Abstract
Neuraminidase inhibitors (NAIs) are antivirals designed to target conserved residues at the neuraminidase (NA) enzyme active site in influenza A and B viruses. The conserved residues that interact with NAIs are under selective pressure, but only a few have been linked to resistance. In the A/Wuhan/359/95 (H3N2) recombinant virus background, we characterized seven charged, conserved NA residues (R118, R371, E227, R152, R224, E276, and D151) that directly interact with the NAIs but have not been reported to confer resistance to NAIs. These NA residues were replaced with amino acids that possess side chains having similar properties to maintain their original charge. The NA mutations we introduced significantly decreased NA activity compared to that of the A/Wuhan/359/95 recombinant wild-type and R292K (an NA mutation frequently reported to confer resistance) viruses, which were analyzed for comparison. However, the recombinant viruses differed in replication efficiency when we serially passaged them in vitro; the growth of the R118K and E227D viruses was most impaired. The R224K, E276D, and R371K mutations conferred resistance to both zanamivir and oseltamivir, while the D151E mutation reduced susceptibility to oseltamivir only (∼10-fold) and the R152K mutation did not alter susceptibility to either drug. Because the R224K mutation was genetically unstable and the emergence of the R371K mutation in the N2 subtype is statistically unlikely, our results suggest that only the E276D mutation is likely to emerge under selective pressure. The results of our study may help to optimize the design of NAIs.
Analysis of the influenza virus neuraminidase (NA) active site revealed residues that are conserved in all NA subtypes (6), including catalytic sites (R118, D151, R152, R224, E276, R292, R371, and Y406) (in N2 numbering) that directly interact with the substrate and framework sites (E119, R156, W178, S179, D/N198, I222, E227, H274, E277, N294, and E425) that support the catalytic residues (3, 7, 8, 16). The design of NA inhibitors (NAIs) was based on the conserved structure of the NA active site (36). NAIs interrupt the virus replication cycle by preventing the release of virus from infected cells and may interfere with the initiation of infection (6, 24).
The optimal design of an antimicrobial compound requires an understanding of the molecular mechanisms that confer resistance to that agent. NAIs interact with multiple residues in the NA active site, but NA mutations selected from in vitro or in vivo experiments are limited to several conserved or semiconserved residues: R292K and E119G/A/D/V in N9 and N2 subtypes; H274Y in the N1 subtype; and E119G, D198N, R152K in influenza B virus NA (12, 26, 27). Influenza virus variants with the N294S mutation in NA were recently isolated after oseltamivir treatment from patients infected with either H3N2 or H5N1 influenza viruses (20, 21). In addition, broad screening for the susceptibility of influenza virus to NAIs also identified viruses with natural variations at several conserved or semiconserved NA residues (25; Neuraminidase Inhibitor Susceptibility Network, unpublished data), suggesting that mutations at other NA residues may also confer resistance.
With increasing clinical use and stockpiling of NAIs for pandemic preparedness, it is important to further elucidate the possible causes of resistance to this class of drugs. The potential ability of other conserved and/or semiconserved NA residues to confer resistance to NAIs requires further exploration, and additional information about the biological properties of the conserved NA residues will also help to refine the design of existing NAIs. Mutagenesis studies of the conserved NA residues using expressed NA proteins of A/Tokyo/3/67 (H2N2) and B/Lee/40 viruses showed that amino acid substitutions at conserved NA residues may decrease NA enzymatic activity (10, 22, 23, 37). As an aid to drug design, site-directed mutagenesis has been used to investigate the effect of mutation of conserved NA residues of B/Lee/40; however, the NAI sensitivity of the expressed NA proteins was not assayed (10). Amino acid substitution of residues 119 and 227 in the N9 glycoprotein of NWS-G70c virus can decrease NA enzymatic activity, and expressed NA with E119Q/T/G/A/V mutations showed reduced sensitivity to 4-guanidino-Neu5Ac2en (zanamivir) (11). However, all of these studies were based on analysis of expressed NA proteins; the effect of the NA mutations on the biological viability of the virus was not studied. Although reverse genetics has been used to generate recombinant viruses carrying NA mutations in the influenza A virus H3N2 background (38), the H1N1 background (1), and the influenza B virus background (19), the main focus of those studies was to characterize the conserved or semiconserved NA residues previously reported to be associated with NAI resistance. The role of other conserved or semiconserved NA residues in NAI resistance is still not clear.
We previously studied the effect of two clinically derived NA mutations (E119V and R292K) in A/Wuhan/359/95 (H3N2) recombinant virus background (38). We observed that different NA mutations may result in different levels of NAI resistance and NA functional loss (38). In the present study, we used a similar approach to characterize conserved NA residues that have not been associated with NAI resistance in the N2 subtype. We created mutations based on hypotheses arising from structural analysis of the NA active site rather than on the resistance mutations that have been identified clinically. Seven mutations (R118K, R371K, E227D, D151E, R152K, R224K, and E276D) studied here have never been reported to confer resistance in the N2 background (D151E has been reported as a natural variation [25]). The recombinant wild-type virus and a recombinant virus carrying the previously characterized R292K mutation were included as controls. The NA enzymatic activity, NAI resistance, viability, and genetic stability of recombinant A/Wuhan/359/95 (H3N2) viruses carrying these NA mutations were characterized.
MATERIALS AND METHODS
Compounds.
The NAI oseltamivir carboxylate (oseltamivir) [GS4071; 4-N-acetyl-5-amino-3-(1-ethylpropoxy)-1-cyclohexane-1 carboxylic acid] was provided by Hoffmann-La Roche, Inc. (Nutley, NJ). Zanamivir (GG167; 4-guanidino-Neu5Ac2en) was provided by the R. W. Johnson Pharmaceutical Research Institute (Raritan, NJ). The compounds were dissolved in distilled water, and aliquots were stored at −20°C until they were used.
Cells.
MDCK and human embryonic kidney 293T cells were obtained from the American Type Culture Collection (Manassas, VA). MDCK cells were maintained in minimal essential medium (MEM) with 5% fetal bovine serum and antibiotics antimycotics (antibiotics/antimycotics; 100 U of penicillin, 0.1 mg of streptomycin, and 0.25 μg of amphotericin B per ml) (Sigma, St. Louis, MO). 293T cells were maintained in OptiMEM (Invitrogen, Carlsbad, CA) with 5% fetal bovine serum and antibiotics/antimycotics. MEM with 0.3% bovine serum albumin, antibiotics/antimycotics, and 1 μg of TPCK (tolylsulfonyl phenylalanyl chloromethyl ketone)-treated trypsin (Worthington, Lakewood, NJ) per ml was used as an infection medium for MDCK cells.
Generation of A/Wuhan/359/95-like viruses by reverse genetics.
