Abstract
The global eradication of poliomyelitis caused by wild-type virus is likely to be completed within the next few years, despite immense logistic and political difficulties, and may ultimately be followed by the cessation of vaccination. However, the existing live-attenuated vaccines have the potential to revert to virulence, causing occasional disease, and viruses can be shed by immunocompromised individuals for prolonged periods of time. Moreover, several outbreaks of poliomyelitis have been shown to be caused by viruses derived from the Sabin vaccine strains. The appearance of such strains depends on the prevailing circumstances but poses a severe obstacle to strategies for stopping vaccination. Vaccine strains that are incapable of reversion at a measurable rate would provide a possible solution. Here, we describe the constructions of strains of type 3 poliovirus that are stabilized by the introduction of four mutations in the 5′ noncoding region compared to the present vaccine. The strains are genetically and phenotypically stable under conditions where the present vaccine loses the attenuating mutation in the 5′ noncoding region completely. Type 1 and type 2 strains in which the entire 5′ noncoding regions of Sabin 1 and Sabin 2 were replaced exactly with that of one of the type 3 strains were also constructed. The genetic stability of 5′ noncoding regions of these viruses matched that of the type 3 strains, but significant phenotypic reversion occurred, illustrating the potential limitations of a rational approach to the genetic stabilization of live RNA virus vaccines.
Poliomyelitis is caused by poliovirus, a member of the picornavirus family that occurs in three serotypes such that immunity to one serotype does not protect against the other two. The existence of safe and effective vaccines and the absence of an animal reservoir prompted the World Health Assembly to adopt a resolution in 1988 committing the WHO to the eradication of poliomyelitis by the year 2000. Although this deadline has passed, there has been major progress towards the goal. The Americas, Europe, and the Western Pacific region, including China, have been certified free of poliomyelitis caused by wild-type polio. Endemic transmission is now restricted to Nigeria, India, Pakistan, and Afghanistan, although in the last few years, several countries that were previously certified as free of wild-type polio have suffered significant importations from the remaining reservoirs (http://www.polioeradication.org/). Eradication has depended on the use of the live oral polio vaccines (OPVs) originally developed by Sabin (35, 36), and progress has been such that it is necessary to consider the strategies for stopping vaccination altogether.
The situation is complicated by a number of factors. First, the live oral polio vaccine is known to be able to cause poliomyelitis in rare cases in both vaccinees and their contacts (40). Second, some hypogammaglobulinemic patients are known to excrete virus for long periods of time, giving opportunities for the virus to evolve to transmissible and virulent forms (1, 6, 11, 14, 25, 26). Finally, several outbreaks of poliomyelitis caused by vaccine-derived strains have occurred. The first outbreak to be reported happened during 2000 and 2001 in Hispaniola, which had been certified free of polio in 1994 along with the rest of the countries in the Americas and which had a vaccination program of declining coverage, leading to the appearance of a vaccine-derived strain which could both cause disease and transmit readily from person to person (13). Similar outbreaks in China, Egypt, Madagascar, and the Philippines have also been reported (15). The ability of the vaccine to evolve to cause epidemic poliomyelitis given the right selective pressures is therefore a major threat to the completion of the eradication program. Furthermore, after cessation of vaccination, there would be a need to stockpile OPVs for use in outbreaks or cases of reemergence, and it would be preferable to use a ring-fencing strategy that would maintain a polio-free world. This would be difficult to do using strains that can themselves seed new epidemics. One option would be to develop a novel, genetically stable vaccine.
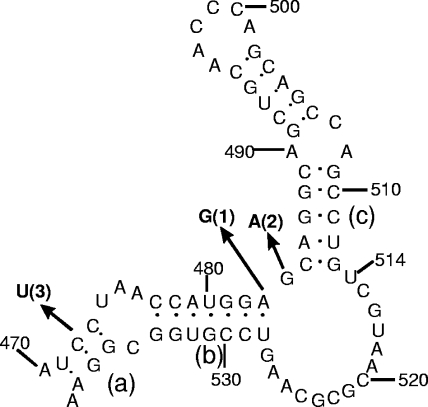
Over a period of 20 years, the molecular basis of the attenuation of the Sabin strains of poliomyelitis has been studied in detail (33). For all three serotypes, while mutations in other regions also have an effect, attenuating mutations have been identified in the 5′ noncoding region (NCR) of the genome, a highly structured sequence involved in both replication and the initiation of protein synthesis (38). The attenuating mutations act to reduce the thermodynamic stability of a particular portion of the structure, designated domain V (Fig. 1), and are genetically unstable as the virus replicates in recipients (5, 7, 8). For the type 3 strain, reversion to the wild-type domain V structure is complete in 2 to 5 days and involves the mutation of a U at base 472 to a C, changing a weak U-G base pair to a C-G base pair (Fig. 1). For the type 1 strain, the G-U base pair involving bases 480 and 525 can mutate to the wild-type A-U base pair by a mutation of base 480 or to a G-C pair by a mutation at base 525. In about 10% of isolates, a U-U mismatch in the type 1 stem changes to a U-A base pair without other changes but with the same effect on thermodynamic stability (5, 30).
FIG. 1.
Predicted RNA secondary structure of domain V (nucleotides 471 to 538) of the type 3 vaccine parent, P3/Leon. Arrows show attenuating nucleotide changes found in the three Sabin vaccine strains (attenuating bases are in boldface type, followed by the relevant serotype in parentheses). Due to slight differences in lengths of the 5′ noncoding regions, nucleotide 480 in Sabin 1 is at position 483 in this figure, and nucleotide 481 in Sabin 2 is at position 484. The base-paired stem regions are designated a, b, and c.
All three serotypes possess a single mutation in domain V so that the wild-type structure is easily regenerated by a single base change. It should be possible to reproduce the differences in thermodynamic stability of domain V of the vaccine and wild-type strains by the manipulation of base pairs, replacing C-G pairs by weaker A-U pairs and eliminating G-U pairs, which can revert to stronger G-C or A-U pairs by single base changes. In the resulting structure, simultaneous multiple mutations would be required to restore the wild-type structure. For instance, an A-U base pair could strengthen to a G-C base pair only via the weaker and thus less favored G-U pair or via two simultaneous mutations.
This paper describes the construction of versions of the Sabin type 3 strain of poliovirus by this strategy. Two strains are of particular interest, as they have in vitro and in vivo properties that are very similar to those of the parental vaccine, differ from it by only four mutations, and are extremely stable under culture conditions that cause the rapid reversion of the Sabin strain itself. It is predicted that the strains would be stable in vaccinees, at least in the absence of potential recombination partners such as the type 1 and type 2 vaccine strains, which are coadministered in trivalent oral polio vaccines.
Recombination between polioviruses is common. Type 1 and type 2 strains in which the entire 5′ NCRs of Sabin 1 and Sabin 2 were replaced exactly with that of one of the stabilized type 3 strains were also constructed so that the three serotypic strains would not be able to revert to virulence by intertypic recombination in the 5′ NCR.
MATERIALS AND METHODS
Cells.
HEp2C, BGM, and Vero cells were grown in monolayers as described previously (22). L20B cells (mouse L cells expressing the human poliovirus receptor) were grown as previously described (31). MRC-5 cells were grown in monolayers in the same growth medium as BGM cells.
Virus passage.
MRC-5, Vero, or L20B cell monolayers in 25-cm2 flasks were inoculated with viruses at a multiplicity of infection of 10. Infected cell sheets were incubated in minimal essential medium containing antibiotics but no serum at 33°C or 37°C until the complete cytopathic effect (CPE) was apparent. Flasks were frozen at −70°C and thawed, three times, and cell debris was removed by centrifugation. Supernatants were used for further passage, as described above, or for biological and molecular analysis.
Construction and recovery of site-directed mutants.
Derivation of the hybrid type 3/type 2 virus Leon/Lansing (L3L2) and construction of L3L2 472/537 UG and L3L2 472/537 UA have been described previously (20, 38). All mutants listed in Table 2 were constructed in a similar way. Briefly, subclones of the Leon 5′ NCR in M13 were substrates for mutagenesis using the Mutagene kit (Bio-Rad). Correct sequences were reintegrated into full-length clones on MluI-SstI (positions 279 to 751) fragments.
TABLE 2.
