-linked immunosorbent assay study. J. Clin. Microbiol. 38:2043-2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ren, B., A. J. Szalai, S. K. Hollingshead, and D. E. Briles. 2004. Effects of PspA and antibodies to PspA on activation and deposition of complement on the pneumococcal surface. Infect. Immun. 72:114-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rennels, M. B., K. M. Edwards, H. L. Keyserling, K. S. Reisinger, D. A. Hogerman, D. V. Madore, I. Chang, P. R. Paradiso, F. J. Malinoski, and A. Kimura. 1998. Safety and immunogenicity of heptavalent pneumococcal vaccine conjugated to CRM197 in United States infants. Pediatrics 101:604-611. [DOI] [PubMed] [Google Scholar]
- 15.Robbins, J. B., R. Austrian, C. J. Lee, S. C. Rastogi, G. Schiffman, J. Henrichsen, P. H. Makela, C. V. Broome, R. R. Facklam, R. H. Tiesjema, and J. C. Parke, Jr. 1983. Considerations for formulating the second-generation pneumococcal capsular polysaccharide vaccine with emphasis on the cross-reactive types within groups. J. Infect. Dis. 148:1136-1159. [DOI] [PubMed] [Google Scholar]
- 16.Romero-Steiner, S., C. E. Frasch, G. Carlone, R. A. Fleck, D. Goldblatt, and M. H. Nahm. 2006. Use of opsonophagocytosis for the serological evaluation of pneumococcal vaccines. Clin. Vaccine Immunol. 13:165-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Romero-Steiner, S., D. Libutti, L. B. Pais, J. Dykes, P. Anderson, J. C. Whitin, H. L. Keyserling, and G. M. Carlone. 1997. Standardization of an opsonophagocytic assay for the measurement of functional antibody activity against Streptococcus pneumoniae using differentiated HL-60 cells. Clin. Diagn. Lab. Immunol. 4:415-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Romero-Steiner, S., D. M. Musher, M. S. Cetron, L. B. Pais, J. E. Groover, A. F. Fiore, B. D. Plikaytis, and G. M. Carlone. 1999. Reduction in functional antibody activity against Streptococcus pneumoniae in vaccinated elderly individuals highly correlates with decreased IgG antibody avidity. Clin. Infect. Dis. 29:281-288. [DOI] [PubMed] [Google Scholar]
- 19.Rubins, J. B., M. Alter, J. Loch, and E. N. Janoff. 1999. Determination of antibody responses of elderly adults to all 23 capsular polysaccharides after pneumococcal vaccination. Infect. Immun. 67:5979-5984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shinefield, H. R., and S. Black. 2000. Efficacy of pneumococcal conjugate vaccines in large scale field trials. Pediatr. Infect. Dis. J. 19:394-397. [DOI] [PubMed] [Google Scholar]
- 21.Shinefield, H. R., S. Black, P. Ray, I. Chang, N. Lewis, B. Fireman, J. Hackell, P. R. Paradiso, G. Siber, R. Kohberger, D. V. Madore, F. J. Malinowski, A. Kimura, C. Le, I. Landaw, J. Aguilar, and J. Hansen. 1999. Safety and immunogenicity of heptavalent pneumococcal CRM197 conjugate vaccine in infants and toddlers. Pediatr. Infect. Dis. J. 18:757-763. [DOI] [PubMed] [Google Scholar]
- 22.Wernette, C. M., C. E. Frasch, D. Madore, G. Carlone, D. Goldblatt, B. Plikaytis, W. Benjamin, S. A. Quataert, S. Hildreth, D. J. Sikkema, H. Kayhty, I. Jonsdottir, and M. H. Nahm. 2003. Enzyme-linked immunosorbent assay for quantitation of human antibodies to pneumococcal polysaccharides. Clin. Diagn. Lab. Immunol. 10:514-519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Whitney, C. G., M. M. Farley, J. Hadler, L. H. Harrison, N. M. Bennett, R. Lynfield, A. Reingold, P. R. Cieslak, T. Pilishvili, D. Jackson, R. R. Facklam, J. H. Jorgensen, and A. Schuchat. 2003. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N. Engl. J. Med. 348:1737-1746. [DOI] [PubMed] [Google Scholar]