Wild-type A/Wuhan/359/95-like (H3N2) influenza virus (referred to hereafter as A/Wuhan/359/95 virus) provided by Hoffmann-La Roche, Inc., was used as the backbone of recombinant viruses generated in the present study. Eight plasmids were constructed, each containing the cDNA of one of the eight gene segments of the wild-type virus, as described previously (38). Mutations at conserved NA catalytic residues (R118K, D151E, R152K, R224K, E227D, E276D, and R371K) were separately introduced into the NA plasmids by using a QuikChange site-directed mutagenesis kit (Stratagene, La Jolla, CA). The constructed plasmids were sequenced to ensure their identity to the field strain. Recombinant viruses that were identical with the exception of a single amino acid change in a conserved NA residue were rescued in parallel in the presence or absence of 2 mU of Clostridium perfringens NA (Sigma, St. Louis, MO) per ml in the supernatant by transfecting 293T cells (17). Transfection allowed the generation of the recombinant virus even with a large deletion in the coding region of the NA, as shown previously (9). The recombinant viruses generated by reverse genetics were designated the R118K, D151E, R152K, R224K, E227D, E276D, and R371K viruses. The NA plasmid containing the R292K mutation (constructed previously) and the wild-type NA plasmid were used to generate recombinant R292K and wild-type viruses for comparison (38). The HA and NA genes of all recombinant viruses were verified by sequence analysis.
Passage of the recombinant viruses in MDCK cells.
Mutations at conserved NA residues may impair NA stability and/or enzymatic activity. To assay the genetic stability and growth of the recombinant viruses, we rescued each in the presence or absence of 2 mU of C. perfringens NA per ml and subsequently passaged it five times at 37°C for 72 h in MDCK cells in the presence or absence of 2 mU of C. perfringens NA per ml. Because storage and freezing-thawing procedures might further damage NA protein, we conducted nonstop serial passages of the recombinant viruses in MDCK cells. Since plaque assay as a method for the determination of the multiplicity of infection (MOI) requires a 3-day incubation period, we determined the virus dose for the next passage based on the hemagglutinin (HA) agglutination/unit, except a 1:50 dilution of transfection supernatant was used for all recombinant viruses at the first passage. We previously determined the correlation of the HA titer and PFU per ml of the A/Wuhan/359/95 recombinant wild-type virus, and the dilution factor based on HA titer will give a corresponding MOI at ca. 0.0001 to 0.01 PFU/cell, which is within the dose range of a multicycle infection. The HA titers were determined with 0.5% turkey red blood cells at 4°C for 30 min. The virus yield (in PFU/ml) and plaque morphology were recorded for each passage separately.
Plaque assay in MDCK cells.
Confluent MDCK cells were incubated for 1 h at 37°C with 10-fold serial dilutions of virus in 1 ml of infection medium. The cells were then washed and overlaid with freshly prepared MEM containing 0.3% bovine serum albumin, 0.9% Bacto agar, and 1 μg of TPCK trypsin/ml. The plaques were visualized after incubation at 37°C for 3 days by staining with a 0.1% crystal violet solution containing 10% formaldehyde.
Concentration of the viruses.
The concentrated virus preparations were made after three passages in MDCK cells in the presence of 2 mU of C. perfringens NA per ml. The genetic stability of the recombinant viruses was monitored by plaque morphology. Only R118K and E227D viruses were not able to maintain a homogeneous virus population, and thus the concentrated virus preparation of these two recombinant viruses was not used to determine their NA activity and sensitivity to NAIs. The culture supernatants were clarified by centrifugation at 450 × g for 30 min. Virus particles were pelleted at 57,000 × g for 1.5 h at 4°C and purified by centrifugation through a continuous 25 to 70% sucrose gradient at 76,000 × g for 2.5 h at 4°C. Fractions containing virus particles were collected and centrifuged at 76,000 × g for 2.5 h at 4°C. Virus pellets were resuspended in STE buffer (0.05 M Tris-HCl, 0.01 M EDTA, 0.1 M NaCl), and aliquots were stored at −70°C.
NA activity and NA inhibition assays.
A modified fluorometric assay was used to determine the NA activity of the viruses after the third passage in MDCK cells (15, 30). The NA assay was done in 33 mM morpholineethanesulfonic acid (Sigma) and 4 mM CaCl2 with the fluorogenic substrate 2′-(4-methylumbelliferyl)-α-d-N-acetylneuraminic acid (MUNANA; Sigma) at a final concentration of 100 μM. The pH of the enzyme buffer was adjusted to 7.2 to assay the NA activity in order to resemble the pH of MDCK cell culture media. The reaction was incubated at 37°C for 30 min and stopped by the addition of 150 μl of stop solution (0.014 M NaCl and 0.1 M glycine in 25% ethanol; pH 10.7). The fluorescence of the released 4-methylumbelliferone was measured in a Fluoroskan II (Labsystems, Helsinki, Finland) spectrophotometer using excitation and emission wavelengths of 355 and 460 nm, respectively. Before the determination of NA activity, the concentrated recombinant virus preparations were standardized on the basis of the intensity of the M1 protein band by sodium dodecyl sulfate-polyacrylamide gel electrophoresis in a 12% polyacrylamide gel. Enzyme activity was expressed as the quantity of substrate (in picomoles) converted during 30 min of incubation at 37°C per ng of M1 protein. The NA inhibition was assayed with viruses standardized to the equivalent NA enzyme activity and incubated with oseltamivir or zanamivir at concentrations of 0.00005 to 10 μM (16). The drug concentration required to inhibit 50% of the NA enzymatic activity (IC50) was determined by plotting the percent inhibition of NA activity as a function of the compound concentration calculated from the dose-response curve.
RT-PCR and sequencing.
The NA genes of viruses that formed plaques that differed in morphology were sequenced as follows. The plaques were visualized by staining with 0.01% neutral red and were individually picked and incubated overnight at 4°C with 250 μl of infection medium. The RNeasy Kit (QIAGEN, Chatsworth, CA) was used to extract vRNA, and the One-Step RT-PCR kit (QIAGEN) was used for reverse transcription-PCR (RT-PCR) according to the protocol provided. Universal primers were used for amplification (18). A TOPO TA cloning kit for sequencing (Invitrogen) was used to analyze the viral sequences obtained after the fifth passage in MDCK cells. Viral RNAs were extracted from the culture supernatant, and one-step RT-PCR was done as described above. PCR products were gel purified with the QIAquick gel extraction kit (QIAGEN), ligated to the pCR4-TOPO vector (Invitrogen), and used for the transformation of TOP10 cells (Invitrogen). Plasmid DNA was prepared by using the QIAprep Spin Miniprep Kit (QIAGEN). Ten plasmids of the NA genes were sequenced for each virus. The HA genes of the recombinant viruses were also amplified by RT-PCR and sequenced without cloning into the TOPO TA cloning vectors. The sequences were determined by the Hartwell Center for Bioinformatics and Biotechnology at St. Jude Children's Research Hospital by using BigDye terminator (v. 3) chemistry and synthetic oligonucleotides. Samples were analyzed on Applied Biosystems 3700 DNA analyzers.
RESULTS AND DISCUSSION
Generation of the recombinant viruses by reverse genetics.