Sequence and temperature sensitivity of domain V mutants
| Virus | Sequence of domain V | Ta (°C) | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stem a
|
Stem b
|
||||||||||||||||||||
| 471 | 473 | 477 | 483 | ||||||||||||||||||
| Leon/Lansing | U | C | C | .... | C | C | A | U | G | G | A | 39.4 | |||||||||
| A | G | G | .... | G | G | U | G | C | C | U | |||||||||||
| 538 | 536 | 534 | 528 | ||||||||||||||||||
| L3L2 472/537 UA | |||||||||||||||||||||
| (mutant L1) | U | 39.1 | |||||||||||||||||||
| A | |||||||||||||||||||||
| L3L2 472/537 UG | |||||||||||||||||||||
| (mutant L2) | U | 38.7 | |||||||||||||||||||
| G | |||||||||||||||||||||
| Mutant L5 | U | U | 38.0 | ||||||||||||||||||
| A | A | ||||||||||||||||||||
| Mutant L8 | U | U | 38.0 | ||||||||||||||||||
| A | A | ||||||||||||||||||||
| Mutant L10 | U | A | 38.0 | ||||||||||||||||||
| A | U | ||||||||||||||||||||
| Mutant L14 | U | U | U | 38.7 | |||||||||||||||||
| A | A | A | |||||||||||||||||||
| Mutant L15 | U | U | U | 38.7 | |||||||||||||||||
| A | A | A | |||||||||||||||||||
| Mutant L16 | U | U | A | 38.7 | |||||||||||||||||
| A | A | U | |||||||||||||||||||
Temperature at which the number of PFU was reduced by 1.0 log10 relative to the number of PFU at 35°C in BGM cells.
Derivation of Leon and Sabin 3 cDNA clones and construction of S3/472C (previously 119:786/SGDW), S3/2034C (previously LV3/S), and S3/472C/2034C (previously L472V3/S) have been described previously (43). S3/472C is identical to Sabin 3 except for a U-C substitution at nucleotide 472, S3/2034C is identical to Sabin 3 except for a U-C substitution at nucleotide 2034, and S3/472C/2034C is identical to Sabin 3 except for U-C substitutions at nucleotides 472 and 2034. Mutants Leon-UA and Leon-UG are identical to T7/Leon except for a U-C substitution at positions 472 and (for Leon-UA) a G-A substitution at position 537. They were constructed by partial SstI-SalI fragment exchanges between the relevant Leon/Lansing mutant and T7/Leon full-length clones. Mutants shown in Table 3 were constructed in two steps. M1uI-SstI fragments of relevant Leon/Lansing mutants were ligated into Sabin 3 clones lacking the SstI-SstI (positions 751 to 1900) fragment. Full-length infectious clones were generated by the addition of a partial SstI-SmaI (position 2768) fragment.
TABLE 3.
Temperature sensitivities of Sabin 3 and mutants
| Virus | Domain V sequence | Ta (°C) |
|---|---|---|
| Sabin 3 | Vaccine-like (as mutant L2b) | 37.2 |
| Strain S14 | As mutant L14b | 37.0 |
| Strain S15 | As mutant L15b | 37.3 |
| Strain S16 | As mutant L16b | 37.1 |
Temperature at which the number of PFU were reduced by 1.0 log10 relative to the number PFU at 35°C in L20B cells.
See Table 2.
To make S15/1, the 5′ noncoding region of S15 was spliced precisely onto the coding region of Sabin 1 by PCR mutagenesis. The start of the coding region of the Sabin 1 clone pT7/S1F (27) was amplified using primers SAC1 (5′-ATCATAATGGGAGCTCAGGTTTCA-3′) and AM13 (5′-GAGGTAATCAACTGGGCAGAA-3′), digested with SacI and AatII, and gel purified. Plasmid pT7/S15 was digested with EcoRI and SacI, and the 0.78-kb fragment containing the T7 promoter and the first 751 nucleotides of the genome was gel purified. These fragments were ligated together into EcoRI-AatII-digested pT7/S1F to produce the full-length plasmid clone pT7/S15/1, which contained the entire 5′ NCR of S15 and the coding region and 3′ NCR of Sabin 1, as verified by sequencing of the first 1,200 nucleotides of the genome. As a consequence of the mutagenesis strategy, a silent T→A change was introduced into the second codon of the coding region of pT7/S15/1 compared to Sabin 1.
To make S15/2, the 5′ noncoding region of T7/S15 was spliced precisely onto the coding region of Sabin 2 by overlapping PCR. The 5′ NCR of pT7/S15 was amplified with primers NP7 (5′-ACGGGCCCGCGGCCGCTAATACGACTCACTATAGGGTTAAAACAG-3′) and NCR2 (5′-GATGAAACTTGAGCGCCCATT-3′), and the start of the coding region of the Sabin 2 clone pS2 (32) was amplified with primers SAC2a (5′-ACAATGGGCGCTCAAG-3′) and AM13 (5′-GAGGTAATCAACTGGGCAGAA-3′); the overlapping fragments were gel purified, mixed, and reamplified with outer primers NP7 and AM13; the resulting fragment was digested with NotI and SacI, gel purified, and ligated into NotI-SacI-digested pS2 to produce the full-length plasmid clone pT7/S15/2, which contained the entire 5′ NCR of S15 and the coding region and 3′ NCR of Sabin 2, as verified by sequencing of the first 1,500 nucleotides of the genome. Other than the exchanged 5′ noncoding region, no mutations were introduced into the Sabin 2 sequence.
Viruses were recovered by transfection of HEp2C monolayers with ≥2 μg T7 transcripts (41), followed by incubation at 34°C for 24 to 48 h, by which time the complete CPE was apparent. Sequences of nucleotides 450 to 550 of all mutants were confirmed following RNA extraction and reverse transcription-PCR (RT-PCR).
Mutant analysis by PCR and restriction enzyme cleavage.
Mutant analysis by PCR and restriction enzyme cleavage (MAPREC) is a quantitative assay of the proportion of sequences among a population with a defined nucleotide at a particular position (4) and is based on restriction endonuclease digestion after PCR amplification. The method has been applied to the quantitation of the proportion of type 3 polioviruses with a C at position 472 by PCR amplification of cDNA with primers that create an MboI restriction site only in PCR fragments that have a C at position 472. Following radiolabeling, restriction digestion, and polyacrylamide gel electrophoresis, the ratio of cut PCR product to uncut PCR product was determined using a two-dimensional beta imager, and the ratio, along with data for control preparations, was used to calculate the proportion of the viral population that has a C at position 472.
Assays of passaged Sabin 3 virus stocks described here were performed according to the standard operating procedure prepared for the WHO Collaborative Study on MAPREC by K. Chumakov (obtainable from Chief, Biologicals, WHO Geneva). Briefly, RNA was phenol extracted from virus samples and used to make cDNA with random hexamers and Moloney murine leukemia virus reverse transcriptase. cDNAs were denatured at 95°C for 10 s and then amplified for 40 cycles of 15 s at 95°C, 15 s at 60°C, and 15 s at 72°C using AmpliTaq Gold, primer pA3 (5′-CAGGCTGGCTGCTGGGTTGCAGCTGCCTGC-3′) (positions 523 to 484), and primer pS3 (5′-TGAGCTACATGAGAGTGCTCCGGCCCCTGAATGCGGCTGA-3′) (positions 431 to 470). Aliquots of PCR products were used as templates for primer extension using γ-32P-labeled pA3 and fresh AmpliTaq Gold at 72°C for 10 min. Aliquots of primer extension reaction mixtures were digested with MboI and analyzed on 10% polyacrylamide gels.
MAPREC assays of passaged Sabin 1 and Sabin 2 virus stocks were performed using a modified protocol that avoided radiochemicals and employed agarose gel electrophoresis for high throughput. Viral RNA was extracted using High Pure Viral Nucleic acid kits (Roche), and RT-PCRs were then carried out using the One-Step RT-PCR kit (QIAGEN), according to the manufacturers' protocols in both cases. Amplification was achieved with 40 cycles of 15 s at 95°C, 15 s at 60°C, and 15 s at 72°C using appropriate primers (see below). After restriction enzyme digestion, PCR fragments and products were separated on 3% NuSieve 3:1 agarose (FMC BioProducts) gels. Gels were scanned using an AutoChemi System imager (UVP BioImaging Systems) and analyzed using LabWorks software to calculate proportions of digested and undigested fragments.
Passaged Sabin 1 viruses were amplified with pA1 (5′-ACAGGCCAATCACTGGTTTGTGACCACGTG-3′) (positions 511 to 482) and pS1 (5′-CTGCGTTGGCGGCCTACCTATGGCTAACG-3′) (positions 359 to 387), and fragments were digested with BsiHKAI, which cuts if there is an A at nucleotide 480, and (separately) with AvaI, which cuts if there is a G at nucleotide 480 and a U at nucleotide 476, as found in Sabin viruses. Proportions of viruses with a U-A mutation at nucleotide 476 (identified by sequence analysis) were calculated by the subtraction of BsiHKAI from AvaI data. Passaged Sabin 1 viruses were also amplified with S1M525A (5′-CCCAAAGTAGTCGGTTCCGCCACGT-3′) (positions 550 to 526) and S1M525S (5′-GAGCCTATTGAGCTACATAAGAATC-3′) (positions 420 to 444), and fragments were digested with RsaI, which cuts if there is an A at nucleotide 525, as found in Sabin 1 viruses. Passaged Sabin 2 viruses were amplified with pA2M2 (5′-GACTTGCGCGTTACGACAAGACAGTCACTGATTCGCGACCGCCAG-3′) (positions 526 to 482) and pS2M2 (5′-TAGGACGTTAGATGTGAACAAGGTGTGAAGAGCCTATTGATGTACAT-3′) (positions 391 to 437), and fragments were digested with AluI, which cuts if there is a G at nucleotide 481.
Results obtained using the simplified MAPREC protocol were not as accurate as those obtained from standard MAPREC assays for two reasons: the lower sensitivity of the imaging system resulted in variation in replica assays of up to 5% for mean values of >50% reversion (data not shown), and the amplification protocol did not have a step to prevent the formation of heteroduplex fragments resulting from annealing during the last amplification cycle, so sequences containing the intact restriction enzyme site would tend to be underestimated after digestion, with the problem being worse with 50:50 mixtures where the maximum error was estimated at 5%. Neither of these errors was significant for nearly homogeneous populations, so trends in mutation selection were easily observable and credible.
Temperature sensitivity.
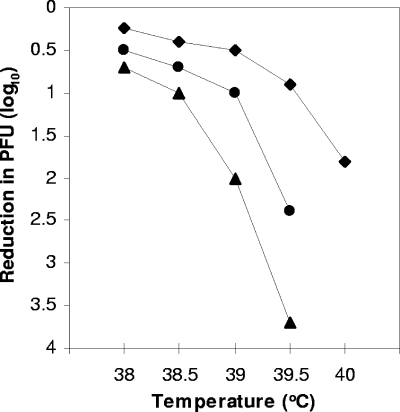
BGM cells were used for temperature sensitivity assays as previously described (22). L20B cells were used for temperature sensitivity assays as described previously for CM-1 cells (20). Briefly, viruses were assayed by plaque formation at different temperatures. These assays were controlled by the incubation of inoculated plates in sealed plastic boxes submerged in water baths whose temperatures fluctuated by <0.01°C. All viruses were assayed at least twice, and control viruses with known phenotypes were always included for validation. Results were plotted onto graphs such as that shown in Fig. 2, and these graphs were used to estimate the temperature (T) at which the number of PFU were reduced by 1.0 log10 compared to the number of PFU at 35°C.
FIG. 2.
Correlation of base pair strength of nucleotides 472/537 with temperature sensitivity. Leon and site-directed mutants, which differed from Leon only at nucleotides 472 and 537, were assayed by plaque formation at different temperatures in L20B cells. Curves represent the reductions in numbers of plaques compared to the numbers of plaques formed at 35°C as a function of temperature. Symbols: ⧫, Leon; •, Leon/UA; ▴, Leon/UG.
Viruses with a Leon/Lansing genomic background were assayed in BGM cells; Sabin 3, Leon, and mutants of these viruses were assayed in L20B cells and HEp2C cells. The range of temperatures over which variation in domain V stability influences viral growth depends on the cell substrate used (20, 22), being the lowest in L20B cells and the highest in HEp2c cells. For Sabin 3, the major temperature-sensitive (ts) determinant is found at VP3-91 (29), and this influences temperature sensitivity at temperatures higher than that of domain V in L20B cells but approximately the same as that of domain V in BGM cells and Hep2c cells (A. J. Macadam, unpublished data). Consequently, temperature sensitivity assays of L20B cells can be used to distinguish viruses with different mutations in domain V irrespective of the residue at VP3-91.
Neurovirulence.
Viruses were assayed using monkeys by the standard WHO-approved test for vaccine safety (44), except that fewer animals were used per virus. Historical data on reference viruses have demonstrated the comparability between results of tests carried out on different occasions. Neurovirulence in TgPVR mice was tested by intramuscular injection of Tg66-C57 mice, which are transgenic for the human poliovirus receptor gene (Macadam, unpublished). Mice were inoculated in the left hind limb with 50 μl of 10-fold virus dilutions (eight mice per dose [four males and four females]), monitored twice daily for 14 days, and scored for paralysis. The 50% paralytic dose (PD50) was calculated using the probit method.
RESULTS
Selection of candidate domain V sequences. (i) Correlates of attenuation.
Previously, we have shown that for genetically defined strains that differ only in RNA domain V of the 5′ NCR, temperature sensitivity of growth is quantitatively related to the predicted stability of the folded RNA (20). Temperature sensitivity of growth is measured by the temperature at which the titer of virus is reduced by 1.0 log10 compared to that at 35°C. The relationship between temperature sensitivity, using L20B cells as the substrate, and neurovirulence for the type 3 strain P3/Leon/37 (the virulent parent of Sabin 3) is shown in Table 1 and Fig. 2, where the effect of the progressive weakening of the base pair at positions 472/537 was examined. Replacement of the wild-type C-G base pair by a weaker U-A base pair rendered virus growth in L20B cells more sensitive to high temperatures (T = 39.6°C to 39.0°C) and decreased neurovirulence, as shown by a reduction in the proportion of clinically affected animals from 4/4 to 6/8 and a decrease in histological damage from a score of 2.71 to 2.0. Replacement of positions 472/537 by a U-G base pair, as found in the Sabin type 3 strain, resulted in a higher level of attenuation, with 4/8 animals affected, a lesion score of 1.78, and a greater temperature sensitivity (T = 38.4°C). Thus, the level of attenuation conferred by these mutations was directly related to the extent of secondary structure destabilization. This result confirms that the attenuation phenotype conferred by the C-to-U substitution at nucleotide 472 in the type 3 vaccine (44) is due to the weakness of the resulting U-G base pair at positions 472/537 (compared to the wild-type C-G base pair) rather than the U substitution per se. It also supports the conclusion that temperature sensitivity as defined here is a correlate of attenuation (20). Based on these studies, we have used temperature sensitivity in appropriate tissue culture assays as a guide to the level of attenuation of mutant strains.
TABLE 1.
Correlation of base pair 472/537 with neurovirulence and temperature sensitivity
| Virus | Base pair at nucleotides 472/537 | Ta (°C) | Clinical score (no. of paralyzed animals/total no. of animals) | Mean lesion score (SD) |
|---|---|---|---|---|
| Leon | C/G | 39.6 | 4/4b | 2.71 (0.23)b |
| Leon-UA | U/A | 39.0 | 6/8 | 2.0 (0.51) |
| Leon-UG | U/G | 38.4 | 4/8 | 1.78 (0.27) |
Temperature at which numbers of PFU were reduced by 1.0 log10 relative to the number of PFU at 35°C in L20B cells.
Results were from obtained from the work of Westrop et al. (43).
(ii) Adjustment of domain V stability.
Viruses were constructed with mutations designed to alter the thermodynamic stability of domain V. This was achieved by a combination of replacing C-G base pairs with U-A or A-U base pairs to lower thermodynamic stability and replacing U-G base pairs with U-A base pairs to raise it. To allow a comparison with previous studies (20), mutations were first introduced into the genome of the hybrid virus Leon/Lansing (L3L2), in which the 5′ noncoding region of the mouse-adapted type 2 poliovirus Lansing was replaced by modified versions of the 5′ noncoding region of P3/Leon. The mutants constructed and their ts phenotypes are shown in Table 2.
As previously reported (20) and consistent with the data shown in Table 1, mutant L1, possessing a U-A base pair at positions 472/537, had a ts phenotype (T = 39.1°C) that was intermediate between viruses with base pairs corresponding to those of the wild type (C-G) (T = 39.4°C) and Sabin 3, mutant L2 (U-G) (T = 38.7°C). Further weakening of the domain V structure of mutant L1 by mutation of other C-G base pairs to U-A or A-U base pairs in addition to the substitution of U-A for C-G at bases 472/537 resulted in increased temperature sensitivity of growth. Mutant L5 possessed a U-A base pair at positions 478/533, mutant L8 possessed a U-A base pair at positions 481/530, and mutant L10 possessed an A-U base pair at positions 482/529 in place of the wild-type C-G or G-C base pair. All showed a 1-log drop in titer at 38°C, whereas mutant L2, the strain with the same domain V structure as the Sabin type 3 vaccine strain, showed a 1-log drop in titer at 38.7°C for mutant L2, the strain with the same domain V structure as the Sabin type 3 vaccine strain. It was therefore considered likely that they would be more attenuated in vivo and potentially less immunogenic than Sabin 3, so that it was necessary to modify the structure further to strengthen it to a small degree. The U-G base pair at positions 480/531 was therefore converted to a stronger U-A base pair. This base pair was chosen for modification, as any U-G base pair could, in principle, mutate to a C-G base pair upon replication, thus significantly increasing the stability of the structure with a concomitant increase in virulence. The U-A base pair that was introduced could mutate to a C-G base pair only via the weaker and therefore more attenuating U-G base pair or by two simultaneous mutations. The viruses derived from L5, L8, and L10 by modifying base 531 were L14, L15, and L16, respectively, and all were of the same ts phenotype as L2, with the strain having the Sabin type 3 vaccine strain 5′ noncoding region (T = 38.7°C). It was therefore predicted that the introduction of four base changes in the Sabin type 3 sequence, namely, G to A at positions 537 and 531 with a G-C or C-G to U-A or A-U change at positions 478 to 533, 481 to 530, or 482 to 529, would give a virus with the same degree of attenuation as the Sabin type 3 vaccine strain itself.