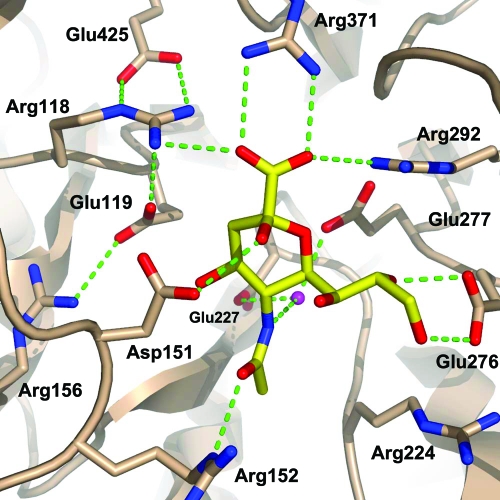
We studied seven charged, conserved NA residues that directly interact with the NAIs but have not been reported to be associated with NAI resistance. To evaluate the ability of the mutations to confer clinical resistance, we included recombinant virus carrying R292K mutation in an NA as a control. R292K mutation is one of the mutations most frequently reported to be associated with NAI resistance (16, 26). Previously, we observed that recombinant virus with this mutation showed compromised fitness and transmissibility in ferrets (38). The wild-type recombinant virus, which was also characterized previously (38), was included for comparison. The location of the conserved residues characterized in the present study (R118, R292, R371, E227, R152, R224, E276, and D151) and their interaction with other NA residues is shown in Fig. 1 with the structure of A/Tokyo/3/67 (H2N2) NA complexed with sialic acid [The RCSB Protein Data Bank (PDB) code: 2bat; http://www.rcsb.org/pdb/].
FIG. 1.
Structure of the complex between A/Tokyo/3/67 (H2N2) influenza virus NA and sialic acid (PDB code: 2bat). The conserved NA residues (R118, D151, R152, R224, E227, E276, R292, and R371) addressed in the present study were drawn together with sialic acid. Hydrogen bonds are shown as green dotted lines, and a conserved water molecule is drawn as a magenta sphere. The picture was drawn by using PyMol application software.
The use of site-directed mutagenesis and plasmid-based reverse genetics allowed us not only to evaluate the effect of conserved residues on NAI resistance but also to assay the viability of the recombinant viruses carrying mutations of those residues. In the seven new recombinant viruses generated in the present study, the NA residues were substituted with amino acids that possess side chains having similar properties (R↔ K and E↔ D) in order to maintain their original charge. Only one nucleotide change was required to encode the amino acid changes at these locations, with the exception of R→K at position 371, which required three nucleotide changes (CGC→AAG) (Table 1) .
TABLE 1.
Recombinant influenza viruses generated by reverse genetics for this study and their interactions with NAIsa
| Recombinant virusb | Nucleotide changes | Interaction of the residue with:
|
||
|---|---|---|---|---|
| Sialic acid | Oseltamivir carboxylate | Zanamivir | ||
| R118K | AGA→AAA | Carboxylate group | Carboxylate group | Carboxylate group |
| R292K | AGA→AAA | Carboxylate group | Carboxylate group | Carboxylate group |
| R371K | CGC→AAG | Carboxylate group | Carboxylate group | Carboxylate group |
| E227D | GAG→GAT | No direct interactionc | Amino group | Guanidino group |
| R152K | AGG→AAG | Amide nitrogen | Amide nitrogen | Amide nitrogen |
| R224K | AGG→AAG | Glycerol side chain | Pentyl ether group | Glycerol side chain |
| E276D | GAG→GAT | Glycerol side chain | Pentyl ether group | Glycerol side chain |
| D151E | GAT→GAG | Acid/base catalyst | Acid/base catalyst | Acid/base catalyst |
The interactions of the residues with sialic acid, oseltamivir carboxylate, or zanamivir were based on previously published results (27, 31, 33).
Each recombinant virus contained a mutation at one of the eight charged conserved NA residues that interact directly with NAIs.
E227 interacts indirectly with sialic acid by hydrogen bonding to a water molecule that hydrogen bonds to the amide of the sialic acid N-acetyl group.
The NAIs were structure-based designed, and each has modifications that differentiate them from the natural substrate, sialic acid. Zanamivir is modified at C4, where the hydroxyl group of sialic acid is substituted with a guanidino group (21). Oseltamivir has not only a cyclohexene ring instead of a sugar ring but also modifications at both C4 (hydroxyl group → amino group) and C6 (glycerol side chain → pentyl ether group) (27). Table 1 summarizes the interactions of the NAI functional groups with each of the mutant conserved catalytic residues that were characterized.
We were able to rescue all of the recombinant viruses from transfected 293T cells as described previously (17). We performed plaque assay with the transfection supernatant and observed that all recombinant viruses formed pinpoint-sized plaques (mean ± the standard deviation [SD]; 0.3 ± 0.2 mm in diameter); in particular, the R118K and E227D viruses form unclear plaques that are not easily recognized. On the other hand, the wild-type virus formed significantly larger plaques (2.0 ± 0.2 mm in diameter) (P < 0.05) (38). We showed before that a single R292K mutation in the NA can significantly reduce the plaque size due to decreased NA enzymatic activity (38). The fact that all recombinant viruses formed significantly smaller plaques suggested that the seven mutations that were introduced individually into the recombinant viruses reduced the NA enzymatic activity of the viruses.
Residues 118, 292, and 371 that interact with the carboxylate group of sialic acid, oseltamivir carboxylate, or zanamivir.
Three conserved arginines (R118, R371, and R292) form a triad that interacts with the carboxylate group of the substrate (Table 1). Residue 292 (R→K) is frequently substituted among clinically derived NAI-resistant influenza variants in the N2 subtype (16, 26). No reports have been published regarding R118 and R371 being associated with NAI resistance in any NA subtype.
(i) Growth in MDCK cells.
To assay the growth and genetic stability of the recombinant viruses in vitro, we serially passaged each virus five times in MDCK cells. Serial passages were done in parallel in the presence or absence of 2 mU of C. perfringens NA/ml to determine whether the recombinant viruses would require additional NA activity for growth in MDCK cells. We observed that both R292K and R371K viruses had sufficient NA activity to replicate efficiently in MDCK cells: (i) the virus yields at each passage did not differ significantly in the absence or in the presence of C. perfringens NA since the second passage (due to differences in transfection efficiency, slight difference in viral yield was observed in the first passage), and (ii) both R292K and R371K viruses maintained the small-plaque phenotype in the absence of bacterial NA (Table 2). However, R118K virus was unable to grow in the absence of C. perfringens NA: growth was not detectable in the culture supernatant by plaque assay (detection limit < 10 PFU/ml) or by RT-PCR assay (Table 2). Although R118K virus does grow in the presence of C. perfringens NA, it was unable to maintain a homogeneous small-plaque phenotype: large plaques were observed at the third passage (0.7%), and the wild-type population continued to increase during the subsequent passages (14.3 and 32.1% for fourth and fifth passages, respectively) (Table 2).
TABLE 2.
Characterization of R292K, R371K, and R118K virusesa
| Reverse genetics virus | Growth of the virus in MDCK cellsb
|
NA activity (mean pmol/30 min ng−1 ± SD) | IC50 (nM)c
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| C. perfringens NA | First passage
|
Third passage
|
Fifth passage
|
|||||||
| Virus titer | Plaque size (%) | Virus titer | Plaque size (%) | Virus titer | Plaque size (%) | Oseltamivir carboxylate | Zanamivir | |||
| Wild type | − | 7.4 | L (100) | 7.7 | L (100) | 7.5 | L (100) | 2,861.4 ± 107.2 | 0.5 | 2.8 |
| R292K | − | 3.4 | S (100) | 7.3 | S (100) | 7.5 | S (97), L (3) | 171.6 ± 33.9 | >30,000 (+++) | 19.9 |
| + | 5.6 | S (100) | 7.3 | S (100) | 7.6 | S (100) | ||||
| R371K | − | 4.0 | S (100) | 7.3 | S (100) | 7.0 | S (100) | 74.2 ± 25.4 | 23.4 (+) | 46.3 (+) |
| + | 5.0 | S (100) | 7.4 | S (100) | 6.9 | S (100) | ||||
| R118K | − | <1.0 | NAV | <1.0 | NAV | <1.0 | NAV | ND | ND | ND |
| + | 2.8 | S (100) | 5.8 | S (99.3), L (0.7) | 7.7 | S (67.9), L (32.1) | ||||
Data for the second and fourth passages were determined but are not shown for the sake of brevity. ND, not determined due to compromised growth of the virus.
The recombinant viruses were grown in the presence (+) or absence (−) of 2 mU of C. perfringens NA/ml during the five serial passages in MDCK cells. NAV, not available. Virus titers were determined by plaque assay in MDCK cells in the absence of C. perfringens NA and expressed as the log10 PFU/ml. Plaque sizes: S, small (0.2 to 0.6 mm in diameter); L, large (1.0 to 2.0 mm in diameter), as determined by the Finescale comparator (Los Angeles, CA). The percentage of small or large plaques is shown in parentheses.
Drug resistance is expressed as a multiple of the IC50 of the wild-type virus as determined by NA inhibition assay: +, multiple > 10; ++, multiple > 100; +++, multiple > 1,000.
(ii) Sequence analysis.
To determine whether the recombinant viruses remained genetically stable after serial passage in MDCK cells, we sequenced their NA genes after the fifth passages in the absence of C. perfringens NA. The NA genes of the recombinant viruses were amplified by RT-PCR and cloned into TOPO TA cloning vectors. Sequencing of the plasmids allowed us to avoid the genetic dominant sequence and to obtain broader information about genetic differences within the virus population. All 10 clones from R292K and all 10 clones from R371K viruses maintained the introduced mutations. The R118K virus was not analyzed due to its inability to grow in the absence of C. perfringens.
The HA sequence of the recombinant viruses was also analyzed after the fifth passage in MDCK cells in the absence of C. perfringens. Instead of cloning the amplified HA gene into TOPO TA cloning vectors, we sequenced the RT-PCR product. Neither the R371K nor the R292K virus contained any amino acid changes in HA after five serial passages in MDCK cells.
(iii) Sensitivity to NAIs and NA activity.
The R371K virus conferred resistance to both oseltamivir carboxylate (∼45-fold) and zanamivir (∼15-fold) (Table 2), while the sensitivity of R292K virus to these drugs was comparable to that reported previously (16, 38). The NA activity of R292K and R371K viruses was significantly lower than that of the wild-type virus (Table 2). However, R292K virus had a significantly higher NA activity (171.6 ± 33.9 pmol/30 min ng−1) than the R371K virus (74.2 ± 25.4 pmol/30 min ng−1) (Table 2). We were not able to assay the NA activity of R118K virus due to its inability to maintain a homogeneous virus population even in the presence of bacterial NA. Therefore, a homogeneous concentrated virus preparation could not be made for this virus.
(iv) Structure analysis.
The R371 was previously considered the most important residue among the three arginines that interact with the carboxylate group of sialic acid (5) (Fig. 1). However, the distinct growth efficiency of the R118K, R292K, and R371K recombinant viruses suggests that conserved residue R118 is actually the most important of the three, since its growth is severely compromised in MDCK cells. The structure of the complex formed by A/Tokyo/3/67 (H2N2) influenza virus NA and sialic acid (Fig. 1) confirms the importance of residue R118, which via its Nɛ group forms a salt bridge with E425; this interaction is conserved in all NA subtypes. R118 (through its Nη1 group) also interacts with E119, which in turn interacts with R156. Therefore, there is a salt-bridge complex, or relay, from E425 to R118 to E119 to R156. Mutation of R118 to a lysine probably disrupts this network, since the Nζ group of a lysine is probably unable to span the E425 and E119 interactions (Fig. 1). On the other hand, R292K, frequently reported to confer resistance to NAIs in vitro or in vivo (16, 26), would probably have little effect on the structure around position 292. The amino group would still be in a position to interact with the side chains of N294, E277, and Y406. We also found the R292K virus to possess the highest NA activity and genetic stability among the recombinant viruses assayed, suggesting that the ability to maintain a certain level of NA enzymatic activity is an important determinant of the emergence of NAI-resistant variants from the viral quasispecies in nature. The genetic stability of R371 can also be explained structurally. R371 forms a bifurcated interaction with the carboxyl group of the ligand. As a lysine, the Cζ position would be replaced by an amino group that would still be able to participate in a salt-bridge interaction with the carboxylate. However, alignment of N2 sequences from influenza viruses of an avian, swine, or human origin revealed that the predominant nucleotide sequence encoding residue 371 is CGC, although CGT, CGA, and CGG were present in some isolates. At least two nucleotide changes (CGA→AAA) are required to produce a virus with this NA mutation. Therefore, an amino acid change from R to K at position 371 is unlikely to occur in nature and indeed has not been reported among naturally occurring NAI-resistant variants.
Residue 227 that interacts with the C4 group of zanamivir and oseltamivir carboxylate.
Glutamic acid at residues 119 and 227 interacts with the C4 guanidino group of zanamivir (36) and possibly with the C4 amino group of oseltamivir (Table 1). Therefore, both E119 and E227 are under selective pressure of the NAIs. Amino acid substitution of E119 is associated with resistance to zanamivir (E119A/D/G) (2, 13, 26, 28) and oseltamivir (E119V) (4). We further analyzed recombinant virus with the E227D mutation because there is no information about the role of this mutation in NAI resistance.
(i) Growth in MDCK cells.
The growth of the E227D virus was compromised in the absence of C. perfringens NA, since growth was not detected by plaque assay (detection limit < 10 PFU/ml) until the fourth passage (data not shown). The E227D virus grew in the presence of C. perfringens NA, but it was not able to maintain a homogeneous small-plaque phenotype: large plaques were observed at the third passage, and the wild-type population continued to increase during the subsequent passages (Table 3).
TABLE 3.
Characterization of E227D virusa
| Reverse genetics virus | Growth of the virus in MDCK cellsb
|
NA activity (mean pmol/30 min ng−1 ± SD) | IC50 (nM)
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| C. perfringens NA | First passage
|
Third passage
|
Fifth passage
|
|||||||
| Virus titer | Plaque size (%) | Virus titer | Plaque size (%) | Virus titer | Plaque size (%) | Oseltamivir carboxylate | Zanamivir | |||
| E227D | − | <1.0 | NAV | <1.0 | NAV | 2.0 | S (100) | ND | ND | ND |
| + | 4.0 | S (100) | 7.3 | S (88.1), L (11.9) | 6.8 | S (72), L (28) | ND | ND | ND | |
Data for the second and fourth passages were determined but are not shown for the sake of brevity. ND, not determined due to compromised growth of the virus.
The recombinant viruses were grown in the presence (+) or absence (−) of 2 mU of C. perfringens NA/ml during the five serial passages in MDCK cells. NAV, not available. Virus titers were determined by plaque assay in MDCK cells in the absence of C. perfringens NA and expressed as the log10 PFU/ml. Plaque sizes: S, small (0.2 to 0.6 mm in diameter); L, large (1.0 to 2.0 mm in diameter), as determined by the Finescale comparator (Los Angeles, CA). The percentage of small or large plaques is shown in parentheses.