(iii) Attenuation phenotypes.
The mutations in domain V of mutants L14, L15, and L16 were introduced into a Sabin 3 genomic background, and viruses were assayed for temperature sensitivity in L20B cells. ts phenotypes of strains S14, S15, and S16 were all similar to that of Sabin 3 (Table 3). Mutants S15 and S16 were tested for neurovirulence in monkeys, and results are shown in Table 4, along with results for the cloned Sabin 3 strain. As predicted, the attenuation phenotypes of strains S15 and S16 were not statistically different from that of Sabin 3. No animals were paralyzed by any of the viruses. The mean lesion score of strain S15 (0.61) was almost identical to the score for Sabin 3 (0.63). Strain S16 had a lower mean lesion score of 0.42, but the difference was not significant. These results must be viewed in light of the limited number of animals used; small differences between attenuated viruses cannot be detected reliably without larger-scale tests. While there is variation between vaccine strains and vaccine lots, polio vaccines typically produce lesion scores of less than 1.0, so on the basis of these results, both strains S15 and S16 would be expected to pass the WHO monkey neurovirulence test for vaccine safety (44).
TABLE 4.
Neurovirulence of vaccines and new strains
| Virus | TgPVR micea PD50 (log10)b | Cynomolgous macaques
|
||
|---|---|---|---|---|
| Clinical score (no. of paralyzed animals/ total no.) | Mean lesion score (SD) | P valuec | ||
| Sabin 3 | >8.9 | 0/10 | 0.62 (0.66) | |
| S15 | >9.1 | 0/4 | 0.61 (0.63) | 0.96 |
| S16 | NDd | 0/4 | 0.42 (0.25) | 0.41 |
| Sabin 2 | >8.9 | 0/4 | 0.27 (0.12) | |
| S15/2 | 7.5 | 0/4 | 0.80 (0.26) | 0.02 |
| Sabin 1 | 7.6 | 0/6 | 0.63 (0.28) | |
| S15/1 | 7.8 | 0/4 | 0.71 (0.29) | 0.68 |
Tg66-C57.
Intramuscular route.
Student's t test.
ND, not determined.
Candidate strains of all three serotypes.
The entire 5′ noncoding region of Sabin 1 was replaced exactly with that of strain S15 to create S15/1, and the entire 5′ noncoding region of Sabin 2 was replaced exactly with that of strain S15 to create S15/2. This approach was predicted to generate genetically stable strains of all three serotypes that, if administered together, would not be able to revert to virulence by recombination in the 5′ NCR. The choice of the S15 sequence over that of S16 was arbitrary. RNA transcripts from resultant cDNA clones were highly infectious, causing a complete CPE in Hep2C monolayers after 24 to 48 h. Viruses were sequenced through the 5′ NCR and part of VP4 to verify their identity before biological characterization was carried out.
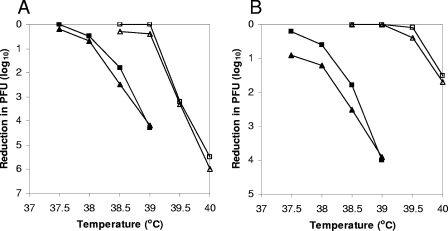
(i) Temperature sensitivity phenotypes.
In L20B cells, the ts phenotypes of Sabin 1 and Sabin 2 are due mainly to attenuating determinants in the 5′ noncoding region (Macadam, unpublished). In these cells, the ts phenotypes of strain S15/1 (T = 38.2°C) and Sabin 1 (T = 38.1°C) were similar (Fig. 3A), suggesting that the 5′ noncoding regions of Sabin 1 and Sabin 3 are equivalent at least with respect to this property. In L20B cells, the ts phenotype of S15/2 (T = 38.2°C) was expressed at a higher temperature than that of Sabin 2 (T = 37.7°C) (Fig. 3B), suggesting that the 5′ noncoding region of Sabin 2 has a stronger influence on this property than that of Sabin 3, consistent with the finding that this region contains the major determinant(s) of temperature sensitivity of Sabin 2 in other cell lines as well (22). In HEp2C cells, the phenotypes of Sabin 1 and S15/1 were similar (T = 39.1°C), as were those of Sabin 2 and S15/2 (T = 39.8°C and 39.7°C, respectively) (Fig. 3). In these cells, determinants in the coding regions (which are the same for each pair of viruses) control ts phenotypes (22; Macadam, unpublished).
FIG. 3.
Temperature sensitivities of type 1 and type 2 strains in different cells. Viruses were assayed by plaque formation at different temperatures in L20B cells (filled symbols) and Hep2C cells (open symbols), and results were plotted on graphs showing the reduction in the numbers of PFU at each temperature compared to the numbers of PFU at 35°C. (A) Triangles, Sabin 1; squares, S15/1. (B) Triangles, Sabin 2; squares, S15/2.
(ii) Attenuation phenotypes.
Strains S15/1 and S15/2 were tested for neurovirulence in monkeys and TgPVR mice, and results are shown in Table 4. Strain S15/1 was equivalent to Sabin 1 in both animal models: no monkeys were paralyzed by either virus, and histological lesion scores were not statistically different (0.71 for S15/1 and 0.63 for Sabin 1; P = 0.68); PD50 values were also similar (7.8 log10 for S15/1 and 7.6 log10 for Sabin 1). These results are consistent with the similar ts phenotypes of the two viruses in L20B cells described above, again suggesting the equivalence of the 5′ noncoding regions of Sabin 1 and Sabin 3.
The type 2 strain S15/2, however, was appreciably less attenuated than Sabin 2 in both models. While no monkeys were paralyzed by either virus, the histological lesion score for S15/2 (0.8) was significantly higher than that of Sabin 2 (0.27) (P = 0.02). The PD50 value for S15/2 (7.5 log10) was substantially lower than that of Sabin 2 (>8.9 log10). This suggests that the 5′ NCR of Sabin 2 is more strongly attenuating than the 5′ NCR of S15 and, hence, that of Sabin 3. This result is consistent with the results of temperature sensitivity assays of L20B cells described above, which showed that the 5′ NCR of Sabin 2 had a stronger effect than that of Sabin 3 on this phenotype as well. Sabin 2 is more attenuated than Sabin 3 (Table 4), and while the two attenuating determinants of Sabin 3 are of comparable strengths (Table 5), the 5′ NCR of Sabin 2 contains stronger determinants of attenuation than the rest of the genome (23). The attenuation phenotype of S15/2 in TgPVR mice is similar to that of Sabin 1, suggesting that this virus may be sufficiently attenuated to be considered for use as a vaccine. The mean histological lesion score of S15/2 in the monkey neurovirulence test is at the upper end of the range of scores usually observed for any vaccine but is not statistically different from that of Sabin 1 (P = 0.37). Indeed, none of the strains S15, S15/1, and S15/2 gave statistically different lesion scores from each other (P = 0.61 to 0.78).
TABLE 5.
Neurovirulence before and after passage in L20B and Vero cells
| Virus | Unpassaged
|
L20B passage 5
|
Vero passage 10
|
|||
|---|---|---|---|---|---|---|
| Clinical score (no. of animals paralyzed/total no. of animals) | Mean lesion score (SD) | Clinical score (no. of animals paralyzed/total no. of animals) | Mean lesion score (SD) | Clinical score (no. of animals paralyzed/total no. of animals) | Mean lesion score (SD) | |
| Sabin3 (S3) | 0/10 | 0.62 (0.66) | 1/4 | 1.92 (0.26) | 4/5 | 1.95 (0.13) |
| Strain S15 | 0/4 | 0.61 (0.63) | 0/4 | 0.53 (0.37) | 0/5 | 1.41 (0.42) |
| Strain S16 | 0/4 | 0.42 (0.25) | 0/4 | 0.68 (0.34) | 0/5 | 0.88 (0.27) |
| S3/472Ca | 0/4 | 1.58 (0.49) | ||||
| S3/2034Ca | 1/8 | 1.45 (0.60) | ||||
| S3/472C/2034Ca | 3/4 | 2.07 (0.42) | ||||
Results were obtained from data reported previously by Westrop et al. (44).
Genetic stability. (i) Type 3 viruses.