(ii) Sequence analysis.
Because the E227D virus showed significantly compromised growth in the absence of C. perfringens in MDCK cells, we did not assay its genetic stability, since this mutation had already significantly impaired NA function.
(iii) Sensitivity to NAIs and NA activity.
We were not able to assay the NA activity and sensitivity of E227D virus because it did not maintain a homogeneous virus population even in the presence of C. perfringens NA.
(iv) Structure analysis.
The severe growth defect of E227D virus in vitro may explain why resistant variants with this mutation have not been isolated in nature. Examination of the NA structure (Fig. 1) shows that E227 has an important role in stabilizing the structure of the NA active site. E227 has several roles: (i) through one of its carboxyl oxygens, it hydrogen bonds to the Oγ of S179 and the main-chain amide of D180; (ii) through the other carboxyl oxygen, E227 hydrogen bonds to a water molecule that sits beneath, and hydrogen bonds with, the amide of the N-acetyl group of the substrate; and (iii) the same water molecule forms a hydrogen bond with E277 (Fig. 1). Shortening this side chain to an aspartic acid would disrupt several of these interactions. Overall, the significantly impaired growth of the E227D virus suggests that E227 may provide a good target for NAI refinement, since this conserved residue could not tolerate the most conserved amino acid substitution (E→D).
Residue 152 that interacts with the oxygen of the N-acetyl moiety of sialic acid and NAIs.
The R152K mutation in NA is reportedly associated with zanamivir and oseltamivir resistance in influenza B viruses (14, 16, 19), but amino acid changes at this conserved residue have not been observed in influenza A viruses. We evaluated here its potential to confer resistance to NAIs in the N2 background.
(i) Growth in MDCK cells.
The R152K mutant was able to grow in the absence of C. perfringens. However, a mixture of small and large (wild-type revertant) plaques was detected at the fourth passage, and the large plaque population increased from 6.8% (data not shown) to 14.1% in the fifth passage (Table 4). In the presence of additional NA activity, R152K virus was able to maintain a homogeneous small-plaque phenotype throughout the five serial passages (Table 4).
TABLE 4.
Characterization of R152K virusa
| Reverse genetics virus | Growth of the virus in MDCK cellsb
|
NA activity (mean pmol/30 min ng−1 ± SD) | IC50 (nM)c
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| C. perfringens NA | First passage
|
Third passage
|
Fifth passage
|
|||||||
| Virus titer | Plaque size (%) | Virus titer | Plaque size (%) | Virus titer | Plaque size (%) | Oseltamivir carboxylate | Zanamivir | |||
| R152K | − | 6.5 | S (100) | 7.1 | S (100) | 7.3 | S (85.9), L (14.1) | 50.1 ± 10.6 | 0.6 | 2.3 |
| + | 7.7 | S (100) | 6.9 | S (100) | 7.0 | S (99.2), L (0.8) | ||||
Data for the second and fourth passages were determined but are not shown for the sake of brevity.
The recombinant viruses were grown in the presence (+) or absence (−) of 2 mU of C. perfringens NA/ml during the five serial passages in MDCK cells. Virus titers were determined by plaque assay in MDCK cells in the absence of C. perfringens NA and expressed as the log10 PFU/ml. Plaque sizes: S, small (0.2 to 0.6 mm in diameter); L, large (1.0 to 2.0 mm in diameter), as determined by the Finescale comparator (Los Angeles, CA). The percentage of small or large plaques is shown in parentheses.
Drug resistance is expressed as a multiple of the IC50 of the wild-type virus as determined by NA inhibition assay: +, multiple > 10; ++, multiple > 100; +++, multiple > 1,000.
(ii) Sequence analysis.
Among 10 clones of the R152K virus that were analyzed, one (10%) showed wild-type NA sequence and nine (90%) maintained the introduced mutation. The percentage of wild-type NA (10%) was consistent with the percentage of large plaques (14.1%) in the fifth passage (Table 4). We also sequenced the HA of the R152K virus and did not find amino acid changes in the HA1 region.
(iii) Sensitivity to NAIs and NA activity.
R152K virus showed lower NA activity (50.1 × 10.6 pmol/30 min ng−1) (Table 4) compared to most recombinant viruses assayed; however, the differences in NA activity are not significantly different compared to E276D, R371K, and D151E viruses (Tables 2, 5, and 6). In addition, R152K in the N2 background did not confer resistance to oseltamivir or zanamivir. This result supports the idea that the resistance of each NA subtype should be considered separately (25, 39).
TABLE 5.
Characterization of R224K and E276D virusesa
| Reverse genetics virus | Growth of the virus in MDCK cellsb
|
NA activity (mean pmol/30 min ng−1 ± SD) | IC50 (nM)c
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| C. perfringens NA | First passage
|
Third passage
|
Fifth passage
|
|||||||
| Virus titer | Plaque size (%) | Virus titer | Plaque size (%) | Virus titer | Plaque size (%) | Oseltamivir carboxylate | Zanamivir | |||
| R224K | − | 1.3 | S (100) | 2.8 | S (91.3), L (8.7) | 8.1 | S (9), L (91) | 17.1 ± 3.2 | >2,000 (+++) | 161.5 (+) |
| + | 4.9 | S (100) | 7.5 | S (100) | 7.5 | S (84.1), L (15.9) | ||||
| E276D | − | 6.5 | S (100) | 7.1 | S (95.5), L (4.5) | 6.9 | S (71.4), L (28.6) | 95.4 ± 43.9 | 8.9 (+) | 463.8 (++) |
| + | 7.6 | S (100) | 7.0 | S (100) | 7.0 | S (100) | ||||
Data for the second and fourth passages were determined but are not shown for the sake of brevity.
The recombinant viruses were grown in the presence (+) or absence (−) of 2 mU of C. perfringens NA/ml during the five serial passages in MDCK cells. Virus titers were determined by plaque assay in MDCK cells in the absence of C. perfringens NA and expressed as the log10 PFU/ml. Plaque sizes: S, small (0.2 to 0.6 mm in diameter); L, large (1.0 to 2.0 mm in diameter), as determined by the Finescale comparator (Los Angeles, CA). The percentage of small or large plaques is shown in parentheses.
Drug resistance is expressed as a multiple of the IC50 of the wild-type virus as determined by NA inhibition assay: +, multiple > 10; ++, multiple > 100; +++, multiple > 1,000.
TABLE 6.
Characterization of D151E virusa
| Reverse genetics virus | Growth of the virus in MDCK cellsb
|
NA activity (mean pmol/30 min ng−1 ± SD) | IC50 (nM)c
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| C. perfringens NA | 1st passage
|
3rd passage
|
5th passage
|
|||||||
| Virus titer | Plaque size (%) | Virus titer | Plaque size (%) | Virus titer | Plaque size (%) | Oseltamivir carboxylate | Zanamivir | |||
| D151E | − | 1.3 | S (100) | 2.8 | S (100) | 7.9 | S (95.1), L (4.9) | 62.3 ± 8.7 | 5.4 (+) | 6.2 |
| + | 5.0 | S (100) | 7.5 | S (100) | 7.6 | S (87.2), L (12.8) | ||||
Data for the second and fourth passages were determined but are not shown for the sake of brevity.
The recombinant viruses were grown in the presence (+) or absence (−) of 2 mU of C. perfringens NA/ml during the five serial passages in MDCK cells. Virus titers were determined by plaque assay in MDCK cells in the absence of C. perfringens NA and expressed as the log10 PFU/ml. Plaque sizes: S, small (0.2 to 0.6 mm in diameter); L, large (1.0 to 2.0 mm in diameter), as determined by the Finescale comparator (Los Angeles, CA). The percentage of small or large plaques is shown in parentheses.
Drug resistance is expressed as a multiple of the IC50 of the wild-type virus as determined by NA inhibition assay: +, multiple > 10; ++, multiple > 100; +++, multiple > 1,000.
(iv) Structure analysis.
Since R152K was previously reported to confer resistance in the influenza B background (14), we overlaid the structures of influenza A/Tokyo/3/67 (H2N2) virus NA (PDB code: 2bat) and influenza B/Beijing/1/87 virus NA (PDB code: 1nsb) to compare them. Previously, recombinant B/Beijing/1/87 virus with R152K mutation in NA was shown to confer resistance to NAIs (19). We found no apparent difference between the N2 and B NA, since R152 has the same interactions with conserved residue D198. More detailed structural analysis of the complex formed by N2 NA and influenza B virus NA with NAIs is required for further insight.
Residues 224 and 276 that interact with the glycerol side chain of sialic acid and zanamivir and the pentyl ether group of oseltamivir carboxylate.
The hydrophobic faces of R224, I222, and A246 form a hydrophobic pocket to accommodate the glycerol side chain of sialic acid and zanamivir, while E276 forms a hydrogen bond with the O8 and O9 hydroxyls of the glycerol group (33, 34). The interaction of R224 and E276 with oseltamivir is different in that the glycerol side chain is substituted by a pentyl ether group (Table 1). Previous reports (32) suggest that E276 and R224 must form a salt bridge to accommodate the large hydrophobic pentyl ether group of oseltamivir.
(i) Growth in MDCK cells.
R224K virus showed inefficient growth in MDCK cells without C. perfringens NA activity: the viral yield was low for the first three passages (<103 PFU/ml). A mixture of small and large (wild-type revertant) plaques was detected at the third passage, and the large-plaque phenotype became predominant in the fourth and fifth passages (Table 5). In the presence of supplemental NA, R224K virus was genetically more stable and replicated efficiently, although a mixture of small and large plaques was detected at the fifth passage (Table 5).
E276D virus showed significantly better growth efficiency and genetic stability than the R224K virus (Table 5). It was able to replicate and reached a viral yield of >106 PFU/ml in the absence of C. perfringens NA, although the percentage of large plaques increased gradually (Table 5). In the presence of supplemental NA, E276D virus was genetically stable, since it was able to replicate efficiently in MDCK cells and maintain a homogeneous small-plaque phenotype throughout the five serial passages (Table 5).
(ii) Sequence analysis.
All 10 clones of the R224K virus that were analyzed (100%) showed the wild-type NA sequence. In addition, the HA sequence of the R224K virus was found to be identical to the original sequence. For E276D virus, 2 of 10 clones (20%) showed a wild-type NA sequence, and 8 of 10 clones (80%) maintained the E276D mutation. No amino acid change was found in the HA1 of the E276D virus after five serial passages in MDCK cells.
(iii) Sensitivity to NAIs and NA activity.
R224K virus possessed the lowest NA activity among the recombinant viruses assayed (P < 0.05) (Tables 2 to 6), except for the R118K and E227D viruses, which were not assayed. The significantly lower NA activity correlates well with the compromised growth and genetic instability of the R224K virus in MDCK cells (Table 5). R224K virus showed reduced NA sensitivity to both oseltamivir (>4,000-fold) and zanamivir (>50-fold).
On the other hand, we observed that E276D virus possessed the second highest NA activity among the recombinant viruses assayed (except for the wild type, R292K virus possessed the highest NA activity) (Table 2 and 5). It also conferred resistance to both oseltamivir (∼15-fold) and zanamivir (∼160-fold) (Table 5).
(iv) Structure analysis.
The guanidino group of R224 reacts on one side with the backbone carbonyl of G244 and on the other side with the Oγ of T242. R224 plays a vital role in that its methylene groups at Cβ, Cγ, and Cδ form part of the hydrophobic pocket that accommodates the methyl group of the N-acetyl moiety of the ligand. Therefore, the vital role of R224 is confirmed by the compromised fitness of the R224K virus in MDCK cells.
As mentioned above, E276 forms a hydrogen bond with the O8 and O9 hydroxyls of the glycerol group of sialic acid or zanamivir. Reducing the side chain to aspartic acid would probably remove these hydrogen bonds, thus conferring resistance to zanamivir. A more detailed crystal structure analysis is required to fully elucidate the mechanism. E276 and R224 must form a salt bridge to accommodate the large hydrophobic pentyl ether group of oseltamivir; since there is room for both residues to move, it is likely that the salt bridge between D276 and R224 could still form, perhaps explaining why E276D virus is only slightly resistant to oseltamivir.
Residue 151 as an acid/base catalyst.
Natural variations (G/V/N/E) at residue D151 have been identified in N1, N2, and influenza B NA in a large-scale influenza virus NAI susceptibility screening, suggesting that D151 may not be as conserved as previously thought (25). In influenza virus NA, D151 is proposed to act as the acid catalyst for the initial step involving sialyl-enzyme formation, since it is well located to hydrogen bond with the glycosidic oxygen (34). The role of residue D151 in NAI resistance was also evaluated.
(i) Growth in MDCK cells.
The growth of D151E virus in the absence of C. perfringens NA was not dramatically impaired compared to the growth of R118K or E227D viruses; however, it was not able to grow to the titer of >106 PFU/ml while maintaining a homogeneous small-plaque phenotype (Table 6). In the presence of supplemental NA activity, it was more stable and replicated more efficiently, although a mixture of small and large (wild-type revertant) plaques was observed at the fifth passage (Table 6).
(ii) Sequence analysis.
All 10 clones of the D151E virus that were analyzed maintained the D151E mutation in NA. However, the HA sequence obtained at the fifth passage in the absence of C. perfringens NA showed one amino acid change (Y→H) at residue 98. Conserved residue Y98 is located at the bottom of the receptor binding site; therefore, this amino acid change may interfere with the binding affinity of the virus. The presence of Y98H HA mutation may contribute to the increased viral yield at the fifth passage. However, the detail effect of this HA mutation requires further studies.
(iii) Sensitivity to NAIs and NA activity.
D151E virus possessed NA activity comparable to that of the R152K virus (Tables 4 and 6). It was only slightly resistant to zanamivir and oseltamivir, since the drug sensitivity decreased 2.2- and 10.8-fold, respectively. We observed that D151E showed a slight decrease in sensitivity to NAIs; this result is similar to that reported previously when natural variation at residue D151 was identified in circulating influenza viruses (25).
(iv) Structure analysis.
Within the sialyl-enzyme intermediate, D151 is well positioned to function as the general base catalyst, assisting nucleophilic attack by the hydroxyl group of a water molecule. Mutation to a glutamic acid would unbalance the role of this group. The longer side chain of E151 could turn to form a salt bridge with the adjacent R152 or interfere with the negative charge on the substrate carboxylate. However, the exact role of D151 will require a more detailed structural analysis.