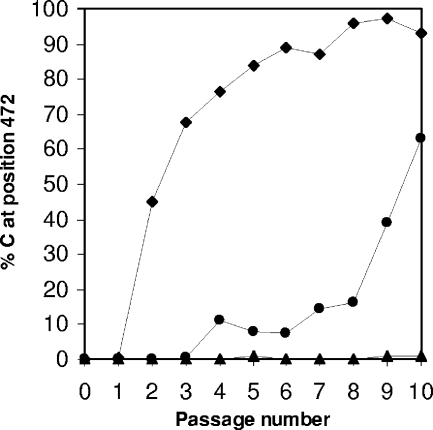
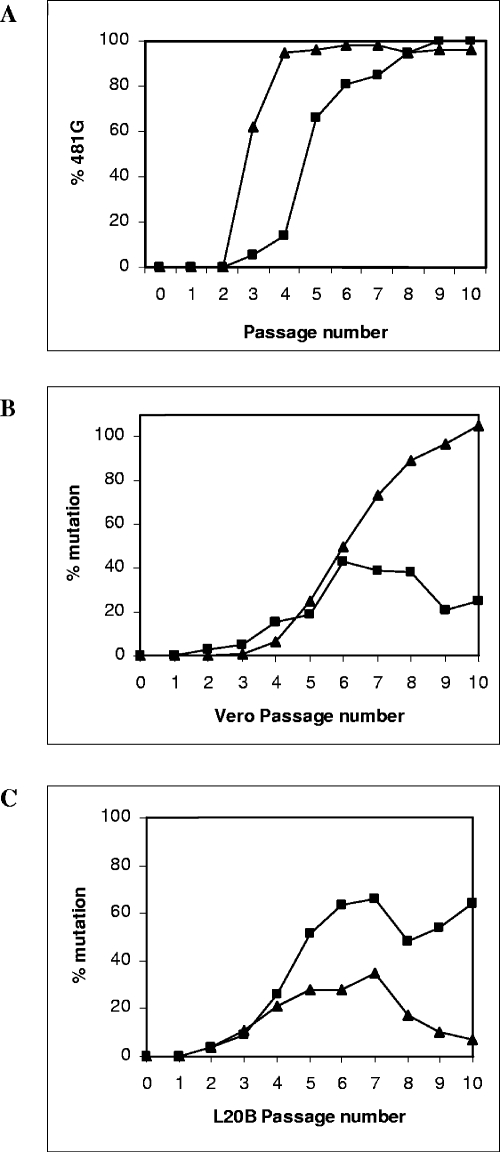
In order to compare the stabilities of strains S15 and S16 with that of Sabin 3, cell culture models that favored rapid reversion at nucleotide 472 were used. The temperature-sensitive phenotype resulting from mutations in domain V is most strongly expressed in L20B cells (20). Therefore, Sabin 3 and strains S15 and S16 were passaged in L20B cells at 37°C using a multiplicity of infection of 10. Viral RNA was extracted from fifth-passage stocks and sequenced through the 5′ NCR after RT-PCR. The degree of reversion from a U to a C at position 472 in Sabin 3 was determined by MAPREC assay (4). Over 50% of the Sabin 3 virus population had a C at nucleotide 472 by passage 3, and by the fifth passage, almost 85% had a C at nucleotide 472, as shown in Fig. 4. No other nucleotide changes were observed in the 5′ NCRs of passaged Sabin type 3 viruses. As expected, no nucleotide changes were observed in 5′ NCRs of the fifth-passage stocks of strain S15 or S16.
FIG. 4.
Stability of 472U in Sabin 3 upon passage in different cell lines. Sabin 3 was passaged 10 times in different cells at 37°C, and the 472C content was then measured by PCR and restriction endonuclease digestion (MAPREC). Symbols: ⧫, L20B cells; •, Vero cells; ▴ MRC-5 cells. L20B cells are mouse L cells expressing the human poliovirus receptor. Vero cells and MRC-5 cells are used for vaccine production.
In a neurovirulence test, the fifth L20B-passaged stock of Sabin 3 was significantly more virulent than the vaccine strain, as shown by both numbers of clinically affected animals and histological lesion scores (Table 5). The results for S3/472C, which differs from the Sabin type 3 strain only by possessing a C in place of a U at base 472, were consistent with the view that the virulence of the passage 5 stock was due largely to reversion at nucleotide 472 (U→C). The results for the fifth-passage stocks of strains S15 and S16, however, were very similar to those for original stocks and the unpassaged vaccine strain (Table 5). Thus, under conditions that rapidly selected neurovirulent variants of Sabin 3, the attenuation phenotypes of strains S15 and S16 were stable.
The African green monkey kidney cell line Vero has been used in the production of oral polio vaccine and expresses the ts phenotype due to domain V mutations less strongly than the L20B cell line. When Sabin 3 was passaged in Vero cells at 37°C, reversion of Sabin 3 at nucleotide 472 was much slower than in L20B cells (Fig. 4), although by the 10th passage, over 60% of the Sabin 3 virus population had a C at nucleotide 472 (Fig. 4). No other nucleotide changes were observed in the 5′ NCR of this virus. As expected, no nucleotide changes were observed in the 5′ NCR of strains S15 and S16 passaged in the same way.
The second major attenuating mutation in Sabin 3 is in the capsid proteins (nucleotide 2034, C-U; VP3-91, S-F). Sequencing of entire P1 regions of all three strains after 10 passages on Vero cells at 37°C showed that there was no reversion at nucleotide 2034, but each strain had had a single, different, point mutation in the capsid proteins, which resulted in a coding change. These changes were found at VP3-85 (L→F) in Sabin 3, VP1-265 (V→I) in S15, and VP3-19 (H→Y) in S16. MAPREC analyses indicated that these changes were all selected at similar rates during passage in Vero cells (data not shown). At the same time, all three strains lost the ts phenotype in Hep2C cells (data not shown), which is due to VP3-91 F (29). Reversion of this phenotype by second-site mutation in the capsid proteins is common (19, 29), and while the particular mutations found here have not been identified in previous studies, it is likely that they were responsible for the suppression of the VP3-91F phenotype.
After 10 passages in Vero cells at 37°C, the neurovirulence of Sabin 3 had increased dramatically. Four out of five animals were paralyzed, and the mean lesion score had increased to 1.95 (Table 5). The neurovirulence phenotype of this virus stock was similar to that of S3/472C/2034C (Table 5), consistent with sequence and ts data indicating reversion of both attenuating mutations in Sabin 3. In contrast, the neurovirulence phenotypes of strains S15 and S16 had changed much less after 10 passages in Vero cells at 37°C. No animals were paralyzed by either virus stock (Table 5). The 10th Vero cell-passaged stock of strain S15 had a higher mean lesion score than that of the unpassaged parent, and this was consistent with the reversion of the attenuating 2034U mutation suggested by sequence and ts data (the mean lesion score was close to that of S3/2034C). The 10th Vero-passaged stock of strain S16 had a mean lesion score that was slightly higher than that of the unpassaged parent. Again, the increase is consistent with a partial reversion of the attenuating 2034U mutation, as indicated by sequence and ts results. Thus, for both strain S15 and strain S16, the attenuation due to mutations in domain V appeared to be completely stable under conditions that selected for the reversion of 472U→C in the majority of the Sabin 3 virus population.
The human diploid cell line MRC-5 has also been used in the production of oral polio vaccine. Under the conditions of passage used, no reversion of nucleotide 472 was observed in the Sabin type 3 strain over 10 passages (Fig. 4).
(ii) Type 2 viruses.
Results for type 3 strains showed that passage in L20B cells and Vero cells at 37°C resulted in the selection of reversion of attenuating mutations in Sabin 3. Therefore, type 2 strains were passaged under the same conditions. Nucleotide changes in domain V of Sabin 2 were monitored by sequencing and MAPREC, and the stability of domain V of S15/2 was assessed by sequencing.
The major attenuating mutation in the 5′ NCR of Sabin 2 is an A at nucleotide 481 (Fig. 1), and an A→G mutation at this position, which results in a significant loss of attenuation (23, 34), was rapidly selected during passage of Sabin 2 in both L20B cells and Vero cells at 37°C. By the third passage in L20B cells, over 60% of the Sabin 2 population had a G at nucleotide 481, and after four passages, selection was almost complete (Fig. 5A). In Vero cells, over 60% of the Sabin 2 population had a G at nucleotide 481 after five passages, and selection was essentially complete after eight to nine passages. No nucleotide changes were observed in domain V of strain S15/2 after 10 passages in either L20B cells or Vero cells.
FIG. 5.
Stability of attenuating mutations in domain V of Sabin 2 and Sabin 1 upon passage in different cell lines. Viruses were passaged 10 times in different cells at 37°C, and mutant proportions were then measured by PCR and restriction endonuclease digestion (MAPREC). (A) Mutation at nucleotide 481 in Sabin 2 during passage in L20B cells (▴) and Vero cells (▪). (B) Mutation in Sabin 1 during passage in Vero cells at nucleotide 480 or 525 (▴) and at nucleotide 476 (▪). (C) Mutation in Sabin 1 during passage in L20B cells at nucleotide 480 or 525 (▴) and at nucleotide 476 (▪).
In a neurovirulence test, the 10th Vero cell-passaged stock of Sabin 2 was significantly more virulent than the vaccine strain, as shown by both numbers of clinically affected animals and histological lesion scores (Table 6). Scores were similar to those of S2/117 5′, a cDNA-derived virus differing from Sabin 2 only at nucleotide 481 (A→G) and nucleotide 437 (U→C) and therefore consistent with the observed sequence change at nucleotide 481 in S15/2. The results for the 10th Vero cell-passaged stock of strain S15/2, however, were very similar to those for original stocks (Table 6). No animals were paralyzed, and the mean histological lesion score showed only a small increase. Thus, under conditions that rapidly selected neurovirulent variants of Sabin 2, the attenuation phenotype of strain S15/2 was relatively stable.