Conclusion.
This study focused on seven charged conserved NA residues that directly interact with NAIs and have not been reported to confer resistance to NAIs. We hypothesized that the NA residues we studied are under strong a selective pressure of the drug and are the residues most likely to confer resistance to NAIs; on the other hand, mutations at these residues could also be the most lethal to the virus. Other conserved or semiconserved NA residues or residues near the receptor binding site of HA also have the potential to confer resistance and may require further exploration. With a single mutation at the conserved NA enzymatic site, all seven recombinant viruses that we studied showed significantly decreased NA activity compared to the recombinant wild-type and R292K viruses; however, they differed in their ability to replicate in MDCK cells. In general, we observed that the NA activity assayed at pH 7.2 correlates with the growth efficiency of the recombinant viruses; the higher the NA activity is, the better the growth. However, it is possible that our assays still have certain limitations so that some differences in enzyme activity between the recombinant viruses are not statistically significant. Preparation of concentrated recombinant viruses by ultracentrifugation may lead to the loss of the NA tetramer structure. In addition, a structurally unstable NA may not be able to tolerate temperature and pH changes as well as the wild-type NA.
Mutations in the present study that did not significantly compromise the growth of the recombinant viruses in MDCK cells and that conferred NAI resistance warrant heightened awareness, such as R371K and E276D viruses that were able to replicate with similar efficiency as the R292K virus. These mutations may have the potential to emerge after NAI treatment. Although the R292K mutation has been identified by various in vitro and in vivo studies (16, 26), the E276D mutation has not been reported to confer resistance to NAIs either in vitro or in vivo. One possible explanation is the relatively infrequent clinical use of zanamivir. E276D virus was observed to be only slightly resistant to oseltamivir, but its sensitivity to zanamivir was reduced by a factor of approximately 160. Zanamivir is administered by inhalation and is not as frequently prescribed as oseltamivir phosphate, which is taken orally. Monitoring amino acid changes should be considered at this position in patients treated with zanamivir.
The compromised growth of most recombinant viruses and the significant reduction in NA enzymatic activity of all of the recombinant viruses support the strategy originally proposed by Varghese et al. in 1998 (35) of designing an inhibitor that is as closely related as possible to the natural ligand of the target (29). Future NAI design may target those residues that are least likely to be substituted, such as R118 and E227. One possibility might be a modification of the acetamido group of the current inhibitors to include a functionality that emulates the conserved water molecule linking E227 and E277. Release of this bound water would also be thermodynamically favorable, potentially adding to the affinity of such analogues. Although our results may not be able to extrapolate to other NA subtypes, the use of site-directed mutagenesis and reverse genetics in tandem should be considered for future related studies of other NA subtypes (especially N1) of influenza A virus and influenza B virus NA with the ultimate goal of NAI refinement.
Acknowledgments
This study was supported by U.S. Public Health Service grants AI95357 and AI57570 from the National Institute of Allergy and Infectious Diseases and by the American Lebanese Syrian Associated Charities (ALSAC).
We thank Louise M. Herlocher for helpful advice and Sharon Naron for editorial assistance.
REFERENCES
- 1.Abed, Y., N. Goyette, and G. Boivin. 2004. A reverse genetics study of resistance to neuraminidase inhibitors in an influenza A/H1N1 virus. Antivir. Ther. 9:577-581. [PubMed] [Google Scholar]
- 2.Blick, T. J., T. Tiong, A. Sahasrabudhe, J. N. Varghese, P. M. Colman, G. J. Hart, R. C. Bethell, and J. L. McKimm-Breschkin. 1995. Generation and characterization of an influenza virus neuraminidase variant with decreased sensitivity to the neuraminidase-specific inhibitor 4-guanidino-Neu5Ac2en. Virology 214:475-484. [DOI] [PubMed] [Google Scholar]
- 3.Burmeister, W. P., R. W. Ruigrok, and S. Cusack. 1992. The 2.2 Å resolution crystal structure of influenza B neuraminidase and its complex with sialic acid. EMBO J. 11:49-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carr, J., J. Ives, N. Roberts, C. Y. Tai, M. Wang, M. Meng, D. Mendel, L. Kelly, R. Lambkin, and J. Oxford. 1999. An oseltamivir-treatment selected influenzaA/Wuhan/359/95 virus with an E119V mutation in the neuraminidase gene has reduced infectivity in vivo. Second International Symposium for Influenza and Other Respiratory Viruses, Grand Cayman Islands.
- 5.Chong, A. K., M. S. Pegg, N. R. Taylor, and I. M. von. 1992. Evidence for a sialosyl cation transition-state complex in the reaction of sialidase from influenza virus. Eur. J. Biochem. 207:335-343. [DOI] [PubMed] [Google Scholar]
- 6.Colman, P. M. 1994. Influenza virus neuraminidase: structure, antibodies, and inhibitors. Protein Sci. 3:1687-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Colman, P. M., P. A. Hoyne, and M. C. Lawrence. 1993. Sequence and structure alignment of paramyxovirus hemagglutinin-neuraminidase with influenza virus neuraminidase. J. Virol. 67:2972-2980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Colman, P. M., J. N. Varghese, and W. G. Laver. 1983. Structure of the catalytic and antigenic sites in influenza virus neuraminidase. Nature 303:41-44. [DOI] [PubMed] [Google Scholar]
- 9.Fujii, Y., H. Goto, T. Watanabe, T. Yoshida, and Y. Kawaoka. 2003. Selective incorporation of influenza virus RNA segments into virions. Proc. Natl. Acad. Sci. USA 100:2002-2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ghate, A. A., and G. M. Air. 1998. Site-directed mutagenesis of catalytic residues of influenza virus neuraminidase as an aid to drug design. Eur. J. Biochem. 258:320-331. [DOI] [PubMed] [Google Scholar]
- 11.Goto, H., R. C. Bethell, and Y. Kawaoka. 1997. Mutations affecting the sensitivity of the influenza virus neuraminidase to 4-guanidino-2,4-dideoxy-2,3-dehydro-N-acetylneuraminic acid. Virology 238:265-272. [DOI] [PubMed] [Google Scholar]
- 12.Gubareva, L. V. 2004. Molecular mechanisms of influenza virus resistance to neuraminidase inhibitors. Virus Res. 103:199-203. [DOI] [PubMed] [Google Scholar]
- 13.Gubareva, L. V., R. Bethell, G. J. Hart, K. G. Murti, C. R. Penn, and R. G. Webster. 1996. Characterization of mutants of influenza A virus selected with the neuraminidase inhibitor 4-guanidino-Neu5Ac2en. J. Virol. 70:1818-1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gubareva, L. V., M. N. Matrosovich, M. K. Brenner, R. C. Bethell, and R. G. Webster. 1998. Evidence for zanamivir resistance in an immunocompromised child infected with influenza B virus. J. Infect. Dis. 178:1257-1262. [DOI] [PubMed] [Google Scholar]
- 15.Gubareva, L. V., R. G. Webster, and F. G. Hayden. 2002. Detection of influenza virus resistance to neuraminidase inhibitors by an enzyme inhibition assay. Antivir. Res. 53:47-61. [DOI] [PubMed] [Google Scholar]
- 16.Gubareva, L. V., R. G. Webster, and F. G. Hayden. 2001. Comparison of the activities of zanamivir, oseltamivir, and RWJ-270201 against clinical isolates of influenza virus and neuraminidase inhibitor-resistant variants. Antimicrob. Agents Chemother. 45:3403-3408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoffmann, E., G. Neumann, Y. Kawaoka, G. Hobom, and R. G. Webster. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. USA 97:6108-6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoffmann, E., J. Stech, Y. Guan, R. G. Webster, and D. R. Perez. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146:2275-2289. [DOI] [PubMed] [Google Scholar]
- 19.Jackson, D., W. Barclay, and T. Zurcher. 2005. Characterization of recombinant influenza B viruses with key neuraminidase inhibitor resistance mutations. J. Antimicrob. Chemother. 55:162-169. [DOI] [PubMed] [Google Scholar]
- 20.Kiso, M., K. Mitamura, Y. Sakai-Tagawa, K. Shiraishi, C. Kawakami, K. Kimura, F. G. Hayden, N. Sugaya, and Y. Kawaoka. 2004. Resistant influenza A viruses in children treated with oseltamivir: descriptive study. Lancet 364:759-765. [DOI] [PubMed] [Google Scholar]
- 21.Le, Q. M., M. Kiso, K. Someya, Y. T. Sakai, T. H. Nguyen, K. H. Nguyen, N. D. Pham, H. H. Ngyen, S. Yamada, Y. Muramoto, T. Horimoto, A. Takada, H. Goto, T. Suzuki, Y. Suzuki, and Y. Kawaoka. 2005. Avian flu: isolation of drug-resistant H5N1 virus. Nature 437:1108. [DOI] [PubMed] [Google Scholar]
- 22.Lentz, M. R., and G. M. Air. 1986. Loss of enzyme activity in a site-directed mutant of influenza neuraminidase compared to expressed wild-type protein. Virology 148:74-83. [DOI] [PubMed] [Google Scholar]
- 23.Lentz, M. R., R. G. Webster, and G. M. Air. 1987. Site-directed mutation of the active site of influenza neuraminidase and implications for the catalytic mechanism. Biochemistry 26:5351-5358. [DOI] [PubMed] [Google Scholar]
- 24.Matrosovich, M. N., T. Y. Matrosovich, T. Gray, N. A. Roberts, and H. D. Klenk. 2004. Neuraminidase is important for the initiation of influenza virus infection in human airway epithelium. J. Virol. 78:12665-12667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McKimm-Breschkin, J., T. Trivedi, A. Hampson, A. Hay, A. Klimov, M. Tashiro, F. Hayden, and M. Zambon. 2003. Neuraminidase sequence analysis and susceptibilities of influenza virus clinical isolates to zanamivir and oseltamivir. Antimicrob. Agents Chemother. 47:2264-2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McKimm-Breschkin, J. L. 2000. Resistance of influenza viruses to neuraminidase inhibitors: a review. Antivir. Res. 47:1-17. [DOI] [PubMed] [Google Scholar]
- 27.McKimm-Breschkin, J. L. 2002. Neuraminidase inhibitors for the treatment and prevention of influenza. Expert. Opin. Pharmacother. 3:103-112. [DOI] [PubMed] [Google Scholar]
- 28.McKimm-Breschkin, J. L., M. McDonald, T. J. Blick, and P. M. Colman. 1996. Mutation in the influenza virus neuraminidase gene resulting in decreased sensitivity to the neuraminidase inhibitor 4-guanidino-Neu5Ac2en leads to instability of the enzyme. Virology 225:240-242. [DOI] [PubMed] [Google Scholar]
- 29.McKimm-Breschkin, J. L., A. Sahasrabudhe, T. J. Blick, M. McDonald, P. M. Colman, G. J. Hart, R. C. Bethell, and J. N. Varghese. 1998. Mutations in a conserved residue in the influenza virus neuraminidase active site decreases sensitivity to Neu5Ac2en-derived inhibitors. J. Virol. 72:2456-2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Potier, M., L. Mameli, M. Belisle, L. Dallaire, and S. B. Melancon. 1979. Fluorometric assay of neuraminidase with a sodium (4-methylumbelliferyl-α-d-N-acetylneuraminate) substrate. Anal. Biochem. 94:287-296. [DOI] [PubMed] [Google Scholar]
- 31.Smith, B. J., P. M. Colman, I. M. von, B. Danylec, and J. N. Varghese. 2001. Analysis of inhibitor binding in influenza virus neuraminidase. Protein Sci. 10:689-696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smith, B. J., J. L. Kimm-Breshkin, M. McDonald, R. T. Fernley, J. N. Varghese, and P. M. Colman. 2002. Structural studies of the resistance of influenza virus neuraminidase to inhibitors. J. Med. Chem. 45:2207-2212. [DOI] [PubMed] [Google Scholar]
- 33.Stoll, V., K. D. Stewart, C. J. Maring, S. Muchmore, V. Giranda, Y. G. Gu, G. Wang, Y. Chen, M. Sun, C. Zhao, A. L. Kennedy, D. L. Madigan, Y. Xu, A. Saldivar, W. Kati, G. Laver, T. Sowin, H. L. Sham, J. Greer, and D. Kempf. 2003. Influenza neuraminidase inhibitors: structure-based design of a novel inhibitor series. Biochemistry 42:718-727. [DOI] [PubMed] [Google Scholar]
- 34.Varghese, J. N., J. L. McKimm-Breschkin, J. B. Caldwell, A. A. Kortt, and P. M. Colman. 1992. The structure of the complex between influenza virus neuraminidase and sialic acid, the viral receptor. Proteins 14:327-332. [DOI] [PubMed] [Google Scholar]
- 35.Varghese, J. N., P. W. Smith, S. L. Sollis, T. J. Blick, A. Sahasrabudhe, J. L. McKimm-Breschkin, and P. M. Colman. 1998. Drug design against a shifting target: a structural basis for resistance to inhibitors in a variant of influenza virus neuraminidase. Structure 6:735-746. [DOI] [PubMed] [Google Scholar]
- 36.Von, I. M., W. Y. Wu, G. B. Kok, M. S. Pegg, J. C. Dyason, B. Jin, P. T. Van, M. L. Smythe, H. F. White, and S. W. Oliver. 1993. Rational design of potent sialidase-based inhibitors of influenza virus replication. Nature 363:418-423. [DOI] [PubMed] [Google Scholar]
- 37.Wei, X., M. C. Els, R. G. Webster, and G. M. Air. 1987. Effects of site-specific mutation on structure and activity of influenza virus B/Lee/40 neuraminidase. Virology 156:253-258. [DOI] [PubMed] [Google Scholar]
- 38.Yen, H.-L., M. L. Herlocher, E. Hoffmann, M. N. Matrosovich, A. S. Monto, R. G. Webster, and E. A. Govorkova. 2005. Neuraminidase inhibitor-resistant influenza viruses may differ substantially in fitness and transmissibility. Antimicrob. Agents Chemother. 49:4075-4084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zambon, M., and F. G. Hayden. 2001. Position statement: global neuraminidase inhibitor susceptibility network. Antivir. Res. 49:147-156. [DOI] [PubMed] [Google Scholar]