TABLE 6.
Neurovirulence before and after 6 or 10 passages in Vero and L20B cells
| Passage (cell line) | Sabin 2
|
S15/2
|
S2/117 5′b
|
117b
|
Sabin 1
|
S15/1
|
S1/480Ac
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical score (no. of animals sacrificed/total no. of animalsa) | Mean lesion score (SD) | Clinical score (no. of animals sacrificed/total no. of animalsa) | Mean lesion score (SD) | Clinical score (no. of animals sacrificed/total no. of animalsa) | Mean lesion score (SD) | Clinical score (no. of animals sacrificed/total no. of animalsa) | Mean lesion score (SD) | Clinical score (no. of animals sacrificed/total no. of animalsa) | Mean lesion score (SD) | Clinical score (no. of animals sacrificed/total no. of animalsa) | Mean lesion score (SD) | Clinical score (no. of animals sacrificed/total no. of animalsa) | Mean lesion score (SD) | |
| 0 | 0/4 (0/4) | 0.27 (0.12) | 0/4 (0/4) | 0.80 (.026) | 2/4 (2/4) | 1.39 (0.47) | 4/4 (4/4) | 1.76 (0.32) | 0/6 (0/6) | 0.63 (0.28) | 0/4 (0/4) | 0.71 (0.29) | 1/4 (1/4) | 0.92 (0.18) |
| 6 (Vero) | 1/3 (1/3) | 1.01 (0.77) | 0/3 (0/3) | 0.61 (0.15) | ||||||||||
| 10 (Vero) | 2/4 (2/4) | 1.85 (0.27) | 0/3 (0/3) | 0.92 (0.37) | 1/4 (1/4) | 1.44 (0.39) | 0/4 (0/4) | 1.06 (0.26) | ||||||
| 6 (L20B) | 2/3 (2/3) | 1.04 (0.08) | 1/4 (1/4) | 0.88 (0.53) | ||||||||||
| 10 (L20B) | 3/4 (4/4) | 1.76 (0.38) | 1/4 (3/4) | 1.87 (0.32) | 1/4 (4/4) | 1.41 (0.17) | 0/4 (3/4) | 1.57 (0.02) | ||||||
The 10th L20B cell-passaged stock of Sabin 2 was also significantly more virulent than the vaccine strain, in line with the observed mutation at nucleotide 481. In a neurovirulence test of this virus stock, three out of four animals were sacrificed, and all four animals had complete paralysis in at least one limb (Table 6). The histological lesion score (1.76) was as high as that for strain 117, a neurovirulent virus from a case of vaccine-associated paralysis (32). In contrast to the results using Vero cells, passage of strain S15/2 in L20B cells resulted in significantly increased neurovirulence, as indicated by higher paralysis rates and higher histological lesion scores (Table 6). In light of the sequencing data showing the stability of the domain V sequence of S15/2 throughout this passage, the observed increase in virulence must have been due to mutations outside this region.
The clinical score for strain S15/2 after 10 L20B passages was lower than that of Sabin 2 after similar passage (1/3 sacrificed and 3/4 paralyzed versus 3/4 sacrificed and 4/4 paralyzed) (Table 6), although the histological scores for the two viruses were similar. Along with the results for the Vero cell passage of type 2 strains, this suggests that the genetic stability of domain V of S15/2 resulted in greater stability of the attenuation phenotype compared to Sabin 2, although the effects were not as dramatic as those for the type 3 strains S15 and S16.
(iii) Type 1 viruses.
Type 1 strains Sabin 1 and S15/1 were passaged in L20B cells and Vero cells in the same way as the type 2 and type 3 strains. Nucleotide changes in domain V of Sabin 1 were monitored by sequencing and MAPREC assays, and the stability of domain V of S15/1 was assessed by sequencing.
Three different mutations in domain V of Sabin 1 are selected during replication in the gut (5, 30), all of which strengthen base pairing: G→A at position 480, U→C at position 525, and U→A at position 476. Nucleotides 480 and 525 form a base pair (positions 483/528 in Fig. 1), so mutations occur at one or the other position in a virus but not at both positions. In Vero cells, mutations at all three positions were selected in Sabin 1 at a steady rate (Fig. 5B), so that after six passages, half of the virus population had a mutation at either nucleotide 480 or 525 and more than 40% of the virus population had a mutation at nucleotide 476 (assays did not provide information on the proportions that had zero, one, or two mutations). During the last four passages, the proportion of the virus population that had a mutation at either nucleotide 480 or 525 increased to approximately 100% (mainly due to a mutation at nucleotide 480) (data not shown), while the proportion of viruses with mutations at nucleotide 476 declined slightly. Mutations at all three positions were also selected in Sabin 1 during passage in L20B cells, although, in contrast to results using Vero cells, mutations at nucleotide 476 were selected at a higher rate than those at nucleotides 480 and 525 (Fig. 5C), so that after six passages, approximately 60% of the virus population had a mutation at nucleotide 476 and 30% had a mutation at either nucleotide 480 or 525. During the eighth passage, the proportion of mutations at each position declined, suggesting that strong selection was occurring at another position(s) in the genome. Thereafter, selection of mutations at nucleotide 476, but not at nucleotide 480 or 525, continued. No nucleotide changes were observed in domain V of strain S15/1 after 10 passages in either L20B cells or Vero cells.
In light of the evidence from MAPREC assays showing that several lineages of viruses were evolving during the passages of the type 1 viruses, neurovirulence tests were carried out on virus stocks obtained after 6 as well as after 10 passages. After six passages in Vero cells, the virulence of Sabin 1 had increased, in terms of both numbers of clinically affected animals and histological lesion scores, to a level similar to that of S1/480A, a site-directed mutant of Sabin 1 with a G→A substitution at nucleotide 480 (Table 6), consistent with the MAPREC results showing that at least 50% of the viruses in this virus stock had mutated at nucleotides 480 or 525 and at least 40% had mutated at nucleotide 476 (Fig. 5B). Under these conditions, the virulence of strain S15/1 had not increased: no animals were paralyzed, and the lesion score was slightly lower than that of the original stock (Table 6). After a further four passages, the virulences of both viruses had increased in terms of histological lesion scores, reflecting (for S15/1 at least) the accumulation of mutations at positions outside domain V. The 10th Vero cell-passaged stock of Sabin 1 was, however, more neurovirulent than that of S15/1 by both measures, consistent with the additional mutations in domain V of Sabin 1 (Fig. 5B).
After six passages in L20B cells, both Sabin 1 and S15/1 gave increased clinical and histological lesion scores in neurovirulence tests, although the increases in both scores were greater for Sabin 1 than for S15/1 (Table 6). For S15/1, these increases were the result of mutations in regions outside domain V, suggesting that passage in L20B cells also exerted selection pressures on one or more of the other attenuating mutations in the genome. The differential increase in virulence between the two viruses is consistent with the observed mutations in domain V of Sabin 1 (Fig. 5C) compared to the genetic stability of domain V of strain S15/1. During four additional passages in L20B cells, the neurovirulence of both viruses increased further in terms of paralysis rates and histological lesion scores (Table 6) as a result of the selection of mutations outside domain V: the sequence of domain V of S15/1 was completely stable throughout the passages, the proportion of viruses in the 10th L20B cell-passaged stock of Sabin 1 with mutations at nucleotide 476 was similar to that in the 6th-passage stock, and the proportion of viruses with mutations at nucleotide 480 or 525 had decreased (Fig. 5C). These results showed that the genetic instability of domain V of Sabin 1 was only one of the factors in the observed reversion to virulence during cell culture passage, and consequently, the genetic stability of domain V of S15/1 was only marginally advantageous in this respect.
DISCUSSION
For all three serotypes of Sabin polio vaccine strains, attenuating mutations have been identified in the 5′ noncoding region of the genome, and the direct effect of these mutations is on the RNA secondary structural stability of part of this region known as domain V. The work described here was based on the premise that the overall stability of domain V rather than any particular base or base pair dictates the level of virulence and the observation that during replication, polio vaccines incorporate changes that strengthen base pairing and thereby regain virulence. Results demonstrated that it was possible to manipulate the sequence of domain V to alter viral virulence in a predictable way and at the same time increase genetic stability to the extent that reversion was at undetectable levels.
The ability to control these two key features of a live-virus vaccine is unprecedented and could theoretically lead to the generation of improved polio vaccines. However, at this stage in the eradication of poliomyelitis, what is required in a live vaccine is complete genetic stability rather than improvement, however significant, and complete stability cannot be achieved for two reasons: domain V is not the only region containing determinants of attenuation, so reversion at other positions can in time produce highly virulent viruses (as observed during cell culture passage here), and recombination between members of the group C enteroviruses is now known to be so frequent in humans (3, 9, 18) that the exchange of the stabilized region would be very likely if not inevitable if the viruses circulated to any extent.
A number of strains that potentially have more stable attenuation phenotypes than the Sabin strains have been described previously (10, 12, 16, 39), and all but one were derived by the deletion or substitution of (large) stretches of nucleotides in the 5′ NCR (21). All strains were attenuated when tested in monkeys and/or TgPVR mice, and attenuation phenotypes of some of these strains might be more genetically stable than those of the Sabin strains, but this has not been tested.
The type 3 viruses described in this paper are derived from the existing Sabin type 3 vaccine strain, from which they differ by four mutations at most, and were designed according to our current understanding of the molecular basis of its attenuated phenotype (24, 28). They were constructed to be genetically stable and to display a level of attenuation in the neurovirulence assay comparable to that of the existing Sabin strain. Theoretically, vaccines prepared from such strains would have a greatly reduced potential for reversion to virulence, since reversion would depend on the simultaneous change of several nucleotides in stem-loop V, compared to only a single change in Sabin 3. For the S15 and S16 strains, two base pair reversions and a single point mutation would be required to revert to the wild-type (P3/Leon) sequence. With a mutation frequency of approximately 10−5/nucleotide (17, 37), chances of this combination of mutations occurring in a single genome would be 1020-fold less than the chance of a reversion of U to C at nucleotide 472 in Sabin 3. Moreover, a reversion to the wild-type sequence by successive single base changes would be unlikely, because intermediates would be less fit and unlikely to establish themselves. Any single mutation in domain V of strain S15 or S16 would weaken or disrupt base pairs, forming mismatches such as U-G or A-C, thus generating a more attenuated and temperature-sensitive virus that would be at a replicative disadvantage compared to the parental strain. Consistent with these predictions, the strains appeared to be extremely stable when passaged under strongly selective conditions in culture. The 5′ noncoding regions of type 1 and type 2 viruses S15/1 and S15/2 were also extremely stable under these conditions. Despite this, both strains acquired relatively high levels of neurovirulence upon L20B cell culture passage, presumably due to the instability of other attenuating determinants during passage. Mutations in the coding region of the genome are known to affect attenuation phenotypes of Sabin strains (2, 23, 34, 43). In another cell line currently used for vaccine production, reversion of S15/1 and S15/2 was substantially less and/or delayed during passage compared to the type 1 and type 2 Sabin strains, reflecting the genetic stability, or not, of domain V sequences in these viruses.
Genetic stability of polio vaccines could potentially be further improved by increasing the fidelity of the viral RNA polymerase. It has recently been shown that a single substitution in poliovirus 3Dpol (G64S) decreased the rate of mutation three- to sixfold (42), with dramatic consequences on quasispecies diversity and tropism in vivo. This is a relatively small reduction in the mutation rate given the trillions of live vaccine viruses administered annually worldwide, but it may be possible to increase polymerase fidelity more significantly, with concomitant effects on reversion frequencies at all attenuating positions.
Given sufficient time, the G64S mutation could itself revert or, like the genetically stabilized domain V derived from S15, be removed by recombination with another group C enterovirus, and this could be avoided only by inhibiting transmission. It has been shown that Sabin 3 strains with a U at nucleotide 472 do not replicate in the human gut for longer than 5 days, after which time type 3 poliovirus is eliminated or mutants with a C at nucleotide 472 become established (7). It is therefore conceivable that viruses such as strains S15, S15/1, and S15/2, which cannot revert in domain V, would not “take” very efficiently. If this were the case, rates of transmission of S15-derived strains would also be substantially lower than those of Sabin strains. As a consequence, such strains might be poorly immunogenic, requiring the administration of higher doses than those currently used, but the inefficient “take” would be an advantage when it came to the cessation of vaccination. If strains with poor “take” rates were employed as seeds for inactivated polio vaccine production, the likelihood of virus “escape” from a production plant would also be reduced, and the consequences would be less severe after live-virus vaccination has ceased.
The possibility that poliomyelitis will reemerge at some time after eradication cannot be ignored. Although inactivated polio vaccine could be used in such situations, it has been argued that monovalent OPV strains would be the most rapid and effective choice, and the use of genetically stabilized strains such as S15, S15/1, and S15/2 in this situation would have the advantage of increased safety for vaccine recipients and, potentially, a decreased likelihood of reemergence of poliomyelitis after vaccination is stopped for the second time. The strains described were not recovered under GMP conditions, but this could be readily done in principle. Given the limited time available before the worldwide eradication of wild poliovirus, the questions of funding and infrastructure for the clinical trials necessary for a new vaccine need to be tackled now by manufacturers and regulatory bodies, with the support of the WHO.
Acknowledgments
We thank Glynis Dunn for help with MAPREC assays.
REFERENCES
- 1.Bellmunt, A., G. May, R. Zell, P. Pring-Akerblom, W. Verhagen, and A. Heim. 1999. Evolution of poliovirus type I during 5.5 years of prolonged enteral replication in an immunodeficient patient. Virology 265:178-184. [DOI] [PubMed] [Google Scholar]
- 2.Bouchard, M. J., D. H. Lam, and V. R. Racaniello. 1995. Determinants of attenuation and temperature sensitivity in the type 1 poliovirus Sabin vaccine. J. Virol. 69:4972-4978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown, B., M. S. Oberste, K. Maher, and M. A. Pallansch. 2003. Complete genomic sequencing shows that polioviruses and members of human enterovirus species C are closely related in the noncapsid coding region. J. Virol. 77:8973-8984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chumakov, K. M., L. B. Powers, K. E. Noonan, I. B. Roninson, and I. S. Levenbook. 1991. Correlation between amount of virus with altered nucleotide sequence and the monkey test for acceptability of oral poliovirus vaccine. Proc. Natl. Acad. Sci. USA 88:199-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Contreras, G., K. Dimock, J. Furesz, C. Gardell, D. Hazlett, K. Karpinski, G. McCorkle, and L. Wu. 1992. Genetic characterization of Sabin types 1 and 3 polio vaccine virus following serial passage in the human intestinal tract. Biologicals 20:15-26. [DOI] [PubMed] [Google Scholar]
- 6.Davis, L. E., D. Bodian, D. Price, I. J. Butler, and J. H. Vickers. 1977. Chronic progressive poliomyelitis secondary to vaccination of an immunodeficient child. N. Engl. J. Med. 297:241-245. [DOI] [PubMed] [Google Scholar]
- 7.Dunn, G., N. T. Begg, N. Cammack, and P. D. Minor. 1990. Virus excretion and mutation by infants following primary vaccination with live oral polio vaccine from two sources. J. Med. Virol. 32:92-95. [DOI] [PubMed] [Google Scholar]
- 8.Evans, D. M., G. Dunn, P. D. Minor, G. C. Schild, A. J. Cann, G. Stanway, J. W. Almond, K. Currey, and J. V. Maizel, Jr. 1985. Increased neurovirulence associated with a single nucleotide change in a noncoding region of the Sabin type 3 polio vaccine genome. Nature 314:548-550. [DOI] [PubMed] [Google Scholar]
- 9.Georgescu, M. M., F. Delpeyroux, and R. Crainic. 1995. Tripartite genome organization of a natural type 2 vaccine/nonvaccine recombinant poliovirus. J. Gen. Virol. 76:2343-2348. [DOI] [PubMed] [Google Scholar]
- 10.Gromeier, M., B. Bossert, M. Arita, A. Nomoto, and E. Wimmer. 1999. Dual stem loops within the poliovirus internal ribosomal entry site control neurovirulence. J. Virol. 73:958-964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hara, M., Y. Saito, T. Komatsu, H. Kodama, W. Abo, S. Chiba, and T. Nakao. 1981. Antigenic analysis of polioviruses isolated from a child with agammaglobulinemia and paralytic poliomyelitis after Sabin vaccine administration. Microbiol. Immunol. 25:905-913. [DOI] [PubMed] [Google Scholar]
- 12.Iizuka, N., M. Kohara, K. Hagino-Yamagishi, S. Abe, T. Komatsu, K. Tago, M. Arita, and A. Nomoto. 1989. Construction of less neurovirulent polioviruses by introducing deletions into the 5′ noncoding sequence of the genome. J. Virol. 63:5354-5363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kew, O., V. Morris-Glasgow, M. Landaverde, C. Burns, J. Shaw, Z. Garib, J. Andre, E. Blackman, C. J. Freeman, J. Jorba, R. Sutter, G. Tambini, L. Venczel, C. Pedreira, F. Laender, H. Shimizu, T. Yoneyama, T. Miyamura, H. van Der Avoort, M. S. Oberste, D. Kilpatrick, S. Cochi, M. Pallansch, and C. de Quadros. 2002. Outbreak of poliomyelitis in Hispaniola associated with circulating type 1 vaccine-derived poliovirus. Science 296:356-359. [DOI] [PubMed] [Google Scholar]
- 14.Kew, O. M., R. W. Sutter, B. K. Nottay, M. J. McDonough, D. R. Prevots, L. Quick, and M. A. Pallansch. 1998. Prolonged replication of a type 1 vaccine-derived poliovirus in an immunodeficient patient. J. Clin. Microbiol. 36:2893-2899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kew, O. M., P. F. Wright, V. I. Agol, F. Delpeyroux, H. Shimizu, N. Nathanson, and M. A. Pallansch. 2004. Circulating vaccine-derived polioviruses: current state of knowledge. Bull. W. H. O. 82:16-23. [PMC free article] [PubMed] [Google Scholar]
- 16.Kohara, M., S. Abe, I. Yoshioka, and A. Nomoto. 1993. Development of candidates for new type 2 and type 3 oral poliovirus vaccines. Dev. Biol. Stand. 78:141-148. [PubMed] [Google Scholar]
- 17.Kuge, S., N. Kawamura, and A. Nomoto. 1989. Strong inclination toward transition mutation in nucleotide substitutions by poliovirus replicase. J. Mol. Biol. 207:175-182. [DOI] [PubMed] [Google Scholar]
- 18.Liu, H. M., D. P. Zheng, L. B. Zhang, M. S. Oberste, O. M. Kew, and M. A. Pallansch. 2003. Serial recombination during circulation of type 1 wild-vaccine recombinant polioviruses in China. J. Virol. 77:10994-11005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Macadam, A. J., C. Arnold, J. Howlett, A. John, S. Marsden, F. Taffs, P. Reeve, N. Hamada, K. Wareham, J. Almond, et al. 1989. Reversion of the attenuated and temperature-sensitive phenotypes of the Sabin type 3 strain of poliovirus in vaccinees. Virology 172:408-414. [DOI] [PubMed] [Google Scholar]
- 20.Macadam, A. J., G. Ferguson, J. Burlison, D. Stone, R. Skuce, J. W. Almond, and P. D. Minor. 1992. Correlation of RNA secondary structure and attenuation of Sabin vaccine strains of poliovirus in tissue culture. Virology 189:415-422. [DOI] [PubMed] [Google Scholar]
- 21.Macadam, A. J., G. Ferguson, D. M. Stone, J. Meredith, J. W. Almond, and P. D. Minor. 2001. Live-attenuated strains of improved genetic stability. Dev. Biol. (Basel) 105:179-187. [PubMed] [Google Scholar]
- 22.Macadam, A. J., S. R. Pollard, G. Ferguson, G. Dunn, R. Skuce, J. W. Almond, and P. D. Minor. 1991. The 5′ noncoding region of the type 2 poliovirus vaccine strain contains determinants of attenuation and temperature sensitivity. Virology 181:451-458. [DOI] [PubMed] [Google Scholar]
- 23.Macadam, A. J., S. R. Pollard, G. Ferguson, R. Skuce, D. Wood, J. W. Almond, and P. D. Minor. 1993. Genetic basis of attenuation of the Sabin type 2 vaccine strain of poliovirus in primates. Virology 192:18-26. [DOI] [PubMed] [Google Scholar]
- 24.Macadam, A. J., D. M. Stone, J. W. Almond, and P. D. Minor. 1994. The 5′ noncoding region and virulence of poliovirus vaccine strains. Trends Microbiol. 2:449-454. [DOI] [PubMed] [Google Scholar]
- 25.MacCallum, F. O. 1971. Hypogammaglobulinaemia in the United Kingdom. VII. The role of humoral antibodies in protection against and recovery from bacterial and virus infections in hypogammaglobulinaemia. Spec. Rep. Ser. Med. Res. Counc. G. B. 310:72-85. [PubMed] [Google Scholar]
- 26.MacLennan, C., G. Dunn, A. P. Huissoon, D. S. Kumararatne, J. Martin, P. O'Leary, R. A. Thompson, H. Osman, P. Wood, P. Minor, D. J. Wood, and D. Pillay. 2004. Failure to clear persistent vaccine-derived neurovirulent poliovirus infection in an immunodeficient man. Lancet 363:1509-1513. [DOI] [PubMed] [Google Scholar]
- 27.McGoldrick, A., A. J. Macadam, G. Dunn, A. Rowe, J. Burlison, P. D. Minor, J. Meredith, D. J. Evans, and J. W. Almond. 1995. Role of mutations G-480 and C-6203 in the attenuation phenotype of Sabin type 1 poliovirus. J. Virol. 69:7601-7605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Minor, P. D. 1992. The molecular biology of polio vaccines. J. Gen. Virol. 73:3065-3077. [DOI] [PubMed] [Google Scholar]
- 29.Minor, P. D., G. Dunn, D. M. Evans, D. I. Magrath, A. John, J. Howlett, A. Phillips, G. Westrop, K. Wareham, J. W. Almond, et al. 1989. The temperature sensitivity of the Sabin type 3 vaccine strain of poliovirus: molecular and structural effects of a mutation in the capsid protein VP3. J. Gen. Virol. 70:1117-1123. [DOI] [PubMed] [Google Scholar]
- 30.Minor, P. D., G. Dunn, M. E. Ramsay, and D. Brown. 2005. Effect of different immunisation schedules on the excretion and reversion of oral polio vaccine strains. J. Med. Virol. 75:153-160. [DOI] [PubMed] [Google Scholar]
- 31.Pipkin, P. A., D. J. Wood, V. R. Racaniello, and P. D. Minor. 1993. Characterisation of L cells expressing the human poliovirus receptor for the specific detection of polioviruses in vitro. J. Virol. Methods 41:333-340. [DOI] [PubMed] [Google Scholar]
- 32.Pollard, S. R., G. Dunn, N. Cammack, P. D. Minor, and J. W. Almond. 1989. Nucleotide sequence of a neurovirulent variant of the type 2 oral poliovirus vaccine. J. Virol. 63:4949-4951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Racaniello, V. R. 2006. One hundred years of poliovirus pathogenesis. Virology 344:9-16. [DOI] [PubMed] [Google Scholar]
- 34.Ren, R. B., E. G. Moss, and V. R. Racaniello. 1991. Identification of two determinants that attenuate vaccine-related type 2 poliovirus. J. Virol. 65:1377-1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sabin, A. B. 1959. Present position of immunization against poliomyelitis with live virus vaccines. Br. Med. J. 15:663-680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sabin, A. B. 1957. Properties and behavior of orally administered attenuated poliovirus vaccine. JAMA 164:1216-1223. [DOI] [PubMed] [Google Scholar]
- 37.Sedivy, J. M., J. P. Capone, U. L. RajBhandary, and P. A. Sharp. 1987. An inducible mammalian amber suppressor: propagation of a poliovirus mutant. Cell 50:379-389. [DOI] [PubMed] [Google Scholar]
- 38.Skinner, M. A., V. R. Racaniello, G. Dunn, J. Cooper, P. D. Minor, and J. W. Almond. 1989. New model for the secondary structure of the 5′ non-coding RNA of poliovirus is supported by biochemical and genetic data that also show that RNA secondary structure is important in neurovirulence. J. Mol. Biol. 207:379-392. [DOI] [PubMed] [Google Scholar]
- 39.Slobodskaya, O. R., A. P. Gmyl, S. V. Maslova, E. A. Tolskaya, E. G. Viktorova, and V. I. Agol. 1996. Poliovirus neurovirulence correlates with the presence of a cryptic AUG upstream of the initiator codon. Virology 221:141-150. [DOI] [PubMed] [Google Scholar]
- 40.Strebel, P. M., R. W. Sutter, S. L. Cochi, R. J. Biellik, E. W. Brink, O. M. Kew, M. A. Pallansch, W. A. Orenstein, and A. R. Hinman. 1992. Epidemiology of poliomyelitis in the United States one decade after the last reported case of indigenous wild virus-associated disease. Clin. Infect. Dis. 14:568-579. [DOI] [PubMed] [Google Scholar]
- 41.van der Werf, S., J. Bradley, E. Wimmer, F. W. Studier, and J. J. Dunn. 1986. Synthesis of infectious poliovirus RNA by purified T7 RNA polymerase. Proc. Natl. Acad. Sci. USA 83:2330-2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vignuzzi, M., J. K. Stone, J. J. Arnold, C. E. Cameron, and R. Andino. 2006. Quasispecies diversity determines pathogenesis through cooperative interactions in a viral population. Nature 439:344-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Westrop, G. D., K. A. Wareham, D. M. Evans, G. Dunn, P. D. Minor, D. I. Magrath, F. Taffs, S. Marsden, M. A. Skinner, G. C. Schild, and J. W. Almond. 1989. Genetic basis of attenuation of the Sabin type 3 oral poliovirus vaccine. J. Virol. 63:1338-1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.World Health Organization. 1983. Requirements for poliomyelitis vaccine (oral). WHO Tech. Rep. Ser. 687:107-175. [Google Scholar]